Abstract
Marginal Mandibular Nerve (MMN) is a branch of the facial nerve. Muscles supplied by this nerve are responsible for facial symmetry, facial expressions and phonation. Aim was to study the branching pattern and variations in the position of marginal mandibular nerve. 202 patients who underwent neck dissection from June 2005 to October 2006 at Regional Cancer Centre, Trivandrum, India were included in the study. During the course of neck dissection, the marginal mandibular nerve was first identified around the point where the facial artery crossed the lower border of the mandible. Once the nerve was identified, it was traced both backwards and forward till the whole nerve was exposed. Position of the nerve and its relation to lower border of mandible at the point where the facial artery crossed the lower border of the mandible was noted and number and position of each branches were recorded. In 161of the 202 patients (79.7%) the MMN had a single division. Two branches were noted in 26 patients (12.9%). Three branches for MMN are not uncommon, it was noted in 14 patients (6.9%) and in one patient there were four branches. Every effort should be made to preserve all the branches of MMN to ensure cosmesis and decrease morbidity. The mean distance from the lower border of the mandible to the point where the marginal mandibular nerve crossed the facial artery for all the branches taken together was 1.73 mm below the mandible. In 49 patients there was communication between MMN and the cervical branch of facial nerve. The point where the facial artery crosses the lower border of the mandible is a reliable landmark to locate the MMN. Variation in the branching pattern of marginal mandibular nerve is very common.
Keywords: Marginal mandibular nerve, Facial artery, Neck dissection
Introduction
The marginal mandibular nerve is a branch of facial nerve that emerges from the anterior border of the lower part of the parotid gland into the neck where it lies deep to the platysma and the investing layer of deep fascia. It then courses superficial to the facial artery and vein and enters the face by crossing across the lower border of the mandible to innervate the muscles of the lower part of the face and lower lip. The course of the marginal mandibular nerve is usually variable [1]. The cervical portion of the nerve is vulnerable to injury while dissecting the submandibular triangle to clear lymph nodes in Level 1b as part of a neck dissection for head and neck cancers. Injury to this nerve results in facial asymmetry, deviation of the angle of the mouth, drooling of saliva and difficulty of speech and chewing. In order to achieve a thorough clearance of level 1b lymph nodes without damaging the marginal mandibular nerve, the nerve should be identified and preserved in the cervical part of its course. This requires a detailed knowledge of its course in the neck and its anatomic variations, which are quite common. The purpose of this study was to study the variations in the branching and the course of the marginal mandibular nerve.
Patients and Methods
The study was conducted among 202 patients (144 males and 58 females) who underwent neck dissection as part of treatment for head and neck cancers between June 2005 and October 2006 at the Head and Neck Service of Regional Cancer Centre, Trivandrum, India. The patients were positioned in the supine position with the neck extended and the head turned to the contra lateral side. The upper part of the neck was exposed by raising the upper cervical flap carefully in the subplatysmal plane to about 1 cm above the lower border of the mandible. The facial artery was located by palpating its pulsation at the lower border of the mandible. At this point the fascia over the facial artery was opened carefully and the artery dissected for about 1 cm above and below the mandible till the marginal mandibular nerve was found crossing the artery as shown in Fig. 1. The distance from the lower border of the mandible to the point where the marginal mandibular nerve crosses the facial artery was measured as shown in Figs. 2 and 3. The nerve was then very carefully dissected backwards till the point of emergence from the parotid and forward till it crosses the lower border of the mandible to enter the face. The number of branches of the nerve was noted and the distance of each branch from the lower border of the mandible to the point where it crosses the facial artery was measured. Once the marginal mandibular nerve and its branches were identified, preserved and protected, the contents of the submandibular triangle were cleared thoroughly as part of the neck dissection.
