Abstract
Ostium secundum atrial septal defect (ASD) is a common congenital heart defect. The adverse prognosis of untreated ASD diagnosed in childhood is well studied and percutaneous device closure of these ASDs has evolved to become the standard of care in both pediatric and young adult populations. There is a growing body of literature that suggests the benefits of ASD closure are not restricted to younger populations. In older adults, there are beneficial effects on cardiac chamber geometry, pulmonary artery pressures, patient symptoms and exercise capacity with closure of the ASD, and these salutary effects appear to be more pronounced the earlier the defect is closed. There may even be a reduction in the development of atrial arrhythmias, although this remains to be conclusively demonstrated. In this review, we summarize the literature regarding ASD closure in older adults. The weight of evidence suggests that ASD should be closed percutaneously earlier rather than later, and consideration should be given to percutaneous device closure of ASD in adults upon diagnosis, rather than waiting for symptoms or cardiac chamber dilatation.
Keywords: Ostium secundum atrial septal defect (ASD), congenital heart defect, percutaneous device closure, older adults
Introduction
Atrial septal defect (ASD) is the second most common congenital heart disease in adults, accounting for approximately 10% of all congenital heart lesions. Isolated ASD results from abnormal development of the septa that partition the common atrium of the developing heart into right and left chambers. 70% of ASDs are of the ostium secundum variety. The incidence of ASD is approximately 3 per 10,000 live births. For the remainder of this article ASD will refer to isolated ostium secundum ASD unless otherwise specified.
Surgical correction is the standard of care for other types of ASD such as ostium primum and sinus venosus ASD. The surgical approach was once the standard of care for secundum ASD, proving to be both safe and effective. It remains as such in many developing countries. However, over the past few decades many devices have been developed to treat secundum ASD percutaneously. Currently two such devices are approved by the FDA in USA: The Amplatzer Septal Occluder (ASO) and the Helex closure device. The benefit of the percutaneous approach has been well-demonstrated in the pediatric population. The purpose of this review is to illustrate the safety and efficacy of percutaneous device closure of secundum ASD in the adult population. Following percutaneous closure of ASD, adults of all ages experience improved symptoms, reduction in pulmonary artery (PA) pressure and reverse remodeling of the right ventricle (RV). It appears that these effects are more pronounced when the defect is closed earlier, rather than later. The transcatheter approach is evolving to become the new standard of care for adults with ASD. ASD closure should be considered in all hemodynamically significant secundum ASDs regardless of the patient’s age or symptoms.
Natural history of ASD
Natural history of ASD diagnosed in childhood is that the ASD diameter when untreated increases in 65% of cases, and 30% will have more than a 50% increase in diameter. Only 4% of ASDs close spontaneously [1]. A patient with isolated secundum ASD is often asymptomatic until the third and fourth decade of life. Typical symptoms that ensue include decreased exercise capacity, fatigue, syncope and palpitations. Patients with significant shunting may develop right ventricular failure, atrial tachycardia, pulmonary hypertension and embolic events all of which can lead to significant morbidity and potential mortality.
The age at which a patient becomes symptomatic is highly variable and does not correlate well with shunt size (Figure 1). The pressure gradient between the two atria and the amount of shunt flow depend upon both the size of the defect, and the compliance of the right and left sides of the heart. Left untreated over time, even small ASDs can develop increased left-to-right shunting due to progressive increase in left ventricular (LV) diastolic pressure with aging, which causes increased left atrial pressure. In patients who develop pulmonary hypertension (PHTN) from their ASD, approximately 10% will progress to Eisenmenger’s syndrome. Due to the chronic nature of the disease and patient compensation over time many patients remain unaware of their decreased exercise capacity and only realize their symptom improvement post procedure [2].
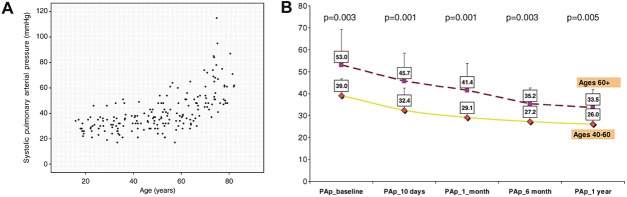
Figure 1.
Relationship between pulmonary artery pressure and age in patients with secundum ASD. (A) Pulmonary artery pressure correlates with patient age. Note there is an exponential increase in pulmonary artery pressure above age 60. (Reprinted with permission from Humenberger M, et al. European Heart Journal 2011;36:553-560. (B) Pulmonary artery pressure improves after ASD closure regardless of patient age. (Reprinted with permission from Yalonetsky S, et al. Congenit Heart Dis 2009; 4: 17-20). ASD = atrial septal defect.
Two hundred unoperated patients over the age of 40 were followed by Rosas et al. from 1.6 to 22 years. They observed 37 events (18.5%): 5 sudden death, 7 heart failure, 13 severe pulmonary infection, 5 embolisms and 4 strokes. Predictors of poor outcome were age at presentation, pulmonary HTN or arterial O2 sat < 80% [3]. Thus, adult patients with unrepaired ASDs are at risk for major cardiovascular events. ASD repair can prevent RV failure, pulmonary hypertension, atrial arrhythmia and thromboembolic complications (Table 1).
