Introduction
Adrenal Myelolipoma is a rare, benign, non functioning neoplasm arising from the adrenal cortex. They are composed of mature adipose tissue and a variable amount of normal haemopoietic elements. Most lesions are small and asymptomatic, diagnosed incidentally, however some may present with nonspecific complaints. Pathogenesis of adrenal myelolipoma remains doubtful. With the advent of ultrasonography, computed tomography, and magnetic resonance imaging, pre-operative diagnosis has improved remarkably and explains the recent increase in rate of detection, however, in doubtful cases; FNAC offers a reliable and simple method for the diagnosis. The management should be individualized ranging from observation for small, asymptomatic lesions to surgical excision for large or symptomatic or functional lesions or where diagnosis is in doubt or malignancy cannot be ruled out. Prognosis is excellent. Less than 300 cases have been reported in literature; however awareness regarding this entity is necessary to avoid extensive surgery [1].
Case Report
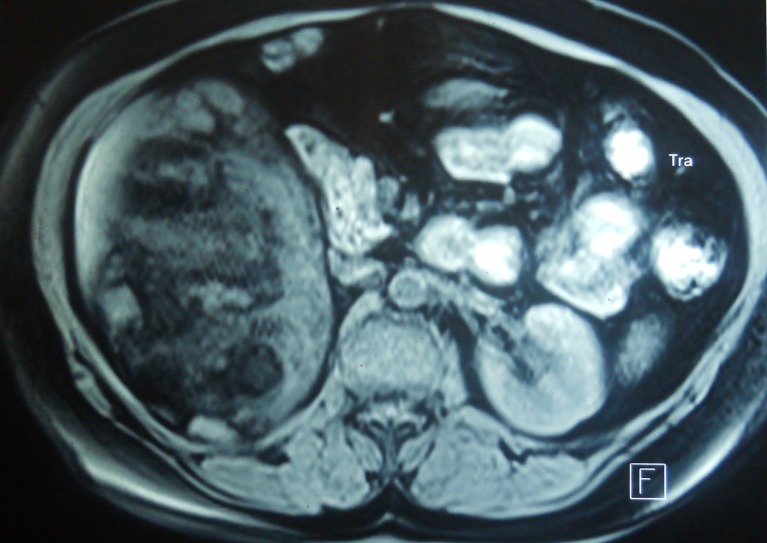
A 43 year old normotensive female presented with complaints of dragging sensation and dull aching pain in the right lumbar region for the past 5 years relieved with oral analgesics. The patient had a known history of allergy to iodinated contrast agents. No other significant history could be elicited. On physical examination, a well defined firm lump could be palpated in the right flank separate from the liver. An ultrasound of the abdomen, revealed an echogenic mass in the upper pole of right kidney with irregular borders, suggestive of a possible renal mass. Routine blood investigations and urine examination were within normal limits for her age and non specific. An MRI of the abdomen was carried out, which noted a large heterogeneous signal intensity lesion in the right suprarenal region with mature and immature fatty component (Fig. 1). The right kidney was seen to be displaced infero-medially and the right adrenal could not be seen separate from the lesion. A possibility of adrenal myelolipoma was suggested. The patient was planned for exploration. A functional adrenal tumor was ruled out by carrying out serum catecholamines and 24 h urinary VMA, which were within normal limits.
Fig. 1.
Large heterogeneous signal intensity lesion in the right suprarenal region with mature and immature fatty component
On exploration done through a hemi-chevron incision, a suprarenal mass measuring 17 × 10 × 6 cm weighing 2400 g was found. The ipsilateral kidney looked grossly normal. Right adrenalectomy was done. Intraoperative period was smooth; there was no fluctuation of blood pressure. On cut sections of the mass, normal adrenal parenchyma was not seen, however microscopy revealed islands of hematopoietic tissue with scattered mature adipocytes (Fig. 2). The mass was seen to replace almost all adrenal tissue, except at the margin beneath the capsule, where scant adrenal tissue was identified.
Fig. 2.

Microscopic image revealing islands of hematopoietic tissue with scattered mature adipocytes; scant adrenal tissue at the margin
The patient had an uneventful postoperative course and recovered well from surgery.
Discussion
Adrenal Myelolipoma is an uncommon benign tumor. It was first described by Gierke in 1905, and later in 1929 Oberling coined the term ‘formations myelolipomatoses’ [2]. In 1957, Dyckman and Freedman reported the first operated case and in 1985, de Blois and de May published the first case of myelolipoma diagnosed only by CT scan and FNAC [3]. Its incidence is 0.08%–0.4% based on autopsy series [4] and constitutes about 3%–5% of all primary adrenal tumors [5]. They are hormonally inactive and account for 7%–15% of adrenal incidentalomas [6].
