Abstract
Objective
To investigate the psychometric properties of the Community Integration Questionnaire (CIQ) in a mixed sample of adults with physical disabilities.
Design
Cross-sectional, survey study.
Setting
Academic and community medical clinics, national registry, and self-referral.
Participants
Community-dwelling adults with spinal cord injury (n=146), multiple sclerosis (n=174), limb loss (n=158), or muscular dystrophy (n=273).
Interventions
Not applicable.
Main Outcome Measures
CIQ, General Health item from the Medical Outcomes Study 36-Item Short-Form Health Survey, and Mental Health Scale from the Medical Outcomes Study 36-Item Short-Form Health Survey.
Results
Based on the original scoring procedures, the CIQ Total scale and Home Integration subscale demonstrated acceptable internal consistency; however, reliability indices for the Social Integration and Productive Activities subscales were suboptimal. The exploratory factor analysis yielded a 4-factor solution (accounting for approximately 63% of the variance) that did not replicate the original factor structure of the CIQ. The results of the confirmatory factor analyses indicated that a modified 3-factor solution provided the best fit to the data from our samples. Using a revised scoring system based on these findings, the CIQ demonstrated improved reliability relative to the original scoring and good concurrent validity.
Conclusions
The results provide general support for the validity of the CIQ as a measure of participation in adults with physical disabilities. However, our results indicate that some small modifications to the original scoring system are needed to optimize its use in this patient group. Additional research is needed to refine the measurement of participation in these and other populations.
Keywords: Disabled persons, Outcome assessment (health care), Psychometrics, Quality of life, Rehabilitation
Functional activity and participation are important outcomes across disease/illness categories.1–3 Participation is conceptualized as the performance of activities in real-world domains, including domestic, social, and occupational activities.4 Participation is an important outcome for individuals with a physical disability, given that engagement in valued activities is associated with quality of life.5 Therefore, instruments are needed that accurately measure this outcome.6
The Community Integration Questionnaire (CIQ)7 is a commonly used measure of participation. Development of the CIQ originated with a panel of experts who sought to assess handicap in 3 primary domains: home, social, and productive activities. These domains are consistent with the World Health Organization (WHO) concept of handicap, but they do not encompass all 6 domains that were articulated by the WHO at that time: orientation, physical independence, mobility, occupation, social integration, and economic self-sufficiency.8 The CIQ is scored to create a Total scale score and 3 subscales assessing Home Integration, Social Integration, and Productive Activities. Although the CIQ assesses level of independence and frequency of engagement in activities, it does not query respondents about their satisfaction in these areas.
The CIQ was originally developed for individuals with a traumatic brain injury (TBI) and is widely used in research in this population.9,10 The CIQ has generally demonstrated good measurement properties in TBI samples (see Methods section below). In the largest principal components analysis to date, Sander et al11 found a 3-factor solution corresponding to home, social, and productive activities to be optimal. The productivity factor was least robust among the 3 factors. Although largely consistent with the original scoring method,7 the authors recommended the following minor changes to the measure: excluding the childcare item from score calculations, scoring the personal finances item on Social Integration rather than Home Integration, dropping the item on shopping frequency, and scoring the travel frequency item on Social Integration rather than Productive Activities.11 Using a revised scoring system, the CIQ demonstrated good concurrent validity through its associations with other well-established measures of functioning.11
The CIQ has also been used recently in research with other patient groups, including spinal cord injury (SCI),12–14 cerebral palsy,15 multiple sclerosis (MS),12,16 muscular dystrophy (MD),12 and aphasia.17 However, little is known about the CIQ’s psychometric properties in these other groups, the 1 exception being aphasia. In a study of 150 individuals with poststroke aphasia, the CIQ demonstrated good internal consistency, excellent test-retest reliability, and acceptable construct validity.17 Other than this exception, we are not aware of any published research that has thoroughly examined the psychometric properties of the CIQ in non-TBI samples.
A few studies are relevant to the issue of establishing the CIQ’s psychometric properties in non-TBI samples. For example, Johnston et al13 found that CIQ scores were significantly lower (indicating more handicap) 1 year after SCI compared with preinjury. Another study found that sports participation after SCI was associated with higher CIQ scores, and the CIQ discriminated between sport and nonsport participants.14 Although these results suggest that the CIQ may be valid in individuals with SCI, they do not sufficiently establish its psychometric properties in this group.
Even less psychometric support is found among other non-TBI groups. In 1 small study, the CIQ did not differentiate between adults with CP and healthy participants.15 Another study of adults with MS found that only the Productive Activities subscale differentiated between those who did and did not have current/recent pain.16 The authors of that study noted that “the psychometric properties of the CIQ may not be as strong in the MS population” and that “research on the psychometric utility of the CIQ in the MS population is recommended” (page 636).16 Although this recommendation echoes that of others,18,19 it has largely been unheeded.
Although it may make intuitive sense that CIQ items are equally important aspects of participation in non-TBI rehabilitation groups, these assumptions must be tested.10 Therefore, the current study examined the psychometric properties of the CIQ in a large sample of adults with a variety of physical disabilities. We combined multiple disability groups and analyzed them collectively for the primary analyses, because we did not have sufficient sample sizes to comprehensively examine the psychometrics of the CIQ in each of the separate disabilities. Moreover, because we could find no previous studies examining its psychometrics in individuals with physical disabilities, we considered it most prudent to analyze the pooled data, which increased the power of our analyses.
METHODS
Participants and Procedures
All procedures were approved by the University of Washington Institutional Review Board. Most participants were recruited through previous survey studies on quality of life conducted in the Department of Rehabilitation Medicine at the University of Washington, and from the national registry of Myotonic Dystrophy and Facioscapulohumeral Muscular Dystrophy. Additional recruitment sources included other survey and treatment studies at the University of Washington, the Northwest Regional Spinal Cord Injury Systems list, referral from local clinics, and self-referral.
