Sir,
The cutaneous manifestations of hyperthyroidism and hypothyroidism are varied and are important for the dermatologists.[1] In hyperthyroidism, the skin is warm, moist, soft, velvety, and smooth simulating the skin texture of an infant. The warmth is secondary to increased cutaneous blood flow and peripheral vasodilation, which is also responsible for facial flushing and palmar erythema.[2,3] Hypothyroidism or thyroid hormone deficiency causes changes in the skin including thickening, hyperkeratosis, diffuse loss of scalp hair, and atrophy of nails.[4,5] The skin is cold, dry, and pale with widespread xerosis, especially on the extensor surfaces.[6]
We selected 50 patients for the study and all the patients were subjected to routine investigations and specialized investigations like T3, T4, TSH, and skin biopsy.
Results
In our study, 72% patients had hypothyroidism and 28% patients had hyperthyroidism. The cutaneous features in patients with hyperthyroidism were warm, moist skin, with increased temperature seen in 85.7% of the patients, Exophthalmos was seen in 85.7% of the patients, diffuse non-scarring alopecia was seen in 71.4% of the patients, palmoplantar hyperhidrosis was seen in 64.3% of the patients, facial flushing was seen in 57.1% of the patients, skin pigmentation in 50% of the patients, pretibial myxedema [Figure 1] was seen in 42.8% of the patients, and nail changes like onycholysis and plummers nails [Figure 2] were seen in 28.6% of the patients. Classic histopathological features of pretibial myxedema consisted of normal collagen in the papillary dermis and separation of the collagen bundles by mucin. Mucin staining demonstrated abundant diffuse mucin within the dermal fenestrations as large amounts of glycosaminoglycans diffusely dispersed in the reticular part of the dermis [Figure 3]. The most common cutaneous feature in patients with hypothyroidism, in our study, was coarse, rough, dry skin seen in 100% of the patients, followed by pallor of skin, with carotenemia seen in 52.75% of the patients, nail changes in 38.9% of the patients, diffuse hair loss in 33.3% of the patients, palmoplantar keratoderma in 33.3% of the patients, and loss of a lateral third of the eyebrows in 22.2% of the patients. Myxedematous facies [Figure 4] were seen in 12% of the hypothyroid patients in our study. Regarding the association of thyroid disease with other autoimmune diseases, it was seen that the most commonly associated autoimmune disease was vitiligo, seen in 8% of the patients, urticaria was seen in 6% of the patients, and alopecia areata was seen in 4% of the patients. To conclude, dermatologists need to be cognizant of the manifold cutaneous manifestations of thyroid disease. Skin signs suggestive of either hyperthyroid or hypothyroid states should be followed up by routine thyroid function studies. Should the thyroid disease be classified as autoimmune, the clinician should be vigilant for any of the potential associated disorders for which the patient may be at risk throughout his / her entire life.
Figure 1.

Pretibial myxedema in a 45-year-old female
Figure 2.

Plummers nails in a patient with hyperthyroidism
Figure 3.
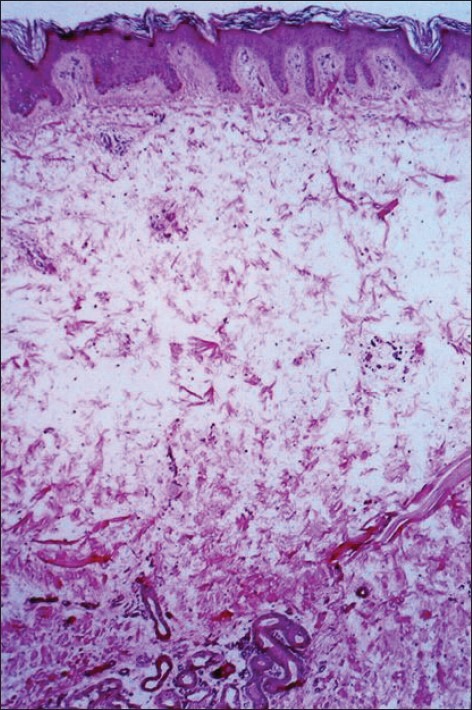
Photomicrograph showing separation of collagen fibers by mucin and lymphocytic infiltration (mucicarmine stain, 100×)
Figure 4.

Typical myxedema facies with puffy face, large tongue, and coarse features
References
- 1.Mullin GE, Eastern JS. Cutaneous signs of thyroid disease. Am Fam Physician. 1986;34:93–8. [PubMed] [Google Scholar]
- 2.Nixon DW, Samols E. Acral changes associated with thyroid diseases. JAMA. 1970;212:1175–81. [PubMed] [Google Scholar]
- 3.Heyman WR. Advances in cutaneous manifestations of thyroid disease. Int J Dermatol. 1997;36:641–5. doi: 10.1046/j.1365-4362.1997.00321.x. [DOI] [PubMed] [Google Scholar]
- 4.King LR, Braunstein H, Chambers D, Goldsmith R. A case study of peculiar soft-tissue and bony changes in association with thyroid disease. J Clin Endocrinol Metab. 1959;19:1323–30. doi: 10.1210/jcem-19-10-1323. [DOI] [PubMed] [Google Scholar]
- 5.Frienkel RK, Frienkel N. Hair growth and alopecia in hypothyroidism. Arch Dermatol. 1972;106:349–52. [PubMed] [Google Scholar]
- 6.Heymann WR. Cutaneous manifestations of thyroid disease. J Am Acad Dermatol. 1992;26:885–902. doi: 10.1016/0190-9622(92)70130-8. [DOI] [PubMed] [Google Scholar]


