Abstract
Context
California is the first and only state to implement a patient-to-nurse ratio mandate for hospitals. Increasing nurse staffing is an important organizational intervention for improving patient outcomes. Evidence suggests that staffing improved in California hospitals after the mandate was enacted, but the outcome for hospitals bearing a disproportionate share of uncompensated care—safety-net hospitals—remains unclear. One concern was that California's mandate would burden safety-net hospitals without improving staffing or that hospitals would reduce their skill mix, that is, the proportion of registered nurses of all nursing staff. We examined the differential effect of California's staffing mandate on safety-net and non-safety-net hospitals.
Methods
We used a time-series design with Annual Hospital Disclosure data files from the California Office of Statewide Health Planning and Development (OSHPD) for the years 1998 to 2007 to assess differences in the effect of California's mandate on staffing outcomes in safety-net and non-safety-net hospitals.
Findings
The mandate resulted in significant staffing improvements, on average nearly a full patient per nurse fewer (−0.98) for all California hospitals. The greatest effect was in those hospitals with the lowest staffing levels at the outset, both safety-net and non-safety-net hospitals, as the legislation intended. The mandate led to significantly improved staffing levels for safety-net hospitals, although there was a small but significant difference in the effect on staffing levels of safety-net and non-safety-net hospitals. Regarding skill mix, a marginally higher proportion of registered nurses was seen in non-safety-net hospitals following the mandate, while the skill mix remained essentially unchanged for safety-net hospitals. The difference between the two groups of hospitals was not significant.
Conclusions
California's mandate improved staffing for all hospitals, including safety-net hospitals. Furthermore, improvement did not come at the cost of a reduced skill mix, as was feared. Alternative and more targeted designs, however, might yield further improvement for safety-net hospitals and reduce potential disparities in the staffing and skill mix of safety-net and non-safety-net hospitals.
Keywords: Safety net, nursing, nurse staffing, California, mandate
Safety-net hospitals have historically served as important health service resources for the vulnerable poor and for increasing numbers of minority and uninsured individuals (Lewin and Altman 2000). Although the sweeping reforms brought by the Patient Protection and Affordable Care Act of 2010 promise increased health care access to vast numbers of the previously uninsured, safety-net facilities will continue to provide vital health care services to the more than 20 million U.S. residents who still will not have health insurance (Hall 2011). Yet, safety-net hospitals are increasingly susceptible to challenging economic environments. This has raised concerns about the extent to which safety-net hospitals will be able to respond to economic and policy challenges and to benefit from initiatives aimed at improving the quality and safety of care (Zwanziger and Khan 2006).
A number of states have considered regulating aspects of nursing as a means of improving health care quality. California was an early adopter of minimum hospital nurse staffing legislation and remains the only state with a comprehensive patient-to-nurse ratio mandate. This mandate was signed into law as Assembly Bill 394 (AB 394) in 1999 and took effect in 2004. Results from early studies of the consequences of California's nurse staffing mandate are mixed (Aiken et al. 2010; Cook et al. 2010; Donaldson and Shapiro 2010; Hickey et al. 2011), and little is known about how this legislation affected safety-net facilities in the state. The purpose of this article is to examine how California's safety-net hospitals responded to the nurse staffing mandate relative to other hospitals in the state.
Our examination of the nation's first comprehensive, fixed minimum nurse staffing mandate may be particularly instructive because it directly addresses the promises and limits of policies aimed at improving health care quality across a variety of health care settings and providers. Mandating nursing resources is controversial and poses a set of challenging questions. We ask whether there were differences in how safety-net and other hospitals responded to the implementation of AB 394 in terms of staffing and skill mix (i.e., the proportion of registered nurses in all nursing staff).
We begin with an overview of California's nurse staffing mandate and background on the efforts that led to its implementation. Next, we discuss the factors affecting safety-net hospitals during the period leading up to the implementation of AB 394. This is followed by an assessment of how California's nurse staffing mandate differentially affected safety-net hospitals in the state. We conclude with research and policy implications learned from the California experience.
Synopsis of AB 394
California's staffing mandate extended preexisting regulations of critical care nurse staffing enacted in the late 1970s (Spetz et al. 2000). The California legislature passed AB 394 after years of intensive lobbying by nursing unions, including the California Nurses Association and the Service Employees International Union. To further their objective, these groups also capitalized on concerns about patients’ safety and the emerging evidence of a relationship between increased nurse staffing and better patient outcomes (Blegen, Goode, and Reed 1998; Flood and Diers 1988; Kovner and Gergen 1998). After the law passed in 1999, the California Department of Health Services spent two years evaluating alternative recommendations from interested groups, including the unions and the California Healthcare Association, which represented the hospitals. The California Department of Health Services then released draft regulations in January 2002. Following an extensive public comment period, the final revisions established licensed patient-to-nurse ratios in acute care hospitals, acute psychiatric hospitals, and specialty hospitals as of January 2004 (Spetz 2004). The legislation focused on licensed nurses, including both registered nurses and licensed vocational nurses (sometimes called licensed practical nurses). The regulations specified staffing ratios for different specialties; for example, minimum staffing in general medical and surgical units were set at one licensed nurse for every six patients for an eighteen-month phase-in period and then to one nurse for every five patients. Hospitals could staff above these ratios but not below.
An additional aspect of AB 394 is that except for intensive care, nursery, emergency triage, and critical care trauma patient assignments, hospitals could be in compliance with the mandate if up to 50 percent of their required licensed nursing staff were licensed vocational nurses. Licensed vocational nurses have less training, a more restricted scope of practice, and are generally paid less than registered nurses (Seago et al. 2004). Since the 1980s, hospitals have utilized a declining number of licensed vocational nurses, opting to meet the growing demand in patient acuity and complexity of care with a higher proportion of registered nurses (Seago et al. 2004). One concern was that the provision in AB 394 allowing licensed vocational nurses to make up 50 percent of the staffing complement would lead some hospitals, particularly those with smaller budgets, to rely more heavily on licensed vocational nurses. This in turn would dilute the skill mix (Buerhaus 1997; Coffman, Seago, and Spetz 2002).
No definitive study has yet identified specific, optimal patient-to-nurse ratios. Research on the relationship between nurse staffing and patient outcomes, along with input from stakeholders, helped inform the final ratios adopted by the California Department of Health Services (California Department of Public Health 2003). Researchers from the University of California at Davis and the University of California at San Francisco estimated the distribution of nurse staffing in California hospitals, the share of hospitals that the minimum staffing requirements likely would affect, as well as the expected costs of the legislation (Kravitz and Sauve 2002; Spetz 2004; Spetz et al. 2000). Before the implementation of AB 394, between 20 and 51 percent of hospitals were projected to be required to hire additional nurses in order to comply with the staffing ratios on medical-surgical units. Experts anticipated statewide labor demands to increase by more than 7,000 licensed nurses. The expected cost per hospital to comply with the mandate was between $700,000 and $800,000.
