Abstract
Paracoccidioidomycosis (PCM) is an endemic Latin American mycosis caused by Paracoccidioides brasiliensis and also by the recently described P. lutzii. The systemic mycosis is the 10th leading cause of death due to infectious diseases in Brazil. As published, 1,853 patients died of PCM in the 1996–2006 decade in this country. The main diagnostic antigen of P.brasiliensis is the 43 kDa glycoprotein gp43, and its 15-mer peptide QTLIAIHTLAIRYAN, known as P10, contains the T-CD4+ epitope that elicits an IFN-γ-mediated Th1 immune response, which effectively treats mice intratracheally infected with PCM. The association of peptide P10 with antifungal drugs rendered an additive protective effect, even in immunosuppressed animals, being the basis of a recommended treatment protocol. Other immunotherapeutic tools include a peptide carrying a B cell epitope as well as protective anti-gp43 monoclonal antibodies. New delivery systems and gene therapy have been studied in prophylactic and therapeutic protocols to improve the efficacy of the recognized antigens aiming at a future vaccine as co-adjuvant therapy in patients with PCM.
Keywords: P. brasiliensis, P. lutzii, paracoccidioidomycosis, vaccine, immunotherapy
INTRODUCTION
Paracoccidioidomycosis (PCM) appears to be caused by a complex group of fungi within the Paracoccidioides genus comprising four distinct phylogenetic lineages known as PS2, PS3, S1, and Pb01-like (Carvalho et al., 2005; Matute et al., 2006). Based on clinical and genetic studies, the Pb01 isolate differs from the other strains and has been included in a new species known as Paracoccidioides lutzii (Teixeira et al., 2009).
The disease is endemic in a broad region from Mexico to Argentina. About 80% of diagnosed patients are from Brazil. Most patients are rural workers but cases in urban centers located on the route of migration movements are also found (Restrepo, 1985; McEwen et al., 1995). The infection starts by inhalation of conidia that subsequently transform into infective yeast forms in the lung. Although acquisition of the fungus typically results in asymptomatic infection, it can progress in susceptible individuals and give rise to acute, subacute, and chronic clinical forms of the disease (Franco et al., 1993). Systemic dissemination of the fungus can be fatal. A mortality evaluation of P.brasiliensis showed that it is the 10th most common cause of death owing to chronic/recurrent infections and parasitic diseases in Brazil. When analyzed as the underlying cause, 51.2% of deaths were due to PCM, which is then one of the most lethal among systemic mycoses. In the 1996–2006 decade, the most severe cases of PCM occurred in the 30–59 years-of-age range, predominantly (87%) in men (Prado et al., 2009). Besides the mortality data, it is important to consider the morbidity associated to the disease, which invariably leads to withdrawal of the patients from labor activities or school. In the severe cases, hospitalization of patients is necessary for long periods of time with high costs.
Antifungal chemotherapy is required for PCM treatment, although there is no assurance, even after treatment, of complete destruction of the fungus. Initial treatment depends on the severity of the disease and may last from 2 to 6 months; it includes sulfonamides, amphotericin B, or azoles. In severe cases endovenous amphotericin B or sulfonamides are required and when there is clinical improvement, it can be switched to oral sulfonamides or azoles. Extended periods of treatment are often necessary, up to 2 or more years, with a significant frequency of relapsing disease. According to Brazilian guidelines, oral itraconazole is the drug of choice (Shikanai-Yasuda, 2005; Shikanai-Yasuda et al., 2006; Travassos and Taborda, 2011).
Although chemotherapy stands as the basic treatment of PCM, therapeutic vaccination with fungal antigens or passive transfer of specific monoclonal antibodies may boost the cell immune response and add to the protective effect of chemotherapy, eventually counteracting a relapsing disease and reducing fibrotic sequels. Both the innate immune response and the adaptive immunity are important for the antifungal protective effect. The immune system recognizes fungal antigens with subsequent eliciting of antibodies and T cell protective responses. Cytokines and chemokines are produced. IFN-γ-activated macrophages have increased fungistatic and fungicidal activities. Antigens of P. brasiliensis, gp43 or P10, depend on IFN-γ for their protective activity (reviewed in Travassos et al., 2008).
The aim of this review is to update the new concepts and methodologies used in the attempt to develop a therapeutic vaccine against PCM.
