Abstract
Chilaiditi syndrome is a rare condition defined by the presence of gastrointestinal symptoms associated with the radiological finding of segmental interposition of the bowel between the liver and the diaphragm. While it is infrequently indentified as a source of abdominal pain, Chilaiditi syndrome carries clinical significance as it can lead to a number of serious complications including intestinal obstruction, perforation, and ischemia. A 58-year-old woman presented with Chilaiditi syndrome immediately following colonoscopic evaluation. Conservative measures failed to alleviate the patient's symptoms, and the patient ultimately elected to have operative management. Pexy of the cecum and ascending colon led to full resolution of her symptoms. To our knowledge, this is the first documented case of Chilaiditi syndrome iatrogenically induced by colonoscopy. Identification of this syndrome as a complication of colonoscopy and a source of post-procedural pain bears significance for providers involved in the peri-operative care of patients with factors predisposing them to the development of this condition.
Introduction
Chilaiditi's sign, or the incidental radiographic finding of bowel positioned between the liver and the right diaphragm, was first documented in 1865.1 This sign attained its namesake in 1910 when Demetrius Chilaiditi reported three cases of asymptomatic patients who had the appearance of intra-abdominal free air on routine abdominal or chest x-ray caused by this interposition of the bowel between the liver and the right hemidiaphragm.1,2 While Chilaiditi's sign does not mandate the accompaniment of symptoms, Chilaiditi syndrome is defined by the presence of symptoms caused by this abnormal anatomic positioning of the bowel. Symptoms associated with Chilaiditi syndrome include abdominal pain, distention, bloating, nausea, vomiting, flatulence, changes in intestinal habits as well as more unusual manifestations such as substernal pain, cardiac arrhythmias, dyspnea, and respiratory distress.3–7
Chilaiditi sign is found incidentally in 0.025%–0.28% of chest and abdominal plain films1,4 and 1.18%–2.4% of abdominal computed tomography (CT) scans.1 Males are affected four times more often than females.1,5 This finding has been documented in a wide age range with patients from 5 months5 up to 81 years of age being afflicted.4 It is more commonly seen in the elderly population, where the incidence is approximately 1%.1 This report describes the first known case of Chilaiditi syndrome precipitated by colonoscopy.
Case Presentation
A 58-year-old woman presented to the emergency department with a two day history of right upper quadrant abdominal pain and nausea following colonoscopic examination. The colonoscopy was performed to evaluate nine months of intermittent abdominal pain originating in the right lower quadrant with occasional migration to the left lower quadrant, right upper quadrant and right flank. Pain was accompanied by abnormal bowel movements with frequent diarrhea and occasional constipation. The patient had undergone extensive work-up for these symptoms including abdominal and pelvic CT scans, pelvic magnetic resonance imaging, upper gastrointestinal with small bowel follow-through, and gynecologic examination. All exam findings were unremarkable. She was managed symptomatically by her physician for presumed irritable bowel syndrome and referred to gastroenterology for a colonoscopy. Colonoscopy revealed only mild sigmoid diverticulosis and a small tubular adenoma. After the procedure, the patient developed severe, sharp, right upper quadrant abdominal pain accompanied by nausea without vomiting. Over the next 2 days, her pain became intolerable despite increased dosages of oral analgesics. At the time of presentation to the emergency department, the patient was still passing flatus and having bowel movements. She had no fever, chills, abdominal distention, or blood per rectum.
The patient's past medical history was significant for Prinzmetal's angina, hyperlipidemia, hypertension, PTSD, depression, migraines, fibromyalgia, lumbar stenosis with chronic low back pain, urethral stricture and diverticula, and osteoporosis. The patient had undergone multiple abdominal procedures: abdominal stab wound repair, right inguinal hernia repair, two Cesarean sections, tubal ligation, and urethral diverticulotomy. Her family history was negative for any gastrointestinal conditions including irritable bowel disease or cancer. Social history was only remarkable for remote tobacco use.
