Abstract
Among the myriad emergencies that could arise in the dental clinical setting there are a few that occur occasionally despite being entirely preventable. Ingestion or aspiration of dental materials, appliances, or instruments comprises this category. Regardless of incidence, foreign body ingestion or aspiration episodes are recognized as potential complications in the specialty of orthodontics. Despite their infrequent occurrence, the morbidity from a single incident and the amount of specialty medical care that may be needed to manage such incidents is too high to ignore. There is also the associated risk of malpractice litigation given the fact that these incidents are preventable. At present, no clear guidelines exist regarding prevention of this emergency in practice. This article attempts to review relevant literature and aims to formulate certain recommendations based on best available evidence to minimize the incidence of such events, while also suggesting guidelines toward making their management more effective. A flow chart outlining management options and strategies to aid the clinician in the event of such an emergency is also presented.
Keywords: foreign bodies, ingestion, orthodontics, respiratory aspiration, orthodontic appliances
Introduction
Ingestion or aspiration of foreign bodies is recognized as a complication in all clinical specialties of dentistry.1 While a wide variety of complications resulting from foreign bodies (FBs) have been documented in clinical practice, broken orthodontic appliances or components and dentures account for the majority of sharp objects ingested by adults in the dental setting. Whereas most FBs pass through uneventfully, some become impacted, often in the esophagus, and have the potential to cause serious complications. Aspiration, fortunately though less common, is associated with higher morbidity and mortality rates. Apart from the physical strain involved, such events are also a source of emotional distress to patients and their families. It is thus evident that accidental ingestion or aspiration of orthodontic appliances or their component parts could pose problems, especially if they obstruct the airway or gastrointestinal tract. Despite the frequency and seriousness of this issue (as seen by the increasing number of case reports in the literature), there is a general lack of consensus on the best possible treatment approach for clinicians confronted with this emergency in the clinical context.
This review aims to develop a rational and systematic procedure in managing such cases by taking into account findings in the orthodontic literature. We begin with an overview of the types of appliances most prone to cause problems and usual sites of impaction at the time of presentation and then formulate an organized line of management in the event of an emergency. Finally, we review various treatment options and conclude with recommendations that can be implemented in clinical practice in order to minimize the occurrence of such events. A management flowchart that can aid the clinician as a ready source of reference has also been formulated.
Reported incidence in the literature
Accidental foreign body ingestion or aspiration is usually handled by physicians in the Accident and Emergency units. A sizeable proportion of those affected are children (80%) below 3 years of age.2 While food materials constitute the majority of foreign bodies found in the airway in children,2 loose dentures, broken orthodontic appliances, or components and dental instruments are the second most commonly ingested objects in adults.3 The reported incidence of swallowing objects of dental origin varies considerably in the literature. In a review by Tamura et al4 in Japan, the range was reported as being between 3.6% and 27.7% of all foreign bodies, with a considerably higher incidence in adults than children. Among all dental specialties, fixed prosthodontic therapy had the highest incidence of adverse outcomes followed by orthodontic treatment.3 Kurkciyan et al5 in 1996 observed that dental procedures involving single tooth cast or prefabricated restorations involving cementation had a higher likelihood of aspiration. In the same study they found ingestion to be more prevalent than aspiration. Published literature that addresses ingestion or aspiration of dental instruments, materials, or prostheses is replete with case reports and descriptions of individual adverse events. Numerous case reports have demonstrated the potentially disastrous complications due to FBs in orthodontic practice. While enumerating the various factors possibly influencing the occurrence of this emergency, complicating sequelae, and their management, we decided that the twin issues of ingestion and aspiration are better addressed together for ease of comparison and sake of clarity.
Types of appliances ingested or aspirated in orthodontics
Although the actual incidence of this complication in orthodontics is speculative, there is considerable variation as to the types of appliances involved. The reported objects include a lower spring retainer,6 fractured twin block appliance,7 expansion keys,8,9 fragment of maxillary removable appliance,10 retainer,11 transpalatal arch,12 and pieces of archwire.13 A rare case of accidental swallowing of a removable quadhelix by a 13-year-old boy affected by Down’s syndrome, which necessitated surgical removal, has also been reported.14 These reports testify that removable appliances are not the only orthodontic appliances that can cause problems. Although no single appliance or procedure has been associated with an increased risk of ingestion; the miniature size of orthodontic components in the presence of saliva coupled with limited working access in posterior segments may be contributing factors. The fact that it is practically untenable to use rubber dams during routine orthodontic treatment compounds this risk. However, gauze throat screens are a feasible alternative and can be used while bonding palatal attachments, although if these screens are placed too far posterior, it could prove uncomfortable for the patient and elicit the gag reflex.