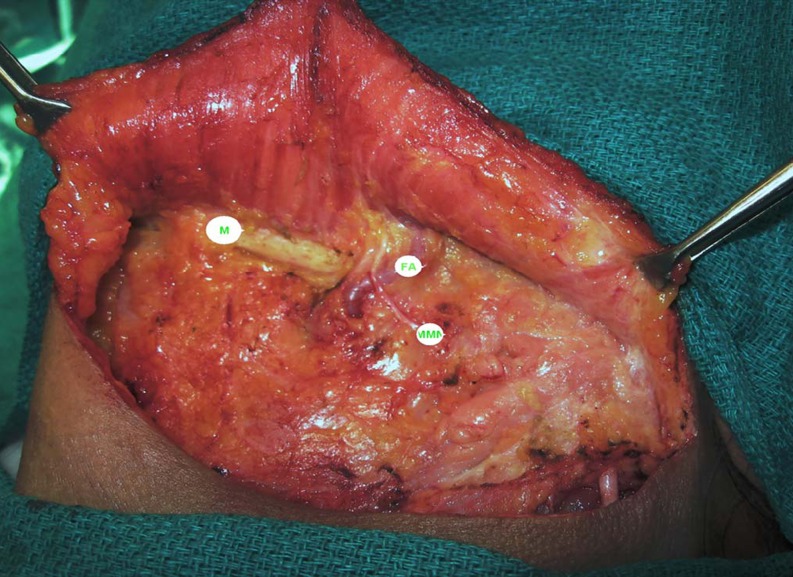
Fig. 1.
Shows the lower border of mandible (M) and the dissected facial artery (FA) with the marginal mandibular nerve (MMN) crossing the facial artery below the lower border of mandible
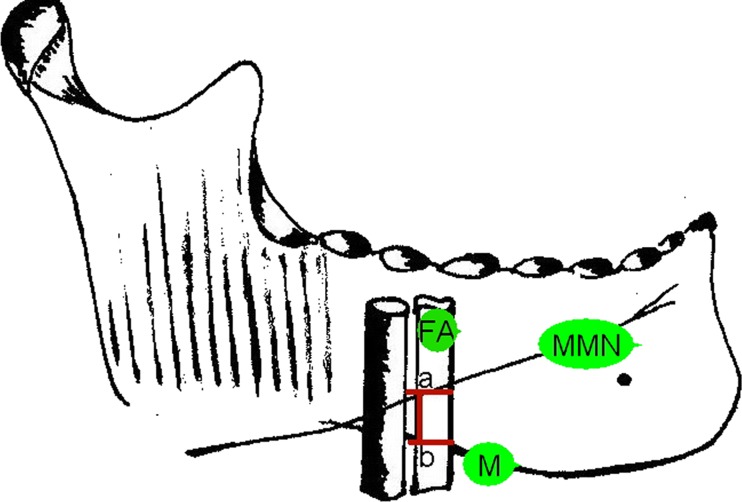
Fig. 2.
Diagram showing the point where the marginal mandibular nerve (MMN) crossed the facial artery (FA), and the measurement (a–b) which is the distance at which MMN was identified crossing the facial artery from the lower border of mandible
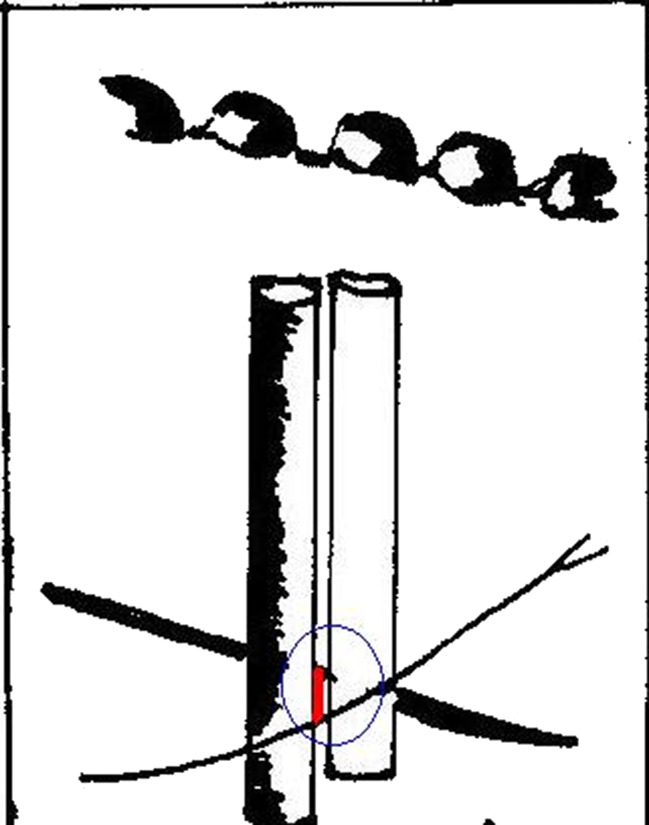
Fig. 3.
