Abstract
Aim:
To evaluate the role of nasal carriage of Staphylococcus aureus in patients suffering from chronic urticaria.
Method:
All total 82 patients were included for this study. Study group comprised 57 patients with chronic urticaria and the control group comprised 25 healthy volunteers. Nasal swab specimens were taken from all the 82 patients for bacterial culture and antimicrobial sensitivity. Patients with chronic urticaria who had positive growth for S. aureus were treated with sensitive antimicrobial agent. Nasal swab specimens were taken again from all the patients who received antimicrobial therapy to ensure complete eradication of S. aureus. All patients were followed up for a period of 6 weeks after the treatment. Urticarial activity was measured with the help of urticarial activity score.
Results:
S. aureus was detected in swab specimens from the nasal cavity in 32 patients in the study group and 7 patients in the control group. In the study group, after the antimicrobial treatment, 9 patients (28.12%) had complete recovery from urticaria during the follow-up period; 4 patients (12.5%) showed partial recovery from urticaria while the remaining patients (59.37%) continued to suffer from urticaria.
Conclusion:
This study showed that nasal carriage of S. aureus can act as an etiological factor in chronic urticaria.
Keywords: Nasal carriage, Staphylococcus aureus, urticaria
Introduction
Urticarial skin eruptions are known to be associated with some of the bacterial infections and foci of chronic infections are found to be associated with chronic urticaria.[1] The exact mechanism of urticaria due to infectious agents is not known. It has been postulated that these agents trigger release of histamine, leukotrienes, responsible for urticaria and angioedema, from the mast cells and basophils by IgE antigen complex; or through anaphylotoxin C3a, C4a generated through activation of complement system or through the kinins, e.g., bradykinin.[2,3] Staphylococcus aureus usually occur as a commensal on skin; it also occurs in the nose frequently in about a third of the population[4] and throat less commonly. Recently, it has been reported that nasal carriage of S. aureus as a focus of infection can play a role in the etiology of chronic urticaria.[5]
The aim of this study was to evaluate the role of nasal carriage of S. aureus in patients suffering from chronic urticaria. It was a clinic-based study.
