Abstract
Background:
Visfatin is a new adipocytokine which is largely secreted by visceral adipose tissue and its effects in the development of diabetes and inflammatory reactions are similar to insulin. It acts synergistically with insulin in increasing glucose cellular uptake, stimulating glucose transfer to the muscle and adipose tissue, as well as in preventing hepatic glucose production. Its insulin-like effects are mediated through direct connection and activation of insulin receptors without any change or competition with the insulin.
Methods:
This case-control study was conducted among 64 women consisting of 32 diabetic patients, and 32 age-matched healthy controls. The case group consisted of 32 post-menopausal diabetic women, aged 45-65 years. Those patients were eligible who had a history of at least five years of type II diabetes, without any complications of diabetes, and who were treated only by oral glucose-lowering medications. Those individuals with C-reactive protein (CRP) test of 3+ and above were excluded from the study. Results were compared with age- and sex- matched controls.
Results:
Average visfatin level was significantly higher in diabetic patients than in controls (4.3 ± 1.06ng/dl vs. 3.15 ± 0.74ng/dl, respectively< 0.001).
The mean values of anthropometric indexes and lipid profile were not significantly different between diabetic patients and controls
Conclusion:
This study documented an inverse relationship between circulating level of visfatin and fasting blood glucose. This finding may suggest the role of increased visfatin level and increase in synthesis and secretion of the cytokines from adipocytes. These findings may be useful for primary and secondary preventive issues in diabetic and pre-diabetic individuals.
Keywords: Lipid profile, type II diabetes, visfatin
INTRODUCTION
It is well-documented that increase in adipose tissue, particularly visceral adipose, is strongly associated with cardiovascular risk, moreover it has an underlying role in the development of diabetes and metabolic syndrome.[1]
According to the World Health Organization, in recent years, 150 million people in the world are suffering from type II diabetes; it is estimated that this number increases to be doubled by 2025.[2] Today, it is no more limited to adults, and is seen in all age groups the age-adjusted mortality rate of diabetic people is 1.5 to 2.5 times higher than the general population.[3] In most of the cases, insulin resistance and type II diabetes are associated with obesity so that overweight and obesity are considered as the main causes of diabetes and insulin resistance.[4]
In addition to its important role in saving energy as triglycerides (TG), adipose tissue has a major role in secretion of various hormones such as leptin, adiponectin and visfatin, therefore it may activate insulin signals. Adipose tissue is an endocrine tissue secreting some proteins as adipokines mostly affecting lipid and glucose metabolism, as well as insulin resistance; whereas some of them as adiponectin have protective effect against insulin resistance.[5]
Visfatin is a new adipocytokine mainly secreted by visceral adipose tissue (VAT) with similar effects of insulin, and a possible role in development of diabetes and inflammatory reactions.[6,7] Experimental studies have confirmed the useful role of visfatin in mimicking the effects of insulin.[8] Its deficiency may be fatal in early embryonic periods of mice. It may also play a role in the inherited and acquired immune responses, colony enhancing, proliferation and maturation of B cells, as well as progression in autoimmune disease. Moreover, visfatin has pre-inflammatory properties and may enhance the concentrations of tumor necrosis factor alpha (TNF-α) and interleukin- 6 (IL-6). This hormone acts synergistically with insulin in increasing glucose cellular uptake, stimulating glucose transfer to the muscle and adipose tissue, as well as preventing from hepatic glucose production and its anti-diabetic insulin effect through insulin mimetic is documented.[9] Visfatin does its insulin-like effects through direct connection and activation of insulin receptors without any change or competition with the insulin.[10,11] Many clinical studies demonstrated the direct association of higher circulating levels of visfatin with body fat percentage, type II diabetes and obesity.[11,12]
Plasma visfatin concentrations increase with abdominal obesity and type II diabetes, it represents hypoglycemia effects with reducing glucose release from the hepatocytes, and it stimulates glucose usage in peripheral tissues.[13,14]
Furthermore, high concentration of plasma visfatin reduces after weight loss and it may be associated with resistance changes toward insulin over time.[15]
Although, some study have done in other side of world but because of high incidence of diabetes and different race and ethnicity in Iran this study is conducted to comparison serum visfatin concentrations in patients with type II diabetes and healthy controls.
