Abstract
The cholecystocolonic fistula is an atypical variant of biliary disease. When presenting with symptomatic disease, surgical treatment with cholecystectomy, fistula takedown and possible colonic resection are indicated, however the role of surgery in asymptomatic patients, especially those deemed higher risk is less clear. Herein we present a case of an incidentially discovered asymptomatic cholecystocolonic fistula in a higher risk surgical patient managed nonoperatively. The presentation and treatment options for this disease are discussed in relation to their application to this patient.
Introduction
The cholecystocolonic fistula is an uncommon but pertinent complication of gallbladder disease, occurring in 0.06%–0.14% of patients with biliary disease.1,2 Among the different types of cholecystoenteric fistulas the cholecystoduodenal is the most common with cholecystocolonic fistulas being the second most common.3 Cholecystocolonic fistulas are most commonly discovered incidentally during cholecystectomy, being diagnosed in 0.5% of these procedures.4 Failure to identify these fistulas during operation can have catastrophic complications, resulting in division of the fistula, perforation of the colon, and resultant fecal peritonitis. In the most severe of cases it can progress to sepsis and death.
Case Presentation
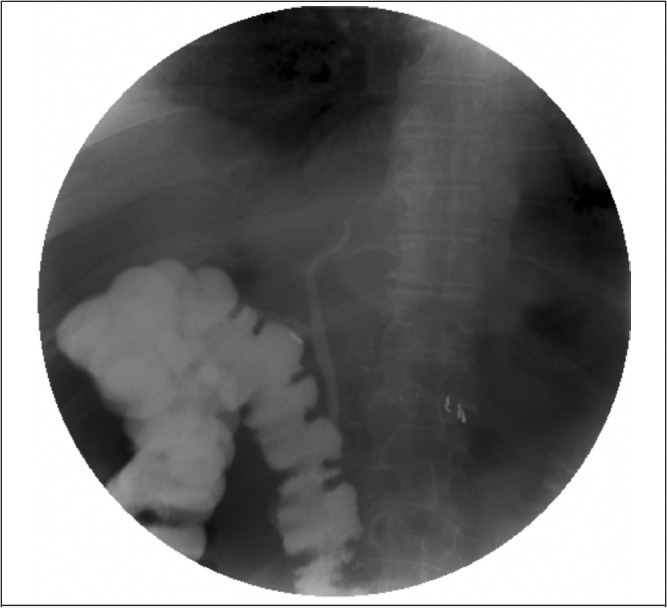
A 55-year-old man presented to the emergency department complaining of chronic abdominal pain from a large ventral hernia. The patient's past medical history was significant for an exploratory celiotomy for a thoracoabdominal gunshot wound 34 years ago. He was uncertain what intra-abdominal injuries he had sustained or what procedures had been performed in conjunction with the exploration. His history was also significant for hypertension, venous stasis, obesity, smoking, chronic obstructive pulmonary disease, and obstructive sleep apnea. On physical exam, the patient was found to have two large, reducible ventral hernias in the left lower quadrant of the abdomen. Laboratory analysis was remarkable for the following normal laboratory values: white blood cell count of 9.7 × 109 cells/L, aspartate transaminase of 18 units/L, alanine transaminase of 25 units/L, alkaline phosphatase of 121 units/L, total bilirubin of 0.3 mg/dL, international normalized ratio of 1.1, and lipase of 25 units/L. A computed tomography examination of the abdomen confirmed the presence of the ventral hernias, but also identified irregular thickening of the gallbladder and chronic fistulous connection to the hepatic flexure of the colon with pneumobilia. A subsequent barium enema confirmed the presence of a cholecystocolonic fistula (Figure 1). The patient also underwent a rigid proctoscopy for hematochezia, which did not reveal the fistula, masses, or other concerning findings.
Figure 1.
On further questioning the patient denied having any right upper quadrant abdominal pain, nausea, vomiting, diarrhea, or constipation. He also denied having any prior episodes of cholecystitis, choledocholithiasis, or other biliary disease. He was offered surgical correction of his cholecystocolonic fistula, followed by a subsequent procedure to treat his hernia, however he was adamant that he would only consent to treatment of his hernia and that he was willing to accept the risk of biliary sepsis in the future. He ultimately underwent an open repair of the hernia with synthetic mesh. His postoperative course was complicated by respiratory failure requiring tracheostomy and several months of pulmonary rehabilitation due to his pulmonary comorbidities. It has been over 4 years since his initial diagnosis of a cholecystocolonic fistula and he has been without an episode of biliary sepsis or associated symptoms.