A total of 1371 (SCI, n=333; MS, n=296; limb loss, n=346; and MD, n=396) survey packets were mailed to prospective participants. Participants who returned a survey were paid $25. The final sample consisted of 751 community-dwelling adults with SCI (n=146), MS (n=174), limb loss (n=158), or MD (n=273). Although the data from this study has been used in previous research,20–23 the current analyses address distinct questions not previously investigated.
Measures
Demographic and clinical characteristics
Respondents provided information about their age, sex, education, employment, race/ethnicity, and marital status, as well as their clinical condition.
Participation
The 15-item CIQ7 was designed to assess 3 domains of handicap (home, social, and productive activities) and was developed based on input from experts in TBI outcomes. For the current study, we followed the original scoring procedures7 that produce a Total scale score and 3 subscales: Home Integration (eg, meal preparation, housework), Social Integration (eg, leisure activities with others), and Productive Activities (eg, employment status). Higher scores indicate better functioning. The subscales were derived from a factor analysis of data from a relatively small sample24; subsequent research replicating this exact factor structure in TBI samples has been mixed.11,18
Evidence for the reliability of the CIQ in TBI is generally positive. Three of 4 studies19,24–26 reported internal consistency for the Total scale score that exceed the traditional cutoff for being acceptable (α<.7027). In 1 study, 10-day test-retest reliability was .91 for the Total scale score, and between .83 and .93 for the subscales.25 Internal consistency for Social Integration and especially Productive Activities is generally lower; the lower values for Productive Activities are likely based, in part, on the fact that this subscale is comprised of only 2 variables.
The validity of the CIQ in TBI is supported by several studies. Whiteneck et al28 reported significant associations between the Total scale, Home Integration, and Productive Activities— but not Social Integration—and scores on the Craig Handicap Assessment and Reporting Technique,28 which is another widely used measure of community integration. The CIQ has also been found to be significantly associated with measures of life satisfaction,26,29 executive functioning, logical memory, and reading ability.30 The CIQ can distinguish between individuals with and without TBI18,25,31 and between individuals with TBI living in different settings.25
General health
General health was assessed with an item from the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36)32: “In general, would you say your health is …” Responses are indicated on a 5-item Likert scale ranging from excellent to poor. Higher scores indicate better general health. This single-item measure is widely used in health outcomes research33–39 and is a substitute for multi-item measures of self-rated health.40,41 The general health item has demonstrated reliability and validity in diverse patient samples.42–44 For example, it significantly predicted mortality, hospitalization, and health care utilization in patients from general internal medicine clinics43; its predictive validity was comparable to that of 2 commonly used, multi-item measures of health.32,45 The general health item has also performed well in acutely ill patients; it was significantly correlated with other general health measures among adults recently discharged from the intensive care unit.42
Psychological functioning
Psychological functioning was assessed with the 5-item Mental Health Scale of the SF-36.32 The Mental Health Scale ranges from 0 to 100, with higher scores indicating better functioning. This measure is widely used and possesses strong psychometric properties. Across numerous studies of diverse patient groups, the Mental Health Scale’s reliability generally exceeds 0.80.46–49 The Mental Health Scale is among the most valid of all the SF-36 scales and is considered by some to be the most valid measure of mental health in studies to date.47,48,50 It is useful in screening for mental health disorders49,51 and is responsive to changes in mental health variables after treatment.52,53
Statistical Analyses
The survey response rate was examined for descriptive purposes. Listwise deletion was used for missing data such that the primary analyses included only participants with complete data on the CIQ, general health, and Mental Health Scale. Listwise deletion was chosen due to the small (<5%) and random nature of the missing data and because of the large sample of the current study.54 We then calculated means and SDs for the CIQ and other measures. Internal consistency of the CIQ was evaluated with Cronbach alpha (coefficients ≥.70 are acceptable27) and corrected item-total and item-subscale correlations (coefficients ≥.30 are acceptable55).
Known-groups validity was evaluated via 1-way analysis of variance (ANOVA) (followed by Bonferroni post hoc tests) comparing CIQ scores among the 4 disability groups. Construct validity was also evaluated with exploratory and confirmatory factor analyses (CFAs). SPSS version 17.0a was used for an exploratory factor analysis examining the CIQ factor structure, without imposing any constraints on the data or analysis. Specifically, we conducted a principal component analysis with varimax (orthogonal) rotation and Kaiser normalization to ease interpretation of the produced factors. A factor threshold of eigenvalues greater than 1 was specified. Factor loadings of .60 or higher were considered meaningful.56
Next, CFAs with maximum likelihood were conducted using LISREL 8.72b to determine whether the CIQ structure found in previous TBI samples fit the current data. Initially, a 3-factor solution was specified in which items were loaded on factors according to the original scoring procedures.7 Specifically, items 1 through 5, 6 through 11, and 12 through 15 loaded on Home Integration, Social Integration, and Productive Activities respectively. Items 13 to 15 are combined into a composite variable (job/school); thus Productive Activities is comprised of only 2 items: item 12 and job/school. In the event this 3-factor model was not a sufficiently good fit, we planned to estimate other models to identify one that best fit the data. Estimation of these additional models will take into account the modification indices from the statistical output, as well as the theoretical and practical purposes of the CIQ (eg, item-factor loadings will be allowed to deviate from the original scoring system only if it makes theoretical and/or practical sense).
