Abstract
Background
Approximately 500,000 patients are discharged from U.S. hospitals against medical advice annually, but the associated risks are unknown.
Methods
We examined 148,810 discharges from an urban, academic health system between 7/1/2002 and 6/30/2008. Of these, 3,544 (2.4%) were discharged against medical advice and 80,536 (54.1%) were discharged home. We excluded inpatient deaths, transfers to other hospitals or nursing facilities, or discharges with home-care. Using adjusted and propensity score matched analyses, we compared 30-day mortality, 30-day readmission, and length of stay between discharges against medical advice and planned discharges.
Results
Discharge against medical advice was associated with higher mortality than planned discharge, after adjustment (ORadj = 2.05, 95% CI: 1.48–2.86), and in propensity-matched analysis (ORmatched = 2.46, 95% CI: 1.29 – 4.68). Discharge against medical advice was also associated with higher 30-day readmission after adjustment (ORadj 1.84; 95% CI 1.69 – 2.01), and in propensity-matched analysis (ORmatched 1.65, 95% CI: 1.46 – 1.87). Finally, discharges against medical advice had shorter lengths-of-stay than matched planned discharges (3.37 vs. 4.16 days, p <0.001).
Conclusions
Discharge against medical advice is associated with increased risk for mortality and readmission. In addition, discharges against medical advice have shorter lengths-of-stay than matched planned discharges, suggesting that the increased risks associated with discharge against medical advice are attributable to premature discharge.
INTRODUCTION
Approximately 500,000 patients are discharged from U.S. hospitals against medical advice each year.1 Discharge against medical advice has been associated with increased risk for readmission among VA medical inpatients,2 and in patients with asthma,3 acute myocardial infarction,4 or HIV.5 Studies have also demonstrated that patients discharged against medical advice are different from those with planned discharges: they are more likely to be younger1;3;4;6–10 male,1;3–6;8–11 lack private insurance,1;3;8–10;12 or have substance abuse2;6;8;9;12;13 or psychiatric diagnoses.4;6;8;12 Some studies have also reported less medical co-morbidity in patients discharged against medical advice.4;13 Because patients discharged against medical advice may be healthier than those with planned discharges, previous estimates that do not account for disease severity may have underestimated the risk of discharge against medical advice. It remains unknown whether discharge against medical advice is independently associated with increased risks of readmission or mortality among general medical inpatients.
When inpatients are considering discharge against medical advice, providers are obligated to obtain informed consent.14,15 A key element of informed consent is disclosure of risks. While providers may be able to estimate the baseline risk associated with the patient’s disease, there are few data to inform estimates of the increased risk associated with discharge against medical advice.
To determine the magnitude of the independent risk associated with discharge against medical advice, we compared outcomes among discharges against medical advice and planned discharges. Because we thought discharge against medical advice might mark admissions that ended prematurely, we also compared length-of-stay between discharges against medical advice and propensity score matched controls (planned discharges). We hypothesized that discharge against medical advice is associated with increased risk for both mortality and readmission among general medical inpatients, due primarily to premature discharge.
METHODS
Study Setting and Patients
Montefiore Medical Center is an urban academic medical center in the Bronx, NY, consisting of two hospitals (381 and 706 beds) affiliated with Albert Einstein College of Medicine. We extracted data on all general medical inpatients who survived to discharge in both hospitals from 7/1/02 through 6/30/08. We excluded patients transferred to another facility, discharged to skilled nursing facilities, or requiring home-care services, because differences between such patients and those discharged against medical advice might confound our analysis. Discharges who left the hospital without notifying nursing staff were also excluded. In addition, because many patients had more than one discharge during the study period, we use discharge rather than patient, as our unit of analysis. Montefiore’s Institutional Review Board approved this study.
Study Design
We conducted a retrospective cohort study comparing risks of mortality and readmission between discharges against medical advice and planned discharges. To address the threat of confounding, in which discharges against medical advice might be different than planned discharges, we performed both logistic regression modeling, adjusting for covariates associated with the two outcomes, and propensity score matching, adjusting for patient factors associated with discharge against medical advice. Clinical data were extracted from a replicate of Montefiore’s Clinical Information System using health care surveillance software (Clinical Looking Glass,™ Emerging Health Information Technology, Yonkers, NY).
Outcomes
30-day mortality was calculated from the date of admission, and analyzed both as a dichotomous and a time-to-event variable. Readmission was defined as any admission for any reason, within 30 days of discharge, to either hospital, and analyzed both as a dichotomous and a time-to-event variable. Mortality data were extracted from the social security death registry. Length of stay was analyzed as a continuous variable, as has been done previously.16–19
Main independent variable: discharge against medical advice
Type of discharge (against medical advice or planned) was determined by a disposition code assigned by nursing staff. Planned discharges included all discharges designated “discharged home, self-care.”