Table 1.
Clinical trials of percutaneous closure of secundum ASD involving more than 50 patients
| Study | Study type | Avg age (years) | Avg ASD size | Avg QP/QS | Closure indication | Subjects | Follow up | Change in RVEDD | Change in PAP (mmHg) | New atrial arrythmias | Major complications | Mortali ty | Residual shunt | Procedural success rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jategonkar | Observational | 69.9±5.3 | 14.8±5.8 mm | N/A | PHTN, significant L to R shunt, symtoms | 96 | 3 months | 38.9±8.7 to 32.3±8.6 | N/A | 16 PAF | None | 0% | Tiny shunt in 16.9% | N/A |
| Humenburger | Observational | 49±18 | 22 mm | 2.2 | Significant L to R shunt, RV volume overload | 236 | 12 months | 43±7 to 34±6 | N/A | 11 AF | N/A | N/A | N/A | 99.60% |
| Balint | Retrospective | 59±15 | 18 ±7 mm | N/A | Moderate or severe PAH | 54 | 31 months | N/A | 58 to 44 | none | N/A | 2 | 4 | N/A |
| Young | Observational | 53.9±15.7 | 18.8±5.5 mm | 2.3 | N/A | 215 | 15 months | N/A | 30 to 25 | 37.5 % reduction | N/A | N/A | Tiny shunt 18.7% | 90.20% |
| Swan | Retrospective | 69±5.8 | 17.5 mm | 2.2 | Right heart dilatation | 50 | 6 weeks | 51.2±9.1 to 43.6±6.6 | N/A | none | 1 pulmonary edema | 0% | Small shunt 16% | 100% |
| Giardini | Observational | 39±19 | 18±5 mm | N/A | Right heart dilatation, CHF, exercise intolerance | 134 | 4.8±2.7 years | N/A | N/A | 6 PAF and 2 Permanen t AF resolved. | N/A | N/A | N/A | N/A |
| Majunke | Observational | 45.8±16.2 | 21.2±5.1 mm Stretched | 1.9±0.7 | QP/Qs > 1.5, dilated RV, paradoxical emboli and symptoms | 650 | 8 years | N/A | 33.3±10.6 to 28.3±10.1 | 4.3% new onset AF | 0.50% | 0.20% | Small 3.4%, Large 0.2% | 99% |
| Spies | Observational | 50±15 | N/A | N/A | N/A | 240 | 20 months | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Jateganokar | Retrospective | 49.4±18 | 14.7±5.3 mm | N/A | N/A | 332 | 904±839 days | 36.4±7.9 to 29.4±6.8 | n/A | 1.20% | 1 | 12.3%, 0.3% severe | 99.40% | |
| Patel | Retrospective | 57.9±11.9 | 17.2±7.3 mm | 2.2 | RV enlargement by echocardiography, clinical symptoms | 113 | 3 years | 35.3±7.6 to 23.8±6.6 | N/A | 2 | 3.50% | N/A | Small 5%, Medium 1% | 99% |
| Wilson | Retrospective | N/A | 22±6 mm stretched | 2.3±1.2 | verload and/or QP/QS≥ 1.5:1 | 149 adults | 1.8 years | N/A | N/A | 6 new cases 3% | 2% | 0% | Moderate 1.4%, large 0.7% | 95% |
| Spies | Retrospective | 47 | 23mm | 1.9 | N/A | 170 | 13 month | N/A | N/A | 6 new AF | 6.50% | 0% | Small 2.5% | 98% |
| Silversides | Prospective | 50±17 | 16±6 mm | N/A | N/A | 200 | 1.9±0.9 years | N/A | N/A | 7 new PAF, 4 new chronic AF | N/A | N/A | N/A | N/A |
| Knepp | Retrospective | 49.9±15.4 | 18 mm stretched | N/A | N/A | 65 adults | 73 months | N/A | N/A | 3 new AF in adults | 0.70% | 0% | N/A | 97% |
| Krumsdorf | Prospectiv | 48±15 | 20±6 mm stretched | 2.0±0.7 | N/A | 407 | 12 months | N/A | N/A | N/A | N/A | N/A | N/A | 100% |
QP/QS: ratio of pulmonary to systemic flow. RVEDD: Right Ventricular End Diastolic Diameter in millimeters. PAP: Mean Pulmonary Artery Pressure in mmHg. NYHA: New York Heart Association classification for heart failure. Peak VO2: maximal oxygen uptake during maximum exercise. RAVI: right atrial volume index in mm3/m2. PAF: paroxysmal atrial fibrillation. AF: atrial fibrillation. LVEDD: left ventricular end diastolic diameter in millimeters. ASO: atrial septal occluder device. Avg: Average. Mos: months. Yrs: years.
