Introduction
Adrenal myelolipoma is a rare, benign, mostly non functional tumor of adrenal gland, picked up incidentally on investigations for an unrelated pathology. Radiological features are diagnostic for this condition. While observation is recommended for smaller lesions, opinion is divided regarding management of larger lesions. In this article we present a case report of a middle aged male with an incidentally detected adrenal myelolipoma.
Case Report
A 41 years old male with no previously known comorbid conditions presented with the history of dysuria of 1 month duration to a district hospital. There was no previous history of urinary tract infection or urinary tract stone disease. Urine analysis and culture were suggestive of urinary tract infection and it was managed with appropriate antibiotics. USG abdomen revealed no abnormality in the urinary tract. However a 7 cm, hypoechoic, right adrenal mass lesion was incidentally detected. Patient was then referred to our centre for further management.
On presentation at our centre, the patient was asymptomatic. His dysuria had subsided and he was passing urine normally. There was no previous history of pain abdomen/episodes of headache/flushing/diarrhea. Patient was not a known diabetic or hypertensive. General examination of the patient was normal. On abdominal examination there was no palpable lump. There was no renal angle tenderness or fullness.
Contrast enhanced CT scan of the abdomen was done for the patient. Plain scans showed a mass lesion involving right adrenal gland with soft tissue and fat density (−91 HU) contents (Fig. 1). Tissue planes with right kidney and liver were well defined. There was a heterogeneous post contrast enhancement in the arterial phase with washout in delayed phase (Fig. 2). A radiological impression of adrenal myelolipoma was given.
Fig. 1.
CECT scan of abdomen—non contrast axial section showing large right adrenal lesion with fat density areas(−91HU) and soft tissue density areas (10HU)
Fig. 2.
CECT Abdomen—Contrast enhanced axial section showing heterogenous enhance ment of the Right Adrenal lesion
His 24 h urinary cortisol was 155.85 μg and plasma ACTH levels was 13.50 pg/ml which were within normal limits. His 24 h urinary catecholamines were within normal limits except for a small elevation in the levels of epinephrine 26.47 μg/24 h (Normal 1.7–247 μg/24 h). His blood pressure recordings in the ward were within normal range.
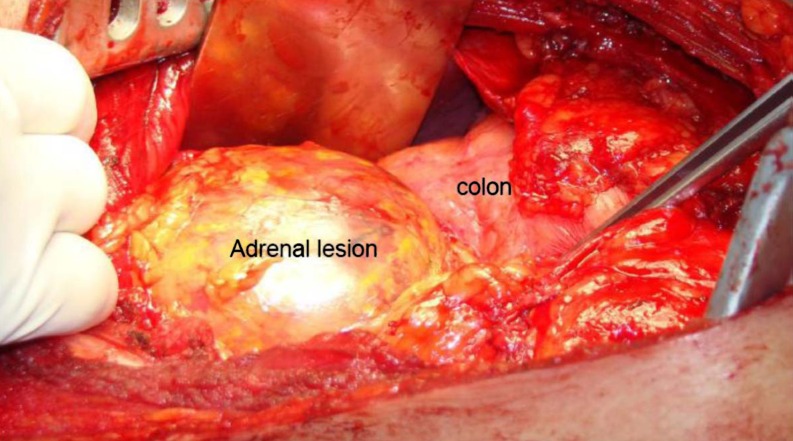
Although our patient was asymptomatic but keeping in view the size of the lesion and mild biochemical abnormality, the patient was offered surgery after a joint clinical discussion. Patient was operated under general anaesthesia with placement of a thoracic epidural catheter for perioperative analgesia. Intraoperatively there were no hemodynamic fluctuations. We used a flank incision (11th rib bed) with a retroperitoneal approach. Intra-operatively the lesion was seen as a well encapsulated tumor arising from the right adrenal gland (Fig. 3). After ligating the vascular pedicles the lesion was excised in toto. Post operatively the patient made an uneventful recovery.
Fig. 3.
Intra operative picture showing Right adrenal lesion behind hepatic flexure of colon
On gross pathological examination the tumor was well encapsulated measuring 9 × 6 × 7 cms. External surface was covered with fat and cut surface revealed yellowish areas mixed with foci of blackish areas (Figs. 4, 5). Histopathology revealed mature adipocytes with mixed foci of mature bone marrow elements. Normal adrenal tissue was also seen. There was no evidence of malignancy (Fig. 6).
Fig. 4.

Gross appearance of resected specimen showing well encapsulated tumor
Fig. 5.
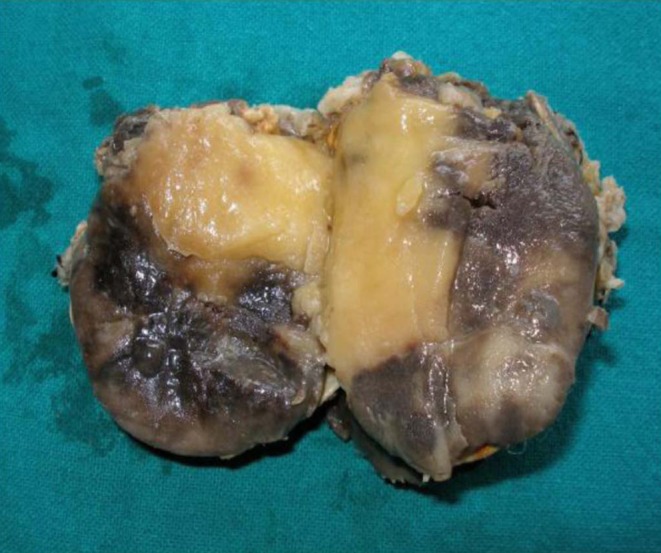
Cut surface of specimen (in formalin) showing dark areas (myeloid) interspersed with yellowish areas(lipomatous)
Fig. 6.