Covariates: patient factors
Because we expected that discharges against medical advice are different than planned discharges, and that those differences would confound our analyses, we extracted data on several patient factors for use in logistic and propensity score adjusted models. Patient characteristics included: age, sex, race/ethnicity, insurance (categorized as Medicare, Medicaid, Commercial, or Self-pay), history of substance abuse or psychiatric illness, ICD-9 code diagnoses from previous admissions and outpatient visits, and primary discharge diagnoses from the current admission. We used ICD-9 codes for alcohol or substance abuse (ICD-9 305.xx) or a positive urine toxicology test in the 10 years prior to the admission, to indicate substance abuse, and ICD-9 codes for schizophrenia, bipolar, depression, paranoia, neurosis, or personality disorder (ICD-9 295.xx-298.xx and 300.xx-301.xx) in the 10 years prior to the admission to indicate psychiatric illness.
For each discharge we calculated two common co-morbidity indices as candidates for inclusion in propensity score and adjustment models: the Charlson co-morbidity score20 and number of Elixhauser comorbidities.21 Albumin and creatinine values were also used as surrogates for overall illness severity,18;19;22–24 because they are useful in quantifying risk.25 In addition, we calculated the Laboratory-based Acute Physiology Score (LAPS) to measure severity of illness.26 When combined with measures of co-morbidity, the LAPS score accounts for significant variance in inpatient mortality (C-statistic 0.88 – 0.91).26;27 LAPS was calculated using 14 common laboratory values, and analyzed as a continuous variable.
To create diagnosis variables, each discharge’s primary ICD-9 code was classified using the Agency for Healthcare Research and Quality system.28 To adjust for diagnoses associated with discharge against medical advice, the proportion of discharges against medical advice was calculated for each diagnosis classification group. The five diagnosis groups with the highest proportion of patients discharged against medical advice (substance abuse, alcohol abuse, medication poisoning, sickle cell disease, and HIV) were individually considered for inclusion in adjustment and propensity score models. To adjust for common admission diagnoses, the diagnosis groups that represent the 10 most frequent reasons for hospitalization in the U.S.29 (congestive heart failure, chest pain, myocardial infarction, pneumonia, asthma/chronic obstructive pulmonary disease (COPD), other coronary disease, diabetes, arrhythmia, sepsis, and gastrointestinal bleeding) were also individually considered for inclusion in the models.
Propensity Score Matching
Our propensity score matched analysis focused on covariates potentially associated with discharge against medical advice, readmission, mortality, or all of these. First, using all admissions discharged to home, a propensity score for being discharged against medical advice was calculated for each discharge using a non-parsimonious logistic regression model.30;31 Variables used in the propensity score model included those likely to be associated with discharge against medical advice (sex, race/ethnicity, insurance type, substance abuse or psychiatric illness, and diagnoses associated with discharge against medical advice), and those likely to be associated with readmission or mortality (age, admission albumin, admission creatinine, Charlson score, Elixhauser diagnoses, LAPS, and common diagnoses). Then, for each discharge against medical advice, one propensity score matched control (planned discharge) was selected using a nearest neighbor greedy match protocol without replacement.32 To minimize matching bias, data were randomly sorted prior to matching. In sensitivity analyses, the matching protocol and subsequent analysis was repeated after different random sorts, and the estimated association between discharge against medical advice and outcomes did not change.
Of 3,544 discharges against medical advice, 13.7% were missing the albumin value, and 1.9% were missing the creatinine value. Of 80,536 planned discharges, 13.8% were missing albumin, and 0.9% were missing creatinine. So that each of these would have a calculable propensity score and be eligible for matching, the missing albumin and creatinine values were imputed at the median for the study population (4.0 for albumin, and 1.0 for creatinine). Sensitivity analyses excluding discharges with imputed values did not change the estimated associations between discharge against medical advice and outcomes.
Statistical Analysis
Discharges against medical advice and planned discharges were first compared with respect to sociodemographic characteristics and measures of co-morbidity and illness severity, using t-tests, Mann-Whitney, or chi-squared tests. To assess univariate associations between discharge against medical advice and both 30-day mortality and 30-day readmission, we compared rates of these outcomes between discharge groups using chi-squared tests.
Unmatched Analysis of Readmission and Mortality
To assess the independent association between discharge against medical advice and outcomes, we constructed logistic regression models for each outcome using the unmatched cohorts. First, we constructed an unadjusted model including only discharge against medical advice as an independent variable. Then, we constructed a covariate and propensity score adjusted model. The above covariates were considered candidates for inclusion, and propensity score was forced into this model. We chose variables for inclusion in a backwards, stepwise fashion, and included those that were independently associated with the outcome (Wald-statistic p < 0.20). Variables were excluded if they were co-linear with other independent variables.
Matched Analysis of Readmission and Mortality
To adjust for variables unbalanced after propensity score matching, we used conditional logistic regression for a third set of models. We chose variables for inclusion in a backwards, stepwise fashion including those that were independently associated with the outcome (Wald-statistic p < 0.20), and excluding those that were co-linear with other independent variables. Because the matched cohorts were similar at admission, which makes comparisons of outcomes meaningful, we also plotted time to mortality and time to readmission for discharges against medical advice and planned discharges using Kaplan-Meier methods, and compared them using log-rank tests.