Discussion
The cholecystoenteric fistula was first described by Courvoisier in 1890. It is believed that these fistulas occur chiefly as a result of inflammation in the gallbladder due to cholecystitis.5 However, other origins of these anomalies have been reported as consequences of cancer, trauma, amebic infections, peptic ulcers, and diverticulitis.6–9 The origin of this patient's fistula remains elusive. Current speculation is that it may have been the result of his traumatic injury, however as it occurred in a combat environment almost 35 years earlier no records are available to support this assertion.
cholecystocolonic fistulae typically form between the gallbladder and the hepatic flexure of the colon due to their proximity in relation to each other (as occurred in this patient).1 When symptomatic, patients generally present with vague abdominal symptoms. These include diarrhea, abdominal pain, jaundice, fever, nausea, vomiting, steatorrhea, and weight loss.3 In contrast, fistulae to the small bowel classically present with a gallstone ileus. The combination of pneumobilia, chronic diarrhea, and vitamin K malabsorption has been proposed as a pathognomonic triad for cholecystocolonic fistula by Savvidou et al.7 However, this triad is not present in all patients and no studies have been performed to calculate the sensitivity and/or specificity of this triad. A history of gallstones, cholecystitis, ascending cholangitis, gallstone ileus, obstructive jaundice, diverticulitis, or gastrointestinal cancer in the presence of the aforementioned symptoms should raise the clinician's concern for a possible fistula. No one mode of imaging has proven itself to be highly sensitive for the detection of a cholecystocolonic fistula and the diagnosis typically occurs intraoperatively, hence the need for the surgeon to have an appropriate level of concern.3 When suspected intraoperatively, the diagnosis can be confirmed with a cholangiogram.
Classically, this problem, regardless of the presence or absence of symptoms, has been treated with fistula resection, cholecystectomy, and, if necessary, common bile duct exploration.1 When colonic inflammation is severe or there is concern for a malignancy, segmental resection of the colon with reanastomosis is also performed. While this was traditionally performed through an open approach, several case series have demonstrated equivalent or better results with a laparoscopic approach.4,10 Operation has been favored as it corrects the fistula and removes the theoretic risk of cholangitis from colonic bacterial translocation through the fistula into the biliary tree. This risk has been reported to be as high as 5% in experimental animal models and the presenting complaint in up to 60% of patients.11,12 Furthermore, biliary sepsis in these patients is associated with a 13% mortality.12
This surgical dictum has been questioned over the past several years. Several groups have advocated for observation of the asymptomatic patient, reserving surgery for those that present with biliary sepsis. These authors have argued that given the life expectancy and medical comorbidities of some patients, surgery as a preventative measure would be of limited benefit. Instead these authors have advocated for clinical observation and symptomatic treatment. Symptomatic treatment has consisted of vitamin supplementation to address the decreased absorption of fat soluble vitamins due to diversion of bile into the colon, prophylactic antibiotics, and endoscopic retrograde cholangiography and sphincterotomy to treat episodes of biliary obstruction and infection.13,14 While this policy is only espoused in a limited number of case reports and small case series, it does seem a valid approach.
While we initially advocated for a definitive surgical procedure, we ultimately agreed with these authors and supported the patient's decision to undergo observation alone. This was based, in part, upon concerns about his overall life expectancy and ability to tolerate a surgical procedure. Several factors contributed to the concern about his life expectancy including morbid obesity, severe chronic obstructive pulmonary disease, and tobacco dependence. Given the decrease in his life expectancy, the potential time to benefit from a surgery seemed limited. The severity of his chronic obstructive pulmonary disease would have precluded a laparoscopic repair and an open repair would have required a larger incision than was used for his hernia repair. Thus, given his significant pulmonary complications with the hernia repair, we believe that a more involved procedure (ie, open cholecystectomy, fistula takedown, and possible colon resection) would have been potentially catastrophic for the patient. Taken together this constellation of factors support the decision to proceed with observation in this patient and highlight the need to reconsider routine surgical intervention in asymptomatic patients.