It has been reported predominantly in the 5th to 7th decade of life, without any sex predilection. Right adrenal is more commonly involved than the left. They are generally solitary, unilateral, small measuring less than 5 cm in diameter and grow slowly [7], however giant myelolipoma (>10 cm in diameter) weighing a heavy as 6 kg has been reported [8, 9]. Only 7 case reports worldwide for bilateral giant adrenal myelolipoma exist [4]. Frequent association with obesity, type 2 diabetes mellitus and hypertension has been noted, and may be coincidental [10]. They commonly arise from the zona fasciculate of the adrenal cortex, but extra adrenal myelolipomas have been found in various sites, including presacral region, cranium, mediastinum, thoracic spine, liver, stomach, spleen, mesentry, lymph nodes, retroperitoneum, testis, and pelvis [11].
They are mostly asymptomatic [12]; diagnosed incidentally during imaging procedures or autopsy; however larger tumors may cause local, non specific symptoms. Some of them may present with abdominal and flank pain associated with mechanical compression or tumor necrosis, or a dragging sensation due to a large mass [13]. Rare presentations include hematuria, constipation, and bowel obstruction. The most dramatic presentation of myelolipoma is that of an acute retroperitoneal haemorrhage or hemoperitoneum following spontaneous rupture of the tumor. Tumors >10 cm are four times more likely to bleed, hence merit surgical excision [14]. Though hormonally silent, they may coexist with congenital adrenal hyperplasia, Cushing’s syndrome, Conn’s syndrome, Addison’s syndrome, Androgenital syndrome, phaeochromocytoma and other functional adenomas. In 85% of these patients, the abnormality involves the pituitary axis and in these patients stimulation with cortisol or adrenocortical hormone has been suggested to be involved in the pathogenesis of myelolipomas [15]. There are still no reports of malignant change even in giant myelolipoma [16].
The natural history of this lesion has been studied in detail and several theories have been proposed regarding the etiology of this tumor; however the cause of this tumor is still unknown. The most accepted of these is that proposed by Meaglia and Schmidt in 1992, which states that myelolipomas arise due to metaplasia of the reticulo-endothelial cells of blood capillaries in the adrenal gland in response to stimuli such as chronic stress, infection, necrosis or inflammation [17]. Other hypotheses include autonomous proliferation of stem cell during embryogenesis, adrenal cortical cell degeneration, bone marrow embolism, and extramedullary haematopoiesis [18]. In 1950, Seyle and Stone succeeded in producing myelolipoma tissue in reticular layer of adrenal cortex in moue by injecting undeveloped extract of hypophysis and testosterone [19].
With improved radiologic techniques, the rate of detection of lesions is gradually increasing. Presence of fat density within adrenal mass on CT scan and hyperintense (fat containing) areas on T1 weighted should raise the suspicion of an adrenal myelolipoma. Myelolipomas appear as well delineated heterogeneous masses with low-density mature fat (less than -30 Hounsfield Units [HU]) interspersed with more dense myeloid tissue. A fatty adrenal mass is virtually diagnostic of myelolipoma, although other less common adrenal tumors containing fat such as teratoma, lipoma, and liposarcoma should be considered [20]. FNAC is a recommended and reliable method of diagnosis in cases where doubt exists after imaging. The aspirate is usually cellular and shows mature adipose tissue fragment with many trilineage haematopoietic cells with a bloody background, mimicking red bone marrow specimens [21]. Though the tumor does not have any intrinsic hormonal activity, we recommend hormonal studies to rule out any probable association with cortical adenoma.
The management of adrenal myelolipoma depends on size of the lesion, tumor growth and symptoms. A small, (<5 cm), asymptomatic myelolipoma showing no tumor growth could be followed-up at increasing time intervals over a 1–2 year period with imaging controls. On the contrary, a symptomatic lesion or a large (>5 cm) myelolipoma or one showing evident growth should be surgically excised as potential risk of haemorrhage exists [22]. However lifelong follow up is recommended in both groups, because of reports of interval growth in residual myelolipoma and of contralateral myelolipoma after resection of the primary lesion [15]. The laparoscopic approach seems to be gaining ground in the management of such benign adrenal tumors [16, 23], but this procedure is not indicated for masses larger than 10 cm or including adhesions and infiltration of the surrounding structures [24].