In post-hoc analyses of the matched cohorts, we assessed the association between discharge against medical advice and mortality in specific subgroups defined by sex, race/ethnicity, age (≤65 v >65), insurance status, Charlson score, LAPS and HIV serostatus. A separate univariate conditional logistic regression model was constructed for each outcome and subgroup, with discharge against medical advice as the single independent variable33
Matched Analysis of Length of Stay
Length of stay was not included as a variable in the adjustment or propensity score regression models because we theorized that the shorter Length of stay associated with discharge against medical advice might cause worse outcomes, and if on the causal pathway, should not be included in adjustment models. We also did not compare length of stay in the unmatched cohorts, because the patient groups were dissimilar on admission. Instead, we compared length of stay between discharges against medical advice and propensity score matched controls (planned discharges) using the Wilcoxon rank-sum test.
STATA/IC software, version 10.0, (StataCorp, College Station, TX) was used for all statistical analysis and data management.
RESULTS
Study Population
Of 148,810 discharges, 5,285 (3.6%) died in the hospital, 9,320 (6.3%) were transferred to another hospital, 23,926 (16.1%) were discharged to a skilled nursing facility, 26,178 (17.6%) required home-care services and 21 (0.01%) left the hospital without notifying nursing staff; these were all excluded. There were 3,544 (2.4%) discharges against medical advice and 80,536 (54.1%) planned discharges. The five diagnosis groups with the highest proportion of discharges against medical advice were: alcohol-related (16.5% discharged against medical advice), substance abuse (14.7% discharged against medical advice), other medication poisoning (11.0% discharged against medical advice), sickle cell disease diagnosis (9.0% discharged against medical advice), and HIV-related (8.4% discharged against medical advice).
Discharges against medical advice were younger, and more likely to be male, have Medicaid as primary insurance, have a history of substance abuse or psychiatric disease, and have higher Charlson and LAPS scores (Table 1).
Table 1.
Characteristics of Discharges Against Medical Advice and Planned Discharges
| Characteristic | All Patients (n = 84,080) |
Discharged AMA (n = 3,544) |
Planned Discharge (n = 80,536) |
p value |
|---|---|---|---|---|
| Age | 57.8 ± 17.0 | 48.7 ± 15.4 | 58.2 ± 17.0 | <0.001 |
| Male | 36,980 (44.0) | 2225 (62.8) | 34,755 (43.1) | <0.001 |
| Race | ||||
| White | 15,860 (18.9) | 625 (17.6) | 15,235 (18.9) | 0.06 |
| Black | 29,492 (35.1) | 1289 (36.4) | 28,203 (35.0) | 0.10 |
| Hispanic | 33,084 (39.3) | 1461 (41.2) | 31,623 (39.3) | 0.02 |
| Other/Unknown | 5,644 (6.7) | 169 (4.8) | 5475 (6.8) | <0.001 |
| Insurance | ||||
| Medicare | 31,640 (37.6) | 924 (26.1) | 30,716 (38.1) | <0.001 |
| Medicaid | 30,058 (35.7) | 2137 (60.3) | 27,921 (34.7) | <0.001 |
| Commercial | 21,695 (25.8) | 441 (12.4) | 21,254 (26.4) | <0.001 |
| Self | 685 (0.8) | 42 (1.2) | 643 (0.8) | 0.01 |
| History of substance abuse | 11,365 (13.5) | 1344 (37.9) | 10,021 (12.4) | <0.001 |
| History of psychiatric illness | 12,041 (14.3) | 924 (26.1) | 11,117 (13.8) | <0.001 |
| Charlson score | 1.79 ± 2.01 | 2.27 ± 2.53 | 1.77 ± 1.98 | <0.001 |
| # Elixhauser diagnoses | 2.26 ± 1.53 | 2.31 ± 1.63 | 2.26 ± 1.53 | 0.23 |
| Admission albumina | 3.95 ± 0.52 | 3.86 ± 0.65 | 3.95 ± 0.52 | <0.001 |
| Admission creatinineb | 1.0 (0.8 – 1.3) | 0.9 (0.7 – 1.3) | 1.0 (0.8 – 1.3) | <0.001 |
| LAPS scorec | 18.6 ± 14.7 | 19.5 ± 16.1 | 18.6 ± 14.6 | 0.13 |
| Diagnoses, No.(%) | All Patients (n = 84,080) |
Discharged AMA (n = 3544) |
Planned Discharge (n = 80,536) |
p value |
|---|---|---|---|---|
| Diagnoses associated with discharge AMAa | ||||
| Substance abuse | 136 (0.2) | 20 (0.6) | 116 (0.1) | <0.001 |
| Alcohol abuse | 1098 (1.3) | 248 (7.0) | 850 (1.1) | <0.001 |
| Medication poisoning | 881 (1.0) | 120 (3.4) | 761 (0.9) | <0.001 |
| Sickle Cell Crisis | 1998 (2.4) | 191 (5.4) | 1807 (2.2) | <0.001 |
| Human Immunodeficiency Virus | 1920 (2.3) | 267 (7.5) | 1653 (2.0) | <0.001 |
| Common discharge diagnosesb | ||||
| Congestive Heart Failure | 5501 (6.5) | 155 (4.4) | 5346 (6.6) | <0.001 |
| Chest pain | 7877 (9.4) | 263 (7.4) | 7614 (9.4) | <0.001 |
| Myocardial infarction | 2100 (2.5) | 62 (1.7) | 2038 (2.5) | 0.004 |
| Pneumonia | 3163 (3.8) | 75 (2.1) | 3088 (3.8) | <0.001 |
| Asthma/Chronic Obstructive Pulmonary Disease | 4847 (5.8) | 158 (4.5) | 4689 (5.8) | 0.00 |
| Other coronary disease | 5100 (6.1) | 155 (4.4) | 4945 (6.1) | <0.001 |
| Diabetes | 2943 (3.5) | 130 (3.7) | 2813 (3.5) | 0.58 |
| Arrythmia | 3742 (4.4) | 89 (2.5) | 3653 (4.5) | <0.001 |
| Sepsis | 614 (0.7) | 39 (1.1) | 575 (0.7) | 0.01 |
| Gastrointestinal bleeding | 1298 (1.5) | 49 (1.4) | 1249 (1.5) | 0.43 |
continuous variables reported as mean ± standard deviation, compared using t-tests with unequal variances
dichotomous variables reported as number (percent), compared using chi-squared tests
creatinine reported as median (inter-quartile range), compared using Wilcoxon rank-sum
13.8% of discharges did not have an albumin value available and were imputed as normal
0.8% of discharges did not have a creatinine value available and were imputed as normal
Laboratory-based Acute Physiology Score
The five diagnoses with highest proportion of discharge AMA
The ten most frequent diagnoses among medical inpatients reported in the U.S.