Position of the patient
For the routine delivery of orthodontic care, the general trend is to treat patients in a supine position to improve access to the oral cavity and additionally improve the ergonomic comfort for the clinician. Although it seems obvious that there may be a greater risk of objects entering the oropharynx in this position,15,16 Neuhauser17 suggested that the supine patient is prevented from swallowing and hence there is less chance of accidental aspiration or ingestion. Accidents, however, are always possible when treating patients in any position.
Sites of impaction and related symptoms
Along the gastrointestinal tract (ingestion)
The majority of foreign bodies entering the oropharynx will pass through the alimentary canal uneventfully.18 Although complications are higher with sharp components, reported rates of gastrointestinal perforation still remain rare at less than 1%.19–21 Ghori et al22 reported on a swallowed dental plate that went unnoticed and caused perforation of the sigmoid colon, ultimately proving lethal to the patient. Usually, only large objects and those with sharp edges are likely to become impacted, and if impaction does occur it is usually at the level of the fourth cervical vertebra. The authors had previously reported a case of laryngeal impaction of an archwire segment following accidental ingestion during orthodontic adjustment that necessitated endoscopic retrieval in the hospital.23 Patient presentations vary, although dysphagia and odynophagia are the most frequently reported symptoms.24,25 Other features may include a history of FB ingestion, persistent presence of FB sensation, chest pain, drooling of saliva, muscle incoordination, incessant twitching, hematemesis, vomiting, or regurgitation that may be construed as symptoms of esophageal obstruction. The commonest sites for perforation are the ileo-cecal junction and the sigmoid colon. Once here, the symptoms vary between abdominal pain, fever, nausea, vomiting, and abdominal distension that may complicate diagnosis.20 The time taken for an FB to traverse the intestinal tract can also vary from anywhere between 2 and 12 days.6
Along the respiratory tract (aspiration)
Despite being less common than ingestion, aspirated foreign bodies are emergency situations and require timely management because of the potentially life threatening complications they pose. The presenting symptoms are dependent on the site where the object becomes impacted. If it gets trapped above the level of the vocal cords, acute respiratory distress can result. Smaller objects tend to pass through the vocal cords and do not cause upper airway obstruction.26 The most common symptoms of laryngo-tracheal FBs are dyspnea, cough, and stridor; while bronchial FBs are associated with cough, decreased air entry, dyspnea, and wheezing.27 Inability to talk and coughing forcefully with the patient’s hands clutched to the throat may be the earliest sign of choking. A partial blockage can quickly become life threatening if the patient cannot breathe properly. Hoarseness may accompany laryngeal obstruction with or without cyanosis depending on whether the obstruction is partial or complete.28 Initial symptoms can subside or small FBs may go unrecognized until later when complications, like pneumonia, atelectasis, or bronchiectasis, develop. Retrieval of the FB in such instances can be further complicated by granulation or scar tissue formation.29
Management
Management of this emergency in the clinic is the most critical aspect should it occur, and it is this area that is shrouded in the greatest controversy. Even with the myriad management techniques available today, there exists significant debate about the appropriate procedures to be followed. A variety of management options are available. However, the clinician will need to confirm that accidental ingestion or aspiration may have occurred by elucidating a proper history.
Positive history
If this occurs outside the confines of the clinic, a positive history can often be elicited. However, it should be noted that a negative history in itself does not exclude FB swallowing, and a high degree of suspicion should be maintained in children and impaired adults with missing orthodontic appliance fragments or components.