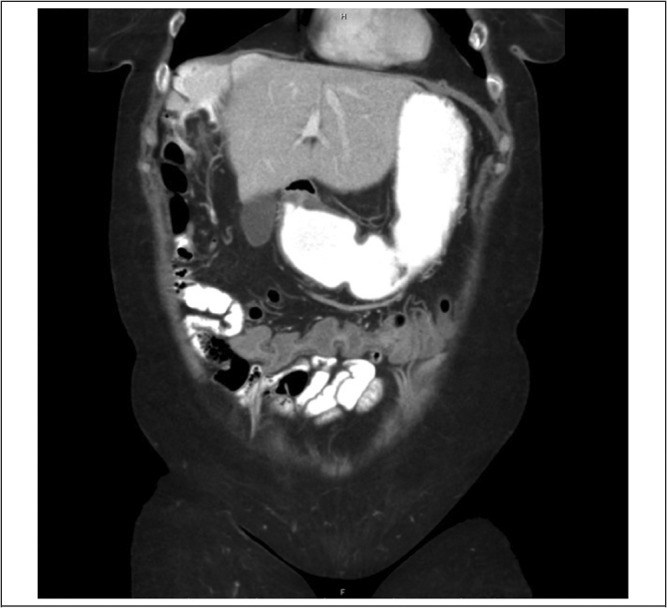
On initial evaluation, the patient was afebrile with stable vital signs. Physical exam was notable for right upper quadrant tenderness without any findings suggestive of peritonitis such as rigidity, guarding, rebound tenderness, or Murphy's sign. Laboratory work-up including complete blood count, basic metabolic panel, liver function tests, amylase and lipase levels, coagulation studies, and urinalysis were all unremarkable. CT scan of the abdomen and pelvis with contrast showed new interposition of the cecum and ascending colon in between the liver and diaphragm with slight mass effect on the liver but no volvulus, twisting or wall thickening of the intestines (Figures 1 & 2). In light of the patient's symptoms and the radiographic findings, the diagnosis of Chilaiditi syndrome was made.
Figure 1.
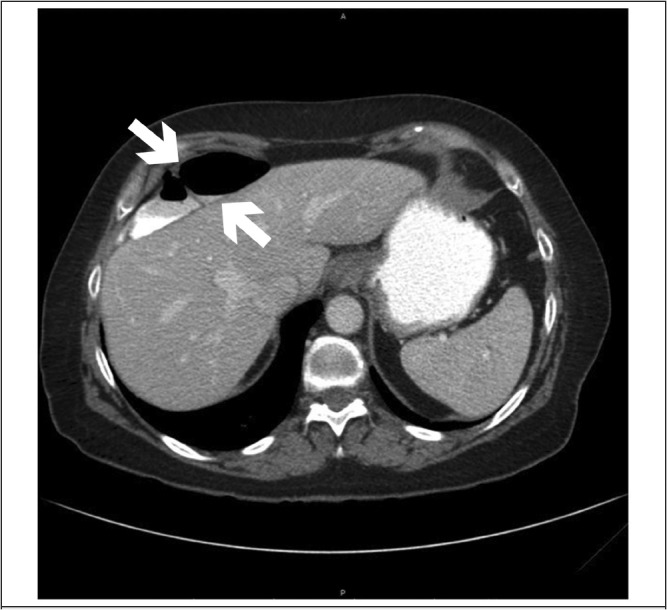
Figure 2.
Since the patient was clinically stable and without evidence of obstruction or perforation, she was managed conservatively with a stool softeners and analgesics. However, the patient's symptoms persisted upon re-evaluation after 1 week so she elected to undergo pexy of the cecum and ascending colon and appendectomy. Intra-operative findings included a viable, yet highly redundant and hypermobile bowel with an elongated mesentery (Figure 3). Her post-operative course was complicated by urinary retention that resolved after the administration of bethanechol. At 3 week follow-up, the patient reported complete resolution of abdominal pain with improved regularity of bowel movements. She remained symptom free at 2 month follow up.
Figure 3.

Discussion
Chilaiditi syndrome associated with unusual clinical scenarios is well documented. However, only two other case reports describe iatrogenically induced Chilaiditi syndrome; one in the setting of bariatric surgery8 and the other in the setting of enteral feeding tube insertion.4 This case illustrates a rare but clinically important syndrome that has not been previously reported as a complication of colonoscopy.
Anatomically, Chilaiditi's sign may be divided into anterior and posterior types according to the position of the interposed bowel relative to the liver.7 The interposed bowel is most commonly the hepatic flexure, ascending colon, or transverse colon but involvement of the small bowel, either alone or in combination with the colon, has been reported.3,9 The patient in this case was somewhat unusual in that the cecum, along with the ascending colon, was highly mobile and abnormally positioned.