Matched Study Population
Of 3,544 discharges against medical advice, 3,533 had a propensity score calculated and were matched with 3,533 eligible planned discharges. The propensity score model performed well at predicting discharge against medical advice (C-statistic: 0.78). After matching, discharges against medical advice and planned discharges were similar with respect to age, sex, race/ethnicity, insurance type, admission albumin, admission creatinine, Charlson score, number of Elixhauser diagnoses, LAPS score, substance abuse and psychiatric illness history, and discharge diagnoses (Table 2).
Table 2.
Characteristics of Matched Discharges AMA and Planned Discharges
| Characteristic | Discharged AMA (n = 3533) |
Planned Discharge (n = 3533) |
p value |
|---|---|---|---|
| Age | 48.7 ± 15.4 | 48.7 ± 15.7 | 0.89 |
| Male | 2220 (62.8) | 2188 (61.9) | 0.43 |
| Race | |||
| White | 621 (17.6) | 604 (17.1) | 0.59 |
| Black | 1284 (36.3) | 1304 (36.9) | 0.62 |
| Hispanic | 1459 (41.3) | 1482 (41.9) | 0.58 |
| Other/Unknown | 169 (4.8) | 143 (4.0) | 0.13 |
| Insurance | |||
| Medicare | 924 (26.1) | 952 (26.9) | 0.45 |
| Medicaid | 2126 (60.2) | 2057 (58.2) | 0.09 |
| Commercial | 441 (12.5) | 480 (13.6) | 0.17 |
| Self | 42 (1.2) | 44 (1.2) | 0.83 |
| History of substance abuse | 1337 (37.8) | 1384 (39.2) | 0.25 |
| History of psychiatric illness | 924 (26.1) | 918 (26.0) | 0.87 |
| Charlson score | 2.27 ± 2.53 | 2.28 ± 2.51 | 0.46 |
| # Elixhauser diagnoses | 2.31 ± 1.63 | 2.34 ± 1.59 | 0.30 |
| Admission albumina | 3.86 ± 0.65 | 3.86 ± 0.62 | 0.89 |
| Admission creatinineb | 0.9 (0.7 – 1.3) | 1.0 (0.8 – 1.3) | 0.13 |
| LAPS Scorec | 19.5 ± 16.1 | 19.7 ± 16.0 | 0.60 |
| Diagnoses, No.(%) | Discharged AMA (n = 3533) |
Planned Discharge (n = 3533) |
p value |
|---|---|---|---|
| Diagnoses associated with discharge AMAa | |||
| Substance abuse | 20 (0.6) | 22 (0.6) | 0.76 |
| Alcohol abuse | 248 (7.0) | 263 (7.4) | 0.49 |
| Medication poisoning | 120 (3.4) | 127 (3.6) | 0.65 |
| Sickle Cell Crisis | 190 (5.4) | 184 (5.2) | 0.75 |
| Human Immunodeficiency Virus | 263 (7.4) | 268 (7.6) | 0.82 |
| Common discharge diagnosesb | |||
| Congestive Heart Failure | 155 (4.4) | 145 (4.1) | 0.55 |
| Chest pain | 260 (7.4) | 299 (8.5) | 0.09 |
| Myocardial infarction | 61 (1.7) | 62 (1.7) | 0.93 |
| Pneumonia | 75 (2.1) | 77 (2.2) | 0.87 |
| Asthma/Chronic Obstructive Pulmonary Disease | 158 (4.5) | 161 (4.6) | 0.86 |
| Other coronary disease | 154 (4.4) | 147 (4.2) | 0.68 |
| Diabetes | 130 (3.7) | 144 (4.1) | 0.39 |
| Arrythmia | 89 (2.5) | 99 (2.8) | 0.46 |
| Sepsis | 39 (1.1) | 36 (1.0) | 0.73 |
| Gastrointestinal bleeding | 49 (1.4) | 36 (1.0) | 0.16 |
continuous variables reported as mean ± standard deviation, compared using t-tests
dichotomous variables reported as number (percent), compared using chi-squared tests
creatinine reported as median (inter-quartile range), compared using Wilcoxon rank-sum
13.4% of discharges did not have an albumin value available and were imputed as normal
1.6% of discharges did not have an albumin value available and were imputed as normal
Laboratory-based Acute Physiology Score
The five diagnoses with highest proportion of discharge AMA
The ten most frequent diagnoses among medical inpatients reported in the U.S.