THE USE OF FUNGAL WHOLE CELLS AS VACCINE
The use of low-virulence yeast cells as the immunization tool has been investigated. Subcutaneous infection with P. brasiliensis Pb265 induced cellular immunity with high T cell reactivity in susceptible mice which resulted in immunoprotection or disease exacerbation depending on the route of a secondary infection (Arruda et al., 2007a). Immunoprotection with aseptical cure was shown in the pre-immunization procedure and required a combination of CD4+ T cells and CD8+ T cells and the production of endogenous IFN-γ and IL-12 as well as increased levels of anti-P. brasiliensis-specific IgG1 and IgG2a antibodies (Arruda et al., 2007b).
Radio-attenuated yeast cells lost their virulence after the exposure to 6.5 kGy. The irradiated cells were examined by scanning, and also transmission electron microscopy. When examined 2 h after irradiation the cells showed deep folds or collapsed. The plasma membrane and cell wall were intact, but an extensive DNA fragmentation was found (Demicheli et al., 2007). The use of attenuated yeast cells by gamma-irradiation induced a long lasting protection in BALB/c mice (Demicheli et al., 2006; do Nascimento Martins et al., 2007). For this purpose, BALB/c mice were immunized twice in the ocular plexus with 105 viable cells. Animals were then challenged, by the same route, with yeast cells after 30, 45, and 60 days after the last immunization. Thirty days after the challenge, a significant reduction in the fungal burden was observed in the lung, spleen, and liver. A 99.5% decrease in CFU was obtained 90 days post challenge. The animals showed high levels of IFN-γ and IgG2a with very low production of IL-10 and IL-5, suggestive of a Th1 immune cell response (do Nascimento Martins et al., 2007). The number of immunizations with radio-attenuated yeast cells also interferes with the immune response. Authors found that mice immunized once developed a mixed Th1/Th2 response, which was less efficient in the control of the infection, whereas a Th1 pattern was obtained with two immunizations resulting in the elimination of P. brasiliensis yeast cells (do Nascimento Martins et al., 2009).
UNDEFINED SOLUBLE ANTIGENS
Soluble antigens of P. brasiliensis and fractions obtained by ion exchange chromatography of P. brasiliensis extract (F0, FII, and FIII), showed variations in the induction of a protective immune response. Mice immunized with F0 and FII developed benign chronic PCM restricted to the lung, associated with low mortality rates and the presence of compact granulomas with few fungal cells. Significant enhancement of IFN-γ and high levels of IgG2a and IgG3 were found in animals immunized with F0. Immunizations with FII induced significant production of IFN-γ and IL-10 associated with high levels of IgG1 and IgG2a. In contrast, mice immunized with FIII developed a progressive disease with dissemination to spleen and liver. These animals did not control the spread of the fungus showing granulomas with a high number of viable fungal cells (Diniz et al., 2004). A fraction of approximately 380 kDa designated high-molecular-mass (hMM) fraction was able to induce lymphocyte proliferation and production of IFN-γ but not IL-4 when incubated with spleen cells from BALB/c mice infected intravenous with P. brasiliensis (isolate Pb18). Animals previously immunized s.c. with hMM and infected with virulent yeast cells showed a significant reduction of the fungal burden in the lungs and spleen (Pavanelli et al., 2007).
PURIFIED ANTIGEN AND PEPTIDE
The major diagnostic antigen gp43 was isolated from P. brasiliensis culture supernatant fluids in 1986 (Puccia et al., 1986). It reacted with antibodies from virtually 100% of patients with PMC, except some patients exposed to P. lutzii, who showed irregular reactivity to gp43 (Batista et al., 2010). Epitopes in gp43 that elicit a strong antibody response are peptidic in nature (Puccia and Travassos, 1991) and different isoforms of gp43 vary in their reactivity with patients sera. The gp43 gene was cloned and sequenced (Cisalpino et al., 1996); gene expression and polymorphism have been shown (Travassos et al., 2004a,b).
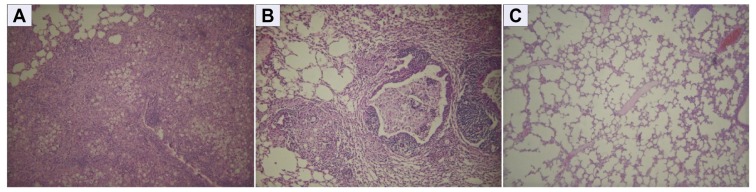
The first evidence that gp43 carried an immunodominant epitope able to elicit DTH reactions was shown in guinea pigs (Rodrigues and Travassos, 1994) and later in patients (Saraiva et al., 1996) using the purified antigen. The T cell epitope responsible for DTH reactions, and CD4+ T cell proliferation, was mapped to a peptide called P10 with the sequence QTLIAIHTLAIRYAN (Taborda et al., 1998). The hexapeptide HTLAIR has been shown to be essential for priming the cellular immune response. In P.lutzii, there is, however, an important mutation in this hexapeptide (Teixeira et al., 2009). Peptide P10 showed to be promiscuous in its presentation by MHC class II molecules from three different mouse haplotypes (Taborda et al., 1998). This was extended to most Caucasian HLA-DR molecules (Iwai et al., 2003). By using the TEPITOPE algorithm neighboring peptides to P10 were also recognized with high affinity HLA-DR binding (Iwai et al., 2007). The protective effect of P10 using complete Freund’s adjuvant (CFA) against intratracheally infected mice is shown in Figure 1.
