Abstract
The article presents the intervention model and primary outcomes of a preventive intervention designed to reduce anxiety symptoms and prevent the onset of anxiety disorders in the offspring of parents with anxiety disorders. Participants were 40 volunteer children (mean age = 8.94 years; 45% girls; 90% Caucasian) whose parents met criteria for a broad range of anxiety disorders. Families were randomly assigned to an 8-week cognitive–behavioral intervention, the Coping and Promoting Strength program (CAPS; n = 20) or a wait list control condition (WL; n = 20). Independent evaluators (IEs) conducted diagnostic interviews, and children and parents completed measures of anxiety symptoms. Assessments were conducted pre- and postintervention and 6 and 12 months after the postintervention assessment. On the basis of intent to treat analyses, 30% of the children in the WL group developed an anxiety disorder by the 1-year follow-up compared with 0% in the CAPS group. IE and parent-reported (but not child-reported) levels of anxiety showed significant decreases from the preintervention assessment to the 1-year follow-up assessment in the CAPS but not the WL group. Parental satisfaction with the intervention was high. Findings suggest that a family-based intervention may prevent the onset of anxiety disorders in the offspring of parents with anxiety disorders.
Keywords: anxiety disorders, prevention, children
The promise of preventive interventions for reducing the incidence of child psychiatric disorders and promoting well-being has a long history (Greenberg, Domitrovich, & Bumbarger, 2001). The application of prevention science to reduce anxiety disorders, however, is in its infancy. To date, only six published studies have been conducted (all in Australia and all but one school based) and none of these studies have targeted children who are likely to be at the greatest risk for developing an anxiety disorder, namely, the offspring of parents with anxiety disorders.
Family aggregation studies consistently find that anxiety disorders run in families: Children of parents with anxiety disorders are two to seven times more likely to have an anxiety disorder compared with children from families in which neither parent has an anxiety disorder (Beidel & Turner, 1997; Kashani et al., 1990; Merikangas, Dierker, & Szatmari, 1998). Indeed, as many as 65% of children of parents with anxiety disorders meet criteria for an anxiety disorder (Capps, Sigman, Sena, & Henker, 1996; Whaley, Pinto, & Sigman, 1999; Woodruff-Borden, Morrow, Bourland, & Cambron, 2002). Despite the elevated risk to these children, no study has attempted to reduce the incidence of anxiety disorders in this population. The present study addressed this need.
The purpose of the Child Anxiety Prevention Study was to develop and evaluate the efficacy of a preventive intervention designed to reduce anxiety symptoms and prevent the onset of anxiety disorders among children of parents with anxiety disorders. The intervention is theoretically derived and designed to change a set of modifiable risk factors, which, on the basis of prior research and theory, are believed to mediate the development of anxiety disorders in children. In this article, I present the intervention model and primary outcomes.
Method
Participants
Participants were 40 volunteer families. Inclusion criteria for children were that they (a) were between the ages of 7 and 12 years, (b) showed no presence of an anxiety disorder, (c) had no medical or psychiatric conditions contraindicating study intervention (e.g., suicidality), and (d) were not currently receiving treatment for anxiety reduction. Inclusion criteria for parents were (a) the presence of a current or lifetime diagnosis of an anxiety disorder (excluding posttraumatic stress disorder and acute stress disorder) and (b) no medical or comorbid psychiatric condition contraindicating study intervention. All parents met Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) criteria for a current primary anxiety disorder. These disorders were generalized anxiety disorder (n = 22), social phobia (n = 7), panic disorder with agoraphobia (n = 5), panic disorder without agoraphobia (n = 3), specific phobia (n = 2), and obsessive–compulsive disorder (n = 1). In addition, 73% (n = 29) of the parents with anxiety disorders met criteria for a current comorbid disorder. The most common comorbid disorders were anxiety (n = 23) and mood disorders (n = 6). Additional information about the sample appears in Table 1.
Table 1.