The CFA goodness-of-fit indices describe how well an identified model can reproduce the actual data. We examined the Non-Normed Fit Index (NNFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). The NNFI takes into account the number of parameters in a model by correcting for the chi-square/degrees of freedom ratio; coefficients between .90 and .95 are considered acceptable, and good fitting models have values of .95 or higher.57,58 The RMSEA is based on the noncentrality parameter. Good models have an RMSEA of .05 or less, while models with values of .10 or higher have poor fit.57,58 Ideally, the values for the 90% confidence interval of the RMSEA range from 0 to .10.57,58 The SRMR is the standardized difference between the observed and predicted covariance. A value of zero indicates perfect fit, and values of .08 or less indicate good fit.57,58
Concurrent validity was assessed with correlations between the CIQ and both general health and Mental Health Scale because these domains are related to, but distinct from, participation. Coefficients of moderate magnitude (r≈.30)59 were expected; coefficients that met or exceeded this expectation were considered to support the CIQ’s concurrent validity.
RESULTS
Participant Characteristics
The sample included 751 individuals (response rate=55%) with 1 of 4 physical disabilities (SCI, n=146; MS, n=174; limb loss, n=158; MD, n=273). There were slightly more men (52%) and a preponderance of whites (93%). The average age ± SD was 50.86±13.48 years (range, 18 –91). Most were married or living with a significant other (66%), and the remainder were never married (17%), divorced/separated (14%), or widowed (4%). Most reported education beyond high school (84%), and only 2% did not graduate high school or attain their General Educational Development certificate. Thirty-six percent were working full- or part-time, and 41% were unemployed due to pain or disability.
The majority of participants with SCI reported thoracic (42%) or cervical (41%) injuries. Fifty-one percent reported an incomplete SCI, 39% a complete SCI, and 10% did not know. Forty-one percent reportedly were injured in a motor vehicle collision, 17% in a fall, 15% in a sporting/diving accident, 3% from a gunshot, and the remainder from miscellaneous causes. Participants with SCI reported a mean injury duration ± SD of 16.12±10.63 years. Among participants with MS, the following disease types were reported: relapsing-remitting (59%), secondary-progressive (19%), primary-progressive (15%), and progressive-relapsing (7%). These participants reported an average disease duration ± SD of 17.35±9.72 years. Most participants with limb loss reported lower limb loss only (95%). The modal causes of limb loss were injury (51%), diabetes/vascular disease (20%), and infection (20%). The average duration ± SD of limb loss was 20.72±16.52 years. Participants with MD reported an average disease duration ±SD of 15.54±12.04 years.
Internal Consistency
Table 1 contains means and SDs for the CIQ. Results of internal consistency analyses, using the original scoring procedures,7 indicated that the Total scale (α=.75) and Home Integration (α=.84) demonstrated adequate-to-good reliability, whereas Social Integration (α=.51) and Productive Activities (α=.45) did not. Correlation analyses indicated that the Total scale score was significantly (all Ps<.001) and strongly associated with Home Integration (r=.77), Social Integration (r=.78), and Productive Activities (r=.69). Corrected item-total and item-subscale correlations are presented in table 2. There was considerable variability in item-subscale (range, .10 –.89) and item-total (range, .26 –.71) coefficients; the strongest associations and those indicative of sufficient internal consistency were generally found for Home Integration and the weakest for Social Integration.
Table 1.
Descriptive Data on the CIQ and SF-36 Scales
| Measure | Range | Mean ± SD
|
||||
|---|---|---|---|---|---|---|
| Total Sample | SCI | MS | Limb Loss | MD | ||
| CIQ | ||||||
| Total | 0–25 | 17.09±5.11 | 17.30±5.13 | 17.34±5.21 | 16.80±5.30 | 16.98±4.94 |
| Home Integration | 0–10 | 4.93±2.63 | 4.65±2.85 | 5.46±2.59 | 4.80±2.60 | 4.83±2.52 |
| Social Integration | 0–10 | 8.46±2.15 | 8.66±2.12 | 8.33±2.14 | 8.46±2.24 | 8.44±2.13 |
| Productivity | 0–5 | 3.69±2.04 | 3.99±2.02 | 3.55±2.00 | 3.54±2.05 | 3.71±2.07 |
| SF-36 | ||||||
| General health | 0–5 | 3.24±1.14 | 3.39±1.11 | 3.31±1.12 | 3.36±1.17 | 3.04±1.12 |
| Mental Health Scale | 0–100 | 70.95±19.37 | 71.37±18.61 | 69.66±19.44 | 74.41±19.11 | 69.54±19.73 |
Table 2.
Corrected Item-Total and Item-Subscale Correlations
| CIQ Items | Home Integration | Total | Social Integration | Total | Productive Activities | Total |
|---|---|---|---|---|---|---|
| Who does the shopping? | .66 | .64 | ||||
| Who does the meal preparation? | .72 | .60 | ||||
| Who does the housework? | .66 | .57 | ||||
| Who provides childcare? | .89 | .71 | ||||
| Who plans the social arrangements? | .36 | .47 | ||||
| Who does the personal finances? | .10 | .40 | ||||
| Shopping frequency? | .30 | .52 | ||||
| Frequency of leisure activities? | .43 | .47 | ||||
| Frequency of visiting friends or relatives? | .46 | .47 | ||||
| Activities alone or with others? | .26 | .26 | ||||
| Do you have a best friend? | .17 | .30 | ||||
| Frequency of travel outside the home? | .46 | .56 | ||||
| Job/school?* | .46 | .46 |
NOTE. All correlations are significant at P<.01.
Combination of items 13 to 15 assessing work, school activities, and volunteer activities.
Known-Groups Validity
Separate 1-way ANOVAs compared the CIQ Total scale and subscales across the disability groups (see table 1). Of these, analysis of Home Integration returned the only significant result (F3,747=3.17, P<.05). Post hoc comparisons indicated the MS group reported better functioning on Home Integration than the SCI group (P<.05), although the magnitude of this difference (Cohen’s d=.30) was modest.59 There were no other significant differences between disability groups, suggesting that the CIQ does not demonstrate measurement invariance across disability groups.