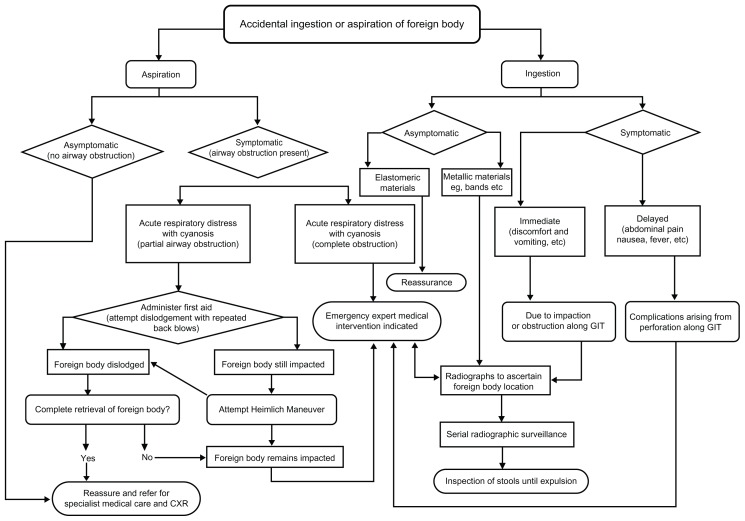
The clinician would primarily need to assess and ascertain whether the FB has been ingested or aspirated by the patient. In either situation, the subject may show symptoms or be entirely asymptomatic. The specific steps undertaken by the clinician should be based on the clinical situation. The major management options are outlined below and the flowchart (Figure 1) represents a source of ready reference that can be used by clinicians as a guide to management in the event of such emergencies.
Figure 1.
A flowchart for management of ingestion or aspiration can aid clinicians to make instant decisions in the event of this emergency.
Abbreviation: CXR, chest radiograph; GIT, gastrointestinal tract.
Clinical retrieval
Should an object be dropped into the mouth of a supine patient, the head may be turned to one side to encourage the object to fall into the cheek rather than the oropharynx.16 The oral cavity and oropharynx should next be examined under good illumination and if the object is visible, it should be retrieved with forceps or high-volume suction. The most readily visible area that lends itself to FB entrapment is the supra-tonsillar recess followed by the epiglottic vallecula and the piriform recess. If it cannot be seen in these areas, it may be assumed that the object has either been swallowed or aspirated.30 The FB type, nature, and duration of symptoms are all useful indicators regarding the lodgment site and the need for immediate intervention.
Observation and radiographic assessment
In noncritical cases, it is prudent to adopt a wait and watch approach in order to ascertain if the FB can be expelled of its own accord. Observation is generally indicated for asymptomatic patients with a positive history of non-threatening FB ingestion over periods of less than 24 hours and without any respiratory symptoms.24 A chest radiograph, although not mandatory, is recommended. However, if the FB is known to be a radiolucent object (eg, acrylic), radiography as a diagnostic means for localization may be ruled out. The patient should be asked for any areas of discomfort or made to swallow to determine the approximate site of lodgment. Occasionally, patients have been advised to supplement their diet with a large amount of cellulose, which theoretically could aid the passage of the object through the gut.17,31 For radiolucent objects, ingestion of cotton wool pellets mixed with small amounts of barium sulfate suspension has been reported to form a radio-opaque bolus around the object, which allows it to be tracked through the gut radiographically.32 Smaller radio-opaque objects that have passed on should be managed conservatively by serial radiographic surveillance and inspection of stools.
Non-invasive emergency measures
Unlike ingested FBs, treatment of aspirated FBs demands urgent attention and is dependent on the severity of presenting symptoms. Complete blockage constitutes a medical emergency. Cyanosis, loss of consciousness, and permanent brain damage occurs within 4 to 6 minutes if the obstruction is not relieved. Therefore, speed and updated cardiopulmonary resuscitation (CPR) skills are vital on the part of the clinician. If the FB is obstructive and the patient is in respiratory distress, dislodgement should initially be attempted with back blows and abdominal thrusts (Heimlich maneuver).15,26,32,33 If this fails to dislodge the object, positive airway pressure needs to be maintained by artificial respiration until emergency services arrive.
Invasive emergency measures
Should conservative methods prove unsuccessful, the object should be bypassed and an emergency airway established (by an experienced medical practitioner). Even if the object has passed the vocal cords and there is no sign of airway obstruction, the patient should still be referred for immediate medical attention.18 Although spontaneous expectoration of inhaled foreign bodies is known to occur in 1%–2% of cases,34 it is recommended not to wait for this to happen but to treat all such cases with extreme urgency. If the airway is not compromised, the patient must be escorted to the hospital for clinical and radiographic examinations to identify the location of the object for planning the means of retrieval. Complications have been estimated to occur in 6% of cases of aspiration, with mortality being a serious but rare outcome.27
The most prevalent emergency diagnostic and management method for lodged esophageal and tracheal FBs is endoscopy. Forward viewing flexible pan endoscopy can be performed under local anesthesia and is best suited for intrathoracic objects24 and is available in most tertiary medical centers. This is preferred to rigid endoscopy because of lower complication rates.