Mortality
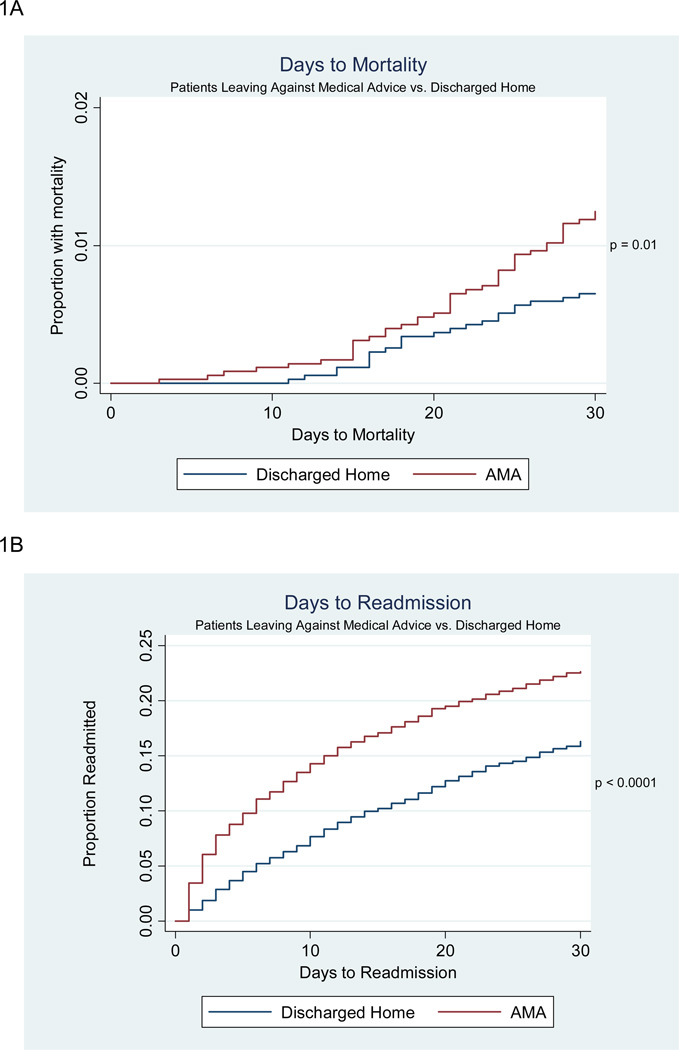
In unmatched analysis, 30-day mortality was significantly higher among discharges against medical advice than planned discharges (1.3% vs. 0.7%, p <0.001), and remained higher after adjustment for propensity score and sociodemographic and clinical characteristics (ORadj = 2.05, 95% CI: 1.48–2.86, C-statistic: 0.84). In matched analysis, more discharges against medical advice died than planned discharges (45 vs. 23, p = 0.007). After adjustment for covariates unbalanced after matching, discharge against medical advice remained associated with an increased risk of mortality (ORmatched = 2.46, 95% CI: 1.29 – 4.68) (Table 3).Time to 30-day mortality for the matched populations are presented in Figure 1A.
Table 3.
Associations between Discharge AMA and 30-day Mortality & 30-day Readmission
| Model | Mortality OR (95% CI) |
Readmission OR (95% CI) |
|---|---|---|
| Unadjusted | 1.92 (1.41 – 2.61) | 2.58 (2.38 – 2.79) |
| Propensity score & covariate adjusted | 2.05 (1.48 – 2.86)a | 1.84 (1.69 – 2.01)b |
| Propensity score matched & covariate adjusted | 2.46 (1.29 – 4.68)c | 1.65 (1.46 – 1.87)c |
Adjusted for propensity score, age, sex, race/ethnicity, insurance, history of substance abuse, Charlson co-morbidity score, laboratory-based acute physiology score (LAPS), and discharge diagnosis
Adjusted for propensity score, age, sex, race/ethnicity, insurance, history of substance abuse, history of psychiatric disease, Charlson co-morbidity score, laboratory-based acute physiology score (LAPS), and discharge diagnosis
Adjusted for covariates unbalanced after matching: race/ethnicity, insurance, creatinine, and discharge diagnosis
Figure 1.