Cross-sectional work has shown that many patient outcomes are better when hospitals have more nursing staff (Aiken et al. 2002; Kane et al. 2007; Needleman et al. 2002). Since California implemented its staffing mandate, a few studies have more directly evaluated the impact of AB 394 and suggest that California's staffing mandate has resulted in improved licensed nurse staffing (Donaldson and Shapiro 2010; McHugh et al. 2011). For example, California hospitals had better staffing and related patient outcomes compared with those hospitals in states without a similar staffing law (Aiken et al. 2010). Although longitudinal increases in nurse staffing are associated with better patient outcomes, the findings in California, both before the legislation and covering the pre- and postlegislation period, are mixed (Burnes Bolton et al. 2007; Cook et al. 2010; Donaldson and Shapiro 2010; Harless and Mark 2010; Hickey et al. 2011; Sochalski et al. 2008).
The benefits of better nurse staffing may be less likely to translate into better patient outcomes in safety-net hospitals compared with those in non-safety-net hospitals (Blegen et al. 2011). The reasons cited include higher patient acuity, poorer quality of care in nonnursing domains, and the use of less effective staffing strategies to maintain staffing (e.g., more contract nurses and more overtime) in safety-net hospitals. Despite other states’ interest in nurse staffing mandates (American Nurses Association 2011), little longitudinal research has focused on the differential effects of California's nurse staffing mandate for those hospitals that, because of fiscal constraints, may be less able to invest in additional licensed nursing personnel. To date, only one study has considered how staffing varied in safety-net and non-safety-net hospitals in California (Conway et al. 2008). Furthermore, the data for that study extended only through 2004, the year of AB 394's implementation. We fill this gap by using data before and after implementation to assess how safety-net and other hospitals responded to the mandate.
The Safety Net
The Institute of Medicine defines safety-net hospitals as having two distinguishing characteristics: “(1) by legal mandate or explicitly adopted mission they maintain an ‘open door,’ offering access to services for patients regardless of their ability to pay; and (2) a substantial share of their patient mix is uninsured, Medicaid, and other vulnerable patients” (Lewin and Altman 2000, 21).
Despite the critical function performed by safety-net hospitals over the past century, their capacity to provide needed services has been hampered in recent decades. Safety-net hospitals are especially vulnerable to varying market and policy forces and continue to struggle to operate and succeed in increasingly competitive and technologically sophisticated environments (Fishman and Bentley 1997; Lewin and Baxter 2007).
During the late 1990s, state, local, and federal efforts to decrease spending and meet increasing budgetary constraints targeted public subsidies such as disproportionate share hospital payments, which is one of safety-net hospitals’ primary means of covering unpaid costs (Fishman and Bentley 1997). The Balanced Budget Act of 1997 proposed cuts to hospital Medicare and Medicaid payments, and even though revisions in 1999 and 2000 lessened the impact of the proposed cuts, total Medicare margins declined from 10.3 percent in 1996 to 1.7 percent in 2002 (Bazzoli et al. 2005). Private-sector payment-to-cost ratios fell to roughly 115 percent in the early 2000s from a high of approximately 130 percent in the early 1990s (Bazzoli et al. 2005) while at the same time Medicaid's managed care programs grew (Marquis, Rogowski, and Escarce 2004). With this increase in Medicaid's managed care penetration, non-safety-net hospitals began competing for lower-risk Medicaid patients (e.g., uncomplicated maternity cases). This left safety-net facilities with a greater burden to care for less profitable, higher-risk Medicaid patients (Gaskin, Hadley, and Freeman 2001). Despite dramatically decreasing the number of uninsured, the Patient Protection and Affordable Care Act of 2010 will substantially reduce each state's disproportionate share hospital allotment beginning in fiscal year (FY) 2014 and each subsequent year. The ramifications for safety-net hospitals—a critical source of health care for many people in the United States—remains to be seen.
One of the challenges for studies of safety-net hospitals is that there is no consensus on how best to define them. In their review, Zwanziger and Khan (2008) suggest using a continuous measure to define safety-net hospitals, based on serving a low socioeconomic status population, providing uncompensated care, and having a high proportion of Medicaid patients. In their 1999 and 2001 studies, Gaskin and colleagues (Gaskin and Hadley 1999; Gaskin, Hadley, and Freeman 2001) identified urban safety-net hospitals as those institutions belonging to the National Association of Public Hospitals or having a proportion of discharges of low-income patients that is more than one standard deviation above the average proportion for all urban short-term general hospitals in the state. Low-income patients were defined as those whose source of income was Medicaid, charity care, or self-pay. Werner, Goldman, and Dudley (2008) designated safety-net status based on the percentage of Medicaid patients served. Safety-net status has also been defined in terms of the proportion of uncompensated care costs (Bazzoli et al. 2005; Zuckerman et al. 2001). McHugh, Kang, and Hasnain-Wynia (2009) examined the criterion used in safety-net studies between 1996 and 2008 and found variations in definitions ranging from market and facility characteristics to uncompensated care burden and total Medicaid caseload. In this article, we characterize safety-net hospitals based on common definitions consistent with the Institute of Medicine's conceptualization, as those hospitals with a burden of uncompensated care as well as public hospitals with large charity and indigent care patient populations (Bazzoli et al. 2005; Lindrooth et al. 2006; McHugh, Kang, and Hasnain-Wynia 2009; Zuckerman et al. 2001).
Study Data and Methods
Design
We used a time-series design to compare the effects of AB 394 on nurse staffing and skill mix in safety-net hospitals and non-safety-net hospitals in California from 1998 to 2007.
Data Sources and Variables
We obtained our primary data from the Annual Hospital Disclosure data files from the California Office of Statewide Health Planning and Development (OSHPD) for the years 1998 to 2007. The OSHPD data provide information on all California hospitals, including detailed staffing information and hospital characteristics. We also used data from the U.S. Bureau of Labor Statistics and the Centers for Medicare and Medicaid Services (CMS).
Outcomes
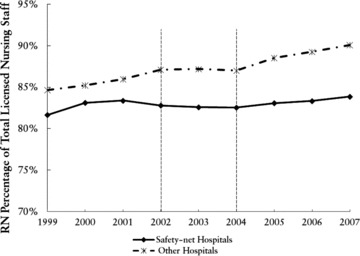
The primary outcomes that we analyzed were nurse staffing and skill mix. Our measure of nurse staffing was the number of inpatient medical-surgical patients per licensed nurse. We obtained this measure from the OSHPD hospital files, which supply detailed information on licensed nurses’ (both registered nurses and licensed vocational nurses) hours and patient days across revenue centers, including medical-surgical units. We then converted nurse hours per patient day to patients per nurse using the following formula:
 |
This approach makes our staffing measure consistent with the legislation of interest (Spetz et al. 2008; Unruh, Fottler, and Talbott 2003). We used medical-surgical staffing because this represents the majority of hospital nurse staffing and allowed us to use a staffing measure that could be readily and directly evaluated with respect to the requirements of California's mandate. To calculate the skill mix in each hospital, we divided registered nurses’ hours by total licensed nursing staff (the sum of registered nurses plus licensed vocational nurses) hours.
Safety-Net Status
Our analysis included all adult, nonfederal acute care facilities in the state of California from 1998 to 2007. We identified safety-net hospitals based on each hospital's average burden of uncompensated care in the years before the mandate was implemented in 2004 (Bazzoli et al. 2005, 2006; Fishman and Bentley 1997; Lindrooth et al. 2006; McHugh, Kang, and Hasnain-Wynia 2009; Zuckerman et al. 2001). To calculate a hospital's total uncompensated care, we added bad debt and charity care, adjusting this sum by the hospital's cost-to-charge ratio. Those hospitals in the top decile, based on the ratio of uncompensated care to total expenses, were considered to be “high-burden” hospitals, or safety-net hospitals, as we use the term here.