Another established procedure that is relatively safe and more cost effective is the use of Foley’s catheter. This involves passing a balloon distal to the ingested object, usually under fluoroscopic guidance, inflating the balloon, and then withdrawing the catheter along with the object proximally.
Surgical intervention
Surgery, often the last resort and although rarely performed, is relatively successful. Gastrointestinal perforation or lodgment in the airway, presence of other complicating factors, and failure to remove the FB by other preceding techniques are all indications for surgical intervention.
Recommendations for prevention
The adage “An ounce of prevention is worth more than a pound of cure” may sound clichéd but is relevant when it comes to preventing such incidents. Dentistry, as such and orthodontics in particular, poses a high risk of ingestion or inhalation of materials and appliance components. Therefore any attempt at prevention should be aimed at securing potentially loose orthodontic components in the mouth during all procedures. Precautions that may be followed to minimize such incidents include the following recommendations.
Patient selection
There is a need to be extra vigilant during the initial consult appointment with special-needs patients or very young children. These groups are often unable to comprehend instructions given by the orthodontist. It is the legal responsibility of the clinician to individually assess the degree of cooperation that can be gleaned from the patient and the support afforded by their parents or guardians. The orthodontist must ensure complete cooperation and active involvement of parents in constantly supervising their children to ensure that professional instructions are respected. This is important from a medical–legal standpoint. Rarely, the clinician may opt to delay treatment (until patients are older in the latter case) or not provide treatment at all on legal grounds. Reasons for doing so will have to be made clear so that the parties are aware of the risks involved, and this may help avoid fallouts later.
General precautions
Use of textured latex gloves may help improve grip on instruments and orthodontic components, like bands etc.35,36
The orthodontist must ensure adequate retention and integrity of the appliance at each appointment before and after the planned adjustment.
Patient advice should include both verbal and written instructions at the time of appliance placement that they should not try to reseat damaged, ill-fitting, or broken fragments of any appliance, but instead see the orthodontist to have the appliance checked.7
All practices should take into account the possibility of such an emergency in their standard operating procedures and be well prepared for any contingencies. Staff must be trained to recognize emergencies, and individual responsibilities must be delegated to offset any confusion in the event of an emergency.
Every orthodontist must undergo a basic life support and first-aid skills course. Updating and honing these skills at least once every 2 years is recommended as CPR recommendations are updated every 5 years.
Precautions with fixed appliances
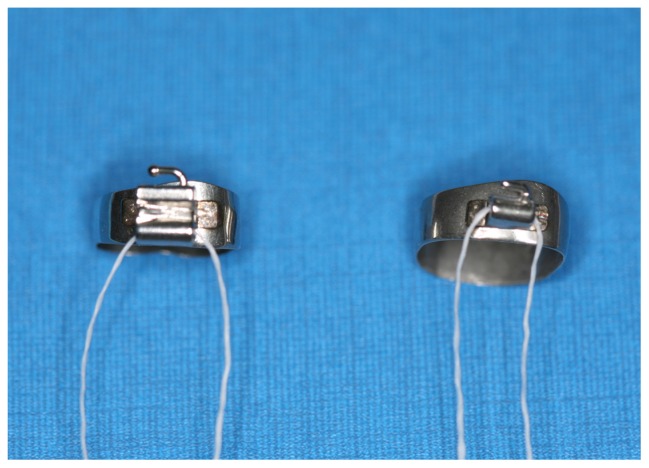
Bands could be secured by an adequate length of floss through the molar tubes and the free ends left outside the mouth, especially while banding the second molars (Figure 2).
Use of bondable tubes and attachments increases the risk of these attachments being inhaled or swallowed if they are dislodged, so it is advisable to cinch the archwire whenever possible.
Use of a gauze pad as protection distal to the archwire or appliance will prevent injury to the mucosa as well as trap any stray wires that fail the “safety hold” of the pliers.
High-volume suction should be used while attempting procedures such as banding and bonding of teeth.
