Abstract
Introduction
Few modern population-based estimates of the prognosis of ruptured abdominal aortic aneurysm (rAAA) exist.
Methods and materials
From 1994–2008, a total of 6954 rAAA cases were identified in Danish nationwide population-based registries.
Results
Of 3148 (45%) surgery cases, 1454 (46%) died within 30 days of surgery. The overall mortality risk of rAAA was 76%. The proportion of patients who received surgery increased from 44%, in the first study period, to 47% in the last study period; the 30-day postoperative mortality rate decreased from 51% to 42%; and the overall mortality risk declined significantly from 77% to 74% (odds ratio: 0.86: 95% confidence interval: 0.77–0.97). However, the age-adjusted mortality rate remained unchanged, due to the increased incidence of rAAA.
Keywords: prognosis, ruptured abdominal aortic aneurysm, epidemiology, mortality
Introduction
The prognosis of ruptured abdominal aortic aneurysm (rAAA) was described during the 1980s and 1990s, but the reporting was sparse and seldom was population-based.1 Since then, modern cardiovascular prevention has improved treatment of hypertension: prehospital care2 and postoperative intensive care3 have become more sophisticated and treatment has become more centralized.
The probability that a patient will reach the hospital alive and survive surgery is highly context-specific, due to infrastructure, iatrogenic thresholds, comorbidities, and the skills of the multidisciplinary team involved. Older estimates for the prognosis of rAAA could, therefore, be outdated. This paper reports a nationwide population-based epidemiological study of the prognosis of rAAA today (2001–2008), and compares it against the past (1994–2000).
Material and methods
Data from 1994 to 2008 were extracted from national registries, and merged at the individual level. Deaths caused by rAAA were identified in the National Registry of Death Causes, using the primary cause of death codes I71.3, I71.8, and I71.9, or the primary, or contributory cause of death code: I71.4 (if an admission due to rupture was registered at the same time). The Danish Vascular Registry (Indik1 = 5) was used to identify patients with rAAA who had undergone surgery, and to obtain their vital status 30 days postoperatively. The study was approved by the Danish Data Protection Agency (J Number: 7-505-29-1515/1).
The proportion of rAAA cases that reached surgery was calculated as the number of procedures for rupture, divided by the number of ruptures. The overall mortality risk was calculated as the number of non-operated rAAA cases plus the number of deaths within 30 days of surgery, divided by the total number of rAAA cases. Due to the relatively limited number of cases, patients of all ages, both female and male, were used for estimation. The periods 1994–2000 and 2001–2008 were compared, using logistic regression models, according to whether patients reached surgery, their postoperative mortality, and the overall mortality, as dependent variables, adjusting for age and gender. Odds ratios (OR) with confidence intervals (CI) are reported.
Results
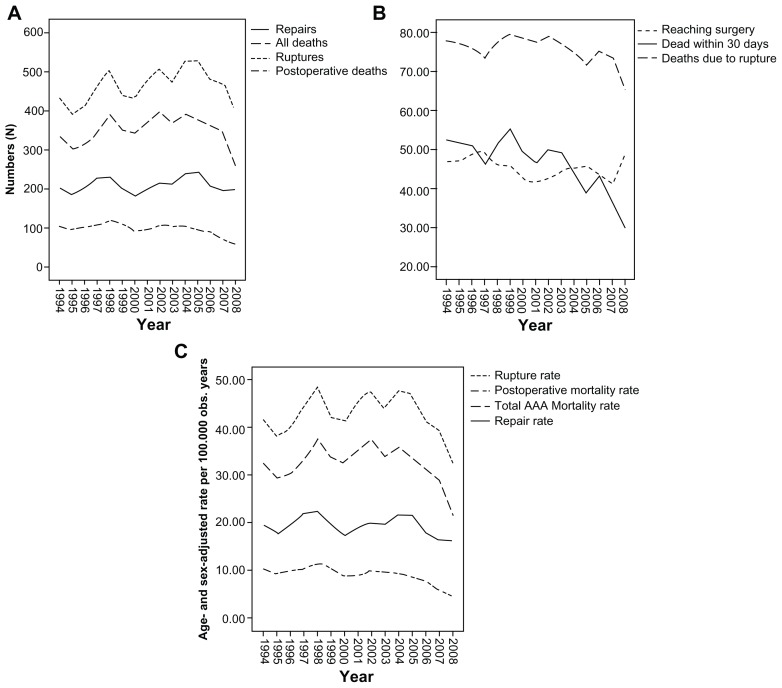
A total of 6954 ruptures were identified. An increasing trend in the number of cases was observed until approximately 2005. A declining trend was observed thereafter (Figure 1). The age-adjusted incidence of ruptures was 44.3 per 100,000 person-years. A total of 3148 (45%) patients had surgery, of whom 1454 (46%) died within 30 days of surgery. Consequently, the overall mortality risk from experiencing rAAA was 5260/6954 (76%). The age-adjusted mortality rate was 33.5 per 100,000 person-years.