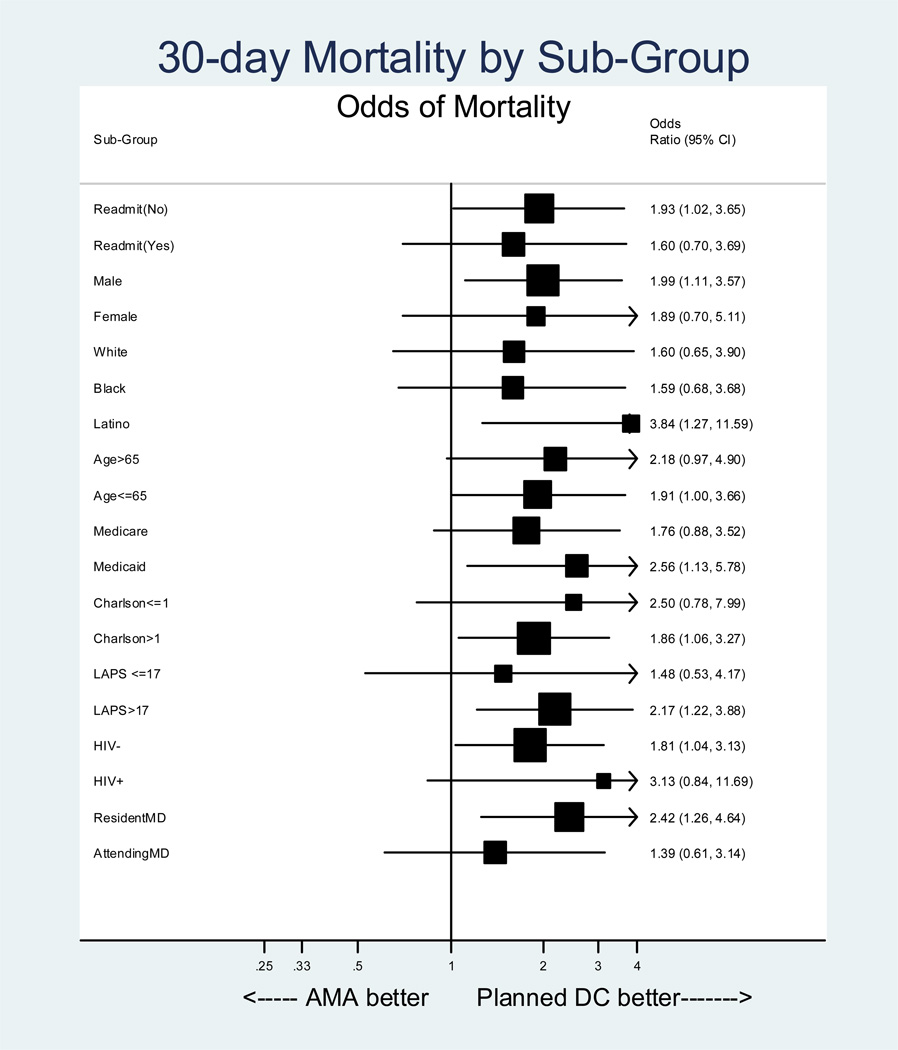
In post-hoc analysis (Figure 2), we observed several groups with a pronounced increased risk of mortality associated with discharge against medical advice, including Latino patients (OR = 3.84, 95% CI: 1.27 – 11.59), patients with Medicaid (OR = 2.56, 95% CI: 1.13 – 5.78), patients with LAPS scores above the median (OR = 2.17, 95% CI: 1.22 – 3.88), and patients with a resident as their primary physician (OR = 2.42, 95% CI: 1.26 – 4.64). Strikingly, however, the increased risk we observed was present in all subgroups.
Figure 2.
Readmission
In unmatched analysis, 30-day readmission was significantly higher among discharges against medical advice than planned discharges (24.7% vs. 11.3%, p <0.001) and remained after adjustment (ORadj = 1.84, 95% CI: 1.69–2.01, C-statistic: 0.72) (Table 3). In matched analysis, more discharges against medical advice were readmitted than matched planned discharges (876 vs. 586, p <0.001). After adjustment for covariates unbalanced after matching, discharge against medical advice remained associated with an increased risk of readmission (ORadj = 1.65, 95% CI: 1.46 – 1.87). The median number of days to readmission for discharges against medical advice was 6 (IQR 2–13) versus 11 (IQR 4–19 days) for planned discharges (p < 0.0001, Figure 1B).
Length of stay
Length of stay was significantly shorter for discharges against medical advice compared to matched planned discharges (3.37 ± 4.20 vs. 4.16 ± 3.77 days, p <0.001).
DISCUSSION
In a large, carefully controlled retrospective study of 148,000 inpatients at an urban academic medical center, we found that discharge against medical advice was associated with approximately double the risk of death within 30 days. In addition, we found a strong and significantly increased risk for readmission associated with discharge against medical advice. When hospitalized patients are considering leaving the hospital against medical advice, they are often asked to sign waivers attesting that they have been informed of, and understand, the risks associated with discharge against medical advice.34 Our findings should help providers to estimate the increased risk associated with leaving the hospital against medical advice. We are the first to report the increased mortality risk of discharge against medical advice among general medical patients. Though previous research demonstrated an association between discharge against medical advice and mortality among patients with acute myocardial infarction,4 one large study of general medical patients in the Veteran’s Affairs (VA) system failed to find an increased risk of mortality among patients discharged against medical advice (HR = 1.10).2 However, because discharges against medical advice may be less severely ill than planned discharges, observational studies may be biased toward failing to find the harm associated with discharge against medical advice. After careful measurement of comorbidity and disease severity, and appropriate adjustment, we found a large and significantly increased risk of mortality among discharges against medical advice.