Exploratory Factor Analysis
The principal component analysis returned a 4-factor solution accounting for approximately 63% of the variance in the data. Table 3 presents individual item loadings for the 4 factors. Note that only 13 items are included because items 13 to 15 are combined into job/school in accord with the original scoring system.7 Although these results did not exactly replicate the original factor structure,7 there were several consistencies in the findings, particularly for Home Integration and Social Integration. Consistent with the original scoring, items 1 to 4 loaded on factor 1 (Home Integration), and items 7 to 9 loaded on factor 2 (Social Integration). Factor 3 is comprised of items that typically load on Home Integration (social arrangements), Social Integration (finances), and Productive Activities (job/school), suggesting some degree of overlap in how respondents answered those questions. The 2 items loading on factor 4 are typically scored on Social Integration.
Table 3.
Individual Item Loadings for Exploratory Factor Analysis That Yielded 4 Factors
| CIQ Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|
| Who does the shopping? | .783 | |||
| Who does the meal preparation? | .851 | |||
| Who does the housework? | .801 | |||
| Who provides childcare? | .883 | |||
| Who plans the social arrangements? | .590 | |||
| Who does the personal finances? | .679 | |||
| Shopping frequency? | .617 | |||
| Frequency of leisure activities? | .776 | |||
| Frequency of visiting friends or relatives? | .677 | |||
| Activities alone or with others? | .635 | |||
| Do you have a best friend? | .726 | |||
| Frequency of travel outside the home? | .702 | |||
| Job/school?* | .597 |
NOTE. Extraction method: principal component analysis. Rotation method: varimax with Kaiser normalization.
Combination of items 13 to 15 assessing work, school activities, and volunteer activities.
Confirmatory Factor Analysis
Given the results above, several CFAs were conducted to further explore the structure of the data. Initially, a 3-factor solution was specified in which items were constrained to load on only 1 factor according to the original scoring,7 and the factors were not allowed to covary. Using the aforementioned parameters, the specified model failed to converge. When alternative models were explored, item 4 (childcare) proved consistently problematic (eg, nonsignificant error variances, inconsistent factor loadings, poor model convergence when included in the analyses). Item 4 has been discussed frequently in previous studies, with several investigators recommending it be dropped for statistical and practical (ie, many respondents do not have children) reasons.11,60,61 Given this, our examination of alternative models also included analyses in which item 4 was excluded.
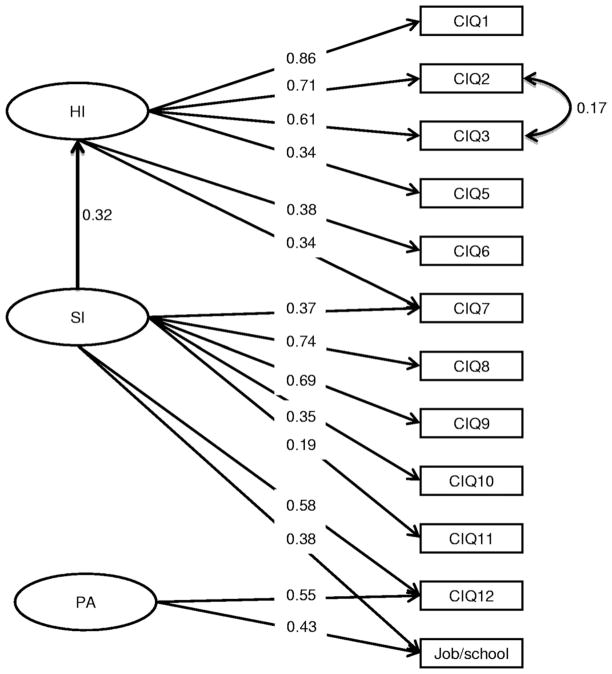
An alternative 3-factor model excluding item 4 provided the best fit for the current data. The goodness-of-fit indices include: (df=50; RMSEA=.05; 90% confidence interval for RMSEA, .04 –.06; P for test of close fit [RMSEA<.05]=.23; NNFI=.95; Goodness of Fit Index=0.97; and Adjusted Goodness of Fit Index=.95). The individual item loadings (fig 1) for this best-fitting model were generally consistent with the original scoring; however, some loadings deviated. Items 6 and 7 are typically scored on Social Integration; however, in our analyses, item 6 loaded on Home Integration, and item 7 cross-loaded on Home Integration and Social Integration. Items 12 and job/school cross-loaded on Social Integration and Productive Activities in our analyses but are originally scored on Productive Activities only. Two additional considerations were made to produce the well-fitting model presented herein. First, the parameter between Home Integration and Social Integration was freed, thus allowing these factors to covary. Second, the error terms for items 2 and 3 were also allowed to covary.
Fig 1.
Results of the CFA identifying the best-fitting model. CFA with maximum likelihood. CIQ item 4 was not included in these analyses. Job/school is a combination of items 13 to 15 assessing work, school, and volunteer activities. HI, Home Integration; PA, Productive Activities; SI, Social Integration.
Concurrent Validity
The results of correlation analyses (table 4) indicated that the CIQ Total scale score was significantly associated with general health (r=.34, P<.001) and Mental Health Scale (r=.21, P<.001). Only the correlation with general health met our a priori expectation regarding the strength of the relationships (r≈.30). Nevertheless, the results indicated that more participation was related to higher levels of perceived general and mental health.
Table 4.
Correlations Between CIQ and SF-36 Scales
| SF-36 | Total | CIQ Original Scoring
|
CIQ Revised Scoring
|
||||
|---|---|---|---|---|---|---|---|
| Home Integration | Social Integration | Productive Activities | Home Integration | Social Integration | Productive Activities | ||
| General health | .340* | .152* | .300* | .341* | .151* | .341* | .306* |
| Mental Health Scale | .205* | .048 | .249* | .190* | .048 | .302* | .125* |
Significant at P<.01.