MMN shown crossing the facial artery below the lower border of mandible
Results
In 161of the 202 patients (79.7%) the MMN was a single division. It had branched in the others and was in form of two branches in 26(12.9%) patients, three branches in 14(6.9%) patients and four branches in one patient. In patients with a single branch, the nerve crossed the facial artery below the lower border of the mandible in 97/161 (60%) patients, at the lower border of the mandible in 42/161(26%) patients and above the lower border in 22/161 (14%) patients. Among patients with two branches, one crossed the facial artery above the lower border of the mandible and the other crossed at the lower border in 16/26(61.5%) patients while in 7/26 (26.9%) patients one branch crossed at the lower border and the second crossed below the lower border of the mandible. In one patient, one branch crossed above the lower border of the mandible and the other branch below the lower border of the mandible. In another patient both branches crossed the facial artery below the lower border of the mandible. Among patients with three branches of the marginal mandibular nerve, two branches crossed the facial artery below and one branch above the lower border of the mandible in 4/14(28.5%) patients. In 9/14(64.2%) patients, two branches crossed the facial artery below the lower border of the mandible and the third branch crossed the artery at the lower border of the mandible. In one patient all the branches crossed the facial artery below the mandible. In the single patient who had four branches of the nerve, three of the branches crossed the facial artery below the lower border of the mandible and the fourth branch crossed above the lower border of the mandible. The lowest branch crossed the facial artery 8 mm below the lower border of the mandible and the highest branch crossed the artery 5 mm above the lower border of the mandible. The mean distance from the lower border of the mandible to the point where the marginal mandibular nerve crossed the facial artery for all the branches taken together was 1.73 mm below the mandible (SD 1.57 mm) .In our series we found that among women 20/69 (29%) had more than one branch for the marginal mandibular nerve, and in men 20/132 (15%) had multiple branching pattern. MMN with four branches was seen in a male. Temporary dysfunction was noticed in 39/202(19%) patients, and nearly all recovered in the course of time.
Discussion
Marginal mandibular nerve, a branch of the facial nerve supplies the depressor anguli oris, the depressor labii inferioris, the mentalis and the orbicularis oris. The part of this nerve which lies in the upper neck lies in close relation to the perifacial lymph nodes along the facial vessels in the submandibular triangle. Since the incidence of metastasis to perifacial lymph nodes in oral cancer has been reported to be 35% and the incidence of occult metastasis is 27% a thorough clearance of level 1b nodes including the facial lymph nodes is mandated in oral cancer since these nodes are the primary sites of lymphatic drainage in oral cancer [2]. This could cause injury to the nerve resulting in facial asymmetry, deviation of the angle of the mouth, drooling of saliva and difficulty of speech and chewing. Techniques described to avoid injury to the nerve include placement of a low cervical incision and low ligation of the facial vein and flipping over the vein to the cranial end of the patient. These techniques would protect the nerve, but are not suited for patients with malignancy, as they do not clear the lymph nodes thoroughly. A thorough clearance of level 1b lymph nodes could be achieved without permanent damage to the marginal mandibular nerve only if the nerve is identified, preserved and protected during surgery. For this a detailed knowledge of its anatomy and its branching patterns is essential.