In conclusion, while the presence of a cholecystocolonic fistula is a rare entity, it is one that health care providers should be aware of. We advocate that non-operative management and clinical observation is an appropriate treatment option to consider.
Footnotes
The views expressed in this manuscript are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the US Government.
Conflict of Interest
The authors report no conflict of interest.
References
- 1.Glenn F, Reed C, Grafe WR. Biliary enteric fistula. Surg Gynecol Obstet. 1981;153:527–532. [PubMed] [Google Scholar]
- 2.Haff RC, Wise L, Ballinger W. Biliary-Enteric Fistulas. Surg Gynecol Obstet. 1971;133:84–88. [PubMed] [Google Scholar]
- 3.Costi R, Randone B, Violi V, et al. Cholecystocolonic fistula: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg. 2009;16:8–18. doi: 10.1007/s00534-008-0014-1. [DOI] [PubMed] [Google Scholar]
- 4.Chowbey PK, Bandyopadhyay SK, Sharma A, Khullar R, Soni V, Baijal M. Laparoscopic management of cholecystoenteric fistulas. J Laparoendosc Adv Surg Tech A. 2006;16:467–472. doi: 10.1089/lap.2006.16.467. [DOI] [PubMed] [Google Scholar]
- 5.Abou-Saif A, Al-Kawas F. Complications of gallstone disease: Mirrizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002;97:249–254. doi: 10.1111/j.1572-0241.2002.05451.x. [DOI] [PubMed] [Google Scholar]
- 6.Goenka P, Iqbal M, Manalo G, Youngberg GA, Thomas E. Colo-cholecystic fistula: an unusual complication of colonic diverticular disease. Am J Gastroenterol. 1999;94:2558–2560. doi: 10.1111/j.1572-0241.1999.01396.x. [DOI] [PubMed] [Google Scholar]
- 7.Savvidou S, Goulis J, Gantzarou A, Ilonidis G. Pneumobilia, chronic diarrhea, vitamin K malabsorption: a pathognomonic triad for cholecystocolonic fistulas. World J Gastroenterol. 2009;15:4077–4082. doi: 10.3748/wjg.15.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Menda RK, Chulani HL. Cholecystocolonic fistula following ameboma of the ascending colon: report of a case. Dis Colon Rectum. 1971;14:386–388. doi: 10.1007/BF02553429. [DOI] [PubMed] [Google Scholar]
- 9.Craighead CC, Raymon AH., Jr With special reference to choledochoduodenal fistula complicating duodenal ulcer. Am J Surg. 1954;87:523–533. doi: 10.1016/0002-9610(54)90414-6. [DOI] [PubMed] [Google Scholar]
- 10.Angrisani L, Corcione F, Tartaglia A, et al. Cholecystoenteric fistula (CF) is not a contraindication for laparoscopic surgery. Surg Endosc. 2001;15:1038–1041. doi: 10.1007/s004640000317. [DOI] [PubMed] [Google Scholar]
- 11.Madden John L, Chun John Y, Kandalaft S, Parekh M. Choledochoduodenostomy: an unjustly maligned Surgical procedure? Am J Surg. 1970;119:45–52. doi: 10.1016/0002-9610(70)90010-3. [DOI] [PubMed] [Google Scholar]
- 12.Safaie-Shirazi S, Zike WL, Printen KJ. Spontaneous enterobiliary fistulas. Surg Gynecol Obstet. 1973;137:769–772. [PubMed] [Google Scholar]
- 13.Velayos Jimenez B, Gonzalo Molina MA, Carbonero Diaz P, Diaz Gutierrez F, Garcia Madrid A, Hernandez Hernandez JM. Cholecystocolonic fistula demonstrated by barium enema: an uncommon cause of chronic diarrhoea. Rev Esp Enferm Dig. 2003;95:809–812. [PubMed] [Google Scholar]
- 14.Caroli-Bosc FX, Ferrero JM, Grimaldi C, Dumas R, Arpurt JP, Delmont J. Cholecystocolic fistula: from symptoms to diagnosis. Gastroenterol Clin Biol. 1990;14:767–770. [PubMed] [Google Scholar]