Cutting tips of instruments must be periodically checked for any sign of “wear or work fatigue.” Damaged tips must be replaced.
Removable quadhelices and transpalatal arches must be tethered by a floss during placement and additionally reinforced at the point of attachment (in palatal sheaths), using elastomeric ligatures and or preferably stainless steel ligatures (Figure 3).
During appliance debond, it may be less risky if the brackets removed are allowed to remain attached to the base archwire.
Micro-implants must be adequately harbored by steel ligatures to the main appliance through eyelets of the implant (if present); if Nitinol springs are planned for use in retraction the clinician must ensure proper attachment to the appliance.
Archwires must be trimmed approximately using study models or a fresh wax arch template obtained from the patient so that not more than 5 mm of length will remain beyond the last molar buccal tube(s).
A visual check of the cutting ends of distal cutters for trapped wires and wiping with sterile gauze after every cut is recommended.
Figure 2.
Prefabricated bands prior to placement in the mouth being secured with an adequate length of floss as a precaution.
Figure 3.
A removable quadhelix on a patient’s model just prior to placement that has been tethered with a length of floss to preclude any emergency.
Precautions with removable appliances
All metal retentive components should be inspected at every appointment for any sign of fracture due to repeated wear. Refabrication of the appliance is indicated if this is observed.
The acrylic plate(s) should be inspected for cracks due to crazing or thinned-out areas, especially on load-bearing surfaces to preclude accidental damage to appliance during use.
It is recommended that the acrylic used to fabricate the appliance be preferably radio-opaque. This will facilitate easier localization in the event of ingestion of the appliance or part(s) thereof.31
Developing guidelines and effecting changes in postgraduate curriculum
Orthodontic treatment duration usually spans from a few months to a few years. During treatment it is common to have patients report missing or swallowed rubber rings. These elastomeric materials if swallowed usually remain asymptomatic. As clinicians, we tend to take such incidents lightly, and this is probably one reason why accidental ingestion and aspiration is one of the most under reported and ignored topics in our specialty. We strongly feel that the current reported incidence may not reflect the actual numbers in clinical practice. Most cases go unreported as there is no legal body that collects reports on such events. However, metallic orthodontic components (particularly sharps) may pose a potential hazard if ingested or aspirated, and it is adverse events like these that have obvious healthcare implications. Albeit their infrequent occurrence, the potential morbidity associated with any single incident is too great to be ignored. This is especially true from the viewpoint of the degree of specialty medical care and resources needed to manage such incidents, the associated high financial cost, as well as the risk of malpractice litigation.23 The morbidity as a result assumes significance when one considers that aspiration and ingestion are entirely preventable. From the clinician’s viewpoint, a single such episode can result in disruption of the normal clinical schedule and can be quite psychologically upsetting. There is the possibility of being potentially liable for negligence and malpractice.
On the other hand, the aspect that is most often ignored in the existing literature is the psychological impact that the event may have on patients and their family members. Development of a phobic attitude toward continuation of treatment and possible loss of operator trust on part of the patient are probable outcomes. Therefore, we feel the best approach to this problem lies in developing standard operating guidelines for preventing such emergencies. We suggest that such complications during orthodontic treatment should be made aware to novice postgraduate trainees prior to embarking on their clinical training. We also strongly recommend that methods for prevention (by ensuring adherence to recommended precautions) and management options in the event of an emergency be mandatorily included as part of an emergency management module in postgraduate training programs.
Conclusion
To summarize, the relevance of the aforementioned situations among possible clinical emergencies is that they comprise a subgroup that are totally preventable. Conscientious patient selection, meticulous adherence to clinical procedures, periodic inspection of instruments and appliances for wear and timely replacement if warranted, appropriate use of high-volume suction during high-risk procedures, as well as proper patient education are all vital factors in prevention. If despite following standard operating procedures, an emergency situation does arise, the clinician must be capable of recognizing and managing it early and effectively so that patient discomfort and morbidity may be kept minimal. In this litigious era, it is our recommendation that appropriate consideration be given to the inclusion of such emergencies and their management in contemporary graduate curricula.