METHODS
This case-control study was conducted among post-menopausal diabetic women, aged 45-65-years, referred to the Isfahan Diabetes Charity Center in Isfahan city, Iran. Those patients were eligible who had a history of at least 5 years of type II diabetes, without any complications of diabetes, and who were treated only by oral glucose-lowering medications. Those individuals with C-reactive protein (CRP) test of 3+ and above were excluded from the study. Results were compared with age- and sex- matched controls. Written informed consent was obtained from all participants. By considering a power of 80%, the sample size was calculated as 32 in each group.
After physical examination and anthropometric measurement, fasting venous blood was obtained; serum visfatin was measured through the standard kits using ELISA (Enzyme-linked immune sorbent assay) method with the sensitivity of 30 pg/ml via Human visfatin kit made by a Korean company (ADIPOGEN Inc.). Lipid profiles were measured by Pars Azmoon kit. All the tests were conducted automatically by HITACHI 911. The obtained data analyzed using software SPSS version 18.0 (SPSS, Chicago, IL., USA) and differences were considered significant when P<0.05 and statistical tests, tables and charts. The qualitative data was done using Fisher's exact test and quantitative data using student t-test. The weight changes measured by chi-square test and Pearson correlation test was used for the data correlation. Moreover, paired t-test was used for comparing serum visfatin concentration.
The study subjects filled in a questionnaire including age, height, weight, waist circumference, hip circumference, physical activity, kind of diet (Arbitrary diet, No diet an Under dietitian supervision); besides, their blood sample were taken for the blood tests.
RESULTS
The study participants consisted of 64 individuals including 32 diabetic patients, and 32 healthy controls. The mean age of the diabetic patients and controls was not significantly different (53.6 ± 4.3 years vs. 51.7 ± 5 years, respectively = 0.1).
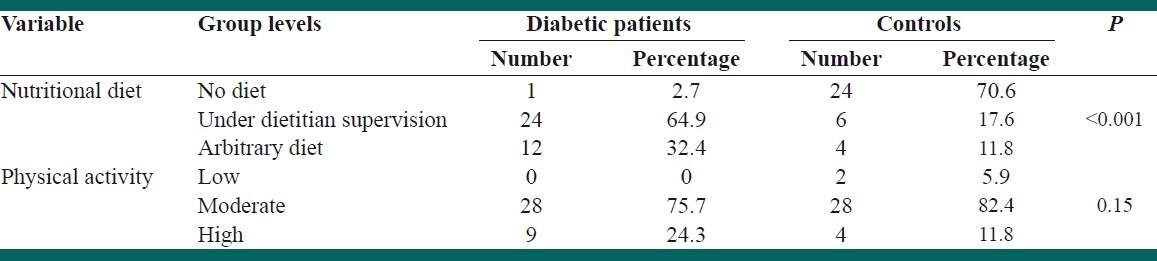
Table 1 shows the frequency distribution of the type of diet and physical activity in the two groups.
Table 1.
Frequency distribution of diet, exercise and physical activity in the two groups of the study
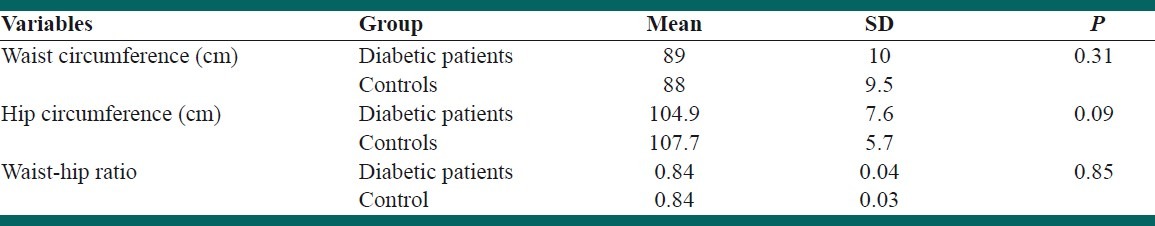
As presented in Table 2, the mean values of anthropometric measures were not significantly different between the diabetic group and controls.