In the past when radical surgery was the dictum in head and neck cancers, the morbidity of marginal mandibular nerve was over shadowed by other more serious morbidities and the medical fraternity mostly ignored it. This aspect of head and neck surgery did not receive much attention till recently. With advances in multimodality treatment and more emphasis to conservation surgery, function preservation and cosmesis, there was an overall reduction of the other morbidities of head and neck surgery and marginal mandibular nerve and its dysfunction has received considerable attention. The anatomy of marginal mandibular nerve and most importantly its course is variable in different patients. Till recently all the studies on marginal mandibular nerve was done on cadaveric tissue where the tissues are contracted and relatively immobile [3]. Dingman and Grabb described the nerve in relation to the lower border of mandible [4]. In his finding when the course of the marginal mandibular nerve was posterior to the facial artery, it was found to pass over the lower border of the mandible in 81% of dissected cadavers and in 19% one or two branches were found to course up to 1 cm below the rami of the mandible. In contrast if the nerve was found above the facial artery it never coursed below the lower border of the mandible. In contrast during neck dissection with the neck of the patient extended and rotated to the contra lateral side there is gross variation of the course and position due to extension of the neck and traction on the investing layer of deep fascia. Baker and Conley [5], from their experience on parotidectomies reported that the marginal mandibular nerve almost always has a course 1 to 2 cm below the lower border of the mandible. This study clearly demonstrates the difference in the course of the marginal mandibular nerve in preserved cadavers and during actual neck dissection. Till recently marginal mandibular nerve was thought to be a single nerve without branching. This classical teaching was contradicted by studies of Dingman who reported two branches in 67% of the dissected specimens and Wang [6] who described two or more branches in 68%. Nelson et al. described three branches in all the cases [7]. Our study showed two branches in 12.8% of patients and three or more branches in 6.9% of patients. Even though there is a wide variation in the number of branches and their location in relation to the facial artery, the mean distance from the lower mandible was only 1.73 mm in our study. This indicates that a branch of the nerve could easily be located crossing the facial artery within a few mm of the lower border of the mandible. Once a branch is identified it is traced backwards to the parotid and the other branches if any can also be identified. An extensive search of literature did not reveal any series which compared the branching pattern of the marginal mandibular nerve and sex of the individual. In our series up to 30% of women and 15% males had multiple branches for the marginal mandibular nerve. Dissection around the nerve for identifying it leads to temporary neuropraxia in 16–23% of patients, which usually lasts for a few weeks [8, 9]. Our study also had a similar rate of temporary nerve paresis.
Conclusion
The marginal mandibular nerve shows considerable variation in its branching and its course in the upper neck. Unless the nerve and its branches are identified, it is vulnerable to injury while performing a thorough clearance of level 1b nodes during neck dissections for oral cancer. The nerve could be easily identified in the vicinity of the point where the facial artery crossed the lower border of the mandible.
References
- 1.Al-Hayani A. Anatomical localisation of the marginal mandibular branch of the facial nerve. Folia Morphol (Warsz) 2007;66:307–313. [PubMed] [Google Scholar]
- 2.Lym YC, Lee JS, Choi EC. Perifascial lymph node metastasis in the submandibular triangle of patients with oral and oropharyngeal squamous cell carcinoma with clinically node-positive neck. Laryngoscope. 2006;116:2187–2190. doi: 10.1097/01.mlg.0000244390.40200.e1. [DOI] [PubMed] [Google Scholar]
- 3.Woltmann M, Faveri R, Sgrott EA. Anatomosurgical study of the marginal mandibular branch of the facial nerve for submandibular surgical approach. Braz Dent J. 2006;17:71–74. doi: 10.1590/S0103-64402006000100016. [DOI] [PubMed] [Google Scholar]
- 4.Dingman RO, Grabb WC. Surgical anatomy of the mandibular ramus of the facial nerve based on the dissection of 100 facial halves. Plast Reconst Surg 29:266–690 [DOI] [PubMed]
- 5.Conley J, Baker DC, Selfe RW. Paralysis of the mandibular branch of the facial nerve. Plast Reconst Surg. 1982;70:569–576. doi: 10.1097/00006534-198211000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Wang TM, Lin CL, Kuo KJ, Shih C. Surgical anatomy of mandibular ramus of the facial nerve in Chinese adults. Acta Anat (Basel) 1991;142:126–131. doi: 10.1159/000147176. [DOI] [PubMed] [Google Scholar]
- 7.Nelson DW, Gingrass RP. Anatomy of the mandibular branches of the facial nerve. Plast Reconst Surg. 1979;64:479–482. doi: 10.1097/00006534-197910000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Seppalainen AM, Soderholm AL, Lindqvis C. Neuromuscular dysfunction after surgical treatment of oral cancer. Electromyogr Cl Neurophysiol. 1995;35:45–51. [PubMed] [Google Scholar]
- 9.Nason RW, Binahmed A, Torchia MG, Thliversis J. Clinical observations of the anatomy and function of the marginal mandibular nerve. Int J Oral Maxillofac Surg. 2007;36:712–715. doi: 10.1016/j.ijom.2007.02.011. [DOI] [PubMed] [Google Scholar]