There are multiple potential mechanisms by which discharge against medical advice may increase mortality and readmission. In some cases, discharge against medical advice may cause an admission to end prematurely, before appropriate inpatient treatment is completed. Supporting this hypothesis, we found that discharges against medical advice have shorter lengths-of-stay than matched planned discharges. For some patients discharged against medical advice, inpatient treatment of acute medical issues may be incomplete, and early discharge may result in worsening of the acute condition and death. Further, the short median time to readmission (6 days) after discharge against medical advice suggests that patients discharged against medical advice require, and in some cases return to obtain, additional inpatient treatment.
Although the risks associated with discharge against medical advice were seen in all subgroups in this study, the increased risks were most pronounced in Latinos, patients with Medicaid, patients with higher acute physiology scores, and patients cared for by residents. The increased risk seen in Latino patients suggests that, because of a language barrier, communication of the risks associated with discharge against medical advice may be suboptimal. The increased risk seen in patients with Medicaid suggests that these patients, after discharge against medical advice, may have difficulty in obtaining appropriate outpatient follow-up care, increasing the risk of poor outcome. The increased risks seen in patients with higher acute physiology scores suggests that, the higher the acuity of illness, the higher the risk of poor outcomes after discharge against medical advice. Finally, the increased risks seen in patients cared for by residents suggests that physicians in training may not be able to accurately assess and communicate the risks associated with discharge against medical advice.
Although some patients discharged against medical advice may have left the hospital prematurely, it is also possible that the increased risks associated with discharge against medical advice result from poor post-discharge follow-up. Lack of trust and poor patient/provider communication have been associated with discharge against medical advice34;35 and may be markers for poor outpatient treatment adherence, decreased utilization of necessary healthcare services, or both. It may be that the VA study of general medical patients failed to find harm associated with discharge against medical advice because of excellent outpatient follow-up in the VA system.2
Despite the strengths of our study, it has some limitations. Because the study was observational, there may be unmeasured differences between the groups resulting in residual confounding. To minimize this possibility, we used both logistic regression and propensity score matching to address confounding, and obtained adjustment variables from a wide range of domains. These included factors known to be associated with discharge against medical advice, clinical diagnoses that we found associated with discharge against medical advice, and measures of co-morbidity and severity of illness known to be associated with mortality. Both the logistic regression model and the propensity score matching model performed well, and yielded similar results, suggesting that residual confounding was minimized. Next, we were only able to ascertain readmissions within the Montefiore hospital system and it is unclear if discharges against medical advice might be more (or less) likely to be readmitted outside the Montefiore system. Lastly, the data used for this analysis were from a single institution located in the Bronx, a borough of New York City with high rates of poverty and substance abuse, and the results may not be generalizable.
In sum, we found that discharge against medical advice is associated with approximately double the risk of 30-day mortality, and significantly increased risk of readmission. This excess mortality risk is seen in all subgroups. In addition, discharges against medical advice have shorter lengths-of-stay than planned discharges, suggesting that the increased risk associated with discharge against medical advice may be attributable to premature discharge. If discharge against medical advice cannot be avoided, patients who are considering leaving against medical advice should be advised of these increased risks.
Acknowledgements
We are grateful to the Works in Progress Study Group of the Einstein/Montefiore Division of General Internal Medicine for valuable feedback.
Financial support: This work was supported by the CTSA Grant UL1 RR025750 and KL2 RR025749 and TL1 RR025748 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the Clinical Investigation Core of the Center for AIDS Research at the Albert Einstein College of Medicine and Montefiore Medical Center, funded by the National Institutes of Health (NIH P30 AI51519). Drs. Arnsten and Nahvi were also supported by NIH R25 DA023021.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of this research were presented at the Annual Meeting of the Society of General Internal Medicine, April 2010, Minneapolis, Minnesota and at the Annual Meeting of the Society of Hospital Medicine, April 2010, Washington DC.