Table 2.
Comparison of anthropometric measurements in diabetic patients and controls
As shown in Figure 1, the mean visfatin level of diabetic patients (4.3 ± 1.06 ng/dl) was significantly higher than controls (3.15 ± 0.74 ng/dl) (P< 0.001)
Figure 1.
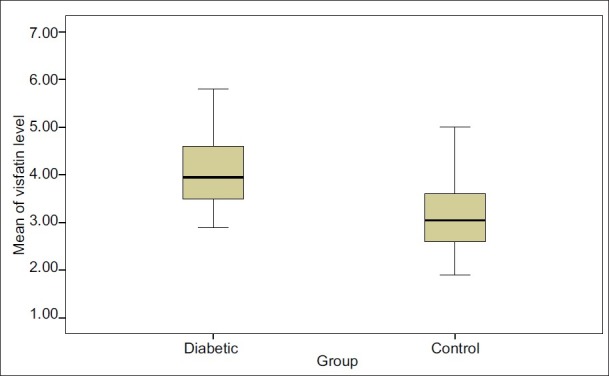
Comparison of the mean and range of confidence of visfatin in diabetic patients and controls
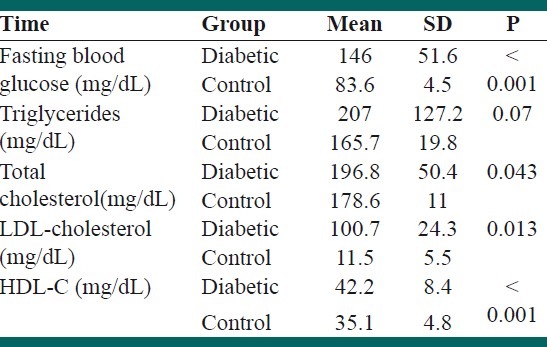
Comparison between the blood lipids (cholesterol, LDL and HDL) had a significant difference, triglyceride was different but they were not significant statistically. Mean LDL level in diabetic and control group was 100.7 ± 24.3 and 111.5 ± 5.1 respectively and the difference between the groups was significant (P < 0.001). Mean cholesterol in diabetic and control group was 196.8 ± 50.4 and 178.6 ± 11 respectively and it was a significant difference (P = 0.043) [Table 3].
Table 3.
Comparing the mean and standard deviation of the lipids between the two groups
DISCUSSION
This study mainly aimed to determine serum visfatin concentration in patients with type II diabetes. It documented an inverse relationship between circulating level of visfatin and fasting blood glucose. This finding is consistent with some previous studies.[7,14,16] Along with the inverse relationship of changes in fasting glucose and visfatin level in both groups despite non-significance results might suggest the role of visfatin in reducing blood glucose. This insulin-like effect may be resulted from an insulin receptor phosphorylation design, activation of signal transferring molecules inside the cells, as well as its role in NAD biosynthesis as phosphoribosyltransferase from nicotinamide (Nampt).[17,18]
Many endocrine factors, as insulin and glucagon are involved in regulation and controlling the blood glucose. In recent years, the importance of adipose tissue has been identified not only as the fat storage location in the body, but also as an endocrine organ which secrets adipocytokines, leptin, adiponectin, resisting, TNF-α, interleukin 6 (IL-6) and visfatin are samples of these cytokines which are involved in etiology of diabetes.[19,20]
These adipocytokines have provided an extensive network where each adipokine is in connection with the other and also affect other tissues and organs of the body. The network is involved in many biological actions such as insulin resistance, adipose metabolism and energy homeostasis through different paths.[20,21]
Visfatin concentration is approximately 10% of insulin concentration in fasting status and 3% in post-prandial status. Visfatin causes pre-adipocyte cells to become mature adipocytes.[6] Omega 3 increases the secretion of visfatin in patient with type II diabetes.[22]
Recent studies documented that visfatin has a role in activation of insulin receptors in different cells, enhanced glucose and lipogenics transferring in adipocyte of 3T3-L1 category or myositis L6 and decrease in glucose secretion by hepatocytes in vitro.[14] It may be secreted from the 3T3-L1 adipocytes, which are associated with endoplasmic reticulum and Golgi or micro-vesicles.[23] It is also reported that hyperglycemia may increase the synthesis of visfatin from the cultured adipocytes.[15]