Baseline Characteristics of Participants and Group Comparisons
| Characteristic | CAPS | WL | Differences |
|---|---|---|---|
| Child’s M age in years | 9.20 (1.91) | 8.68 (1.81) | t(38) = −0.89 |
| Child gender, % female | 50 (10) | 40 (8) | χ2(1, N = 40) = 0.40 |
| Race or ethnicity, % Caucasian | 80 (16) | 100 (20) | χ2(3, N = 40) = 4.44 |
| Parent’s M age | 41.42 (7.36) | 40.65 (4.28) | t(37) = −0.40 |
| Parents marital status, % married | 75 (15) | 95 (19) | χ2(4, N = 40) = 6.47 |
| Parent’s education, % college | 75 (15) | 85 (17) | χ2(4, N = 40) = 2.22 |
| Family income, % over $80,000/year | 65 (13) | 70 (14) | χ2(6, N = 40) = 6.04 |
| % parents with comorbid diagnoses | 70 (14) | 75 (15) | χ2(1, N = 40) = 0.13 |
| % of anxious parents in treatment | 45 (9) | 70 (14) | χ2(1, N = 40) = 2.56 |
| % of coparents with psychiatric diagnoses | 25 (5) | 25 (5) | χ2(1, N = 40) = 0.00 |
| ADIS–C/P CSR M | 2.10 (0.85) | 2.10 (0.72) | t(38) = 0.00 |
| SCARED, parent total M | 15.23 (7.97) | 18.53 (11.89) | t(37) = 1.01 |
| SCARED, child total M | 24.70 (14.61) | 24.39 (10.24) | t(38) = −0.08 |
Note. CAPS = Coping and Promoting Strength program group; WL = wait list group; ADIS–C/P CSR = Anxiety Disorders Interview Schedule for DSM–IV—Child Version clinical severity rating; SCARED = Screen for Child Anxiety Related Emotional Disorders. For results presented as percentages, the number of respondents for categorical variables and standard deviations for continuous variables are indicated in parentheses.
Measures
Anxiety Disorders Interview Schedule for DSM–IV (ADIS; Brown, DiNardo, & Barlow, 1994)
Parental diagnostic status was assessed using the ADIS. The ADIS has demonstrated internal consistency and interrater reliability (Di Nardo, Moras, Barlow, Rapee, & Brown, 1993). I or a trained postdoctoral fellow made parent diagnoses, and I confirmed all diagnoses at a consensus meeting.
ADIS Child Version (ADIS–C/P; Silverman & Albano, 1996)
The ADIS–C/P was used to determine child diagnoses and was administered by trained evaluators. Parents were generally interviewed first, only composite diagnoses were used, and discrepancies between child and parent reports were reconciled on the basis of the clinical judgment of the independent evaluator (IE) conducting the interview and according to ADIS–C/P guidelines. In the majority of cases, the same IE interviewed both the parent and the child (a different IE interviewed the parent about his or her own disorder). Interrater agreement on a random 20% of the baseline and 10% of the 1- year follow-up composite ADIS–C/P diagnoses was 100%.
Screen for Child Anxiety Related Emotional Disorders—Parent and Child Versions (SCARED; Birmaher et al., 1997, 1999)
The SCARED is a widely used 41-item measure of pediatric anxiety with evidence of reliability and validity (Birmaher et al., 1997, 1999). SCARED total scores were used, derived by summing all 41 items; higher scores reflected higher anxiety. Internal consistency was .91 and .89, respectively, for the child- and parent-report SCARED total scores of the present sample.
Demographic information questionnaire
Demographic information was obtained from the parent with anxiety participating in the study.
Intervention satisfaction
Posttreatment, parents anonymously completed a questionnaire evaluating the intervention. Thirteen items assessed how helpful specific aspects of the program were (e.g., cognitive restructuring) on a 5-point scale ranging from 1= very helpful to 5= very unhelpful, and three items rated overall satisfaction on a 7-point scale ranging from 1 = not at all satisfied to 7 = very satisfied. Parents also responded to open-ended questions about the most and least helpful aspects of the program.