We also counted public city and county hospitals—significant providers of care to the vulnerable poor—as safety-net hospitals (Kelch 2011). Under Section 17000 of California's Welfare and Institutions Code, counties are responsible for the care of low-income uninsured residents who have no other source of care. Although our definition of safety-net hospitals based on uncompensated care burden included all city and most county hospitals in our sample, a few county hospitals had a notably low uncompensated care burden. Some county hospitals in California classify uncompensated care on the financial reports to their county indigent program. To account for this, we also classified those county hospitals with very low uncompensated care (bottom decile) as safety-net hospitals if their indigent care burden ranked very high (top decile).
Covariates
Although our fixed-effects modeling approach controls for all time-invariant characteristics of the hospitals in our panel, there are other factors that could be jointly related to staffing and to being a safety-net hospital that are not stable over time. For this reason, we included a number of covariates from the OSHPD data to control for potential confounds. Number of beds was defined as the number of hospital beds staffed within the facility. We also classified hospitals with respect to the amount of technology they possessed; for example, “high-technology” facilities were identified as those that had open-heart surgery capabilities, organ transplant capabilities, or both (Aiken et al. 2002).
We also included covariates to account for variations in hospitals’ financial conditions that could confound our understanding of the effect of the mandate on staffing in safety-net compared with non-safety-net hospitals (Zwanziger, Khan, and Bamezai 2010). The first covariate was net patient revenue per patient day (Bazzoli et al. 2007). In addition, we had an indicator of the hospital's liquidity: the amount of cash on hand as a percentage of total revenue. We used the Herfindahl-Hirschman index (HHI) as a proxy measure for market competition and calculated it as the sum of the squared market shares of the competing hospital area (Hsieh, Clement, and Bazzoli 2010). Markets were designated as the hospital service area defined in the Dartmouth Atlas, and market share data were drawn from the CMS Hospital Services Area Files for each year (Wennberg and Cooper 1998). We also used an annual measure of the Medicare area wage index from the CMS to account for geographic labor input price differences. To account for variability in the economy and nurse supply (Blegen, Vaughn, and Vojir 2008), we estimated a county-level annual unemployment rate as the percentage of people who were jobless, looking for jobs, or available for work, using annual data from the U.S. Bureau of Labor Statistics, Local Area Unemployment Statistics program (U.S. Department of Labor 2010).
We also established controls for differences in patient mix. The annual hospital-level Medicare case-mix index was drawn from the CMS to account for the severity of illness in each hospital's patient population. Finally, we used variables indicating the share of Medicare and Medicaid inpatient days out of all inpatient days (Hsieh, Clement, and Bazzoli 2010).
Analytic Approach
We constructed a balanced longitudinal data set for the time period 1998 to 2007 for our analyses, accounting for hospital consolidations and mergers by combining data before the mergers and dropping those hospitals that closed during the observation interval.
We created a series of dummy variables and interactions to evaluate the effect of the mandate on staffing and skill mix and the difference in this effect by safety-net status. One dummy variable distinguished between the period before 2004 (when the ratios went into effect) and the period after 2004. We refer to these intervals as the preimplementation and postimplementation periods, respectively. Another dummy variable contrasted safety-net hospitals with non-safety-net hospitals.
We labeled those hospitals with patient-to-nurse ratios at or below that required by the mandate (less than or equal to 5:1) before the ratios were released in 2002 as compliant and those hospitals with patient-to-nurse ratios exceeding 5:1 as noncompliant. Because some hospitals—as many as half, by some estimates—were already in compliance with the mandated staffing levels, we expected that the legislation would have a limited effect on those hospitals and would result in little or no change in staffing. Hospitals with patient-to-nurse ratios that exceeded the mandated level before the release of the final ratios would be expected to change and to change the most for those hospitals furthest from the mandated level initially.
With this in mind, we contrasted the change in staffing in safety-net and non-safety-net hospitals as a result of the legislation while taking account of where each type of hospital stood before the legislation in regard to its staffing relative to the mandated levels. We assigned a score to each of the noncompliant hospitals to indicate the number of patients per medical-surgical nurse by which these hospitals, before the final ratios were released, exceeded the mandated level of five patients per nurse. Those hospitals with a patient-to-nurse ratio exceeding the mandated level took the value of the difference between their average patient-to-nurse ratio in the pre-ratio period and five (the final mandate limit). This is a continuous value. We considered those hospitals with an average of five or fewer patients per nurse before the ratios to be compliant and assigned them a value of zero; that is, their patient-to-nurse ratio did not exceed the mandated level. The regulatory intent of the mandate supports comparing hospitals based on this distinction. Indeed, the California Department of Health Services’ Final Statement of Reasons notes that its “policy decisions remediate the hospitals with the leanest staffing, effectively raising the bar for the standard of acceptable staffing” (California Department of Public Health 2003).
We used hospital-level fixed-effects regression models to estimate the effect of AB 394 on California safety-net hospitals compared with non-safety-net hospitals. The fixed-effects approach ensures that the estimated effects of the ratios cannot be attributed to unmeasured time-invariant differences between hospitals in different markets that may be associated with staffing and skill mix over time. We also included time fixed-effects (a dummy variable for the time period, preimplementation versus postimplementation) to control for secular changes that might influence the availability and use of licensed nurses and intertemporal trends common to all hospitals in California. To evaluate the effect of AB 394 on safety-net versus non-safety-net hospitals, we tested the interactions between the time period and safety-net status in which the effects of the mandate were determined by evaluating the sign, size, and significance of the coefficient for the interaction terms. We included an interaction term of the time period variable, and our variable indicating the number of patients per nurse by which noncompliant hospitals initially exceeded the mandated level. This allowed the change over time to differ depending on the initial “degree” of noncompliance. We also assessed an alternative model to determine whether the change in staffing based on initial level of noncompliance was different for safety-net and non-safety-net hospitals. This model included a three-way interaction term of our time period variable, our safety-net indicator, and the variable indicating the initial degree of noncompliance.
Study Results
Our panel contained 173 California hospitals, of which 28 (16%) met our criteria for safety-net hospital (see table 1). On average, the safety-net hospitals had more beds and were more likely to be teaching institutions. All the city or county hospitals in our sample were considered to be safety-net hospitals. Table 1 gives additional descriptive information about the hospitals by safety-net status.
TABLE 1.