According to these findings and the contradictions in the obtained findings, biological mechanisms of visfatin role have not been well identified in pathogenesis of type II diabetes. Besides, there are also controversial debates about the association of the level of the adipocytokines with weight status. While increased visfatin level is found in extreme and morbid obese individuals, and reduces after gastric banding surgery,[15] another study has reported lower levels of visfatin in obese persons.[24]
In type II diabetes, insulin resistance and obesity together cause mild to moderate hypertriglyceridemia and also cause reduction of HDL-C; usually, this dyslipidemia pattern is involved with excessive production of very low density lipoproteins (VLDL). Excessive production of TG-rich lipoproteins and its low clearance by lipoprotein lipase in diabetic patients may lead to hypertriglyceridemia. TG levels inversely are associated with HDL-C, and are considered as the carrier protein for cholesterol ester in transferring cholesterol from HDL-C to VLDL. Lipoproteins in diabetic patients may also change qualitatively and quantitatively. Common quantitative changes in diabetic people include increase in TG level and reduction in HDL-C level. However, LDL-C level in diabetic patients is similar to the normal population. For LDL-C, qualitative changes are more important than quantitative changes; i.e. the size and density of LDL-C and its oxidation would change, and it would make lipoprotein more atherogenic.[25,26]
Some study showed lipid profile is abnormal, and is characterized by modestly elevated LDL cholesterol, high triglyceride levels, and is associated with markedly increased cardiovascular risk among diabetic patients.[27]
The pattern of target lipid in type II diabetes is different from that of normal population, i.e. HDL-C>45mg/dL, LDL-C < 100mg/dL in men; the corresponding figure for women is >55mg/dL, and <150mg/dL, respectively. Considering that cholesterol value is higher than healthy people and LDL-C is lower than normal individuals and HDL-C is higher, and also regarding that TG value is higher in diabetic people, there would be disorder in synthesis of the lipid in diabetic patients.[28] The cause of TG increase can be due to dysfunction of lipase enzyme, which analyzes the chylomicrons. Lower LDL-C probably is associated with reduction of glucose consumption in the cell which causes free fatty acid (FFA) in blood, which would in turn prevent cholesterol synthesis, and may increase the VLDL production.[29]
CONCLUSION
This study suggested the role of increase the visfatin level and increase in synthesis and secretion of the cytokines from adipocytes. Probable cause of this can be due to more accumulation of adipocytes and/or faster differentiation and consequently synthesis and more secretion of serum levels to the patients. Furthermore, considering to the visfatin function which is similar to insulin, the likelihood of elevation of visfatin in diabetic people is a mechanism to compensate insulin deficiency or its inefficiency, so that it can regulate blood glucose level. However, considering that these studies have been new in association with the role of visfatin on type II diabetes, more studies are required in this regard to illustrate relevant mechanisms and role of other involved factors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Greenberg AS, Mc Daniel ML. Identifying the links between obesity, insulin resistance and beta cell function: Potential role of adipocyte-derived cytokines in the pathogenesis of type 2 diabetes. Eur J Clin Invest. 2002;32:s24–34. doi: 10.1046/j.1365-2362.32.s3.4.x. [DOI] [PubMed] [Google Scholar]