Two sets of analyses were conducted to examine the associations between CIQ subscales, general health, and Mental Health Scale. The first included subscales as originally scored. The second included subscales scored based on the factor analytic results of the current study. Specifically, Home Integration was recalculated to exclude item 4 and include item 6. Because items 7, 12, and job/school had cross-loadings on 2 different subscales, we elected to score them based on the highest loading. Thus, items 7 and 12 were scored on Social Integration, and job/school was scored on Productive Activities.
The results of both sets of analyses were similar (see table 4). The only nonsignificant relationships were between Home Integration (original and revised) and Mental Health Scale. All significant relationships were in the expected direction indicating that more participation was related to higher levels of general and mental health. The magnitudes for some, but not all, of these relationships were consistent with our a priori expectations. The biggest difference in results between the 2 scoring systems concerned Social Integration and Productive Activities. Compared with the original, the revised system yielded a stronger relationship between Social Integration and both general health and Mental Health Scale, and a weaker relationship between Productive Activities and both measures. However, the magnitude of these differences was not statistically significant (all Ps>.05).
DISCUSSION
Participation involves functioning in domestic, social, and occupational settings4 and is a key indicator of quality of life. Participation is an important outcome across diverse disease/illness categories.1–3 Despite its importance, few psychometrically sound instruments measure this construct. One of the most commonly used instruments is the CIQ. Although originally developed for use in TBI, it has been used increasingly in research on non-TBI populations.12–16 Nevertheless, we could not find any studies that comprehensively examined its psychometric properties in these groups. The current study addresses this gap. The overall results provide general psychometric support for the CIQ for clinical and research use in this population. However, these results did not exactly replicate those from which the original scoring system was derived. The implications of these discrepancies are discussed throughout the Discussion section.
Our comprehensive analytic approach included exploratory and confirmatory analyses. Because factor analytic results can differ substantially based on parameter specifications,56 using just 1 approach can yield erroneous conclusions. Our approach minimized this possibility and allowed us to determine if consistent patterns emerged across analyses. The results suggest the original scoring system7 may require modification to optimize use of the CIQ in adults with physical disabilities.
Although we largely replicated the item-factor loadings of the original scoring of Home Integration, item 6 (personal finances) loaded on Home Integration in our analyses but is originally scored on Social Integration. Item 6 seems more similar to other home-based activities; therefore, we consider it a reasonable scoring modification to include it on Home Integration when using the CIQ in physically disabled adults. Interestingly, this echoes the suggestion of Sander et al11 based on results of a large TBI study. Also, in keeping with the revised scoring system recommended by Sander,11 we found that dropping item 4 (childcare), which is originally scored on Home Integration, improved the CIQ’s psychometrics. Because many physically disabled respondents may not have children, this too seems a reasonable scoring modification. However, we recommend making this modification on a post hoc basis, as opposed to deleting the item altogether, so as to not lose potentially meaningful information from respondents who do have children.
Several item-factor cross-loadings were also necessary to achieve a well-fitting model in our data. Item 7 (shopping frequency) is originally scored on Social Integration but cross-loaded on Home Integration and Social Integration. The magnitude of these loadings was similar, suggesting this item equally taps a unique component common to both domains. These results are consistent with those from another study in TBI.11 One can certainly conceive shopping as a home-related activity; indeed, another shopping item (item 1) is scored on Home Integration. Conversely, shopping outside the home is inherently social. Moreover, many individuals with a physical disability require assistance to complete shopping-related activities. Although others11 have suggested dropping this item from the CIQ, we suggest retaining it for additional research among physically disabled adults. Our more cautious recommendation is because, unlike TBI, few studies have examined the factor structure of the CIQ in adults with physical disabilities. Thus, we consider it prudent to recommend additional research before making major changes to the CIQ’s item composition.
Item 12 (travel frequency) had equivalent loadings on Social Integration and Productive Activities but is typically scored only on Productive Activities. Physically disabled adults often require assistance from others to travel, thus making this a social activity regardless of travel purpose. However, because travel often relates to academic and/or vocational activities, it also makes sense that item 12 loads on Productive Activities. Sander et al11 found it loaded exclusively on Social Integration, which is reflected in their revised scoring. At this point, it is unclear how to score this item for adults with a physical disability. Because of a slightly stronger loading, we scored it on Social Integration for subsequent analyses. However, further research is needed to determine an optimal long-term solution in physically disabled groups.
Finally, job/school loaded on Social Integration and Productive Activities in our analyses, but is typically scored only on Productive Activities. We analyzed the composite variable, whereas others (eg, Sander11) have considered separately the 3 individual items that comprise job/school. Although these analytic differences could produce discrepant findings, our results are in line with previous research highlighting concerns about Productive Activities. In fact, this factor has consistently been less robust than Home Integration and Social Integration in studies across and within diagnostic groups.11,17–19,61 As such, we agree with others11 that additional items may be needed to improve measurement of this domain.
Our results also help establish the concurrent validity of the CIQ (original and revised scoring) among the current heterogeneous sample, indicating its usefulness in non-TBI groups. With the exception of Home Integration, the Total scale and subscales demonstrated significant and positive associations with 2 well-established measures of general and mental health. Importantly, these associations, although significant, were weak to moderate in magnitude,59 indicating that the CIQ measures a related but distinct construct. Two recent studies in SCI14,62 also support the CIQ’s concurrent validity in non-TBI samples. Although neither study involved an extensive psychometric analysis, they do suggest the CIQ is a useful measure of participation in this diagnostic group.