FIGURE 1.
Representative histopathology of lung lesions caused by P. brasiliensis Pb18 strain in mice immunized with P10 in presence of Freund’s complete adjuvant (CFA). Tissue samples were collected two months after i.t. challenge with the Pb18 strain. (A) Lung section from infected mouse, with a granuloma containing multiple viable fungal cells; (B) Lung section from mouse treated with CFA, showing the extensive granulomatous lesion with intense cellular infiltration and large number of multiplying fungal cells; (C) Lung section from mouse immunized with P10 admixed with CFA showing preserved alveolar structure, absence of granulomatous lesions as well as of fungal cells. All sections were amplified 10-fold and stained with hematoxylin–eosin.
The association of peptide P10 immunization and chemotherapy was tested in i.t. infected BALB/c mice using two protocols. Mice infected with yeast cells of the highly virulent P. brasiliensis (Pb18) underwent P10 and/or drug treatment starting after 48 h or 30 days of infection. The treatment continued for 30 days, during which groups of mice received intraperitoneal doses of itraconazole, fluconazole, ketoconazole, sulfamethoxazole, or trimethoprim/sulfamethoxazole every 24 h. Amphotericin B was administered every 48 h. Immunization with P10 was carried out weekly for 4 weeks, once in CFA and three times in incomplete Freund’s adjuvant (Marques et al., 2006). Animals were sacrificed at different times of infection and significant reduction in the fungal load was observed in both groups, with an additive protective effect obtained with the combination of P10 and antifungal drugs (Marques et al., 2006). Unexpectedly, animals treated with sulfamethoxazole, showed early protection followed by relapse, but the association of sulfamethoxazole and P10 vaccination successfully controlled the infection. The detection of cytokines in lung homogenates from mice vaccinated with P10, showed a typical Th1 response, rich in IFN-γ and IL-12 but without suppression of Th2 cytokines (Marques et al., 2006).
In an attempt to reproduce a general anergic state, BALB/c mice were treated with dexamethasone-21 phosphate added to the drinking water. After 30 days animals showed negative DTH to fungal antigens. Mice were then infected with virulent P. brasiliensis (Pb18) and after 15 days were subjected to chemotherapy and/or P10 immunization. The association of drugs and P10 immunization conferred additive protection. A significant increase in IL-12 and IFN-γ and decrease of IL-4 and IL-10 were observed in mice immunized with P10 alone or in association with antifungal drugs, indicating that also in this case of immune suppression, P10 immunization can be helpful (Marques et al., 2008).
Different ways of peptide delivery using formulations that did not include CFA have also been investigated. The first attempt involved a multiple antigen peptide (MAP) construction. A tetramer of truncated P10 was designated M10 and had four equal LIAIHTLAIRYAN (N-terminal QT-less P10) chains synthesized on a branched lysine core containing glycine at the C-terminal position. Mice immunized with a single dose of M10 without adjuvant and challenged intratracheally with P. brasiliensis showed significantly fewer lung, spleen, and liver CFUs and few or no yeasts in lung sections histopathology (Taborda et al., 2004).
The therapeutic or prophylactic protective effect of P10 was also tested with the peptide admixed with different adjuvants, bacterial flagellin, aluminum hydroxide, cationic lipid in comparison with CFA. A vaccine formulation based on intranasal administrations of gp43 or P10 with the Salmonella enterica FliC flagellin was evaluated in BALB/c mice. Animals were immunized with recombinant purified flagellins genetically fused with P10, either or not flanked by two lysine residues, or with the synthetic P10 admixed with purified FliC. After the last immunization, mice were i.t. infected with P. brasiliensis (Pb18). BALB/c mice immunized with the chimeric flagellins and particularly those immunized with P10 admixed with FliC had reduced fungal burden in the lungs and elicited a predominantly Th1-type immune response (Braga et al., 2009). Other adjuvants were also compared in terms of protective immune response to P10 immunization. Reduction of the pulmonary fungal burden was obtained with aluminum hydroxide, CFA, flagellin, and cationic lipid in intratracheal infected BALB/c mice. The cationic lipid proved to be very efficient in the clearance of fungal load and reduction of fibrotic areas in the lung (Mayorga et al., 2012).