Secundum ASD treatment: surgery vs. medical management
The results of surgically corrected ASD were studied in 123 patients undergoing isolated ASD repair at the Mayo clinic 27 to 32 years after the procedure. Overall survival was 74% compared to 85% for age sex matched controls. Peri-operative mortality was 3.3% (4 deaths). In patients below 24 years of age, survival was the same as age matched controls. In patients who were older than 41, the 27 year survival was 40% compared to 59% in the control group. Independent predictors of long term survival were age at operation and main pulmonary artery systolic Pressure (PASP) [4]. The benefit from surgical approach in adults was once again demonstrated in a later retrospective analysis of 179 patients with isolated ASD diagnosed after age 40 who were followed for a mean of 8.9 years. 47% underwent surgery and the 53% were treated medically. Surgery reduced all cause mortality with relative risk of 0.31 with a 10 year survival rate of 95% vs. 84% compared to medical group. The rate of cerebrovascular accident (CVA) and atrial fibrillation (AF) in both groups were equal, however surgery prevented further functional deterioration [5].
Surgical vs. medical therapy were finally compared prospectively in a randomized trial of 473 patients over 40 with a median follow up of 7.3 years. Overall mortality rate was not statistically different. There was however a higher rate of recurrent pneumonia in the medical arm. There was also a trend towards higher sudden death, CHF, and overall mortality in medical arm which did not reach statistically significance [6].
Benefit of percutaneous ASD occlusion vs. surgery in adults
King and Mills attempted the first transcatheter closure of secundum ASD in 1976. Over the next three decades many different devices and techniques have been introduced. There are currently two such devices which are FDA approved in USA: The Amplatzer Septal Occluder (ASO) device which is a prosthesis that consists of two round nitinol wire disks connected together with a short connecting disk. It can be used in small, moderate and large ASDs. The second is the Helex Septal Occluder (HSO), which is a low profile device that has a double disk non-self-centering design. It has a built-in method for retrieval. It is used for small and moderate size ASDs.
Percutaneous ASD closure results not only in symptomatic improvement and increase in exercise capacity, but also in improvements in cardiac chamber geometry and in cardiac hemodynamics (Table 2). Majunke et al. studied 650 consecutive adults with median age of 45 who underwent closure with ASO. The patients had a mean PASP 33.3 mmHg. Implantation was successful in 98% of patients. Complete closure was achieved in 96% pts (22 of 25 of the incomplete closures had very small residual shunt). Mean PASP decreased to 28.3 mmHg. Intra-procedural complications consisted of 2 pts with device embolization, one pt with transient ST depression. 0.9% needed emergent CT surgery. The authors concluded that ASD closure in adults is safe, efficient with excellent long term outcome [7]. Others have shown that ASD closure with an ASO device leads to significant decrease in RV size (right ventricular end diastolic diameter [RVEDD] 35.3 mm to 29.2 mm in first 24 hours) and improvement of clinical symptoms with an extremely high success rate (112 of 113). As such the authors suggest that ASD closure device should be the first option for management of secundum ASDs [8]. Similar encouraging results have been reported in the Helex closure device. Jones et al. compared HSO to surgery at 12 month follow up and found that closure rate, major and minor adverse outcomes were the not different [9]. Concern about potential development of mitral regurgitation was essentially put to rest when Wilson et al reported that a 2 year follow up of data in 227 adult and children post ASO showed 98.5% success for closure rate, resolution of AF in half of the patients post procedure and the degree of MR which was unchanged in 88% pts (In 1% MR increased by 2 grades and in 9% increase of 1 grade. 7% had decrease is MR) [10].
Table 2.
Beneficial effects of percutaneous ASD closure in adults.
| Definite effects of ASD closure | Possible Effects of ASD closure |
|---|---|
| RV size ↓ | Atrial arrhythmias ↓ |
| LV size ↑ | |
| PA pressure ↓ | |
| RA size ↓ | |
| Exercise capacity ↑ | |
| NYHA class ↓ |
The comparison of surgical vs. percutaneous approach was reported in a large cohort of 596 pediatric patients in a non-randomized parallel group study. In this study, 442 patients received ASO device closure and 154 had surgical closure. Success rate was 95.7% in ASO and 100% in surgical group. There was no mortality observed in either group, however complication rate was significantly lower in the device group (7.2% ASO vs. 24.0% surgical). The length of stay was shorter in the transcatheter arm (1.0 vs. 3.4 days) [11]. Similar rate of success (98%) with an increased length of stay (8 vs. 3 days) was observed by other studies [12]. Five-year follow up data by Knepp et al. for ASO closure showed complete closure rate was 97% with very low incidence of mortality and morbidity [13].
Given the success rate of closure devices and the lower complication rate, adult patients are more likely to select percutaneous approach for secundum ASD closure in order to avoid receiving a sternotomy and having to undergo cardiopulmonary bypass. From a public health standpoint, since the efficacy of both procedures are equal and the complications are generally lower in the percutaneous group there is a significant cost reduction benefit due to a shorter recovery and shorter hospital stay.