Our reliability analyses also raise concerns about the original scoring system in individuals with a physical disability. The revised scoring based on our findings proved superior in this respect; internal consistency coefficients for Home Integration and Social Integration were .74 and .63, respectively (α for Productive Activities could not be calculated because it consisted of a single item). Interestingly, these findings concerning the original scoring are generally consistent with previous research in TBI samples.9
The CIQ is not the only measure of participation for individuals with disabilities.63 However, it is widely used in research and practice, likely due to its face validity, correspondence with the WHO4 concept of handicap, brevity, and ease of administration. Despite these positive features, concerns have been raised about the CIQ. Dijkers’18 critiques regarding scope, content, and norms seem particularly relevant to the current study. In terms of content, as noted in the Introduction and Methods sections, the CIQ was developed to assess 3 domains of handicap; whereas the most recent WHO conceptualization includes 9 domains.4 The CIQ does not assess all of these domains; for example, it does not contain content on learning/applying knowledge or communication. Additional research can determine whether and how to improve existing measures of participation to maximize their research and clinical applications.
Study Limitations
Several study limitations should be considered. First, the sample was largely white and well-educated, which may limit generalizability of the findings. Second, we sampled from 4 disability groups, which represents only a subset of disability diagnoses. Third, because we did not formally screen for cognitive impairment, we cannot be certain these participants comprised a “pure” physical disability sample. Fourth, the CIQ’s psychometric properties might differ across disability diagnoses; for example, functioning at home may differ whether one has MS, SCI, or another disability. Although we found, with the exception of Home Integration, the disability groups did not differ on the CIQ, this is an insufficient level of analysis to determine whether the CIQ has differential performance across groups. Unfortunately, we did not have sufficient sample sizes to more thoroughly examine the CIQ’s psychometrics separately for each group. Finally, conclusions about concurrent validity would have been stronger if nonself-report assessments, such as behavioral measures and spouse/partner report, were included in these analyses.
CONCLUSIONS
This study provides important information about the psychometric properties of the CIQ. The CIQ appears to sufficiently measure participation in adults with physical disabilities. However, our results indicate that scoring modifications are needed to optimize its use in this patient group. Our findings also indicate that additional research is needed to improve the CIQ, particularly related to the subscale purporting to measure productive activities. Such research is needed given the emphasis on participation in clinical and empirical activities involving individuals with rehabilitation needs.
Acknowledgments
We thank Silvia Amtmann, Natalie Brown, Tyler Einheuser, Kevin Gertz, Amy Hoffman, Chiara LaRotonda, Ciara Kim, Kerry Madrone, Kristin McArthur, Laura Nishimura, Sarah O’Brien, Noel Pereyra-Johnston, Emily Phelps, Sophia Purekal, Leo Sim, Joseph Skala, Lindsay Washington, Eric Weitz, and Sylia Wilson in data collection and management.
Supported in part by the National Institutes of Health, National Institute of Child Health and Human Development, and the National Center for Medical Rehabilitation Research (grant nos. T32 HD007424, PO1 HD33988).
List of Abbreviations
- ANOVA
analysis of variance
- CFA
confirmatory factor analysis
- CIQ
Community Integration Questionnaire
- MD
muscular dystrophy
- MS
multiple sclerosis
- NNFI
Non-Normed Fit Index
- RMSEA
root mean square error of approximation
- SCI
spinal cord injury
- SF-36
Medical Outcomes Study 36-Item Short-Form Health Survey
- SRMR
standardized root mean square residual
- TBI
traumatic brain injury
- WHO
World Health Organization
Footnotes
Presented as a poster session to the Society of Behavioral Medicine, April 7–10, 2010, Seattle, WA.
Suppliers
- SPSS Inc, 233 S Wacker Dr, 11th Fl, Chicago, IL 60606.
- Scientific Software International Inc, 7383 N Lincoln Ave, Ste 100, Lincolnwood, IL 60712.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
Contributor Information
Adam T. Hirsh, Department of Psychology, Indiana University – Purdue University Indianapolis, Indianapolis, IN.
Alan L. Braden, Department of Rehabilitation Medicine, University of Washington School of Medicine, Seattle, WA.
Jason G. Craggs, Department of Clinical and Health Psychology, University of Florida, Gainesville, FL.
Mark P. Jensen, Department of Rehabilitation Medicine, University of Washington School of Medicine, Seattle, WA.