The combination of P10 with sulfamethoxazole/trimethoprim entrapped within poly- (lactic acid–glycolic acid) nanoparticles (PLGA) was tested in the experimental therapeutic protocol of PCM. The incorporation of P10 into PLGA reduced the amount of this peptide necessary to decrease the fungal load in the infected animals and avoid disease relapse when compared with P10 emulsified in Freund’s adjuvant (Amaral et al., 2010).
The potential use of the recombinant protein of 27 kDa (rPb27), present in the soluble fraction F0 (Reis et al., 2008), has been investigated. Immunization of rPb27 in the presence of Propionibacterium acnes and aluminum hydroxide prior to intravenous infection by the orbital plexus with virulent P. brasiliensis (Pb18), was able to efficiently protect BALB/c mice. Recently, another recombinant protein, rPb40, was used associated with fluconazole and shown to reduce the fungal burden in the lungs of BALB/c mice (Fernandes et al., 2011, 2012).
DNA VACCINE AND IMMUNOTHERAPY WITH DENDRITIC CELLS
Immunization of BALB/c mice with a mammalian expression vector (VR-gp43) carrying the full gene of gp43 with CMV promoter induced B and T cell-mediated immune responses protective against the intratracheal challenge by virulent P. brasiliensis yeast forms. The cellular immune response in mice immunized with VR-gp43 induced IFN-γ and the response was maintained for at least 6 months although reduced to half of the stimulation index obtained 15 days after immunization (Pinto et al., 2000). In order to develop a more specific DNA vaccine based predominantly on a T cell-mediated immune response, a plasmid encoding the P10 minigene in pcDNA3 expression vector was tested in intratracheally infected BALB/c and B10.A mice. The vaccination with plasmid encoding P10 induced a significant reduction in the fungal burden in the lung. Co-vaccination with a plasmid encoding mouse IL-12 proved to be even more effective in the elimination of the fungus with virtual sterilization in the long-term infection and treatment assay, using the more susceptible B10.A mice. The immunization elicited significant production of IL-12 and IFN-γ (Rittner et al., 2012). Such immunization with plasmid encoding P10 induced memory cells as well as T regulatory cells (Amorim, 2010), that might help reduce the tissue cell damage of the protective immune response.
The use of heterologous DNA plasmid encoding HSP65 from Mycobacterium leprae was used in a prophylactic protocol. Intramuscular immunization with DNAhsp65 induced an increase of Th1 cytokine levels and reduction of the fungal burden with marked reduction of collagen and lung remodeling (Ribeiro et al., 2009). Similar results were obtained with a therapeutic model (Ribeiro et al., 2010).
A competent CD4+ T cell response producing IFN-γ is usually the chief protective mechanism in fungal infections, particularly in PCM, and dendritic cells are able to initiate the response in naïve T cells.
The use of transfected DCs with a plasmid (pMAC/PS-scFv) encoding a single chain variable fragment (scFv) of an anti-Id antibody that is capable of mimicking gp43 from P. brasiliensis was used to subcutaneously immunize BALB/c mice. After 7 days, the scFv peptide was presented to the regional lymph node cells and was capable to activate proliferation resulting in a decrease of fungal burden (Ferreira et al., 2011).
Using an experimental model in BALB/c mice, P10-primed DCs were administrated prior to (subcutaneous vaccination) or weeks after (subcutaneous or intravenous injection) P. brasiliensis infection, and showed to significantly reduce the fungal burden. The protective response mediated by the injection of primed-DCs was mainly characterized by increased production of IFN-γ and IL-12 and reduction in IL-10 and IL-4 compared to infected mice that received saline or unprimed-DCs (Magalhães et al., 2012).