Any condition lending to an enlarged right subdiaphragmatic space or hypermobility of the intestines can predispose patients to Chilaiditi syndrome. Predisposing factors can be categorized into diaphragmatic, intestinal, hepatic, and other miscellaneous causes (Table 1). It is unclear how factors such as ascites and pregnancy contribute to Chilaiditi syndrome. Ascites and pregnancy both increase intra-abdominal pressure which may facilitate the movement of bowel past the liver into the subdiaphragmatic space. In the case reported here, the patient had a hypermobile and elongated bowel, which was likely the etiology of her long history of right lower quadrant pain and predisposed her to the development of Chilaiditi syndrome following intestinal instrumentation. While the patient did have symptoms prior to colonoscopy, interposition of the bowel into the right subdiaphragmatic space was not seen on imaging prior to colonoscopy and symptoms acutely worsened following the procedure.
Table 1.
Predisposing Factors for the Development of Chilaiditi's Sign
|
Of note, this patient had a history of psychiatric drug use for treatment of depression and post traumatic stress disorder, which has been reported in association with Chilaiditi syndrome.1,7 Other conditions associated with Chilaiditi syndrome in the literature include chronic obstructive pulmonary disease,9 scleroderma,3,7 congenital hypothyroidism, paralytic ileus,3 pneumatosis cystoides intestinalis,4 melanosis coli,3,7 and mental retardation.3,7,9,10 There are also documented reports of Chilaiditi syndrome associated with sigmoid or rectal masses.11,12
Traditionally, Chilaiditi's sign is an important clinical finding as it had been mistaken for free air under the diaphragm on a plain x-ray, and has thus lead to unnecessary exploratory laparotomies.10,13 Chilaiditi's sign, or pseudopneumoperitoneum, may be differentiated from true pneumoperitoneum by close inspection of x-ray imaging for colonic haustra under the right hemidiaphragm.1,10,13,14 CT scan of the abdomen and pelvis has been increasingly used to confirm the diagnosis, potentially limiting the likelihood of unnecessary surgeries.
Knowledge of Chilaiditi's sign or Chilaiditi syndrome carries current clinical importance in the procedural setting. As seen in the bariatric surgery case,8 the feeding tube insertion case,4 and this colonoscopy case, procedures may cause Chilaiditi syndrome, especially in patients with predisposing factors such as bowel hypermobility. Moreover, while no cases of Chilaiditi syndrome induced by colonoscopy have been reported, there have been reported cases of Chilaiditi syndrome complicating or preventing completion of colonoscopic evaluation.7,9,14, Colonoscopy in the setting of Chilaiditi syndrome may also lead to perforation due to progressive trapping of administered air in an acutely angulated segment of bowel.9 Additionally, it is important to note Chilaiditi's sign or Chilaiditi syndrome in patients undergoing liver biopsies as the abnormally positioned bowel is at risk for perforation, particularly during percutaneous transhepatic procedures.4,9
Management for Chilaiditi syndrome is usually conservative with nasogastric decompression, stool softeners and/or enemas, and intravenous hydration. Conservative management is preferred and usually sufficient, but surgical treatment may be indicated for intestinal obstruction, ischemia, or perforation. Documented rare complications of Chilaiditi syndrome requiring emergent surgery include cecal and colonic volvulus,1,3,6,8,15,16 subphrenic appendicitis,1,3 internal herniation,3 and cecal perforation4. Chilaitidi syndrome may also be the initial presentation of malignancies which require rapid medical or surgical management.11,12 Otherwise, elective surgery may be considered for unresolved symptoms as was done in our case. There is no clear consensus on the best surgical approach to correct the bowel interposition. A variety of procedures described in the literature including colon resection, hepatopexy, colopexy, right hemicolectomy, sigmoidectomy, and subtotal colectomy3,6,7,8,13,17 have been performed with success. Minimally invasive procedures, such as laparoscopic colopexy18, have been used and may also be considered. The woman described in this case suffered from continued right upper and lower abdominal symptoms refractory to conservative management. Elective pexy of the ascending colon and cecum led to complete resolution of her symptoms.
Conclusion
In sum, this case report is the first to present Chilaiditi syndrome as an acute complication of a colonoscopy. Awareness of this syndrome as well as Chilaiditi's sign is essential for all care providers as it should be considered during pre-procedural workup, as well as in the evaluation of post-procedural abdominal pain. Attention should be paid to factors predisposing patients to the development of Chilaiditi syndrome and treatment altered accordingly.
Conflict of Interest
None of the authors identify any conflict of interest.