Summary Statistics of Hospitals, 1998–2007
| All Hospitals | Compliant | Noncompliant | ||||
|---|---|---|---|---|---|---|
| Safety Net | Non-safety Net | Safety Net | Non-safety Net | Safety Net | Non-safety Net | |
| Hospital beds | 261 (148) | 240 (144) | 283 (134) | 254 (171) | 248 (154) | 228.93 (114.02) |
| Resident physician/bed ratio | 0.21 (0.30) | 0.04 (0.15) | 0.15 (0.17) | 0.08 (0.20) | 0.24 (0.35) | 0.01 (0.04) |
| Case mix index | 1.39 (0.20) | 1.45 (0.22) | 1.40 (0.21) | 1.47 (0.24) | 1.39 (0.19) | 1.44 (0.21) |
| Medicare share | 0.31 (0.16) | 0.44 (0.12) | 0.34 (0.16) | 0.44 (0.13) | 0.30 (0.16) | 0.44 (0.121) |
| Medicaid share | 0.28 (0.12) | 0.14 (0.13) | 0.27 (0.13) | 0.14 (0.13) | 0.28 (0.12) | 0.15 (0.12) |
| Net revenue/patient day | 2493 (960) | 2345 (1156) | 2403 (1140) | 2640 (1359) | 2551 (821) | 2092 (873) |
| Cash on hand/revenue ratio | 0.04 (0.09) | 0.05 (0.14) | 0.04 (0.11) | 0.06 (0.12) | 0.04 (0.07) | 0.05 (0.16) |
| Area wage index | 1.22 (0.16) | 1.20 (0.14) | 1.32 (0.16) | 1.22 (0.15) | 1.15 (0.12) | 1.18 (0.12) |
| Unemployment rate (%) | 6.15 (2.90) | 5.86 (2.06) | 4.91 (1.31) | 5.84 (2.09) | 6.90 (3.32) | 5.88 (2.04) |
| HHI | 781 (489) | 835 (480) | 914 (510) | 950 (464) | 701(460) | 737 (472) |
| High technology, n(%) | 130 (46%) | 920 (63%) | 50 (45%) | 430 (64%) | 80 (47%) | 490 (63%) |
| Ownership | ||||||
| City or county, n(%) | 130 (46%) | 0 (0.00) | 40 (36%) | 0 (0%) | 90 (53%) | 0 (0%) |
| District hospital,n(%) | 10 (4%) | 190 (13%) | 0 (0%) | 100 (15%) | 10 (6%) | 90 (12%) |
| For-profit, n(%) | 90 (32%) | 300 (21%) | 30 (27%) | 90 (14%) | 60 (36%) | 210 (27%) |
| Nonprofit, n(%) | 50 (18%) | 960 (66%) | 40 (36%) | 480 (72%) | 10 (6%) | 480 (62%) |
| Number of hospitals,(%) | 28 (16%) | 145 (84%) | 11 (6%) | 67 (39%) | 17 (10%) | 78 (45%) |
Note: HHI = Herfindahl-Hirschman Index. Entries are means and, in parentheses, standard deviations unless noted otherwise.
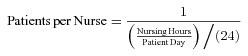
We plotted the average patient-to-nurse ratio over time to see whether there were differences between the safety-net and non-safety-net hospitals (figure 1). Safety-net and non-safety-net hospitals differed modestly in their staffing level before the legislation was passed in 1999. Nursing workload in terms of patient-to-nurse ratio decreased for both safety-net and non-safety-net hospitals, corresponding to the announcement of the final ratios by the California Department of Health Services in 2002 and continuing after the implementation in 2004.
FIGURE 1.
Trends in Medical-Surgical Nurse Staffing among Safety-net and Non-safety-net Hospitals in California, 1998–2007 Note: Final ratios were released publicly in 2002; AB 394 was implemented in 2004.
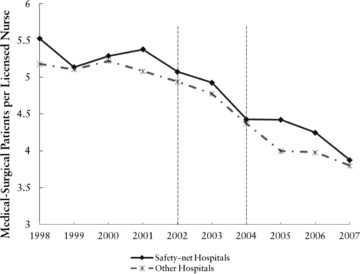
We also plotted nursing skill mix over the same period to examine differences in trends between the safety-net and non-safety-net hospitals (figure 2). Safety-net and non-safety-net hospitals had different initial levels of skill mix, with the safety-net hospitals having a significantly lower skill mix before the legislation was passed in 1999. On visual inspection and before any controls, it appears that skill mix increased for non-safety-net hospitals while remaining steady or increasing only slightly for safety-net hospitals. This contradicts concerns about skill mix reductions for safety-net hospitals. The gap between safety-net and non-safety-net hospitals, however, appears to have grown.
FIGURE 2.
Trends in Medical-Surgical Nurse Skill Mix among Safety-net and Non-safety-net Hospitals in California, 1998–2007 Note: Final ratios were released publicly in 2002; AB 394 was implemented in 2004. RN = registered nurse, LVN = Licensed Vocational Nurse, Total Licensed Nursing Staff =[RNs/(RNs + LVNs)].
When the California Department of Health Services released the final ratios in 2002, 45 percent of all the hospitals in our sample (39% of the safety-net and 46% of the non-safety-net hospitals) were staffed at a level that would have put them in compliance with the law (see table 2). The difference between safety-net and non-safety-net hospitals was not statistically significant (p= 0.50). In the period following the 2004 implementation of the mandate, 82 percent of safety-net hospitals and 92 percent of non-safety-net hospitals were staffed at a level consistent with compliance. The difference in the proportion of compliant safety-net hospitals versus compliant non-safety-net hospitals following implementation was not statistically significant (p= 0.09). Although a higher percentage of initially noncompliant non-safety-net hospitals became compliant (88%), compared with initially noncompliant safety-net hospitals (76%), the difference was not statistically significant. The average reduction in patient-to-nurse ratio was statistically significant across each group of hospitals (p < 0.001 for all groups except compliant safety-net hospitals, p= 0.03 for this group).
TABLE 2.
Medical-Surgical Patient-to-Nurse Ratio and Compliance Status in the Preimplementation and Postimplementation Periods
| Preimplementation | Postimplementation | |||||
|---|---|---|---|---|---|---|
| Number of Hospitals (%) | Patient-to-Nurse Ratio (SD) | Number of Hospitals (%) | Patient-to-Nurse Ratio (SD) | |||
| Non-safety Net | 145 (84%) | 5.15 (1.03) | 3.93 (0.71) | |||
| Compliant | 67 (46%) | 4.30 (0.51) | { | Compliant | 65 (97%) | 3.59 (0.54) |
| Noncompliant | 2 (3%) | 5.07 (0.03) | ||||
| Noncompliant | 78 (54%) | 5.89 (0.76) | { | Compliant | 69 (88%) | 3.99 (0.47) |
| Noncompliant | 9 (12%) | 5.56 (0.79) | ||||
| Safety Net | 28 (16) | 5.33 (1.42) | 4.18 (1.24) | |||
| Compliant | 11 (39%) | 4.15 (0.74) | { | Compliant | 10 (91%) | 3.33 (0.46) |
| Noncompliant | 1 (9%) | 5.60 (–) | ||||
| Noncompliant | 17 (61%) | 6.10 (1.22) | { | Compliant | 13 (76%) | 4.08 (0.55) |
| Noncompliant | 4 (24%) | 6.28 (1.57) | ||||
Note: Percentages under the Preimplementation column are percentages for each safety-net category. The Postimplementation column shows compliance based on whether hospitals’ average staffing level was greater than 5 patients per nurse (noncompliant) or 5 patients or fewer per nurse after 2004. The percentages under Postimplementation then represent the postimplementation status row percentage based on each safety net's X initial compliance combination.
The fixed effects regression models estimate the effects of the legislation on staffing and skill mix for both safety-net and non-safety-net hospitals. We also included a term to indicate the degree to which each noncompliant hospital initially exceeded the mandated patient-to-nurse ratio, that is, the difference between the hospital's initial patient-to-nurse ratio and the 5:1 patient-to-nurse ratio required by law after 2004. We specified our primary model identifying two time periods: preimplementation, representing the events before the mandate was enforced in 2004, and postimplementation, representing the period following 2004. A model specification with three time intervals (preannouncement, announcement, and postimplementation) demonstrated no significant effects from any announcement, suggesting that the announcement of the ratios in 2002 did not result in meaningful changes in staffing before the legislation's implementation in 2004.