Coping and promoting strength program (CAPS) description
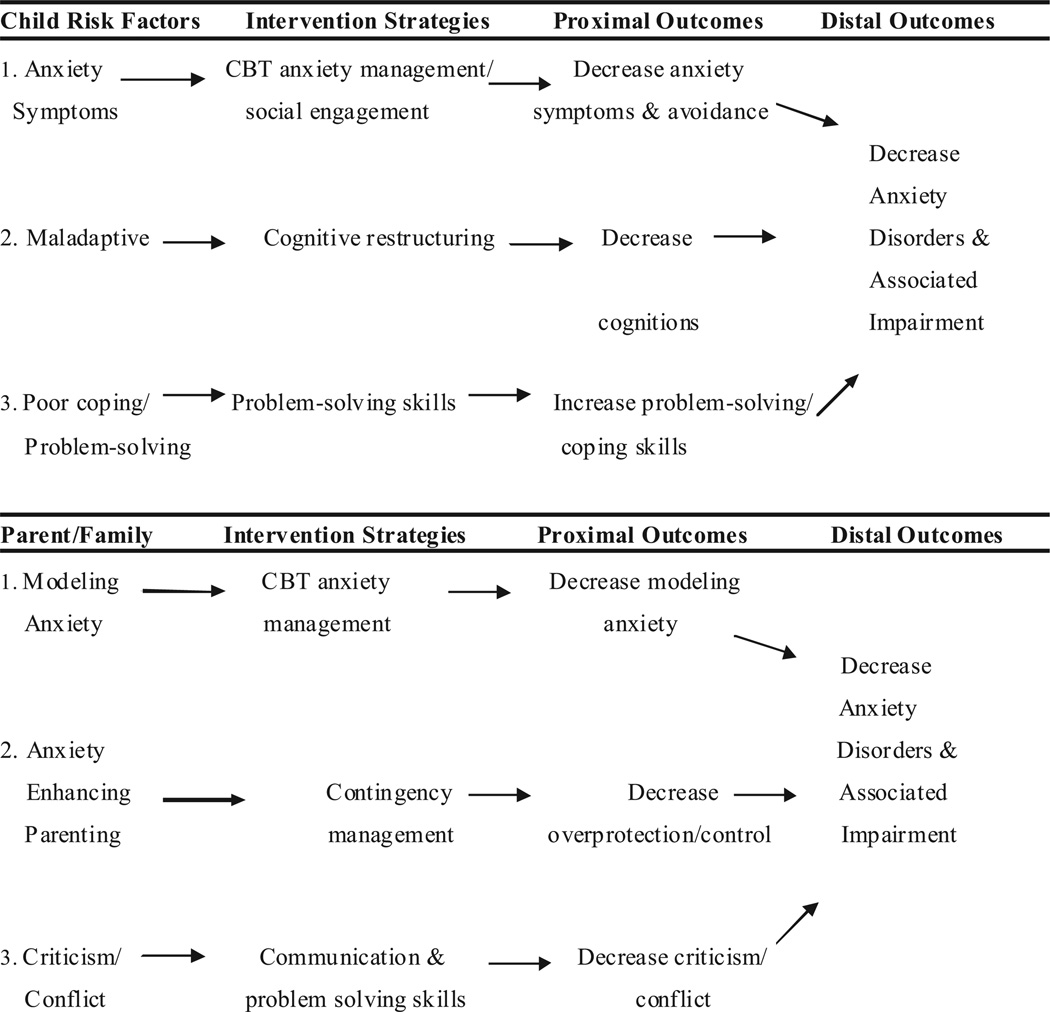
Briefly, the development of the CAPS intervention was guided by the following principles: (a) increasing children’s strength and resilience by teaching specific skills (e.g., problem solving); (b) reducing known risk factors associated with the onset and maintenance of anxiety in children (e.g., parental overprotection), and (c) increasing knowledge of anxiety and its disorders to improve communication among family members, instill hope, and help the child and family make sense of the parental illness. The intervention components and their sequencing were based largely on cognitive–behavioral treatment found to be effective with clinically anxious youth (Silverman et al., 1999) as well as Beardslee’s family-based intervention for the offspring of depressed parents (Beardslee, Gladstone, Wright, & Cooper, 2003). Figure 1 presents the intervention model. As can be seen in the figure, three child and three parent modifiable risk factors were specifically targeted. The targeted child risk factors were (a) elevated anxiety symptoms and social avoidance, (b) maladaptive cognitions, and (c) deficits in coping and problem solving. The targeted parent risk factors were (a) modeling of anxiety symptoms, (b) anxiety-enhancing parenting practices, and (c) criticism and family conflict (i.e., deficits in communication and problem-solving skills) among family members.
Figure 1.
Coping and Promoting Strength program conceptual model and intervention strategies. CBT = cognitive–behavioral therapy.
Intervention format
The CAPS intervention consisted of 6–8 weekly sessions and 3 monthly booster sessions; each session was approximately 60 min in length. The sequence of intervention strategies was based on the transfer of control model (Ginsburg, Silverman, & Kurtines, 1995; Silverman & Kurtines, 1996). Consistent with this model, the first two sessions were with parents alone, and subsequent sessions included all interested family members.