- 2.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995--2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 3.Jung CH, Rhee EJ, Kim SY, Shin HS, Kim BJ, Sung KC, et al. Associations between two single nucleotide polymorphisms of adiponection gene and coronary artery diseases. Endocr J. 2006;53:671–7. doi: 10.1507/endocrj.k06-020. [DOI] [PubMed] [Google Scholar]
- 4.Kleinman JC. Mortality among diabetics in - a national sample. Am J Epidemiol. 1988;128:389–401. doi: 10.1093/oxfordjournals.aje.a114979. [DOI] [PubMed] [Google Scholar]
- 5.Fantuzzi G. Adipose tissue, adipokin and inflammation. J Allergy Clin Immunol. 2005;115:911–9. doi: 10.1016/j.jaci.2005.02.023. quiz 920. [DOI] [PubMed] [Google Scholar]
- 6.Fukuhara A, Matsuda M, Nishizawa M, Segawa K, Tanaka M, Kishmoto K, et al. Visfatin: A protein secreted by visceral fat that mimics the effects of insulin. Science. 2005;21(307):366–7. doi: 10.1126/science.1097243. [DOI] [PubMed] [Google Scholar]
- 7.Chen MP, Chung FM, Chang DM, Tsai JC, Huang HF, Shin SJ, et al. Elevated plasma level of visfatin/pre-B cell colony-enhancing factor in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2006;91:295–9. doi: 10.1210/jc.2005-1475. [DOI] [PubMed] [Google Scholar]
- 8.Imai S. Nicotinamide phosphoribosyltransferase (Nampt): A link between NAD biology, metabolism, and diseases. Curr Pharm Des. 2009;15:20–8. doi: 10.2174/138161209787185814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bemdt J, Kloting N, Kralisch S, Kovacs P, Fasshauer M, Schon MR, et al. Plasma visfatin concentrations and fat depot-specific mRNA expression in humans. Diabetes. 2005;54:2911–6. doi: 10.2337/diabetes.54.10.2911. [DOI] [PubMed] [Google Scholar]
- 10.Bailey SD, Loredo-Osti JC, Lepage P, Faith J, Fontaine J, Desbiens KM, et al. Common polymorphisms in the promoter of the visfatin gene (PBEF1) influence plasma insulin levels. Diabetes. 2006;55:2896–902. doi: 10.2337/db06-0189. [DOI] [PubMed] [Google Scholar]
- 11.Varma V, Yao-Borengasser A, Rasouli N, Bodles AM, Phanavanh B, Lee MJ, et al. Human visfatin expression: Relationship to insulin sensitivity, intramyocellular lipids and inflammation. J Clin Endocrinol Metab. 2007;92:666–72. doi: 10.1210/jc.2006-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haider DG, Pleiner J, Francesconi M, Wiesinger GF, Müller M, Wolzt M. Exercise training lowers plasma visfatin concentrations in patients with type 1 diabetes. J Clin Endocrinol Metab. 2006;91:4702–4. doi: 10.1210/jc.2006-1013. [DOI] [PubMed] [Google Scholar]
- 13.Betowski J. Apelin and visfatin: unique “beneficial” adipokines upregulated in obesity. Med Sci Monit. 2006;12:RA112–9. [PubMed] [Google Scholar]
- 14.Fukuhara A, Matsuda M, Nishizawa M, Segawa K, Tanaka M, Kishimoto K, et al. Visfatin: A protein secreted by visceral fat that mimics the effects of insulin. Science. 2005;307:426–30. doi: 10.1126/science.1097243. [DOI] [PubMed] [Google Scholar]
- 15.Haider DG, Schindler K, Schaller G, Prager G, Wolzt M, Ludvik B. Increased plasma visfatin concentrations in morbidly obese subjects are reduced after gastric banding. J Clin Endocrinol Metab. 2006;91:1578–81. doi: 10.1210/jc.2005-2248. [DOI] [PubMed] [Google Scholar]