We found that the overall effect of implementation of the mandate across all hospitals resulted in nearly one fewer patient per nurse (−0.98 [p < 0.001]). We found significant differences in the effect on staffing based on safety-net status as well as the degree of initial noncompliance (see table 3). For initially compliant non-safety-net hospitals, the mandate had the effect of reducing patient-to-nurse ratios by 0.72 patients per nurse. The effect was smaller for initially compliant safety-net hospitals (a reduction of 0.46 patients per nurse). Although patient-to-nurse ratios fell in both safety-net and non-safety-net hospitals after the mandate, we found a statistically significant disparity in the magnitude of the change between safety-net and non-safety-net hospitals (0.27 patients per nurse, p= 0.02).
TABLE 3.
Effects of Implementation of California Staffing Mandate (AB 394) on Medical-Surgical Nurse Staffing and Skill Mix, 1998–2007
| Patient-to-Nurse Ratio | Skill Mix | |
|---|---|---|
| Postimplementation | −0.72*** (0.06) | .03*** (.004) |
| Safety Net (Postimplementation × safety net) | 0.27* (0.12) | −.02 (.009) |
| Degree of Initial Noncompliance (Postimplementation ×# of patients over mandate) | −0.62*** (0.05) | −.003 (.004) |
Note: Point estimates and standard errors from fixed-effects regression models estimating the effects of AB 394 on medical-surgical patient-to-licensed nurse ratio for hospitals are based on safety net and compliance status; standard errors are in parentheses. Covariates include number of beds, net patient revenue per patient day, cash/revenue ratio, area wage index, case mix index, ranking on high technology index, Medicare share, Medicaid share, Herfindahl-Hirschman index, and local unemployment rate.
The greatest reductions in patient-to-nurse ratio following the implementation of the California mandate were for those hospitals that were initially understaffed to begin with—both safety net and non-safety net. For every additional patient per nurse above the 5:1 ratio in the preimplementation period, hospitals had an additional reduction of 0.62 patients per nurse. An alternative model to determine whether the change in staffing based on initial level of noncompliance was significantly different for safety-net and non-safety-net hospitals showed that the difference was not significant (0.14 patients per nurse, p= 0.2). Thus, our estimate of the effect of the degree of initial noncompliance is effectively an average of both safety-net and non-safety-net hospitals. Figure 3 shows the estimated changes in patient-to-nurse ratio following implementation for safety-net and non-safety-net hospitals based on their initial staffing levels.
FIGURE 3.
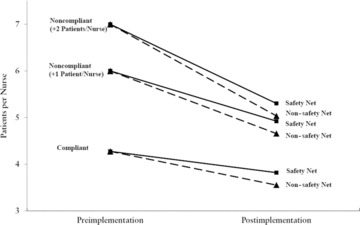
Medical-Surgical Patient-to-Nurse Ratios before and after Reform in Safety-net and Non-safety-net Hospitals by Initial Staffing Level Note: Preimplementation patient per nurse ratios for compliant safety-net and non-safety-net hospitals are based on the estimated (and equal) mean values for those hospitals.
The skill mix in all hospitals rose from the preimplementation period to the postimplementation period by a small but statistically significant amount (0.02 [p < 0.001]). The effect was significant and greatest for those non-safety-net hospitals (0.03 [p < 0.001]) that were initially adequately staffed at a level in compliance with the mandate. There was not a significant effect for safety-net hospitals (0.01 [p= 0.3]). The difference in the effect of implementation on skill mix for safety-net and non-safety-net hospitals was not statistically significant (-0.02 [p= 0.06]). There was no effect on skill mix based on the degree to which hospitals initially needed to increase their staffing in order to be in compliance.
Discussion
Our findings suggest that AB 394 met the goal of increasing nurse staffing in both safety-net and non-safety-net California hospitals. The level of improvement is clinically significant at nearly a full patient per nurse fewer on average (Aiken et al. 2002). That staffing improved significantly in safety-net hospitals is an important policy achievement, as raising nurse staffing levels in these hospitals has long been considered a difficult challenge.
It is notable, however, that the gains for safety-net and non-safety-net hospitals were not equal. Our results show a small but significant difference of up to 0.27 additional patients per nurse in safety-net hospitals compared with non-safety-net hospitals after the implementation of AB 394. A lower percentage of the initially noncompliant safety-net hospitals had average postimplementation staffing levels consistent with compliance (76%), compared with those of similar non-safety-net hospitals (88%).
Despite early concerns, we observed no reductions in skill mix. The skill mix in safety-net hospitals was steady over time, whereas the skill mix in non-safety-net hospitals increased slightly. There was, however, no significant difference based on a hospital's safety-net status or the degree to which noncompliant hospitals (safety net or otherwise) exceeded the mandate.
Several factors put our findings in context. During the initial period of this study and the years preceding it, California was experiencing a severe nursing shortage. This shortage affected all hospitals, although safety-net facilities had more difficulty retaining high-quality health professionals, including nurses, than other hospitals did (Harrison and Montalvo 2002; Lewin and Baxter 2007). This may account for some of the differences in staffing and skill mix of safety-net and non-safety-net hospitals at the beginning of our time-series.
Research of the effect of AB 394 shows that registered nurses’ wages rose after implementation, indicating that the policy may have influenced market forces, shifting the supply of registered nursing staff to hospitals able to pay higher wages (Mark, Harless, and Spetz 2009). This may explain some of the staffing and skill mix differences of safety-net and non-safety-net hospitals. If, for instance, registered nurses working in safety-net hospitals took newly opened positions in non-safety-net hospitals for better pay and more benefits while at the same time safety-net hospitals increasingly relied on licensed vocational nurses to maintain staffing compliance, differences in safety-net and non-safety-net hospitals’ skill mix would be a result of the policy (Spetz 2004).
Ultimately, however, the intended goal of the legislation to increase nurse staffing was achieved in those hospitals in which an improvement in staffing has historically been most difficult and most improvement was needed. Our findings have implications for policymakers in other states considering similar patient-to-nurse staffing ratio mandates. The large majority of poor and minority patients tend to receive their hospital care in a disproportionately small number of safety-net hospitals. As others have shown (Jha, Orav, and Epstein 2008; Jha et al. 2007) and as we have seen in our data, nurse staffing tends to be worse in these hospitals. In terms of staffing, California's mandate was successful, improving staffing for the safety-net hospitals serving California's more vulnerable patients and also improving staffing for the population in general.
Our findings suggest that the gains in staffing among safety-net hospitals and non-safety-net hospitals did not come at the cost of reduced skill mix in safety-net hospitals, as was once feared. The skill mix in safety-net hospitals did not change after AB 394 was implemented. Disparities in the overall skill mix of safety-net hospitals and non-safety-net hospitals continued, however, after the nurse staffing legislation was implemented. Some research indicates that these lower levels of skill may be associated with poor patient outcomes (Estabrooks et al. 2005; Seago, Williamson, and Atwood 2006; Tourangeau et al. 2002). Future studies must determine whether the absolute staffing improvement in safety-net hospitals is more important to improved patient outcomes than the continuing differences in the skill mix of safety-net and non-safety-net hospitals.