Reference List
- 1.Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am JPublic Health. 2007;97:2204–2208. doi: 10.2105/AJPH.2006.100164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25:926–929. doi: 10.1007/s11606-010-1371-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baptist AP, Warrier I, Arora R, Ager J, Massanari RM. Hospitalized patients with asthma who leave against medical advice: characteristics, reasons, and outcomes. J Allergy Clin Immunol. 2007;119:924–929. doi: 10.1016/j.jaci.2006.11.695. [DOI] [PubMed] [Google Scholar]
- 4.Fiscella K, Meldrum S, Barnett S. Hospital discharge against advice after myocardial infarction: deaths and readmissions. Am J Med. 2007;120:1047–1053. doi: 10.1016/j.amjmed.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 5.Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O'Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167:633–637. [PMC free article] [PubMed] [Google Scholar]
- 6.Seaborn MH, Osmun WE. Discharges against medical advice: a community hospital's experience. Can J Rural Med. 2004;9:148–153. [PubMed] [Google Scholar]
- 7.Armenian SH, Chutuape MA, Stitzer ML. Predictors of discharges against medical advice from a short-term hospital detoxification unit. Drug Alcohol Depend. 1999;56:1–8. doi: 10.1016/s0376-8716(99)00027-7. [DOI] [PubMed] [Google Scholar]
- 8.Myers RP, Shaheen AA, Hubbard JN, Kaplan GG. Characteristics of Patients With Cirrhosis Who Are Discharged From the Hospital Against Medical Advice. Clin Gastroenterol Hepatol. 2009 doi: 10.1016/j.cgh.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Saitz R, Ghali WA, Moskowitz MA. Characteristics of patients with pneumonia who are discharged from hospitals against medical advice. Am J Med. 1999;107:507–509. doi: 10.1016/s0002-9343(99)00262-4. [DOI] [PubMed] [Google Scholar]
- 10.Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med. 1998;13:568–571. doi: 10.1046/j.1525-1497.1998.00169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang SW, Li J, Gupta R, Chien V, Martin RE. What happens to patients who leave hospital against medical advice? CMAJ. 2003;168:417–420. [PMC free article] [PubMed] [Google Scholar]
- 12.Fiscella K, Meldrum S, Franks P. Post partum discharge against medical advice: who leaves and does it matter? Matern Child Health J. 2007;11:431–436. doi: 10.1007/s10995-007-0194-3. [DOI] [PubMed] [Google Scholar]
- 13.Pages KP, Russo JE, Wingerson DK, Ries RK, Roy-Byrne PP, Cowley DS. Predictors and outcome of discharge against medical advice from the psychiatric units of a general hospital. Psychiatr Serv. 1998;49:1187–1192. doi: 10.1176/ps.49.9.1187. [DOI] [PubMed] [Google Scholar]
- 14.Berger JT. Discharge against medical advice: ethical considerations and professional obligations. J Hosp Med. 2008;3:403–408. doi: 10.1002/jhm.362. [DOI] [PubMed] [Google Scholar]
- 15.Farber Post L, Blustein J, Dubler NN. Handbook for Health Care Ethics Committees. New York, NY: Johns Hopkins University Press; 2006. [Google Scholar]
- 16.Craig DE, Hartka L, Likosky WH, Caplan WM, Litsky P, Smithey J. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med. 1999;130:355–359. doi: 10.7326/0003-4819-130-4-199902161-00005. [DOI] [PubMed] [Google Scholar]
- 17.Bellet PS, Whitaker RC. Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges. Pediatrics. 2000;105:478–484. doi: 10.1542/peds.105.3.478. [DOI] [PubMed] [Google Scholar]
- 18.Meltzer D, Manning WG, Morrison J et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137:866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 19.Southern WN, Berger MA, Bellin EY, Hailpern SM, Arnsten JH. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874. doi: 10.1001/archinte.167.17.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Hollenbeck BK, Miller DC, Taub DA et al. The effects of adjusting for case mix on mortality and length of stay following radical cystectomy. J Urol. 2006;176:1363–1368. doi: 10.1016/j.juro.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 23.Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Height loss in older men: associations with total mortality and incidence of cardiovascular disease. Arch Intern Med. 2006;166:2546–2552. doi: 10.1001/archinte.166.22.2546. [DOI] [PubMed] [Google Scholar]
- 24.Maraldi C, Volpato S, Kritchevsky SB, et al. Impact of inflammation on the relationship among alcohol consumption, mortality, and cardiac events: the health, aging, and body composition study. Arch Intern Med. 2006;166:1490–1497. doi: 10.1001/archinte.166.14.1490. [DOI] [PubMed] [Google Scholar]
- 25.Goldwasser P, Feldman J. Association of serum albumin and mortality risk. J Clin Epidemiol. 1997;50:693–703. doi: 10.1016/s0895-4356(97)00015-2. [DOI] [PubMed] [Google Scholar]
- 26.Escobar GJ, Greene JD, Scheirer P, Gardner MN, Draper D, Kipnis P. Risk-adjusting hospital inpatient mortality using automated inpatient, outpatient, and laboratory databases. Med Care. 2008;46:232–239. doi: 10.1097/MLR.0b013e3181589bb6. [DOI] [PubMed] [Google Scholar]
- 27.van WC, Escobar GJ, Greene JD, Forster AJ. The Kaiser Permanente inpatient risk adjustment methodology was valid in an external patient population. J Clin Epidemiol. 2010;63:798–803. doi: 10.1016/j.jclinepi.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 28.Clinical Classifications Software (CCS) Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Quality and Research (AHRQ); [Google Scholar]
- 29.Healthcare Cost and Utilization Project (HCUP) website Of the Agency for Healthcare Quality and Research (AHRQ) [accessed 2/28/07]; http://hcup.ahrq.gov/HCUPnet.
- 30.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 31.D'Agostino RB, Jr, D'Agostino RB., Sr Estimating treatment effects using observational data. JAMA. 2007;297:314–316. doi: 10.1001/jama.297.3.314. [DOI] [PubMed] [Google Scholar]
- 32.PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching. Boston College School of Economics; 2003. [Google Scholar]
- 33.METAN: Stat module for fixed and random-effects meta-analysis. Boston College Department of Economics; 2009. [Google Scholar]
- 34.Windish DM, Ratanawongsa N. Providers' perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23:1698–1707. doi: 10.1007/s11606-008-0728-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alfandre DJ. "I'm going home" discharges against medical advice. Mayo Clin Proc. 2009;84:255–260. doi: 10.4065/84.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]