Method
All total 82 participants were included for this study. Study group comprised 57 (Male: 25 and Female: 32; Age group: 18-40 year; Mean age: 28.92 year) patients with chronic urticaria. The control group comprised 25 healthy volunteers who were selected randomly (Male: 11 and Female: 14; Age group: 18-35 year; Mean age: 26.65 year). Urticarial activity was measured with the help of urticarial activity score in the study group.
Nasal swab specimens were taken from all the 82 patients and sent for bacterial culture (in Nutrient Agar media) and antimicrobial sensitivity. Patients with chronic urticaria who had positive growth for S. aureus were treated with sensitive antimicrobial agent - they were advised to apply topical antibiotic ointments to the anterior nares of the nose (3 times a day for 1 week) as well as to take a course of oral antibiotic (antibiotic agents were selected as per culture-sensitivity report).
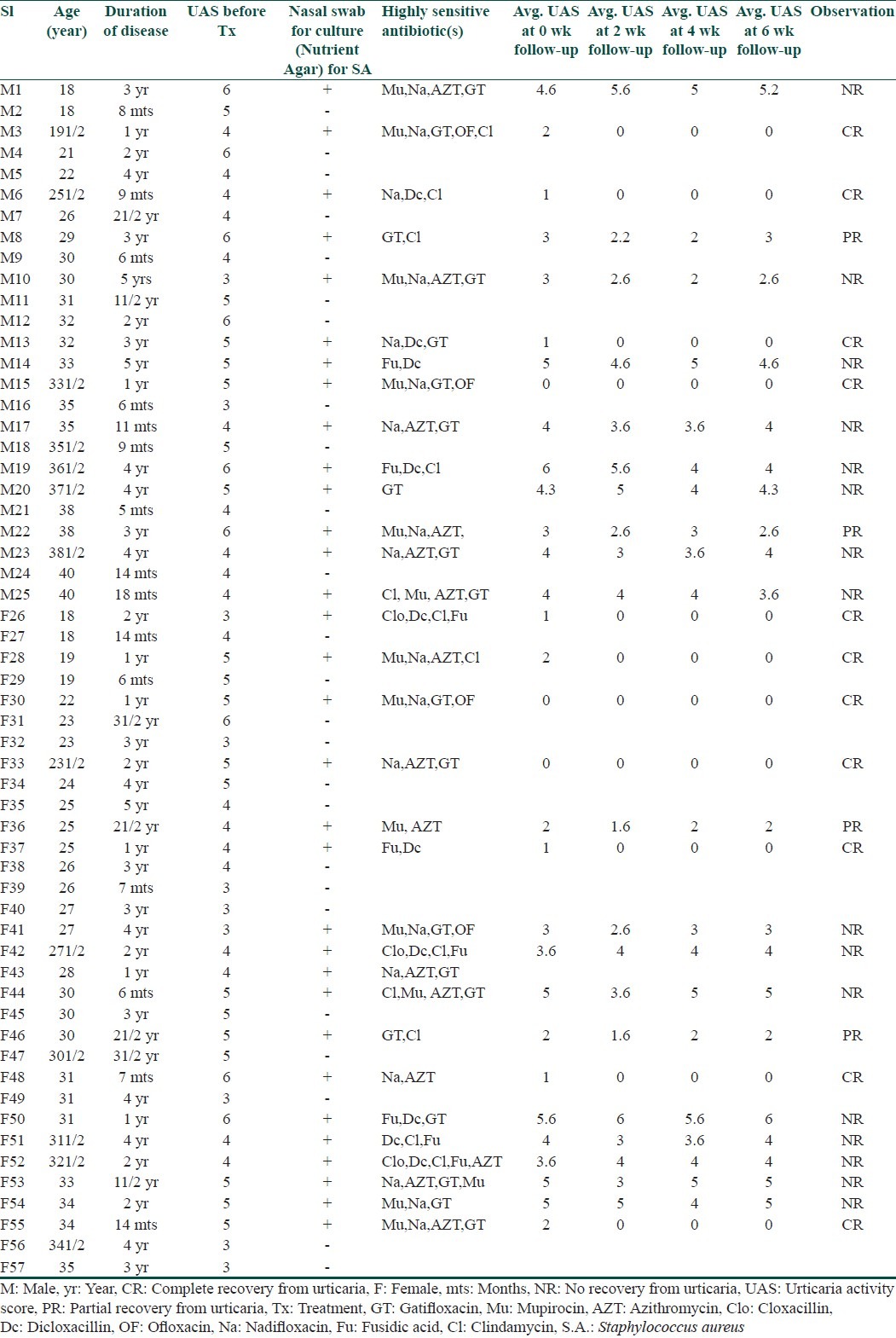
Nasal swab specimens were taken again for culture (in Nutrient Agar) from all the patients who received antimicrobial therapy to ensure complete eradication of nasal carriage of S. aureus. After completion of successful antimicrobial therapy, all patients were followed up at 2-week interval for a period of 6 weeks. On each follow-up, a thorough history was taken from each patient to calculate the average urticarial activity score. Patients whose urticaria was not controlled by antimicrobial therapy were allowed to take antihistaminic only on demand basis.
Patients with chronic urticaria associated with physical urticarias and atopy were not included in this study to avoid complicacy. Pregnant and lactating women were not included in this study. A valid written consent was obtained from each patient.
Results
S. aureus was detected in swab specimens from the nasal cavity in 32 patients (56.14%) in the study group and 7 patients (28%) in the control group. In the study group, after the antimicrobial treatment, 9 patients (28.12%) had complete recovery from urticaria during the follow-up period; 4 patients (12.5%) showed partial recovery (Average UAS≤half of initial UAS) from urticaria while the remaining 19 patients (59.37%) continued to suffer from urticaria [Tables 1–3].
Table 1.
Summary of result
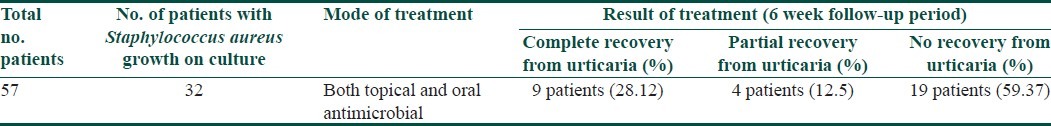
Table 3.