Our findings should be interpreted with some caution. We do not mean to discount the improvements of the safety-net hospitals identified in our study, which should translate into benefits to many vulnerable patients through improvements in nursing resources. Our results do suggest, however, that while the broad mandate approach taken by California was a successful policy design for increasing staffing generally, other states may also want to consider more targeted policies to improve staffing in safety-net hospitals specifically (Ingram and Schneider 1991). This could have the effect of not only increasing staffing for all institutions but also reducing those differences in safety-net and non-safety-net hospitals that may contribute to disparities in patient outcomes.
All hospitals, with some exceptions and a waiver provision for a restricted set of small hospitals, were subject to the California mandate, regardless of whether they were adequately staffed. An alternative policy design targeting those hospitals most in need of more nurses might offer a more efficient approach while allowing better-resourced hospitals more flexibility in staffing and an opportunity to develop innovative staffing models. A targeted approach might combine a mandate with focused compliance incentives for at-risk hospitals (May 1993; Scholz 1984). The incentives could be made relevant to safety-net hospitals’ recruitment and retention needs, be used to reward hospitals’ compliance, and encourage a more even distribution of registered nurses in safety-net versus non-safety-net hospitals.
Policymakers in those states considering a mandate similar to California's might also consider pairing the mandate with initiatives to increase the pool of available registered nurses in the workforce. An example from California that may have attenuated the differences we saw was the state-funded Nurse Workforce Initiative introduced in 2004 to educate 5,000 additional nurses. It took, however, from two to four years before the effects of these programs could be seen in the higher number of newly trained nurses in the California nursing workforce (Spetz 2004). Such a program might include postgraduation “pay-back” obligations to work in safety-net hospitals.
Limitations
This study, like all others, has limitations. First, there is no consensus on the definition of a safety-net hospital. Because researchers use different definitions, the definition chosen could influence the results (McHugh, Kang, and Hasnain-Wynia 2009; Zwanziger and Khan 2008). In addition, as a group, safety-net hospitals are not homogeneous (Zwanziger and Khan 2008). Indeed, the needs, functioning, and service populations of safety-net facilities are, in many ways, specific to the community in which they are located (Taylor, Cunningham, and McKenzie 2006). For example, small safety-net hospitals in rural areas may be different from large safety-net hospitals in urban areas. Our approach encompasses multiple hospital characteristics as well as a hospital fixed effect in order to account for both measured and unmeasured heterogeneity. Further research, however, should examine differential effects within the safety-net group and focus on distinguishing highly adaptive versus less adaptive safety-net hospitals in an effort to understand the factors that help safety-net hospitals successfully weather policy shocks. Other subgroups, such as district hospitals, should be investigated in order to understand the policy's effects on these organizational forms with their particular patient populations.
We also acknowledge that although our analysis of the differential effects of AB 394 provides information about workforce trends, we were unable to determine the causal effect of the change. If similar data were available from other sources, we could compare safety-net hospitals in California with otherwise similar hospitals in other states without a staffing mandate. The OSHPD staffing data are widely considered among the best for examining staffing; however, there are some limitations. We converted nursing hours per patient day into a patient-to-nurse ratio to be consistent with the legislation, but this conversion is admittedly imprecise. Patient days may not average twenty-four hours, depending on when patients are admitted and discharged. We repeated our analysis based on evidence suggesting that hospital stays may be understated by about two hours per discharge (Unruh, Fottler, and Talbott 2003). There were no meaningful differences in the findings or conclusions that resulted from this alternative. We also note that although looking at compliance offers a useful heuristic by which to categorize hospitals, our data were not able to determine true compliance from moment to moment and to say that any one particular hospital was truly in compliance or not at a given time.
By including the covariates that indicate the hospital's financial status, we may have misspecified our model predicting staffing for the purpose of understanding the mandate. We tested the sensitivity of our model to the inclusion of these covariates by estimating models with and without these variables. The effects of the financial variables were not significant, and the models without the hospital financial status variables did not meaningfully differ from the models that did include them.
Finally, although we see that staffing has improved, further investigation must determine the impact on cost, outcomes, and cost-effectiveness for both safety-net and non-safety-net hospitals. Nursing labor constitutes a significant portion of hospital costs, and evaluations of the effect of California's policy on outcomes are limited and show mixed results (Aiken et al. 2010; Cook et al. 2010; Donaldson and Shapiro 2010; Hickey et al. 2011). Some evidence suggests that the costs of staffing increases may be partially offset by the costs of adverse events avoided as a result of those staffing improvements (McCue, Mark, and Harless 2003; Needleman et al. 2006; Rothberg et al. 2005). A larger nursing staff may also yield additional societal benefits through reduced health expenditures and greater productivity (Dall et al. 2009).
Conclusion
The Patient Protection and Affordable Care Act of 2010 will soon give health insurance coverage to more than 30 million currently uninsured people. Even so, many people—more than 20 million nationwide and more than 3 million in California alone—will remain uninsured (Long and Gruber 2011). Among them will be illegal immigrants, people choosing not to be insured despite the minimum essential coverage requirement (the so-called individual mandate) and subsidies, and people without access to affordable coverage (Marmor and Oberlander 2011). Because the health care safety net will continue to be an essential resource for this large and diverse segment of the population, legislators and administrators in a post–health reform world must consider the ramifications of policy reforms on safety-net hospitals.
The implementation of AB 394 appears thus far to be a policy success in meeting its first goal, to improve nurse staffing in California hospitals, including safety-net hospitals. The skill mix did not fall in safety-net hospitals, although differences in skill mix in both safety-net and non-safety-net facilities persist. Future studies must assess the costs associated with the legislation and examine whether these staffing differences affect patient outcomes and quality. Policymakers should note the positive overall improvements in staffing for all hospitals but should also consider the possibility of widening disparities resulting from a broad, unfocused mandate. An alternative approach might pair a mandate with financial and other support for those institutions most in need.
Acknowledgments
This research was supported by the Agency for Healthcare Research and Quality (K08-HS017551, McHugh, PI), the National Institute of Nursing Research (K01-NR012006, Brooks Carthon, PI; and R01-NR-004513, P30-NR-005043, T32-NR007104, Aiken, PI), and the Robert Wood Johnson Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the National Institute of Nursing Research, or the Robert Wood Johnson Foundation. The funding sources had no role in the study design, data collection, analysis, interpretation, or writing of this article. The authors gratefully acknowledge John Marcotte for his assistance with data analysis; Annemarie Marrou, Benjamin Hardy, and Egor Buharin for their assistance with manuscript preparation; and three anonymous reviewers for their insightful comments, which improved our manuscript.