Closure device in the older adult patient population
Harjula et al. studied late result of surgery in patients older than 60. One patient died shortly after surgery (operative mortality, 6%) and major postoperative complications were found in four additional patients (24%). There was however an increase in effort capacity in all surviving patients. The mean PAP had also significantly decreased (25 mmHg vs. 33 mmHg) [14]. In contrast a study of 3 different patient age groups (78 patients younger than 40 years, 84 between 40 to 60 years, and 74 patients older than 60 years) undergoing transcatheter ASD closure showed an improvement in morbidity in all groups with regression of PA pressure and RV size with no increased mortality and recommended ASD closure regardless of age and symptoms in adults [15]. In a comparative study, Rosas et al. showed the superiority of ASO compared to surgery in a 162 patients. All patients were closed successfully with zero mortality, however the surgical group had a significantly higher primary event rate (25% vs. 13%) driven by moderate bleeding, mild respiratory infection and arrhythmias. The event rate was even higher in older patients over the age of 40 and those with systolic PA pressure above 50 mmHg [16].
Swan et al and a more recent study by Khan et al. both demonstrated that short-term follow up in one year in small groups of patients with median age of 70 and as old as 85 have lead to improvement of New York Heart Association (NYHA) class, the 6 minute walk time and improvement of physical and mental health score with an extremely high procedural success rate (98%) [17,18]. Furthermore, Nakahawa et al. prospectively showed that in a population of patients older than 70 years with hemodynamically significant ASD, percutaneous closure is feasible, efficacious and safe. The closure led to significant improvement of PA pressure and NYHA functional class, as well as reversal of RV enlargement [19] (Figure 2).
Figure 2.
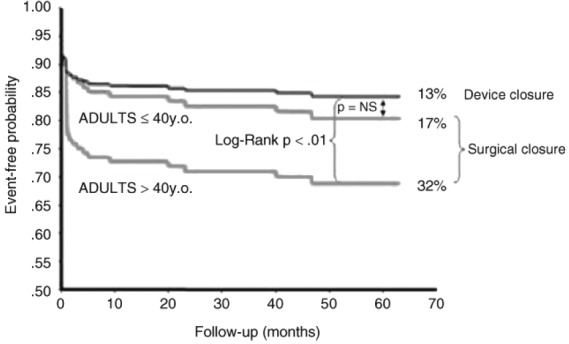
Comparison between surgical and device closure of ASD. Adjusted event-free survival is similar between surgery and percutaneous device closure of ASD in patient under age 40. However, in patients over 40 years, surgery is associated with lower event-free survival. (Reproduced with permission from Rosas M, et al. Congenit Heart Dis 2007; 2: 148-155).
Indications and contraindications to percutaneous ASD closure
The ACC/AHA Guidelines [20] suggest that secundum ASDs larger than 5 mm should be closed in the following scenarios, as long as the PA Pressure is < 2/3 Systemic pressure, pulmonary vascular resistance (PVR) is < 2/3 systemic vascular resistance (SVR), or when the patient is responsive to either pulmonary vasodilator therapy or test occlusion of the defect: (1) Presence of symptoms such as exercise intolerance, shortness of breath, heart failure or atrial arrhythmias; (2) Evidence of RV or RA dilatation on echocardiogram or cardiac CT/MRI with or without symptoms; (3) Presence of paradoxical embolism regardless of the size of the defect; (4) Documentation of orthodeoxia-platypnea. Contra indications are as follows: (1) Presence of other congenital cardiac deformities such as anomalous pulmonary venous drainage, or ostium primum, sinus venosus or coronary sinus ASD which would require surgical correction (should be closed surgically); (2) Severe irreversible pulmonary HTN and no evidence of left to right shunt.
Most operators agree that the majority of secundum ASDs can be closed percutaneously. When it is not feasible, the surgical approach is recommended. Defect size > 40 mm and lack of adequate rims of tissue from the defects to important surrounding structures, atrial thrombus and contraindication to antiplatelet therapy are in this category [20].
Changes in cardiac chamber size and hemodynamics after closure
The effect of ASD closure on cardiac chambers following either surgical or percutaneous closure is well-documented. In a study looking at a mixture of pediatric and adult patients after successful device closures of ASD Kaya et al. observed that over a 2 year follow up right ventricular end diastolic diameter (RVEDD) was lowered from 36mm to 30mm and the left ventricular end diastolic diameter (LVEDD) rose from 33mm to 37mm. Furthermore there was a significant reduction of PAP on echocardiogram, and clinically significant improvement in exercise capacity [21]. Another analysis of patient groups in the 40-59 years and 60+ range showed that when ASD was diagnosed after age 40 there is more pulmonary HTN, tricuspid regurgitation (TR), and right ventricular dilatation. On follow up post closure the older patient population had a greater reduction of PA pressure (19% vs. 11.3%) [22].
In addition to improving the right sided dilatation, including right atrial volume, the ejection fraction of the right ventricle also improves after percutaneous ASD closure (35.5% to 42%) without a significant change in LVEF or LV mass [23]. As encouraging as the data may be on reverse remodeling, it is important to understand that in more than 50% of adult patients reverse remodeling might not be complete. Fang et al showed that right atrial volume index (RAVI) did not fully normalize in patients who had a larger baseline QP/QS, more TR, higher PASP and larger chambers [24]. This suggests that earlier closure of the ASD, before significant right heart dilatation and PHTN have occurred, may prevent the irreversible increase in RV size and PA pressure. Thus earlier closure my lead to better outcomes for patients.