PASSIVE TRANSFERENCE OF ANTIBODIES
The exacerbated humoral immune response in PCM has been associated to a poor prognosis since patients with acute and subacute forms of the disease show high antibody titers. It has been reported, however, that monoclonal antibodies against gp70 were protective against experimental PCM (Mattos Grosso et al., 2003). The same group of researchers also showed that a monoclonal antibody against surface 75 kDa protein was able to inhibit fungal growth (Xander et al., 2007). The protective effect of anti-gp43 mAbs injected intraperitoneally on the i.t. infection by P. brasiliensis was examined in BALB/c mice (Buissa-Filho et al., 2008). Using a panel of monoclonal antibodies, protective and non-protective monoclonal antibodies with similar reactivity with gp43 on ELISA, were found. The reactivity of mAb 3E, the most efficient mAb in the reduction of fungal burden, that was able to enhance phagocytosis, was mapped to the sequence NHVRIPIGYWAV (Buissa-Filho et al., 2008). This peptide could thus represent, together with P10, another candidate for a peptide vaccine against PCM. In a P10-pre-immunization protocol, mAbs were tested as protective agents. The association of P10-pre-immunization and mAb 3E administered 24 h before i.t. challenge with virulent P. brasiliensis and P. lutzii yeasts, resulted in additive protection using short-term protocols in comparison with a non-protective mAb (data not published).
FINAL REMARKS
While chemotherapy has the chief role of reducing the fungal burden in mycotic infections, the long-term control and eventual sterilization involve an effective immune response. The combination of chemotherapy and an effective vaccine against PCM should ideally treat the more serious cases of the systemic mycosis aiming at a shorter period of treatment, prevention of relapses and of fibrotic sequels. A highly immunogenic antigen of P. brasiliensis and the peptide containing a T cell epitope have repeatedly proved to be protective in prophylactic and therapeutic models with massively infected mice. A new peptide also from the gp43 contains a B cell epitope that reacts with a protective monoclonal antibody. Recently, a DNA vaccine expressing the P10 peptide showed a remarkable protective effect in a long-term infection protocol using mice highly susceptible to PCM. Immunized mice had memory T cells as well as T regulatory cells that prevented tissue cell damage due to the initial pro-inflammatory protective response involving T effector cells. These encouraging results, along with other protective immunizations using new adjuvants, delivery systems, and dendritic cells, point to a next stage of experimentation aiming at the clinical use of the peptide vaccines.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
REFERENCES
- Amaral A. C., Marques A. F., Muñoz J. E., Bocca A. L., Simioni A. R., Tedesco A. C., Morais P. C., Travassos L. R., Taborda C. P., Felipe M. S. (2010). Poly(lactic acid-glycolic acid) nanoparticles markedly improve immunological protection provided by peptide P10 against murine paracoccidioidomycosis. Br. J. Pharmacol. 159 1126–1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amorim J.(2010). Geracão de células T de memória e linfócitos T regulares em camundongos BALB/c vacinados com vetor plasmidial contendo o inserto P10 de Paracoccidioides brasiliensis. Master Degree Thesis, Department of Microbiology, Institute of Biomedical Sciences, University of São Paulo, São Paulo. [Google Scholar]
- Arruda C., Kashino S. S., Fazioli R. A, Calich V. L. G. (2007a). A primary subcutaneous infection with Paracoccidioides brasiliensis leads to immunoprotection or exacerbated disease depending on the route of challenge. Microbes Infect. 9 308–316 [DOI] [PubMed] [Google Scholar]
- Arruda C., Vaz C. A. C, Calich V. L. G. (2007b). Aseptic cure of pulmonary paracoccidioidomycosis can be achieved after previous subcutaneous immunization of susceptible but not resistant mice. Microbes Infect. 9 704–713 [DOI] [PubMed] [Google Scholar]