- 16.Haider DG, Schaller G, Kapiotis S, Maier C, Luger A, Wolzt M. The release of the adipocytokine visfatin is regulated by glucose and insulin. Diabetologia. 2006;49:1909–14. doi: 10.1007/s00125-006-0303-7. [DOI] [PubMed] [Google Scholar]
- 17.Revollo JR, Komer A, Mills KF, Satoh A, Wang T, Garten A, et al. Nampt/PBEF/Visfatin regulates insulin secretion in beta cells as a systemic NAD biosynthetic enzyme. Cell Metab. 2007;6:363–75. doi: 10.1016/j.cmet.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Revollo JR, Grimm AA, Imai S. The regulation of nicotinamide adenine dinucleotide biosynthesis by Nampt/PBEF/visfatin in mammals. Curr Opin Gastroenterol. 2007;23:164–70. doi: 10.1097/MOG.0b013e32801b3c8f. [DOI] [PubMed] [Google Scholar]
- 19.Ferris WF, Naran NH, Crowther NJ, Rheeder P, van der Merwe L, Chetty N. The relationship between insulin sensitivity and serum adiponectin levels in three population groups. Horm Metab Res. 2005;37:695–701. doi: 10.1055/s-2005-870580. [DOI] [PubMed] [Google Scholar]
- 20.Matsuzawa Y. Therapy insight: Adipokines in metabolic syndrome and related cardiovascular disease. Nat Clin Pract Cardiovasc Med. 2006;3:3542. doi: 10.1038/ncpcardio0380. [DOI] [PubMed] [Google Scholar]
- 21.Haffner SM, Gingerich RL, Miettinen H, Stern MP. Leptin concentrations in relation to overall adiposity and regional body fat distribution in Mexican Americans. Int J Obes Relat Metab Disord. 1996;20:904–8. [PubMed] [Google Scholar]
- 22.Hajianfar H, Hosseinzadeh MJ, Bahonar A, Mohammad K, Askari GR, Entezari MH, et al. The effect of omega3 on the serum visfatin concentration in patient with type II diabetes. JMRS. 2011;16:490–5. [PMC free article] [PubMed] [Google Scholar]
- 23.Tanaka M, Nozaki M, Fukuhara A, Segawa K, Aoki N, Matsuda M, et al. Visfatin is released from 3T3-L1 adipocytes via a non-classical pathway. Biochem Biophys Res Commun. 2007;359:194–201. doi: 10.1016/j.bbrc.2007.05.096. [DOI] [PubMed] [Google Scholar]
- 24.Pagano C, Pilon C, Olivieri M, Mason P, Fabris R, Serra R, et al. Reduced plasma visfatin/pre B-cell colony enhancing factor in obesity is not related to insulin resistance in humans. J Clin Endocrinol Metab. 2006;91:3165–70. doi: 10.1210/jc.2006-0361. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg IJ. Clinical review 124: Diabetic dyslipidemia: causes and consequences. J Clin Endocrinol Metab. 2001;86:965–71. doi: 10.1210/jcem.86.3.7304. [DOI] [PubMed] [Google Scholar]
- 26.Gotto A, Pownall H. The Manual of Lipid Disorders: Reducing the Risk for Coronary Heart Disease. 3rd ed. New York: Lippincott Williams and Wilkins; 2003. [Google Scholar]
- 27.Sadeghi M, Roohafza H, Shirani S, Poormoghadas M, Kelishadi R, Baghaii A, et al. Diabetes and associated cardiovascular risk factors in Iran: The Isfahan Healthy Heart Programme. Ann Acad Med Singapore. 2007;36:175–80. [PubMed] [Google Scholar]
- 28.Duan Y, Wu Z, Liu B. Relation of plasma glucose levels to serum lipids and apolipoproteins levels in middle and old age males. Hua Xi Yi Ke Da Xue Xue Bao. 2001;32:382–4. [PubMed] [Google Scholar]
- 29.Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, et al. Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1999;100:1134–46. doi: 10.1161/01.cir.100.10.1134. [DOI] [PubMed] [Google Scholar]