Potential improvement in functional capacity and heart failure symptoms
Pulmonary HTN is one of the most serious long-term side effects of ASD. Pulmonary HTN in the setting of ASD likely happens due to histological changes of pulmonary artery and arterioles due to chronic exposure to increased blood flow and resultant luminal narrowing. 11% of patients referred for percutaneous ASD closure have moderate or severe pulmonary HTN. There have been a lot of questions about safety and efficacy of patients with pulmonary HTN who undergo surgical or percutaneous ASD closure. To address this issue, Balint et al. followed 54 patients with moderate (50-59 mmHg) or severe (≥60 mmHg) PHTN who underwent successful device implantation at late follow up of 31 months. 2 patients died. At follow up RVSP decreased from 58 to 44 mmHg, however only 43.6% of patients had normalization of RVSP (<40 mmHg) and 15.4% had persistent severe PHTN [25]. Independent predictors of moderate to severe pulmonary HTN are older age, larger ASD, female gender and at least moderate TR. At 15 months post ASD closure, the magnitude of reduction was respectively 0, 8, 17, 22 mmHg in patients with PASP <40 mmHg, 40-49 mmHg, 50-59 mmHg, 60+ mmHg [26].
In addition to the above-mentioned improvements in objective echocardiographic parameters, studies have shown that adult patients, particularly the older population, had significant symptom and functional class improvement. Jateganokar et al. showed an improvement of NYHA functional class and peak oxygen uptake in 96 patients in the 60-84 year age group [27]. The same authors reported a 3 month follow up of 332 patients with 99.4% closure success rate, with 123 patients reporting improvement of symptoms and 163 with no change [28]. Long term improvement in exercise capacity was not restricted to younger patients, supporting the argument that the ASD lesions in elderly should also be closed. The improvement of cardiopulmonary exercise stress testing at 6 months showed further increase at 36 month follow up [29].
Atrial tachyarrhythmias and ASD
Atrial tachyarrhythmia including AF are generally quite common among the ASD patient population and contribute to their morbidity. The most common arrhythmias in the patient population are AF and atrial flutter. New onset AF was seen in 12% of pts with an underlying ASD. Annual onset of new onset AF is 4.1% [30].
Both Murphy et al. and Gatzoulis et al. have shown that the surgical approach does not prevent the occurrence of arrhythmia [2,4]. Atrial arrhythmia is likely a byproduct of chronic right atrial dilatation and its increases in prevalence progressively with age. Silverside et al. suggested that device closure of an ASD before the onset of atrial arrhythmias may protect against the subsequent development of arrhythmia, in particular in patients less than 55 years of age [30]. In one surgical series comparing adults with ASD who underwent surgical repair vs. medical management showed that they had the same rate of late AF (13.8% vs 15.6%, p=NS) [31,35].
One hundred thirty four patients post ASO closure of their ASD and mean age of 39 were followed up for nearly 5 years. 14 had AF and/or atrial flutter before percutaneous procedure. Older patients had a higher prevalence of AF/Flutter. Patients without history of AF or those who had paroxysmal AF (PAF) showed very low annual risk (0%) of developing post procedural AF [32]. Overall, the chronic increase in atrial stretch likely leads to localized tissue damage and fibrosis and reduced regional atrial conduction velocity, with a subsequent increased propensity to atrial arrhythmia. The above data suggest that ASO is likely more protective against the development of atrial arrhythmias than surgical closure, presumably due to lack of pericardiotomy and atrial scar. Furthermore the reversal of chamber remodeling and decreased RA pressure is protective against future AF/Flutter development.
In a prospective study of 200 adult patients referred for ASD closure 20% had a history of atrial tachyarrhythmia (AT). AT was detected in 16% of pts in late follow-up post closure. After Closure of ASD, the likelihood of remaining arrhythmia free was highest in those without prior history of AT and age < 40 [31]. Taken together, these studies suggest a benefit in arrhythmia by closing defects at a younger age.
Specific complications
In addition to routine complications related to vascular access, there are complications related to the particular procedure as well. Complications of the procedure, including their incidence and management, have been reviewed extensively elsewhere [32-34].
The most serious and life threatening complication of ASD closure with a closure device is atrial roof/wall erosion leading to tamponade. The registry of complications of the ASO device was reviewed by Amin et al. At that time, over 30,000 devices had been implanted worldwide, 9000 of which had been in the USA. They found that from 1998 to 2004, a total of 28 cases of erosion were reported (0.1% rate). All erosions occurred at the dome of the atria near the aortic root. 25 of 28 cases were observed to have a deficient aortic rim or described as high ASD meaning deficient superior rim. The authors recommended the following modifications to decrease rate of erosion: avoid overstretching the balloon, use stop flow technique for balloon sizing (instead of “stretched balloon diameter”) and use gentle motion during the Minnesota Wiggle [32].
There exists a risk of acute pulmonary edema in a susceptible group of patients in both surgical and ASD closures immediately post procedure. When Shubert et al. reviewed the pulmonary edema data, the high-risk group was older and had a higher mean LA pressure (10 mmHg vs. 5 mmHg) and mean PA pressure (26 mmHg vs. 20 mmHg). 25% of these patients over 60 showed pathological atrial pressure rise after temporary septal balloon occlusion. Pre procedural anticongestive therapy with milrinone, dopamine and furosemide was effective in allowing for an uncomplicated post closure course [36].