- Batista J., Jr., Camargo Z. P., Fernandes G. F., Vicentini A. P., Fontes C. J., Hahn R. C. (2010). Is the geographical origin of a Paracoccidioides brasiliensis isolate important for antigen production for regional diagnosis of paracoccidioidomycosis. Mycoses 53 176–180 [DOI] [PubMed] [Google Scholar]
- Braga C. J. M., Rittner G. M., Muñoz J. E., Teixeira A. F., Massis L. M., Sbrogio-Almeida M. E., Taborda C. P., Travassos L. R., Ferreira L. C. (2009). Paracoccidioides brasiliensis vaccine formulations based on the gp43-derived P10 sequence and the Salmonella enterica FliC flagellin. Infect. Immun. 77 1700–1707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buissa-Filho R., Puccia R., Marques A. F., Pinto F. A., Muñoz J. E., Nosanchuk J. D., Travassos L. R., Taborda C. P. (2008). The monoclonal antibody against the major diagnostic antigen of Paracoccidioides brasiliensis mediates immune protection in infected BALB/c mice challenged intratracheally with the fungus. Infect. Immun. 76 3321–3328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho K. C., Ganiko L., Batista W. L., Morais F. V., Marques E. R., Goldman G. H., Franco M. F., Puccia R. (2005). Virulence of Paracoccidioides brasiliensis and gp43 expression in isolates bearing known PbGP43 genotype. Microbes Infect. 7 55–65 [DOI] [PubMed] [Google Scholar]
- Cisalpino P. S., Puccia R., Yamauchi L. M., Cano M. I., da Silveira J. F., Travassos L. R. (1996). Cloning, characterization, and epitope expression of the major diagnostic antigen of Paracoccidioides brasiliensis. J. Biol. Chem. 271 4553–4560 [DOI] [PubMed] [Google Scholar]
- Demicheli M. C., Goes A. M, Andrade A. S. R. (2007). Ultrastructural changes in Paracoccidioides brasiliensis yeast cells attenuated by gamma irradiation. Mycoses 50 397–402 [DOI] [PubMed] [Google Scholar]
- Demicheli M. C., Reis B. S., Goes A.M, de Andrade A. S. (2006). Paracoccidioides brasiliensis: attenuation of yeast cells by gamma irradiation. Mycoses 49 184–189 [DOI] [PubMed] [Google Scholar]
- Diniz S. N., Reis B. S., Goes T. S., Zouain C. S., Leite M. F., Goes A. M. (2004). Protective immunity induced in mice by FO and FII antigens purified from Paracoccidioides brasiliensis. Vaccine 22 485–492 [DOI] [PubMed] [Google Scholar]
- do Nascimento Martins E. M., Reis B. S., de Resende M. A., de Andrade A. S. R., Goes A. M. (2009). Mice immunization with radioattenuated yeast cells of Paracoccidioides brasiliensis: influence of the number of immunizations. Mycopathologia 168 51–58 [DOI] [PubMed] [Google Scholar]
- do Nascimento Martins E. M., Reis B. S., Fernandes V. C., Costa M. M., Goes A. M, de Andrade A. S. (2007). Immunization with radioattenuated yeast cells of Paracoccidioides brasiliensis induces a long lasting protection in BALB/c mice. Vaccine 25 7893–7899 [DOI] [PubMed] [Google Scholar]
- Fernandes V. C., Martins E. M., Boeloni J. N., Coitinho J. B., Serakides R., Goes A. M. (2011). The combined use of Paracoccidioides brasiliensis Pb40 and Pb27 recombinant proteins enhances chemotherapy effects in experimental paracoccidioidomycosis. Microbes Infect. 13 1062–1072 [DOI] [PubMed] [Google Scholar]
- Fernandes V. C., Martins E. M., Boeloni J. N., Serakides R., Goes A. M. (2012). Protective effect of rPb40 as an adjuvant for chemotherapy in experimental paracoccidioidomycosis. Mycopathologia. 10.1007/s11046-012-9530-2 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Ferreira K. S., Maranhão A. Q., Garcia M. C., Brígido M. M., Santos S. S., Lopes J. D., Almeida S. R.(2011). Dendritic cells transfected with scFv from Mab 7.B12 mimicking original antigen gp43 induces protection against experimental paracoccidioidomycosis. PLoS ONE 6 e15935 10.1371/journal.pone.0015935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco M., Peracoli M. T., Soares A., Montenegro R., Mendes R. P., Meira D. A. (1993). Host–parasite relationship in paracoccidioidomycosis. Curr. Top. Med. Mycol. 5 115–149 [PubMed] [Google Scholar]