References
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago JA, Spetz J, Smith HL. Implications of the California Nurse Staffing Mandate for Other States. Health Services Research. 2010;45(4):904–21. doi: 10.1111/j.1475-6773.2010.01114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Nurses Association. Nurse Staffing Plans and Ratios. 2011. Available at http://safestaffingsaveslives.org/WhatisANADoing/StateLegislation.aspx (accessed July 6, 2011)
- Bazzoli GJ, Clement JP, Lindrooth RC, Chen HF, Aydede SK, Braun BI, Loeb JM. Hospital Financial Condition and Operational Decisions Related to the Quality of Hospital Care. Medical Care Research and Review. 2007;64(2):148–68. doi: 10.1177/1077558706298289. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ, Kang R, Hasnain-Wynia R, Lindrooth RC. An Update on Safety-Net Hospitals: Coping with the Late 1990s and Early 2000s. Health Affairs. 2005;24(4):1047–56. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ, Lindrooth RC, Kang R, Hasnain-Wynia R. The Influence of Health Policy and Market Factors on the Hospital Safety Net. Health Services Research. 2006;41(4):1159–80. doi: 10.1111/j.1475-6773.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ, Reed L. Nurse Staffing and Patient Outcomes. Nursing Research. 1998;47(1):43–50. doi: 10.1097/00006199-199801000-00008. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ, Spetz J, Vaughn T, Park SH. Nurse Staffing Effects on Patient Outcomes: Safety-Net and Non-Safety-Net Hospitals. Medical Care. 2011;49(4):406–14. doi: 10.1097/MLR.0b013e318202e129. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Vaughn T, Vojir CP. Nurse Staffing Levels: Impact of Organizational Characteristics and Registered Nurse Supply. Health Services Research. 2008;43(1, pt. 1):154–73. doi: 10.1111/j.1475-6773.2007.00749.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buerhaus PI. What Is the Harm in Imposing Mandatory Hospital Nurse Staffing Regulations. Nursing Economics. 1997;15(2):66–72. [PubMed] [Google Scholar]
- Burnes Bolton L, Aydin CE, Donaldson N, Brown DS, Sandhu M, Fridman M, Aronow HU. Mandated Nurse Staffing Ratios in California: A Comparison of Staffing and Nursing-Sensitive Outcomes Pre- and Postregulation. Policy, Politics, & Nursing Practice. 2007;8(4):238–50. doi: 10.1177/1527154407312737. [DOI] [PubMed] [Google Scholar]
- California Department of Public Health. Final Statement of Reasons, R-37-01. 2003. Available at http://www.cdph.ca.gov/services/DPOPP/regs/Documents/R-37-01_FSOR.pdf (accessed October 25, 2011)
- Coffman JM, Seago JA, Spetz J. Minimum Nurse-to-Patient Ratios in Acute Care Hospitals in California. Health Affairs. 2002;21(5):53–64. doi: 10.1377/hlthaff.21.5.53. [DOI] [PubMed] [Google Scholar]
- Conway PH, Tamara Konetzka R, Zhu J, Volpp KG, Sochalski J. Nurse Staffing Ratios: Trends and Policy Implications for Hospitalists and the Safety Net. Journal of Hospital Medicine. 2008;3(3):193–99. doi: 10.1002/jhm.314. [DOI] [PubMed] [Google Scholar]
- Cook A, Gaynor M, Stephens M, Jr, Taylor L. The Effect of Hospital Nurse Staffing on Patient Health Outcomes: Evidence from California's Minimum Staffing Regulation. 2010. Available at http://www.nber.org/papers/w16077 (accessed October 6, 2011)
- Dall TM, Chen YJ, Seifert RF, Maddox PJ, Hogan PF. The Economic Value of Professional Nursing. Medical Care. 2009;47(1):97–104. doi: 10.1097/MLR.0b013e3181844da8. [DOI] [PubMed] [Google Scholar]
- Donaldson N, Shapiro S. Impact of California Mandated Acute Care Hospital Nurse Staffing Ratios: A Literature Synthesis. Policy, Politics, & Nursing Practice. 2010;11(3):184–201. doi: 10.1177/1527154410392240. [DOI] [PubMed] [Google Scholar]
- Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giovannetti P. The Impact of Hospital Nursing Characteristics on 30-Day Mortality. Nursing Research. 2005;54(2):74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Fishman LE, Bentley JD. The Evolution of Support for Safety-Net Hospitals. Health Affairs. 1997;16(4):30–47. doi: 10.1377/hlthaff.16.4.30. [DOI] [PubMed] [Google Scholar]
- Flood SD, Diers D. Nurse Staffing, Patient Outcome and Cost. Nursing Management. 1988;19(5):34–43. [PubMed] [Google Scholar]
- Gaskin DJ, Hadley J. Population Characteristics of Markets of Safety-Net and Non-Safety-Net Hospitals. Journal of Urban Health. 1999;76(3):351–70. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Hadley J, Freeman VG. Are Urban Safety-Net Hospitals Losing Low-Risk Medicaid Maternity Patients. Health Services Research. 2001;36(1, pt. 1):25–51. [PMC free article] [PubMed] [Google Scholar]
- Hall MA. Getting to Universal Coverage with Better Safety-Net Programs for the Uninsured. Journal of Health Politics Policy and Law. 2011;36(3):521–26. doi: 10.1215/03616878-1271198. [DOI] [PubMed] [Google Scholar]
- Harless DW, Mark BA. Nurse Staffing and Quality of Care with Direct Measurement of Inpatient Staffing. Medical Care. 2010;48(7):659–63. doi: 10.1097/MLR.0b013e3181dbe200. [DOI] [PubMed] [Google Scholar]
- Harrison M, Montalvo C. The Financial Health of California Hospitals: A Looming Crisis. Health Affairs. 2002;21(1):118–26. doi: 10.1377/hlthaff.21.1.118. [DOI] [PubMed] [Google Scholar]
- Hickey PA, Gauvreau K, Jenkins K, Fawcett J, Hayman L. Statewide and National Impact of California's Staffing Law on Pediatric Cardiac Surgery Outcomes. Journal of Nursing Administration. 2011;41(5):218–25. doi: 10.1097/NNA.0b013e3182171b2e. [DOI] [PubMed] [Google Scholar]
- Hsieh H, Clement DG, Bazzoli GJ. Impacts of Market and Organizational Characteristics on Hospital Efficiency and Uncompensated Care. Health Care Management Review. 2010;35(1):77–87. doi: 10.1097/HMR.0b013e3181c09956. [DOI] [PubMed] [Google Scholar]
- Ingram H, Schneider A. The Choice of Target Populations. Administration & Society. 1991;23(3):333–56. [Google Scholar]
- Jha AK, Orav EJ, Epstein AM. The Characteristics and Performance of Hospitals That Care for Elderly Hispanic Americans. Health Affairs (Millwood) 2008;27(2):528–37. doi: 10.1377/hlthaff.27.2.528. [DOI] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and Quality of Hospitals That Care for Elderly Black Patients. Archives of Internal Medicine. 2007;167(11):1177–82. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- Kane RL, Shamliyan T, Mueller C, Duval S, Wilt T. Nursing Staffing and Quality of Patient Care. Rockville, MD: Agency for Healthcare Research and Quality; 2007. [PMC free article] [PubMed] [Google Scholar]
- Kelch DR. The Crucial Role of Counties in the Health of Californians: An Overview. Oakland: California HealthCare Foundation; 2011. [Google Scholar]