Detail result of control group
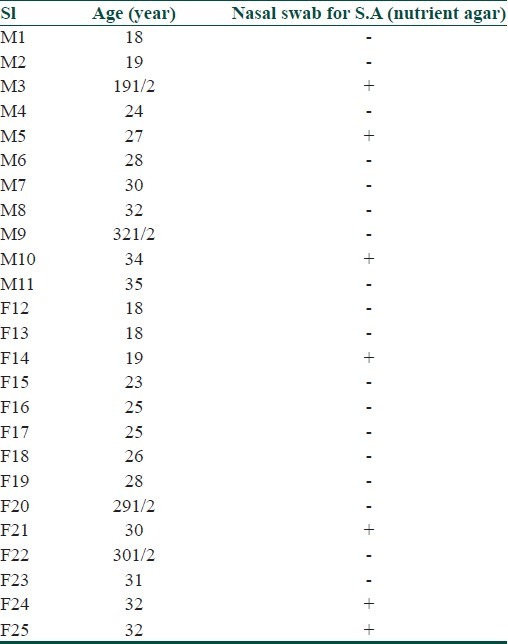
Table 2.
Detail result of study group
Discussion and Conclusions
Chronic infections due to bacteria are found to be associated with some cases of urticaria and treatment of such foci has been helpful in some cases of urticaria although not in all cases.[6,7] However, there are studies showing that chronic bacterial infection has no significant role in the etiology of chronic urticaria.
In the study conducted by Ertam et al.,[5] S. aureus was detected in swab specimens from the nasal cavity in 50 of the 94 patients (53.2%) with chronic urticaria showing high nasal carriage of S. aureus in patients with chronic urticaria indicating the role of S. aureus as an occult focus of infection in chronic urticaria.
In the present study, 56.14% patients in study group showed presence of S. aureus in the nasal swab specimens. This high nasal carriage of S. aureus in patients with chronic urticaria compared to controls (28%) in the present study is statistically significant (χ2 test). Findings of the present study support the observation of the study conducted by Ertam et al.
But in the present study, only 28.12% of patients with nasal carriage of S. aureus suffering from chronic urticaria had complete clearance of uricaria following eradication of their nasal carriage.
While 12.5% patients in the study group had only partial relief from urticaria indicating the presence of multiple etiological factors in those cases; in these cases the nasal carriage of S. aureus acted as an aggravating factor in the course of urticaria.
On the other hand, majority of the patients (59.37%) with nasal carriage of S. aureus suffering from chronic urticaria had received no benefit from the treatment and hence showing that nasal carriage of S. aureus had no relation with their urticaria; these cases were likely to have other cause(s) as the etiological factor(s), for example autoimmunity, etc.
Although high prevalence of nasal carriage of S. aureus in patients with chronic urticaria in the study group was recorded in this present study, only less than one-third of the total cases received benefit of successful antimicrobial therapy and statistically, large sample test shows that value of Z > 2.58 and thus this value is insignificant at 1%.
This study showed that nasal carriage of S. aureus may act as an etiological factor only in some cases in chronic urticaria; however, the result of this study failed to prove the relevance of high nasal carriage of S. aureus in the etiopathogenesis of urticaria. However, the present study is a clinic based study and the study group was small. A further multicentric study comprising large number of patients with longer follow-up will be more informative.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Wedi B, Raap U, Wieczorek D, Kapp A. Urticaria and infections. Allergy Asthma Clin Immunol. 2009;5:10. doi: 10.1186/1710-1492-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cherry DJ. Cutaneous manifestations of systemic infections. In: Feigin RD, Cherry JD, editors. Textbook of pediatric infectious Diseases. 2nd ed. Philadelphia: W.B. Saunders Co; 1987. pp. 786–7. [Google Scholar]
- 3.Mebsh ME. Staphylococcal infection. In: Feigin RD, Cherry DJ, editors. Textbook of pediatric infectious disease. 2nd ed. Philadelphia: W.B.Saunders Co; 1987. pp. 1260–92. [Google Scholar]
- 4.Whitt DD, Salyers AA. Bacterial pathogenesis: A molecular approach. 2nd ed. USA: ASM Press; 2002. [Google Scholar]
- 5.Ertam I, Biyiki SE, Yazkan FA, Aytimur D, Alper S. The frequency of nasal carriage in chronic urticaria patients. J Eur Acad Dermatol Venereol. 2007;21:777–80. doi: 10.1111/j.1468-3083.2006.02083.x. [DOI] [PubMed] [Google Scholar]
- 6.Thanpaichitr K. Chronic urticaria associated with bacterial infectins. Cutis. 1981;27:653–6. [PubMed] [Google Scholar]
- 7.Federman DG, Kirsner RS, Moriarty JP, Concato J. The effect of antibiotic therapy for patients infected with Helicobacter pylori who have chronic urticaria. J Am Acad Dermatol. 2003;49:861–4. doi: 10.1016/s0190-9622(03)00846-6. [DOI] [PubMed] [Google Scholar]