- Iwai L. K., Yoshida M., Sadahiro A., da Silva W. R., Marin M. L., Goldberg A. C., Juliano M. A., Juliano L., Shikanai-Yasuda M. A., Kalil J., Cunha-Neto E., Travassos L. R. (2007). T-cell recognition of Paracoccidioides brasiliensis gp43-derived peptides in patients with paracoccidioidomycosis and healthy individuals. Clin. Vaccine Immunol. 14 474–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwai L. K., Yoshida M., Sidney J., Shikanai-Yasuda M. A., Goldberg A. C., Juliano M. A., Hammer J., Juliano L., Sette A., Kalil J., Travassos L. R., Cunha-Neto E. (2003). In silico prediction of peptides binding to multiple HLA-DR molecules accurately identifies immunodominant epitopes from gp43 of Paracoccidioides brasiliensis frequently recognized in primary peripheral blood mononuclear cell responses from sensitized individuals. Mol. Med. 9 209–219 [PMC free article] [PubMed] [Google Scholar]
- Magalhães A., Ferreira K. S., Almeida S. R., Nosanchuk J. D., Travassos L. R., Taborda C. P. (2012). Prophylactic and therapeutic vaccination using dendritic cells primed with peptide 10 derived from the 43-kilodalton glycoprotein of Paracoccidioides brasiliensis. Clin. Vaccine Immunol. 19 23–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques A. F., da Silva M. B., Juliano M. A., Muñoz J. E., Travassos L. R., Taborda C. P. (2008). Additive effect of P10 immunization and chemotherapy in anergic mice challenged intratracheally with virulent yeast of Paracoccidioides brasiliensis. Microbes Infect. 10 1251–1258 [DOI] [PubMed] [Google Scholar]
- Marques A. F., da Silva M. B., Juliano M. A., Travassos L. R., Taborda C. P. (2006). Peptide immunization as an adjuvant to chemotherapy in mice challenged intratracheally with virulent yeast cells of Paracoccidioides brasiliensis. Antimicrob. Agents Chemother. 50 2814–2819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattos Grosso D., Almeida S. R., Mariano M., Lopes J. D. (2003). Characterization of gp70 and anti-gp70 monoclonal antibodies in Paracoccidioides brasiliensis pathogenesis. Infect. Immun. 71 6534–6542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matute D. R., McEwen J. G., Puccia R., Montes B. A., San-Blas G., Bagagli E., Rauscher J. T., Restrepo A., Morais F., Niño-Vega G., Taylor J. W. (2006). Cryptic speciation and recombination in the fungus Paracoccidioides brasiliensis as revealed by gene genealogies. Mol. Biol. Evol. 23 65–73 [DOI] [PubMed] [Google Scholar]
- Mayorga O., Muñoz J. E., Lincopan N., Teixeira A. F., Ferreira L. C., Travassos L. R., Taborda C. P. (2012). The role of adjuvants in therapeutic protection against paracoccidioidomycosis after immunization with the P10 peptide. Front. Microbiol. 3:154 10.3389/fmicb.2012.00154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen J. G., Garcia A. M., Ortiz B. L., Botero S., Restrepo A. (1995). In search of the natural habitat of Paracoccidioides brasiliensis. Arch. Med. Res. 26 305–306 [PubMed] [Google Scholar]
- Pavanelli W. R., Kaminami M. S., Geres J. R., Sano A., Ono M. A., Camargo I. C., Itano E. N. (2007). Protection induced in BALB/c mice by the high-molecular-mass (hMM) fraction of Paracoccidioides brasiliensis. Mycopathologia 163 117–128 [DOI] [PubMed] [Google Scholar]
- Pinto A. R., Puccia R., Diniz S. N., Franco M. F., Travassos L. R. (2000). DNA-based vaccination against murine paracoccidioidomycosis using the gp43 gene from Paracoccidioides brasiliensis. Vaccine 18 3050–3058 [DOI] [PubMed] [Google Scholar]
- Prado M., Silva M. B., Laurenti R., Travassos L. R., Taborda C. P. (2009). Mortality due to systemic mycoses as a primary cause of death or in association with AIDS in Brazil: a review from 1996 to 2006. Mem. Inst. Oswaldo Cruz 104 513–521 [DOI] [PubMed] [Google Scholar]
- Puccia R., Schenkman S., Gorin P. A., Travassos L. R. (1986). Exocellular components of Paracoccidioides brasiliensis: identification of a specific antigen. Infect. Immun. 53 199–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puccia R., Travassos L. R. (1991). The 43-kDa glycoprotein from the human pathogen Paracoccidioides brasiliensis and its deglycosylated form: excretion and susceptibility to proteolysis. Arch. Biochem. Biophys. 289 298–302 [DOI] [PubMed] [Google Scholar]
- Reis B. S., Fernandes V. C., Martins E. M., Serakides R., Goes A. M. (2008). Protective immunity induced by rPb27 of Paracoccidioides brasiliensis. Vaccine 26 5461–5469 [DOI] [PubMed] [Google Scholar]