Therapists and intervention adherence
Two postdoctoral psychology fellows and I served as the therapists. I delivered the intervention to all but 6 families. Because this was a pilot study, intervention adherence was not formally evaluated. A detailed session-by-session intervention manual with session handouts, weekly supervision, and weekly progress notes documenting the content of each session that I reviewed weekly were used to enhance adherence.
IEs
IEs conducted all postintervention and follow-up assessments. IEs were masters- or doctoral-level psychologists trained in the use of the ADIS–C/P.
Procedure
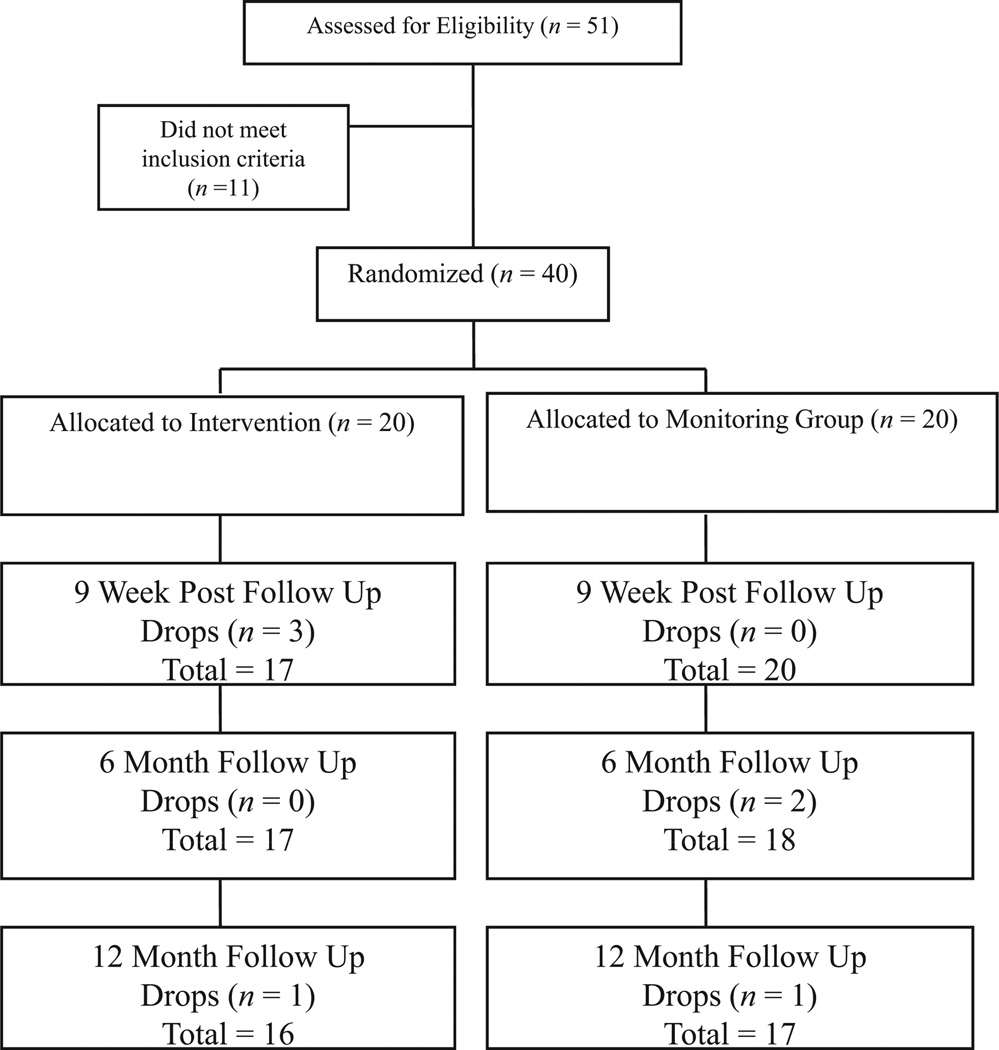
Families were recruited through advertisements in local papers, mailings to local physicians and psychiatrists, and community flyers. Fifty-one families completed an initial assessment. Among them, 9 were excluded because children met diagnostic criteria for an anxiety disorder (and were subsequently referred for treatment) and 2 were excluded because parents did not meet inclusion criteria. One parent had a primary diagnosis of major depression and the other did not meet criteria for any psychiatric disorder. The 40 eligible families were randomized equally to CAPS or the wait list control condition (WL). All families completed assessments pre- and postintervention (or 9 weeks after randomization for the WL group) and again 6 months and 12 months after the postintervention assessment (see Figure 2). Families in both groups were called on a monthly basis by an IE throughout the study to assess any potential changes (e.g., worsening) in anxiety symptoms.