- Kovner C, Gergen PJ. Nurse Staffing Levels and Adverse Events Following Surgery in U.S. Hospitals. Image—The Journal of Nursing Scholarship. 1998;30(4):315–21. [PubMed] [Google Scholar]
- Kravitz RL, Sauve M. Hospital Nursing Staff Ratios and Quality of Care. Davis: University of California; 2002. [Google Scholar]
- Lewin M, Altman S. America's Health Care Safety Net: Intact but Endangered. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- Lewin M, Baxter R. America's Health Care Safety Net: Revisiting the 2000 IOM Report. Health Affairs. 2007;26(5):1490. doi: 10.1377/hlthaff.26.5.1490. [DOI] [PubMed] [Google Scholar]
- Lindrooth RC, Bazzoli GJ, Needleman J, Hasnain-Wynia R. The Effect of Changes in Hospital Reimbursement on Nurse Staffing Decisions at Safety Net and Nonsafety Net Hospitals. Health Services Research. 2006;41(3, pt. 1):701–20. doi: 10.1111/j.1475-6773.2006.00514.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long P, Gruber J. Projecting the Impact of the Affordable Care Act on California. Health Affairs (Millwood) 2011;30(1):63. doi: 10.1377/hlthaff.2010.0961. [DOI] [PubMed] [Google Scholar]
- Mark B, Harless DW, Spetz J. California's Minimum-Nurse-Staffing Legislation and Nurses’ Wages. Health Affairs (Millwood) 2009;28(2):w326–34. doi: 10.1377/hlthaff.28.2.w326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmor T, Oberlander J. The Patchwork: Health Reform, American Style. Social Science & Medicine. 2011;72(2):125–28. doi: 10.1016/j.socscimed.2010.10.016. [DOI] [PubMed] [Google Scholar]
- Marquis MS, Rogowski JA, Escarce JJ. The Managed Care Backlash: Did Consumers Vote with Their Feet? Inquiry. 2004;41(4):376–90. doi: 10.5034/inquiryjrnl_41.4.376. [DOI] [PubMed] [Google Scholar]
- May P. Mandate Design and Implementation: Enhancing Implementation Efforts and Shaping Regulatory Styles. Journal of Policy Analysis and Management. 1993;12(4):634–63. [Google Scholar]
- McCue M, Mark BA, Harless DW. Nurse Staffing, Quality, and Financial Performance. Journal of Health Care Finance. 2003;29(4):54–76. [PubMed] [Google Scholar]
- McHugh M, Kang R, Hasnain-Wynia R. Understanding the Safety Net: Inpatient Quality of Care Varies Based on How One Defines Safety Net Hospitals. Medical Care Research and Review. 2009;66(5):590–605. doi: 10.1177/1077558709334895. [DOI] [PubMed] [Google Scholar]
- McHugh MD, Kelly L, Sloane DM, Aiken LH. Contradicting Fears, California's Nurse-to-Patient Staffing Mandate Did Not Reduce the Skill Level of the Nursing Workforce in Hospitals. Health Affairs (Millwood) 2011;30(7):1299–306. doi: 10.1377/hlthaff.2010.1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-Staffing Levels and the Quality of Care in Hospitals. New England Journal of Medicine. 2002;346(22):1715–22. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S. Nurse Staffing in Hospitals: Is There a Business Case for Quality? Health Affairs. 2006;25(1):204–11. doi: 10.1377/hlthaff.25.1.204. [DOI] [PubMed] [Google Scholar]
- Rothberg MB, Abraham I, Lindenauer PK, Rose DN. Improving Nurse-to-Patient Staffing Ratios as a Cost-Effective Safety Intervention. Medical Care. 2005;43(8):785–91. doi: 10.1097/01.mlr.0000170408.35854.fa. [DOI] [PubMed] [Google Scholar]
- Scholz J. Cooperation, Deterrence, and the Ecology of Regulatory Enforcement. Law and Society Review. 1984;18(2):179–224. [Google Scholar]
- Seago JA, Spetz J, Chapman S, Dyer W, Grumbach K. Supply, Demand, and Use of Licensed Practical Nurses. Washington, DC: U.S. Department of Health and Human Services, Health Resources and Services Administration; 2004. [Google Scholar]
- Seago JA, Williamson A, Atwood C. Longitudinal Analyses of Nurse Staffing and Patient Outcomes: More about Failure to Rescue. Journal of Nursing Administration. 2006;36(1):13–21. doi: 10.1097/00005110-200601000-00005. [DOI] [PubMed] [Google Scholar]
- Sochalski J, Konetzka RT, Zhu J, Volpp K. Will Mandated Minimum Nurse Staffing Ratios Lead to Better Patient Outcomes? Medical Care. 2008;46(6):606–13. doi: 10.1097/MLR.0b013e3181648e5c. [DOI] [PubMed] [Google Scholar]
- Spetz J. California's Minimum Nurse-to-Patient Ratios: The First Few Months. Journal of Nursing Administration. 2004;34(12):571–78. doi: 10.1097/00005110-200412000-00007. [DOI] [PubMed] [Google Scholar]
- Spetz J, Donaldson N, Aydin C, Brown DS. How Many Nurses per Patient? Measurements of Nurse Staffing in Health Services Research. Health Services Research. 2008;43(5):1674–92. doi: 10.1111/j.1475-6773.2008.00850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spetz J, Seago JA, Coffman J, Rosenoff E, O’Neill E. Minimum Nurse Staffing Ratios in California Acute Care Hospitals. San Francisco: University of California; 2000. San Francisco, Center for the Health Professions. [Google Scholar]
- Taylor EF, Cunningham P, McKenzie K. Community Approaches to Providing Care for the Uninsured. Health Affairs. 2006;25(3):w173–82. doi: 10.1377/hlthaff.25.w173. [DOI] [PubMed] [Google Scholar]
- Tourangeau AE, Giovannetti P, Tu JV, Wood M. Nursing-Related Determinants of 30-Day Mortality for Hospitalized Patients. Canadian Journal of Nursing Research. 2002;33(4):71–88. [PubMed] [Google Scholar]
- Unruh LY, Fottler MD, Talbott LL. Improving Nurse Staffing Measures: Discharge Day Measurement in “Adjusted Patient Days of Care. Inquiry. 2003;40(3):295–304. doi: 10.5034/inquiryjrnl_40.3.295. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor, Bureau of Labor Statistics. Local Area Unemployment Statistics. 2010. Available at http://www.bls.gov/lau/home.htm (accessed November 29, 2010)
- Wennberg J, Cooper M. The Dartmouth Atlas of Health Care. Hanover, NH: Center for the Evaluative Clinical Sciences, Dartmouth Medical School; 1998. [PubMed] [Google Scholar]
- Werner RM, Goldman E, Dudley RA. Comparisons of Change in Quality of Care between Safety-Net and Non Safety-Net Hospitals. JAMA. 2008;299(18):2180–87. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- Zuckerman S, Bazzoli GJ, Davidoff A, LoSasso A. How Did Safety-Net Hospitals Cope in the 1990s? Health Affairs. 2001;20(4):159–68. doi: 10.1377/hlthaff.20.4.159. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Khan N. Safety-Net Activities and Hospital Contracting with Managed Care Organizations. Medical Care Research and Review. 2006;63(6):90S–111S. doi: 10.1177/1077558706293838. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Khan N. Safety-Net Hospitals. Medical Care Research and Review. 2008;65(4):478–95. doi: 10.1177/1077558708315440. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Khan N, Bamezai A. The Relationship between Safety Net Activities and Hospital Financial Performance. BMC Health Services Research. 2010;10(15):1–12. doi: 10.1186/1472-6963-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]