Photomicrograph showing normal adrenal with tumor area showing marrow element interspersed with fat globules
Discussion
Myelolipomas are rare benign tumors with an overall incidence of 0.03–0.8%. They form 5–7% of primary adrenal neoplasms. Composed of mature adipose and hematopoietic tissue they are thought to be arising due to metaplasia of the reticulo-endothelial cells of blood capillaries in the adrenal gland in response to stimuli such as infection, stress or necrosis [1].
They are usually noticed in late adulthood with mean age of 62 years. Male and females are equally affected [2]. Although these lesions are usually unilateral, bilateral tumors have been described in 10% cases [3]. Right sided lesions are more common [2, 3].
Myelolipomas are often less than 4 cm in diameter when discovered. However they can attain very large sizes [4]. Although generally hormonally inactive, there are case reports of their association with overproduction of adrenal hormones. Myelolipomas have been associated with overproduction of dehydroepiandrosteronesulphate (DHEAS), congenital adrenal hyperplasia caused by 21-hydroxylase deficiency, congenital adrenal 17 α-hydroxylase deficiency, Cushing disease, Conn syndrome, adrenal insufficiency, and pheochromocytoma[5]. Some of these tumors co-exist with adrenal adenomas which may in part account for the hormonal activity [6]. Due to aforesaid reasons, hormonal profile must be obtained in all patients with this tumor.
Most of the adrenal myelolipomas are asymptomatic and are diagnosed as incidental finding during imaging. They occasionally present with pain due to large size or from spontaneous haemorrhage. They are known to be associated with associated with obesity, hypertension and diabetes [7].
Imaging features are diagnostic. On ultrasonography, myelolipomas appear as a well defined tumor with varying degrees of hyperechoic areas (fatty tissue) and hypoechoic areas (myeloid tissue). The demonstration of fat density (hypodense) within an adrenal mass by CT scan is virtually diagnostic of angiomyolipoma [8]. MRI show homogenous hyperintense mass on T1 weighted images with an intermediate signal on T2 weighted images, suggesting fat containing lesions. The lesion enhances brightly after intravenous administration of gadolinium. Decrease in signal with fat suppression or phase cancellation is confirmatory [9].
Management of small and asymptomatic myelolipomas is observation. Han et al. in their article suggest that almost half of the myelolipomas can be managed conservatively [10]. Symptomatic myelolipomas should be treated with surgical excision as observation is unlikely to relieve symptoms. Larger myelolipomas (>4 cm) are associated with complications, hence surgical excision is preferred over observation. Our patient although asymptomatic, had a large myelolipoma with mild biochemical abnormality and hence merited surgical exploration.
Conclusion
Myelolipoma of adrenal gland is a rare tumor . Radiological investigations are the diagnostic modality of choice. Patients should be worked up for associated adrenal hormone overproduction. Surgery is indicated for large, symptomatic or hormone producing myelolipomas.
References
- 1.Meaglia JP, Schmidt JD. Natural history of an adrenal myelolipoma. J Urol. 1992;147:1089–1090. doi: 10.1016/s0022-5347(17)37482-7. [DOI] [PubMed] [Google Scholar]
- 2.Lam KY, Lo CY. Adrenal lipomatous tumors: a 30 year clinic pathological experience at a single institution. J Clin Pathol. 2001;54:707–712. doi: 10.1136/jcp.54.9.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haque F, Harish SPB, Ahmad I, et al. Adrenal myelolipoma: a case report. Indian J Radiol. 2004;14:301–302. [Google Scholar]
- 4.Lamont JP, Lieberman ZH, Stephens JS. Giant adrenal myelolipoma’s. Am Surg. 2002;68(4):392–394. [PubMed] [Google Scholar]
- 5.Wagnerova H, Lazurova I, Bober J, Sokol L, Zachar M. Adrenal myelolipoma. 6 cases and a review of the literature. Neoplasma. 2004;51:300–305. [PubMed] [Google Scholar]
- 6.Hisamatsu H, Sakai H, Tsuda S, Shigematsu K, Kanetake H. Combined adrenal adenoma and myelolipoma in a patient with Cushing’s syndrome: case report and review of the literature. Int J Urol. 2004;11:416–418. doi: 10.1111/j.1442-2042.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- 7.Puneet, Tiwary SK, Singh S, Kumar M, Shukla VK (2006) Adrenal myelolipoma: a case report. Internet J Third World Med 3(2)
- 8.Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology. 1998;208:87–95. doi: 10.1148/radiology.208.1.9646797. [DOI] [PubMed] [Google Scholar]
- 9.Bhansali A, Dash RJ, Singh SK, Behra A, Singh P, Radotra BD. Adrenal myelolipoma: profile of six patients with a brief review of literature. Int J Endocrinol Metab. 2003;1:33–40. [Google Scholar]
- 10.Han M, Burnett AL, Fishman EK, Marshall FF. The natural history and treatment of adrenal myelolipoma. J Urol. 1997;157:1213–1216. doi: 10.1016/S0022-5347(01)64926-7. [DOI] [PubMed] [Google Scholar]