Thrombus formation is seen in up to 1.2% of post ASD closure population. The observed rate is 0.8% in Helex device and 0% in Amplatzer device. There was a significantly higher rate of thrombus formation on devices such as Cardio-Seal, StarFlex and ASDOS (7.1%, 5.7% ASDOS 3.6%). Post procedure AF and persistent atrial septal aneurysm are significant predictors of thrombus formation. Resolution of thrombus has been achieved medically in 17/20 [37].
Summary and conclusions
Closure of secundum ASD percutaneously has become the standard of care in pediatric and young adult patients. The data presented in this paper strongly suggest that it should also be considered the standard of care in middle-aged and elderly patients (Figure 3). The volume of data from studies regarding percutaneous closure and their safety and efficacy have long surpassed the surgical data in these age-groups. Patients of all ages experience reduction in PA pressure, RV size and an improvement in functional capacity after percutaneous device closure of ASD, and these improvements appear to be greater if the defect is closed earlier. Given the low rate of complications and virtual lack of mortality, isolated secundum ASDs which are larger than 5 mm should be considered for percutaneous device closure regardless of symptoms or patient age.
Figure 3.
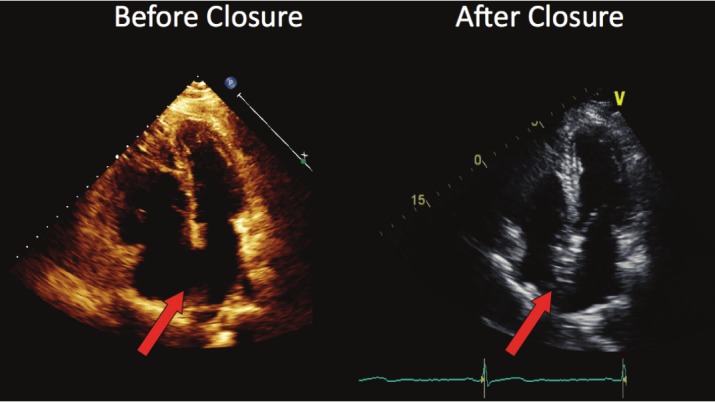
Improved cardiac chamber geometry after ASD closure. Echocardiography in the apical 4-chamber view before and 6 weeks after percutaneous device closure of a large secundum ASD. The arrows point to the defect before, and the ASO device after closure. These diastolic views demonstrate the reduction in size of the right atrium and ventricle, with increase in size of the left ventricle.
References
- 1.McMahon CJ, Feltes TF, Fraley JK, Bricker JT, Grifka Rg, Tortoriello TA, Blake R, Bezold Ll. Natural history of growth of secundum atrial septal defects and implications for transcatheter closure. Heart. 2002;87:256–259. doi: 10.1136/heart.87.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gatzoulis MA, Rodington AN, Somerville J, Shore DF. Should atrial septal defects in adults be closed? Ann Thorac Surg. 1996;61:657–659. doi: 10.1016/0003-4975(95)01043-2. [DOI] [PubMed] [Google Scholar]
- 3.Rosas M, Attie F, Sandoval J, Castellano C, Buendia A, Zabal C, Granados N. Atrial septal defects in adults ≥ 40 years old: negative impact of low arterial saturation. Int J Cardiol. 2004;93:145–155. doi: 10.1016/S0167-5273(03)00192-X. [DOI] [PubMed] [Google Scholar]
- 4.Murphy JG, Gersh BJ, McGoon MD, Mair DD, Porter CJ, Ilstrup DM, McGoon DC, Puga FJ, Kirklin JW, Danielson GK. Long-term outcome after surgical repair of isolated atrial septal defect: follow-up at 27 to 32 years. N Engl J Med. 1990;323:1645–1650. doi: 10.1056/NEJM199012133232401. [DOI] [PubMed] [Google Scholar]
- 5.Konstantinides S, Geibel A, Olschewski M, Gornandt L, Roskamm H, Spillner G, Just H, Kasper W. A comparison of surgical and medical therapy for atrial septal defects in adults. N Engl J Med. 1995;333:469–473. doi: 10.1056/NEJM199508243330801. [DOI] [PubMed] [Google Scholar]
- 6.Attie F, Rosas M, Granados N, Zabal C, Buendia A, Calderon J. Surgical treatment for secundum atrial septal defects in patients > 40 years old. A randomized clinical trial. J Am Coll Cardiol. 2001;38:2035–2042. doi: 10.1016/s0735-1097(01)01635-7. [DOI] [PubMed] [Google Scholar]
- 7.Majunke N, Bialkowski J, Wilson N, Szutnik M, Kusa J, Baranowski A, Heinisch C, Ostermayer S, Wunderlich N, Sievert H. Closure of atrial septal defect with the Amplatzer septal occluder in adults. Am J Cardiol. 2009;103:550–554. doi: 10.1016/j.amjcard.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Patel A, Lopez K, Banerjee A, Joseph A, Cao QL, Hijazi ZM. Transcatheter closure of atrial septal defects in adults ≥ 40 years of age: Immediate and follow-up results. J Interv Cardiol. 2007;20:82–88. doi: 10.1111/j.1540-8183.2007.00216.x. [DOI] [PubMed] [Google Scholar]