- Restrepo A. (1985). The ecology of Paracoccidioides brasiliensis: a puzzle still unsolved. Sabouraudia 23 323–334 [PubMed] [Google Scholar]
- Ribeiro A. M., Bocca A. L., Amaral A. C., Faccioli L. H., Galetti F. C., Zárate-Bladés C. R., Figueiredo F., Silva C. L., Felipe M. S. (2009). DNAhsp65 vaccination induces protection in mice against Paracoccidioides brasiliensis infection. Vaccine 27 606–613 [DOI] [PubMed] [Google Scholar]
- Ribeiro A. M., Bocca A. L., Amaral A. C., Souza A. C., Faccioli L. H., Coelho-Castelo A. A., Figueiredo F., Silva C. L., Felipe M. S. (2010). HSP65 DNA as therapeutic strategy to treat experimental paracoccidioidomycosis. Vaccine 28 1528–1534 [DOI] [PubMed] [Google Scholar]
- Rittner G. M., Muñoz J. E., Marques A. F., Nosanchuk J. D., Taborda C. P., Travassos L. R. (2012). Therapeutic DNA vaccine encoding peptide P10 against experimental paracoccidioidomycosis. PLoS Negl. Trop. Dis. 6 e1519 10.1371/journal.pntd.0001519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues E. G., Travassos L. R. (1994). Nature of the reactive epitopes in Paracoccidioides brasiliensis polysaccharide antigen. J. Med. Vet. Mycol. 32 77–81 [PubMed] [Google Scholar]
- Saraiva E. C., Altemani A., Franco M. F., Unterkircher C. S., Camargo Z. P. (1996). Paracoccidioides brasiliensis-gp43 used as paracoccidioidin. J. Med. Vet. Mycol. 34 155–161 [DOI] [PubMed] [Google Scholar]
- Shikanai-Yasuda M. A. (2005). Pharmacological management of paracoccidioidomycosis. Expert Opin. Pharmacother. 6 385–397 [DOI] [PubMed] [Google Scholar]
- Shikanai-Yasuda M. A., Telles-Filho F. Q., Mendes R. P., Colombo A. L., Moretti M. L. (2006). Guidelines in paracoccidioidomycosis. Rev. Soc. Bras. Med. Trop. 39 297–310 [DOI] [PubMed] [Google Scholar]
- Taborda C. P., Juliano M. A., Puccia R., Franco M., Travassos L. R. (1998). Mapping of the T-cell epitope in the major 43-kilodalton glycoprotein of Paracoccidioides brasiliensis which induces a Th-1 response protective against fungal infection in BALB/c mice. Infect. Immun. 66 786–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taborda C. P., Nakaie C. R., Cilli E. M., Rodrigues E. G., Silva L. S., Franco M. F., Travassos L. R. (2004). Synthesis and immunological activity of a branched peptide carrying the T-cell epitope of gp43, the major exocellular antigen of Paracoccidioides brasiliensis. Scand. J. Immunol. 59 58–65 [DOI] [PubMed] [Google Scholar]
- Teixeira M. M., Theodoro R. C., de Carvalho M. J., Fernandes L., Paes H. C., Hahn R. C., Mendonza L., Bagagli E., San-Blas G., Felipe M. S. (2009). Phylogenetic analysis reveals a high level of speciation in the Paracoccidioides genus. Mol. Phylogenet. Evol. 52 273–283 [DOI] [PubMed] [Google Scholar]
- Travassos L. R., Rodrigues E. G., Iwai L. K., Taborda C. P. (2008). Attempts at a peptide vaccine against paracoccidioidomycosis, adjuvant to chemotherapy. Mycopathologia 165 341–352 [DOI] [PubMed] [Google Scholar]
- Travassos L. R., Taborda C. P. (2011). Paracoccidioidomycosis: advances in treatment incorporating modulators of the immune response. J. Invasive Fungal Infect. 5 1–6 [Google Scholar]
- Travassos L. R., Taborda C. P., Iwai L. K., Cunha Neto E., Puccia R. (2004a). “The gp43 from Paracoccidioides brasiliensis: a major diagnostic antigen and vaccine candidate,” in The Mycota XII, Human Fungal Pathogens eds Domer J.E., Kobayashi G. S.(Berlin: Springer-Verlag; ) 279–296 [Google Scholar]
- Travassos L. R., Casadevall A., Taborda C. P. (2004b). “Immunomodulation and immunoprotection in fungal infections: humoral and cellular immune responses,” in Pathogenic Fungi: Host Interactions and Emerging Strategies for Control eds (Norfolk: Caister Academic Press; ) 241–283 [Google Scholar]
- Xander P., Vigna A. F., Feitosa Ldos S., Pugliese L., Bailão A. M., Soares C. M., Mortara R. A., Mariano M., Lopes J. D. (2007). A surface 75-kDa protein with acid phosphatase activity recognized by monoclonal antibodies that inhibit Paracoccidioides brasiliensis growth. Microbes Infect. 9 1484–1492 [DOI] [PubMed] [Google Scholar]