References
- 1.Salter KL, Foley NC, Jutai JW, Teasell RW. Assessment of participation outcomes in randomized controlled trials of stroke rehabilitation interventions. Int J Rehabil Res. 2007;30:339–42. doi: 10.1097/MRR.0b013e3282f144b7. [DOI] [PubMed] [Google Scholar]
- 2.van der Mei SF, van Sonderen EL, van Son WJ, de Jong PE, Groothoff JW, van den Heuvel WJ. Social participation after successful kidney transplantation. Disabil Rehabil. 2007;29:473–83. doi: 10.1080/09638280600841257. [DOI] [PubMed] [Google Scholar]
- 3.van de Ven L, Post M, de Witte L, van den Heuvel W. It takes two to tango: the integration of people with disabilities into society. Disabil Soc. 2005;20:311–29. [Google Scholar]
- 4.World Health Organization. International Classification of Functioning, Disability and Health (ICF) Geneva: World Health Organization; 2001. [Google Scholar]
- 5.Renwick R, Nourhaghighi N, Manns PJ, Rudman DL. Quality of life for people with physical disabilities: a new instrument. Int J Rehabil Res. 2003;26:279–87. doi: 10.1097/00004356-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Tate DG. Hospital to community: changes in practice and outcomes. Rehabil Psychol. 2001;46:125–38. [Google Scholar]
- 7.Willer B, Rosenthal M, Kreutzer JS, Gordon WA, Rempel R. Assessment of community integration following rehabilitation for traumatic brain injury. J Head Trauma Rehabil. 1993;8:75–87. [Google Scholar]
- 8.World Health Organization. International Classification of Impairments, Disabilities, and Handicaps: A Manual of Classification Relating to the Consequences of Disease (ICIDH) Geneva: World Health Organization; 1980. [Google Scholar]
- 9.Dijkers MP, Whiteneck G, El-Jaroudi R. Measures of social outcomes in disability research. Arch Phys Med Rehabil. 2000;81(12 Suppl 2):S63–80. doi: 10.1053/apmr.2000.20627. [DOI] [PubMed] [Google Scholar]
- 10.Yasui NY, Berven NL. Community integration: conceptualisation and measurement. Disabil Rehabil. 2009;31:761–71. doi: 10.1080/09638280802306638. [DOI] [PubMed] [Google Scholar]
- 11.Sander AM, Fuchs KL, High WM, Jr, Hall KM, Kreutzer JS, Rosenthal M. The Community Integration Questionnaire revisited: assessment of factor structure and validity. Arch Phys Med Rehabil. 1999;80:1303–8. doi: 10.1016/s0003-9993(99)90034-5. [DOI] [PubMed] [Google Scholar]
- 12.Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities: a randomized controlled trial. JAMA. 1996;275:1001–6. [PubMed] [Google Scholar]
- 13.Johnston M, Nissim EN, Wood K, Hwang K, Tulsky D. Objective and subjective handicap following spinal cord injury: interrelationships and predictors. J Spinal Cord Med. 2002;25:11–22. doi: 10.1080/10790268.2002.11753596. [DOI] [PubMed] [Google Scholar]
- 14.McVeigh SA, Hitzig SL, Craven BC. Influence of sport participation on community integration and quality of life: a comparison between sport participants and non-sport participants with spinal cord injury. J Spinal Cord Med. 2009;32:115–24. doi: 10.1080/10790268.2009.11760762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Slot WM, Roebroeck ME, Landkroon AP, Terburg M, van den Berg-Emons RJ, Stam HJ. Everyday physical activity and community participation of adults with hemiplegic cerebral palsy. Disabil Rehabil. 2007;29:179–89. doi: 10.1080/09638280600747686. [DOI] [PubMed] [Google Scholar]
- 16.Ehde DM, Osborne TL, Hanley MA, Jensen MP, Kraft GH. The scope and nature of pain in persons with multiple sclerosis. Mult Scler. 2006;12:629–38. doi: 10.1177/1352458506071346. [DOI] [PubMed] [Google Scholar]
- 17.Dalemans RJ, de Witte LP, Beurskens AJ, van den Heuvel WJ, Wade DT. Psychometric properties of the Community Integration Questionnaire adjusted for people with aphasia. Arch Phys Med Rehabil. 2010;91:395–9. doi: 10.1016/j.apmr.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Dijkers M. Measuring the long-term outcomes of traumatic brain injury: a review of the Community Integration Questionnaire. J Head Trauma Rehabil. 1997;12:74–91. [Google Scholar]
- 19.Corrigan JD, Deming R. Psychometric characteristics of the Community Integration Questionnaire: replication and extension. J Head Trauma Rehabil. 1995;10:41–53. [Google Scholar]
- 20.Molton I, Stoelb B, Jensen MP, Ehde D, Raichle K, Cardenas D. Psychosocial factors and adjustment to chronic pain in spinal cord injury: replication and cross-validation. J Rehabil Res Dev. 2009;46:31–42. doi: 10.1682/jrrd.2008.03.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Osborne TL, Jensen MP, Ehde DM, Hanley MA, Kraft GH. Psychosocial factors associated with pain intensity, pain-related interference, and psychological functioning in persons with multiple sclerosis and pain. Pain. 2007;127:52–62. doi: 10.1016/j.pain.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 22.Hirsh AT, Dillworth TM, Ehde DM, Jensen MP. Sex differences in pain and psychological functioning in persons with limb loss. J Pain. 2010;11:79–86. doi: 10.1016/j.jpain.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miro J, Raichle KA, O’Brien SO, et al. Impact of biopsychosocial factors on chronic pain in persons with myotonic and facioscapulohumeral muscular dystrophy. Am J Hosp Palliat Care. 2009;26:308–19. doi: 10.1177/1049909109335146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Willer B, Linn R, Allen K. Community integration and barriers to integration for individuals with brain injury. In: Finlayson MA, Garner SH, editors. Brain injury rehabilitation: clinical considerations. Baltimore: Williams and Wilkins; 1994. pp. 355–75. [Google Scholar]
- 25.Willer B, Ottenbacher KJ, Coad ML. The Community Integration Questionnaire: a comparative examination. Am J Phys Med Rehabil. 1994;73:103–11. doi: 10.1097/00002060-199404000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Heinemann AW, Whiteneck GG. Relationships among impairment disability handicap and life satisfaction in persons with traumatic brain injury. J Head Trauma Rehabil. 1995;10:54–63. [Google Scholar]
- 27.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. Oxford: Oxford Univ Pr; 1989. [Google Scholar]
- 28.Whiteneck GG, Charlifue SW, Gerhart KA, Overhosler JD, Richardson GN. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil. 1992;73:519–26. [PubMed] [Google Scholar]