Figure 1.
Prognosis of ruptured abdominal aortic aneurysm in Denmark, 1994–2008.
Notes: (A) Numbers of ruptures, postoperative deaths, and total number of deaths. (B) Proportions of patients reaching surgery, 30-day postoperative mortality and overall
From 1994 to 2000, a total of 3081 ruptures occurred, corresponding to a rate of 43.76 per 100,000 age-adjusted person-years. The incidence increased during the period from 2001–2008, when a total of 3873 ruptures occurred, corresponding to a rate of 44.72 per 100,000 age-adjusted person-years.
The mean age of patients at the time of rupture, and the mean age at time of surgery for rupture, increased significantly between the two periods. The proportion of men with rupture who had surgery increased significantly, while the proportion of women with rupture who had surgical repair decreased.
The proportion of patients who had surgery after rupture increased significantly (44% versus 47%; crude OR: 1.20; adjusted OR: 1.27; 95% CI: 1.18–1.37; P > 0.0015). However, the postoperative 30-day mortality risk declined significantly, from 51% to 42% (crude OR: 0.60; adjusted OR: 0.47; 95% CI: 0.39–0.58, P < 0.001), and the overall mortality risk of rAAA declined from 77% to 74% (crude OR: 0.86; adjusted OR: 0.65; 95% CI: 0.61–0.70; P < 0.001). When restricted to the population above 60 years old, the age-adjusted mortality rate per 100,000 person-years was unchanged (33.76 vs 33.29).
Discussion
This short report demonstrates that the incidence of rAAA is still increasing in Denmark, and is still associated with a high mortality risk: approximately 76%. The primary explanation for these results is that less than half of rAAA cases reach the point of surgical repair. However, risk reductions in postoperative mortality have occurred, which may be due to the centralization of treatment in the eastern part of Denmark after 2000, along with improved prehospital care1 and improvements in the function of specialized teams during and after repair. The results cannot be explained by the use of endovascular treatment, as that procedure was not performed during this period, or by a significantly lower autopsy frequency in the last period (the autopsy frequency was only 2.5% lower in the last period than in the first period). Because only 15% of deaths in Denmark had an autopsy during the observation periods, misclassifications seem possible. Due to the frequent comorbidity of known ischemic heart diseases, sudden death outside a hospital, caused by the rupture of an unknown AAA, may be misclassified as death caused by ischemic heart disease, which would increase overall mortality, further emphasizing that rAAA is still associated with a very high mortality risk. Nevertheless, the proportion of patients reaching surgery seems to have increased slightly, and more patients survive surgery. However, there was only a small absolute mortality risk reduction of 3% for a disease that is still increasing in incidence. Consequently, no significant change in the age-adjusted mortality rate for rAAA has occurred. In conclusion, the only proven way to efficiently and substantially reduce the mortality rate of ruptured AAA seems to be using screening to reduce the incidence of rAAA.4,5
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Drott C, Arfvidsson B, Ortenwall P, Lundholm K. Age-standardized incidence of ruptured aortic aneurysm in a defined Swedish population between 1952 and 1988: mortality rate and operative results. Br J Surg. 1992;79(2):175–179. doi: 10.1002/bjs.1800790228. [DOI] [PubMed] [Google Scholar]
- 2.Johansson PI, Stensballe J, Rosenberg I, Hilsløv TL, Jørgensen L, Secher NH. Proactive administration of platelets and plasma for patients with a ruptured abdominal aortic aneurysm: evaluating a change in transfusion practice. Transfusion. 2007;47(4):593–598. doi: 10.1111/j.1537-2995.2007.01160.x. [DOI] [PubMed] [Google Scholar]
- 3.Björck M, Petersson U, Bjarnason T, Cheatham ML. Intra-abdominal hypertension and abdominal compartment syndrome in nontrauma surgical patients. Am Surg. 2011;77(Suppl 1):S62–S66. [PubMed] [Google Scholar]
- 4.Lindholt JS, Sørensen J, Søgaard R, Henneberg EW. Long-term benefit and cost-effectiveness analysis of screening for abdominal aortic aneurysms from a randomized controlled trial. Br J Surg. 2010;97:826–834. doi: 10.1002/bjs.7001. [DOI] [PubMed] [Google Scholar]
- 5.Cosford PA, Leng GC. Screening for abdominal aortic aneurysm. Cochrane Database Syst Rev. 2007;18(2):CD002945. doi: 10.1002/14651858.CD002945.pub2. [DOI] [PubMed] [Google Scholar]