Figure 2.
Subject flow diagram.
Data analysis plan
All missing data on continuous measures were managed using multiple imputation (MI) strategies (Rubin, 1987) with SAS. I imputed the missing outcomes separately for the WL and CAPS groups, assuming that if the missing participants continued in the program as assigned, the parameter distributions of the studied variables for these participants would be similar to those of the nonmissing participants who were assigned to the same group. Twenty imputations were specified. The total percentage of missing information was 10%. To examine differential program effects on diagnostic status, I used Fisher’s exact test, an analytical significance test used in the analysis of categorical data with small, sparse, and unbalanced data. In general, with categorical outcomes, researchers can test the effects at each time point through logistic regression, examine the differences over time using mixed models (Hedeker, 2004), or use discrete-time survival analyses (Singer & Willett, 1993). However, because no child in the CAPS group developed an anxiety disorder (i.e., no variation of the outcome), these analytical procedures were neither appropriate nor feasible.
To examine program effects on the continuous measures of anxiety severity (based on ADIS–C/P and SCARED scores), I used two analytical approaches. First, differences between the WL and CAPS groups at each time point after the intervention were compared using analysis of covariance (ANCOVA), adjusting for the baseline scores. The Baseline × Group interaction was also included in all of the ANCOVA models to test potential differential intervention effects by the baseline measure of the same variable. In the second approach, the intervention effect was examined over time, using all of the repeated measures of anxiety at pretest, posttest, 6-month follow-up, and 12-month follow-up together within a mixed model framework. The linear effects were estimated with unstructured covariance matrix and intercept as a random effect.
Results
Baseline Group Comparisons
I used t tests for continuous variables and chi-square analyses for categorical variables to examine differences on demographic and clinical variables between the two intervention groups at baseline (see Table 1). No significant differences were found between the two groups on any variable.
Attrition
The attrition rate for the entire sample was 17.5%: 20% (4 out of 20) in the CAPS group and 15% (3 out of 20) in the WL group. Analyses (t tests and chi square tests) were conducted to examine differences on demographic and clinical variables between the 7 families that dropped out of the study and the families that completed the study (see Table 2). Children who dropped out of the study were younger and a greater number of their parents were in psychiatric treatment. No other statistically significant differences were found.
Table 2.
Comparison of Baseline Characteristics of Families Who Dropped and Completed the Study
| Characteristic | Dropped (n = 7) | Completed (n = 33) | Differences |
|---|---|---|---|
| Child’s M age | 7.21 (0.99) | 9.30 (1.79) | (38) = −2.97** |
| Child gender, % female | 71 (5) | 39 (13) | χ2(1, N = 40) = 0.12 |
| Race or ethnicity, % Caucasian | 100 (7) | 89 (29) | χ2(1, N = 40) = 0.33 |
| Parent’s M age | 38.00 (3.58) | 41.58 (6.12) | t(38) = −1.14 |
| Marital status, % married | 86 (6) | 85 (28) | χ2(1, N = 40) = 0.95 |
| Parent’s education, % college | 86 (6) | 79 (26) | χ2(1, N = 40) = 0.68 |
| Family income, % over $80,000/year | 86 (6) | 64 (21) | χ2(1, N = 40) = 0.26 |
| % parents with comorbid diagnoses | 72 (5) | 73 (24) | χ2(1, N = 40) = 0.01 |
| % anxious parents in treatment | 100 (7) | 48 (16) | χ2(1, N = 40) = 6.27** |
| % coparents with psychiatric diagnoses | 29 (2) | 24 (8) | χ2(1, N = 40) = 0.81 |
| ADIS–C/P CSR M | 2.57 (0.79) | 2.00 (0.75) | t(38) = 1.81 |
| SCARED, parent total M | 14.92 (10.54) | 17.29 (10.23) | t(38) = −0.65 |
| SCARED, child total M | 18.00 (10.98) | 25.93 (12.45) | t(38) = −1.56 |
Note. For results presented in percentages, the number of respondents for categorical variables or standard deviations for continuous variables are indicated in parentheses. SCARED = Screen for Child Anxiety Related Emotional Disorders; ADIS–C/P CSR = Anxiety Disorders Interview Schedule for DSM–IV—Child Version clinical severity rating. Because of the small sample size for the families who dropped out from the study, the findings should be interpreted with caution.
p < .01.