Clinical relevance of this paper
The actual incidence of accidental ingestion and aspiration of orthodontic consumables, materials, and appliances during treatment is often under reported in our specialty. The current data available may not reflect the actual numbers in practice. This may be due to a number of factors ranging from the fact that there is no central authority to collect data on such incidents and that the average orthodontist is not usually very concerned until faced with such an emergency. In this litigious day and age, it is our recommendation that appropriate consideration be given to the inclusion of such emergencies and their management in contemporary graduate curricula.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Milton TM, Hearing SD, Ireland AJ. Ingested foreign bodies associated with orthodontic treatment: report of three cases and review of ingestion/aspiration incident management. Br Dent J. 2001;190(11):592–596. doi: 10.1038/sj.bdj.4801046. [DOI] [PubMed] [Google Scholar]
- 2.Aytaç A, Yurdakul Y, Ikizler C, Olga R, Saylam A. Inhalation of foreign bodies in children. Report of 500 cases. J Thorac Cardiovasc Surg. 1977;74(1):145–151. [PubMed] [Google Scholar]
- 3.Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: a 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287–1291. doi: 10.14219/jada.archive.2004.0404. [DOI] [PubMed] [Google Scholar]
- 4.Tamura N, Nakajima T, Matsumoto S, Ohyama T, Ohashi Y. Foreign bodies of dental origin in the air and food passages. Int J Oral Maxillofac Surg. 1986;15(6):739–751. doi: 10.1016/s0300-9785(86)80116-8. [DOI] [PubMed] [Google Scholar]
- 5.Kürkciyan I, Frossard M, Kettenbach J, Meron G, Sterz F, Röggla M, et al. Conservative management of foreign bodies in the gastrointestinal tract. Z Gastroenterol. 1996;34(3):173–177. [PubMed] [Google Scholar]
- 6.Hinkle FG. Ingested retainer: a case report. Am J Orthod Dentofacial Orthop. 1987;92(1):46–49. doi: 10.1016/0889-5406(87)90295-2. [DOI] [PubMed] [Google Scholar]
- 7.Rohida NS, Bhad WA. Accidental ingestion of a fractured twin-block appliance. Am J Orthod Dentofacial Orthop. 2011;139(1):123–125. doi: 10.1016/j.ajodo.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 8.Nazif MM, Ready MA. Accidental swallowing of orthodontic expansion appliance keys: report of two cases. ASDC J Dent Child. 1983;50(2):126–127. [PubMed] [Google Scholar]
- 9.Tripathi T, Rai P, Singh H. Foreign body ingestion of orthodontic origin. Am J Orthod Dentofacial Orthop. 2011;139(2):279–283. doi: 10.1016/j.ajodo.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 10.Parkhouse RC. Medical complications in orthodontics. Br J Orthod. 1991;18(1):51–57. doi: 10.1179/bjo.18.1.51. [DOI] [PubMed] [Google Scholar]
- 11.Klein AM, Schoem SR. Unrecognized aspiration of a dental retainer: a case report. Otolaryngol Head Neck Surg. 2002;126(4):438–439. doi: 10.1067/mhn.2002.123834. [DOI] [PubMed] [Google Scholar]
- 12.Abdel-Kader HM. Broken orthodontic trans-palatal archwire stuck to the throat of orthodontic patient: is it strange? J Orthod. 2003;30(1):11. doi: 10.1093/ortho/30.1.11. [DOI] [PubMed] [Google Scholar]
- 13.Lee BW. Case report – swallowed piece of archwire. Aust Orthod J. 1992;12(3):169–170. [PubMed] [Google Scholar]
- 14.Allwork JJ, Edwards IR, Welch IM. Ingestion of a quadhelix appliance requiring surgical removal: a case report. J Orthod. 2007;34(3):154–157. doi: 10.1179/146531207225022131. [DOI] [PubMed] [Google Scholar]
- 15.Lanning GE. Accidental aspiration of a cast crown during attempted delivery. J Indiana Dent Assoc. 1988;67(6):22–23. [PubMed] [Google Scholar]
- 16.Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: a review. J Am Dent Assoc. 1996;127(8):1224–1229. doi: 10.14219/jada.archive.1996.0415. [DOI] [PubMed] [Google Scholar]