- 9.Jones TK, Latson LA, Zahn E, Fleishman CE, Jacobson J, Vincent R, Kanter K Multicenter Pivotal Study of the HELEX Septal Occluder Investigators. Results of the U. S. multicenter pivotal study of the HELEX septal occluder for percutaneous closure of secundum atrial septal defects. J Am Coll Cardiol. 2007;49:2215–2221. doi: 10.1016/j.jacc.2006.11.053. [DOI] [PubMed] [Google Scholar]
- 10.Wilson N, Smith J, Prommete B, O’Donnell C, Gentles TL, Ruygrok PN. Transcatheter closure of secundum atrial septal defects with the Amplatzer septal occluder in adults and children-follow-up closure rates, degree of mitral regurgitation and evolution of arrhythmias. Heart Lung Circ. 2008;17:318–324. doi: 10.1016/j.hlc.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K. Amplatzer investigators. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults. J Am Coll Cardiol. 2002;39:1836–1844. doi: 10.1016/s0735-1097(02)01862-4. [DOI] [PubMed] [Google Scholar]
- 12.Berger F, Vogel M, Alexi-Meshkishvili V, Lange PE. Comparison of results and complications of surgical and amplatzer device closure of atrial septal defects. J Thorac Cardiovasc Surg. 1999;118:678–680. doi: 10.1016/S0022-5223(99)70013-9. [DOI] [PubMed] [Google Scholar]
- 13.Knepp MD, Rocchini AP, Lloyd TR, Aiyagari RM. Long-term follow up of secundum atrial septal defect closure with the Amplatzer septal occluder. Congenit Heart Dis. 2010;5:32–37. doi: 10.1111/j.1747-0803.2009.00358.x. [DOI] [PubMed] [Google Scholar]
- 14.Harjula A, Kupari M, Kyosola K, Ventila M, Hartel G, Maaiies T, Mattila S. Early and late results of surgery for atrial septal defect in patients aged over 60 years. J Cardiovasc Surg. 1998;29:134–139. [PubMed] [Google Scholar]
- 15.Humenberger M, Rosenhek R, Gabriel H, Rader F, Heger M, Klaar U, Binder T, Probst P, Heinze G, Maurer G, Baumgartner H. Benefit of atrial septal defect closure in adults: impact of age. Eur Heart J. 2011;32:553–560. doi: 10.1093/eurheartj/ehq352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosas M, Zabal C, Garcia-Montes J, Buendia A, Webb G, Attie F. Transcatheter versus surgical closure of secundum atrial septal defect in adults: impact of age at Intervention. A concurrent matched comparative study. Congenit Heart Dis. 2007;2:148–155. doi: 10.1111/j.1747-0803.2007.00091.x. [DOI] [PubMed] [Google Scholar]
- 17.Khan AA, Tan JL, Li W, Dimopoulos K, Spence MS, Chow P, Mullen MJ. The impact of transcatheter atrial septal defect closure in older population: a prospective study. JACC Cardiovasc Interv. 2010;3:276–281. doi: 10.1016/j.jcin.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Swan L, Varma C, Yip J, Warr M, Webb G, Benson L, McLaughlin P. Transcatheter device closure of atrial septal defects in the elderly: technical considerations and short-term outcomes. Int J of Cardiol. 2006;107:207–210. doi: 10.1016/j.ijcard.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 19.Nakahawa K, Akagi T, Taniguchi M, Kijima Y, Goto K, Kusano KF, Itoh H, Sano S. Transcatheter closure of atrial septal defect in a geriatric population. Catheter Cardiovasc Interv. 2012 doi: 10.1002/ccd.23457. In Press. [DOI] [PubMed] [Google Scholar]
- 20.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasiles JW, Graham TP Jr, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD. ACC/AHA 2008 Guidelines for the management of adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2008;118:2395–2345. doi: 10.1161/CIRCULATIONAHA.108.190811. [DOI] [PubMed] [Google Scholar]
- 21.Kaya MG, Baykan A, Dogan A, Inanc T, Gunebakmaz O, Dogdu O, Uzum K, Eryol NK, Narin N. Intermediate-term effects of transcatheter secundum atrial septal closure on cardiac remodeling in children and adults. Pediatr Cardiol. 2010;31:474–482. doi: 10.1007/s00246-009-9623-y. [DOI] [PubMed] [Google Scholar]
- 22.Yalonetsky S, Lorber A. Comparative changes of pulmonary artery pressure values and tricuspid valve regurgitation following transcatheter atrial septal defect closure in adults and the elderly. Congenit Heart Dis. 2009;4:17–20. doi: 10.1111/j.1747-0803.2008.00245.x. [DOI] [PubMed] [Google Scholar]