Acknowledgments
None of the authors has any financial interests to disclose
Financial support: nil
References
- 1.Bhurgri A, Bhurgri Y, Khwaja IA. Adrenal myelolipoma – a case report. J Pak Med Assoc. 2001;51:85–86. [PubMed] [Google Scholar]
- 2.Fernandes GC, Gupta RK, Kandalkar BM. Giant adrenal myelolipoma. Indian J Path Microbiol. 2010;53(2):325–326. doi: 10.4103/0377-4929.64314. [DOI] [PubMed] [Google Scholar]
- 3.Dell’avanzato R, Castaldi F, Giovannini C, Mercadante E, Cianciulli P, Carlini M. Giant symptomatic myelolipoma of the right adrenal gland – a case report. Chir Ital. 2009;61(2):231–236. [PubMed] [Google Scholar]
- 4.Lin PC, Yang FS. Bilateral giant adrenal myelolipomas a case report and literature review. Chin J Radiol. 2008;33:261–264. [Google Scholar]
- 5.Daneshmand S, Quek ML. Adrenal myelolipoma: diagnosis and management. Urol J. 2006;3(2):71–74. [PubMed] [Google Scholar]
- 6.Chan KC, Chiang HS, Lin YH. Adrenal myelolipoma: a case report with literature review. J Urol ROC. 2000;11:185–189. [Google Scholar]
- 7.Suranagi VV, Malur PR, Bannur HB, Davanageri R, Nerli RB. Adrenal myelolipoma – a rare case report. Al Ameen J Med Sci. 2009;2(1):87–89. [Google Scholar]
- 8.Chakraborty J, Paul PC, Gumta MK, Ghosh G, Goswami B. Adrenal myelolipoma – report of a case. J Indian Med Assoc. 2006;104(3):148–149. [PubMed] [Google Scholar]
- 9.Akamatsu H, Koseki M, Nakaba H, et al. Giant adrenal myelolipoma: report of a case. Surg Today. 2004;34:283–285. doi: 10.1007/s00595-003-2682-4. [DOI] [PubMed] [Google Scholar]
- 10.Soliman HE, Zein TA, Milad MF, et al. Myelolipoma of the adrenal gland diagnosis and management. Saudi Med J. 2001;22(5):457–459. [PubMed] [Google Scholar]
- 11.Destouni C, Karasavvidou F, Pazaitou K, Vellis A, Vainas H. Adrenal myelolipoma diagnosed by fine needle aspiration biopsy. Arch Onc. 2001;9(3):185–187. [Google Scholar]
- 12.Han M, Burnett AL, Fishman EK, Marshall FF. The natural history and treatment of adrenal myelolipoma. J Urol. 1997;157:1213–1216. doi: 10.1016/S0022-5347(01)64926-7. [DOI] [PubMed] [Google Scholar]
- 13.Répássy DL, Csata S, Sterlik G, Iványi A. Giant adrenal myelolipoma. Path Onc Res. 2001;7(1):72–73. doi: 10.1007/BF03032610. [DOI] [PubMed] [Google Scholar]
- 14.Shih HJ, Chang HK. A huge adrenal myelolipoma: a case report. JTUA. 2007;18:102–104. [Google Scholar]
- 15.Muzaffar N, Hasmi A, Mubarak M, et al. Adrenal myelolipoma: a report of three cases and review of literature. J Pak Med Assoc. 2009;59(7):491–493. [PubMed] [Google Scholar]
- 16.Castillo OA, Vitagliano G, Cortes O, Sánchez-Salas R, Arellano L. Laparoscopic adrenalectomy for adrenal myelolipoma. Arch Esp Urol. 2007;60(1):217–221. doi: 10.4321/S0004-06142007000100010. [DOI] [PubMed] [Google Scholar]
- 17.Haque F, Harish S, Ahmad I, Qamar A, Pandey H. Adrenal myelolipoma a case report. Indian J Radiol Imag. 2004;14:301–302. [Google Scholar]
- 18.Kar DK, Agarwal A, Mishra AK, et al. Adrenal myelolipoma associated with cholelithiasis. Indian J Urol. 2001;18:66–69. [Google Scholar]
- 19.Dadfar MR, Mostofi NE. Adrenal myelolipoma. Urol J. 2004;1(3):211–212. [PubMed] [Google Scholar]
- 20.Daneshmand S, Quek ML. Adrenal myelolipoma: diagnosis and management. Urology Journal. 2006;3(2):71–74. [PubMed] [Google Scholar]
- 21.Akhtar F, Ishtiaq S, Ali Z, Hassan U. Adrenal myelolipoma. Ann Pak Inst Med Sci. 2009;5(4):266–268. [Google Scholar]
- 22.Tyritzis SI, Adamakis I, Migdalis V, Vlachodimitropoulos D, Constantinides CA. Giant adrenal myelolipoma, a rare urological issue with increasing incidence: a case report. Cases J. 2009;2:8863. doi: 10.4076/1757-1626-2-8863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harthi B, Raiz MM, Kalaf AH, Zoum M, Shakweer W. Adrenal myelolipoma a rare benign tumor managed laparoscopically: report of two cases. J Min Acc Surg. 2009;5(4):118–120. doi: 10.4103/0972-9941.59312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsuru N, Suzuki K, Ushiyama T, Ozono S. Laparoscopic adrenalectomy for large adrenal tumors. J Endourol. 2005;19:537–540. doi: 10.1089/end.2005.19.537. [DOI] [PubMed] [Google Scholar]