- 17.Neuhauser W. Swallowing of a temporary bridge by a reclining patient being treated by a seated dentist. Quintessenz. 1975;26(5):19–20. [PubMed] [Google Scholar]
- 18.El Badrawy HE. Aspiration of foreign bodies during dental procedures. J Can Dent Assoc. 1985;2:146–147. [PubMed] [Google Scholar]
- 19.Webb WA, McDaniel L, Jones L. Foreign bodies of the upper gastrointestinal tract: current management. South Med J. 1984;77(9):1083–1086. doi: 10.1097/00007611-198409000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez JG, Gonzalez RR, Patino JV, Garcia AT, Alvarez CP, Pedrosa CS. CT findings in gastrointestinal perforation by ingested fish bones. J Comput Assist Tomogr. 1988;12(1):88–90. doi: 10.1097/00004728-198801000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41(1):39–51. doi: 10.1016/s0016-5107(95)70274-1. [DOI] [PubMed] [Google Scholar]
- 22.Ghori A, Dorricott NJ, Sanders DS. A lethal ectopic denture: an unusual case of sigmoid perforation due to unnoticed swallowed dental plate. J R Coll Surg Edinb. 1999;44(3):203–204. [PubMed] [Google Scholar]
- 23.Umesan UK, Ahmad W, Balakrishnan P. Laryngeal impaction of an archwire segment following accidental ingestion during orthodontic adjustment. Am J Orthod Dentofacial Orthop. 2012 doi: 10.1016/j.ajodo.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 24.Brady PG. Esophageal foreign bodies. Gastroenterol Clin North Am. 1991;20(4):691–701. [PubMed] [Google Scholar]
- 25.Sittitrai P, Pattarasakulchai T, Tapatiwong H. Esophageal foreign bodies. J Med Assoc Thai. 2000;83(12):1514–1518. [PubMed] [Google Scholar]
- 26.Israel HA, Leban SG. Aspiration of an endodontic instrument. J Endod. 1984;10(9):452–454. doi: 10.1016/S0099-2399(84)80268-X. [DOI] [PubMed] [Google Scholar]
- 27.Blazer S, Naveh Y, Friedman A. Foreign body in the airway. A review of 200 cases. Am J Dis Child. 1980;134(1):68–71. doi: 10.1001/archpedi.1980.02130130050015. [DOI] [PubMed] [Google Scholar]
- 28.von Haacke NP, Wilson JA. Missing denture as a cause of recurrent laryngeal nerve palsy. Br Med J (Clin Res Ed) 1986;292(6521):664. doi: 10.1136/bmj.292.6521.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dibiase AT, Samuels RH, Ozdiler E, Akcam MO, Turkkahraman H. Hazards of orthodontics appliances and the oropharynx. J Orthod. 2000;27(4):295–302. doi: 10.1093/ortho/27.4.295. [DOI] [PubMed] [Google Scholar]
- 30.Scott AS, Dooley BE. Displaced post and core in the epiglottic vallecula. Gen Dent. 1978;26(1):26–27. [PubMed] [Google Scholar]
- 31.Absi EG, Buckley JG. The location and tracking of swallowed dental appliances: the role of radiology. Dentomaxillofac Radiol. 1995;24(2):139–142. doi: 10.1259/dmfr.24.2.9515387. [DOI] [PubMed] [Google Scholar]
- 32.Jacobi R, Shillingburg HT., Jr A method to prevent swallowing or aspiration of cast restorations. J Prosthet Dent. 1981;46(6):642–645. doi: 10.1016/0022-3913(81)90072-x. [DOI] [PubMed] [Google Scholar]
- 33.Heimlich HJ. A life-saving maneuver to prevent food-choking. JAMA. 1975;234(4):398–401. [PubMed] [Google Scholar]
- 34.Chatterji S, Chatterji P. The management of foreign bodies in air passages. Anaesthesia. 1972;27(4):390–395. doi: 10.1111/j.1365-2044.1972.tb08243.x. [DOI] [PubMed] [Google Scholar]
- 35.Chua KL, Taylor GS, Bagg J. A clinical and laboratory evaluation of three types of operating gloves for use in orthodontic practice. Br J Orthod. 1996;23(2):115–120. doi: 10.1179/bjo.23.2.115. [DOI] [PubMed] [Google Scholar]
- 36.VanMeter BH, Aggarwal M, Thacker JG, Edlich RF. A new powder-free glove with a textured surface to improve handling of surgical instruments. J Emerg Med. 1995;13(3):365–368. doi: 10.1016/0736-4679(95)00019-7. [DOI] [PubMed] [Google Scholar]