- 23.Teo KS, Dundon BK, Molaee P, Williams KF, Carbone A, Brown MA, Worthley MI, Disney PJ, Sanders P, Worthley SG. Percutanous closure of atrial septal defects leads to normalisation of atrial and ventricular volumes. J Cardiovasc Magn Resonan. 2008;10:55. doi: 10.1186/1532-429X-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fang F, Yu CM, Sanderson JE, Luo XX, Jiang X, Yip GW, Lam YY. Prevalence and determinants of incomplete right atrial reverse remodeling after device closure of atrial septal defects. Am J Cardiol. 2011;108:114–119. doi: 10.1016/j.amjcard.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Balint OH, Samman A, Haberer K, Tobe L, McLaughlin P, Siu SC, Horlick E, Granton J, Silversides CK. Outcomes in patients with pulmonary hypertension undergoing percutanous atrial septal closure. Heart. 2008;94:1189–1193. doi: 10.1136/hrt.2006.114660. [DOI] [PubMed] [Google Scholar]
- 26.Yong G, Khairy P, De Guise P, Dore A, Marcotte F, Mercier LA, Noble S, Ibrahim R. Pulmonary arterial hypertension in patients with transcatheter closure of secundum atrial septal defects: a longitudinal study. Circ Cardiovasc Interv. 2009;2:455–462. doi: 10.1161/CIRCINTERVENTIONS.108.826560. [DOI] [PubMed] [Google Scholar]
- 27.Jateganokar S, Scholtz W, Schmidt H, Horstkotte D. Percutanous closure of atrial septal defects: echocardiographic and functional results in patients older than 60 years. Circ Cardiovasc Interv. 2009;2:85–89. doi: 10.1161/CIRCINTERVENTIONS.108.814046. [DOI] [PubMed] [Google Scholar]
- 28.Jategaonkar S, Scholtz W, Schmidt H, Fassbender D, Horstkotte D. Cardiac remodeling and effects on exercise capacity after interventional closure of atrial septal defects in different adult age groups. Clin Res Cardiol. 2010;99:183–191. doi: 10.1007/s00392-009-0105-2. [DOI] [PubMed] [Google Scholar]
- 29.Giardini A, Donti A, Specchia S, Formigari R, Oppido G, Picchio FM. Long-term impact of transcatheter atrial septal defect closure in adults on cardiac function and exercise capacity. Int J Cardiol. 2008;124:179–182. doi: 10.1016/j.ijcard.2006.12.031. [DOI] [PubMed] [Google Scholar]
- 30.Silversides CK, Haberer K, Siu SC, Webb GD, Benson LN, McLaughlin PR, Harris L. Predictors of atrial arrythmias after device closure of secundum type atrial septal defects in adults. Am J Cardiol. 2008;101:683–687. doi: 10.1016/j.amjcard.2007.10.035. [DOI] [PubMed] [Google Scholar]
- 31.Giardini A, Donti A, Sciarra F, Bronzetti G, Mariucci E, Picchio FM. Long-term incidence of atrial fibrillation and flutter after transcatheter atrial septal closure in adults. Int J of Cardiol. 2009;134:47–51. doi: 10.1016/j.ijcard.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Amin Z, Hijazi ZM, Bass JL, Cheatham JP, Hellenbrand WE, Kleinman CS. Erosion of Amplatzer septal occluder device after closure of secundum atrial septal defects: review of registry of complications and recommendations to minimize future risk. Catheter Cardiovasc Interv. 2004;63:496–502. doi: 10.1002/ccd.20211. [DOI] [PubMed] [Google Scholar]
- 33.Amin Z. Transcatheter closure of secundum atrial septal defects. Catheter Cardiovasc Interv. 2006;68:778–787. doi: 10.1002/ccd.20872. [DOI] [PubMed] [Google Scholar]
- 34.Hijazi ZM, Bass JL, Cheatham JP, Hellenbrand W, Kleinman CS. PFO closure complications from the AGA registry. Catheter Cardiovasc Interv. 2008;72:74–79. doi: 10.1002/ccd.21582. [DOI] [PubMed] [Google Scholar]
- 35.Oliver JM, Gallego P, Gonzalez A, Benito F, Mesa JM, Sobrino JA. Predisposing conditions for atrial fibrillation in atrial septal defect with and without operative closure. Am J Cardiol. 2002;89:39–43. doi: 10.1016/s0002-9149(01)02160-9. [DOI] [PubMed] [Google Scholar]
- 36.Schubert S, Peters B, Abdul-Khalig H, Nagdyman N, Lange PE, Ewert P. Left ventricular conditioning in the elderly patient to prevent congestive heart failure after transcatheter closure of atrial septal defect. Catheter Cardiovasc Interv. 2005;64:333–337. doi: 10.1002/ccd.20292. [DOI] [PubMed] [Google Scholar]
- 37.Krumsdorf U, Ostermayer S, Billinger K, Trepels T, Zadan E, Horvath K, Sievert H. Incidence and clinical course of thrombus formation on atrial septal defect and patent formaen ovale closure devices in 1,000 consecutive patients. J Am Coll Cardiol. 2004;43:302–309. doi: 10.1016/j.jacc.2003.10.030. [DOI] [PubMed] [Google Scholar]