- 29.Burleigh SA, Farber RS, Gillard M. Community integration and life satisfaction after traumatic brain injury: long-term findings. Am J Occup Ther. 1998;52:45–52. doi: 10.5014/ajot.52.1.45. [DOI] [PubMed] [Google Scholar]
- 30.Hanks RA, Rapport LJ, Millis SR, Deshpande SA. Measures of executive functioning as predictors of functional ability and social integration in a rehabilitation sample. Arch Phys Med Rehabil. 1999;80:1030–7. doi: 10.1016/s0003-9993(99)90056-4. [DOI] [PubMed] [Google Scholar]
- 31.Gordon WA, Hibbard MR, Brown M, Flanagan S, Korves Campbell M. Community integration and quality of life of individuals with traumatic brain injury. In: Rosenthal M, Griffith ER, Kreutzer JS, Pentland B, editors. Rehabilitation of the adult and child with traumatic brain injury. 3. Philadelphia: FA Davis; 1999. pp. 312–25. [Google Scholar]
- 32.Ware J, Snow K, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Lincoln: QualityMetric Inc; 2000. [Google Scholar]
- 33.Gandek B, Ware JE, Aronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: multilevel analysis. BMJ. 1998;317:917–21. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crossley TF, Kennedy S. The reliability of self-assessed health status. J Health Econ. 2002;21:643–58. doi: 10.1016/s0167-6296(02)00007-3. [DOI] [PubMed] [Google Scholar]
- 36.Archibald CJ, Auger WR, Fedullo PF, et al. Long term outcome after pulmonary thromboendarterectomy. Am J Respir Crit Care Med. 1999;160:523–8. doi: 10.1164/ajrccm.160.2.9808109. [DOI] [PubMed] [Google Scholar]
- 37.Wagner AK, Gandek B, Aaronson NK, et al. Cross-cultural comparisons of the content of SF-36 translations across 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:925–32. doi: 10.1016/s0895-4356(98)00083-3. [DOI] [PubMed] [Google Scholar]
- 38.Bullinger M, Alonso J, Apolone G, et al. Translating health status questionnaires and evaluating their quality: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:913–23. doi: 10.1016/s0895-4356(98)00082-1. [DOI] [PubMed] [Google Scholar]
- 39.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23:260–8. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 40.Balkrishnan R, Anderson RT. Predictive power of a risk-assessment questionnaire across different disease states: results in an elderly managed care enrolled population. Am J Manag Care. 2001;7:145–53. [PubMed] [Google Scholar]
- 41.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Chrispin PS, Scotton H, Rogers J, Lloyd D, Ridley SA. Short Form 36 in the intensive care unit: assessment of acceptability, reliability and validity of the questionnaire. Anaesthesia. 1997;52:15–23. doi: 10.1111/j.1365-2044.1997.015-az014.x. [DOI] [PubMed] [Google Scholar]
- 43.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Services Res. 2005;40:1234–46. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Diehr P, Williamson J, Patrick DL, Bild DE, Burke GL. Patterns of self-rated health in older adults before and after sentinel health events. J Am Geriatr Soc. 2001;49:36–44. doi: 10.1046/j.1532-5415.2001.49007.x. [DOI] [PubMed] [Google Scholar]
- 45.Fan VS, Au D, Heagerty P, Deyo RA, McDonell MB, Fihn SD. Validation of case-mix measures derived from self-reports of diagnoses and health. J Clin Epidemiol. 2002;55:371–80. doi: 10.1016/s0895-4356(01)00493-0. [DOI] [PubMed] [Google Scholar]
- 46.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 47.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey manual and interpretation guide. Boston: New England Medical Center, The Health Institute; 1993. [Google Scholar]
- 48.Ware JE, Kosinski M, Keller SK. SF-36 Physical and Mental Health Summary Scales: a user’s manual. Boston: The Health Institute; 1994. [Google Scholar]
- 49.Turner-Bowker DM, Bartley PJ, Ware JE., Jr . SF-36 Health Survey & “SF” bibliography. (1988–2000) 3. Lincoln: QualityMetric Inc; 2002. [Google Scholar]
- 50.McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 51.Berwick DM. The double edge of knowledge. JAMA. 1991;266:841–2. [PubMed] [Google Scholar]
- 52.Beusterien KM, Steinwald B, Ware JE. Usefulness of the SF-36 Health Survey in measuring health outcomes in the depressed elderly. J Geriatr Psychiatry Neurol. 1996;9:13–21. doi: 10.1177/089198879600900103. [DOI] [PubMed] [Google Scholar]
- 53.Coulehan JL, Schulberg HC, Block MR, Madonia MJ, Rodrigues E. Treating depressed primary care patients improves their physical, mental, and social functioning. Arch Intern Med. 1997;157:1113–20. [PubMed] [Google Scholar]
- 54.Schafer JL. Analysis of incomplete multivariate data. London: Chapman and Hall; 1997. [Google Scholar]
- 55.Ferketich S. Aspects of item analysis. Res Nurs Health. 1991;14:165–8. doi: 10.1002/nur.4770140211. [DOI] [PubMed] [Google Scholar]
- 56.Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 7. Upper Saddle River: Prentice Hall; 2009. [Google Scholar]
- 57.Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- 58.Bollen KA, Long JS. Testing structural equation models. Newbury Park: Sage; 1993. [Google Scholar]
- 59.Cohen J. Statistical power analysis for the behavioral sciences. 2. New York: Academic Pr; 1988. [Google Scholar]
- 60.Kaplan CP. The Community Integration Questionnaire with new scoring guidelines: concurrent validity and need for appropriate norms. Brain Inj. 2001;15:725–31. doi: 10.1080/02699050010005913. [DOI] [PubMed] [Google Scholar]
- 61.Kuipers DP, Kendall M, Fleming J, Tate R. Comparison of the Sydney Psychosocial Reintegration Scale (SPRS) with the Community Integration Questionnaire (CIQ): psychometric properties. Brain Inj. 2004;18:161–77. doi: 10.1080/0269905031000149524. [DOI] [PubMed] [Google Scholar]
- 62.Gontkovsky ST, Russum P, Stokic DS. Comparison of the CIQ and CHART Short Form in assessing community integration in individuals with chronic spinal cord injury: a pilot study. NeuroRehabilitation. 2009;24:185–92. doi: 10.3233/NRE-2009-0467. [DOI] [PubMed] [Google Scholar]
- 63.Tate RL. A compendium of tests, scales and questionnaires: the practitioner’s guide to measuring outcomes after acquired brain impairment. New York: Psychology Pr; 2010. [Google Scholar]