References
- 1.Farkas R, et al. Chilaiditi's sign in a blunt trauma patient: a case report and review of the literature. J Trauma. 2008;65:1540–1542. doi: 10.1097/01.ta.0000208194.49228.03. [DOI] [PubMed] [Google Scholar]
- 2.Chilaiditi D. Zur Frage der Hapatoptose und Ptose in allgemeinen im Auschluss an drei FŠlle von temporŠrer partieller Leberverlagerung. Fortschritte auf dem Gebiete der Roentgenstrahlen. 1910;16:173–208. [Google Scholar]
- 3.Risaliti A, et al. Chilaiditi's syndrome as a surgical and nonsurgical problem. Surg Gynecol Obstet. 1993;176(1):55–58. [PubMed] [Google Scholar]
- 4.Aldoss IT, et al. Chilaiditi syndrome complicated by cecal perforation. South Med J. 2009 Aug;102(8):841–843. doi: 10.1097/SMJ.0b013e3181ad5d62. [DOI] [PubMed] [Google Scholar]
- 5.Keles S, et al. Chilaiditi syndrome as a cause of respiratory distress. Eur J Pediatr. 2006 Jun;165(6):367–369. doi: 10.1007/s00431-005-0077-9. Epub 2006 Feb 18. [DOI] [PubMed] [Google Scholar]
- 6.Kurt Y, et al. Colonic volvulus associated with Chilaiditi's syndrome: report of a case. Surg Today. 2004;34:613–615. doi: 10.1007/s00595-004-2751-3. [DOI] [PubMed] [Google Scholar]
- 7.Altomare DF, et al. Chilaiditi's syndrome. Successful surgical correction by colopexy. Tech Coloproctol. 2001;5:173–175. doi: 10.1007/s101510100022. [DOI] [PubMed] [Google Scholar]
- 8.Platz TA, et al. Chilaiditi syndrome—an interesting complication in a bariatric surgery patient. Surg Obes Relat Dis. 2006;2:57–60. doi: 10.1016/j.soard.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Gurvits GE, et al. Air under the right diaphragm: colonoscopy in the setting of Chilaiditi syndrome. Gastrointest Endosc. 2009 Mar;69(3):758–759. doi: 10.1016/j.gie.2008.12.238. [DOI] [PubMed] [Google Scholar]
- 10.Saber AA, et al. Chilaiditi's syndrome: what should every surgeon know? Am Surg. 2005 Mar;71(3):261–263. doi: 10.1177/000313480507100318. [DOI] [PubMed] [Google Scholar]
- 11.Antonacci N, et al. Dyspnea and large bowel obstruction: a misleading Chilaiditi syndrome. Am J Surg. 2011 Nov;202(5):e45–e47. doi: 10.1016/j.amjsurg.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Yagnik VD. Chilaiditi syndrome with carcinoma rectum: rare entity. Saudi J Gastroenterol. 2011 Jan-Feb;17(1):85–86. doi: 10.4103/1319-3767.74443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosa F, et al. Chilaiditi's syndrome. Surgery. 2011 Jul;150(1):133–134. doi: 10.1016/j.surg.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Bassan MS, et al. Education and imaging. Gastrointestinal: Chilaiditi syndrome. J Gastroenterol Hepatol. 2008 Mar;23:499. doi: 10.1111/j.1440-1746.2008.05336.x. [DOI] [PubMed] [Google Scholar]
- 15.Chen SY, et al. Sigmoid volvulus and associated Chilaiditi's syndrome. Rev Esp Enferm Dig. 2007 Aug;99(8):482–483. doi: 10.4321/s1130-01082007000800017. [DOI] [PubMed] [Google Scholar]
- 16.Ansari H, et al. Chilaiditi syndrome and associated caecal volvulus. ANZ J Surg. 2011 Jun;81(6):484–485. doi: 10.1111/j.1445-2197.2011.05758.x. [DOI] [PubMed] [Google Scholar]
- 17.Matthews J, et al. Chilaiditi syndrome and recurrent colonic volvulus: a case report. J Royal Naval Medical Service. 2001;87(2):111–112. [PubMed] [Google Scholar]
- 18.Blevins WA, et al. Minimally invasive colopexy for pediatric Chilaiditi syndrome. J Pediatr Surg. 2011 Mar;46(3):e33–e35. doi: 10.1016/j.jpedsurg.2010.11.039. [DOI] [PubMed] [Google Scholar]