Intervention Attendance
Among the CAPS families, the average number of sessions attended was 7.47 (out of 8), with a range of 5 to 8.
Primary Outcomes Analyses: Child Anxiety Diagnoses
Table 3 shows the cumulative number of children who developed an anxiety disorder at each assessment point during the study. Using the intent to treat sample, a total of 6 children (6/20 or 30%) in the WL group developed an anxiety disorder by the 1-year assessment. Five of these children met diagnostic criteria for generalized anxiety disorder and 1 met criteria for social phobia. All children were referred for treatment (and no other children in the WL group received treatment during the study). No child in the CAPS group developed an anxiety disorder (0/20). Using the data for the intent to treat sample, Fisher’s exact test indicated that the frequency of developing an anxiety disorder for the WL group, cumulatively, was significantly different from the frequency in the CAPS group (p < .01).
Table 3.
Cumulative Number of Children Meeting Diagnostic Criteria for an Anxiety Disorder at Each Assessment on the ADIS–C/P
| Assessment | CAPS | Wait list group |
|---|---|---|
| Preintervention | 0 | 0 |
| Postintervention | 0 | 3 (all GAD) |
| 6-month follow-up | 0 | 3 (all GAD) |
| 12-month follow-up | 0 | 6 (5 = GAD, 1 = SOP) |
Note. ADIS–C/P = Anxiety Disorders Interview Schedule—Child Version; CAPS = Coping and Promoting Strength program group; GAD = generalized anxiety disorder; SOP = social phobia.
Child Anxiety Severity
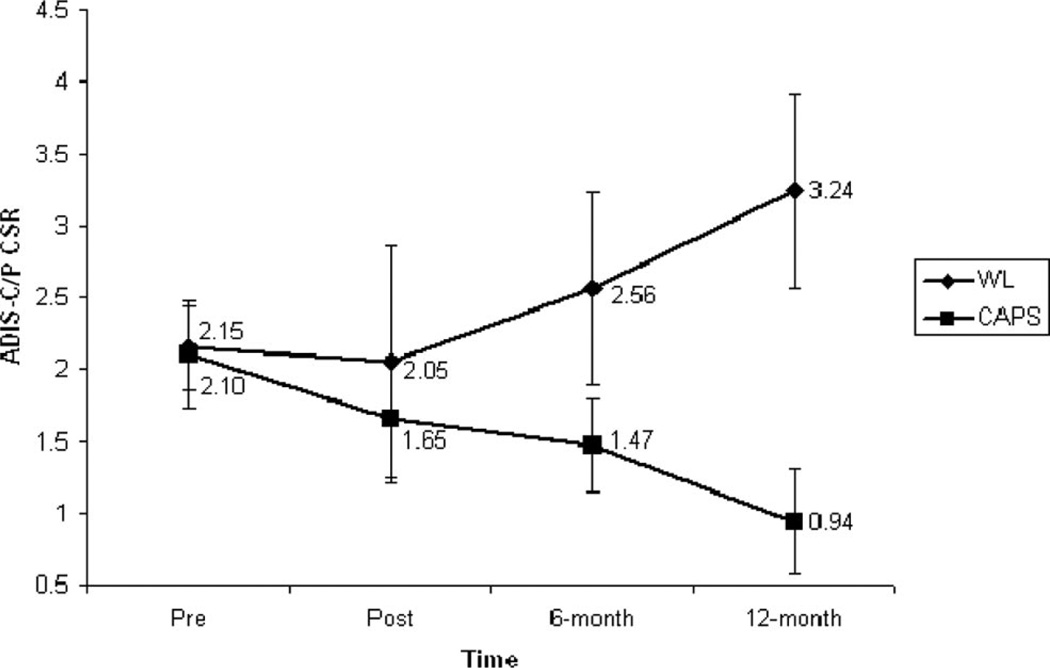
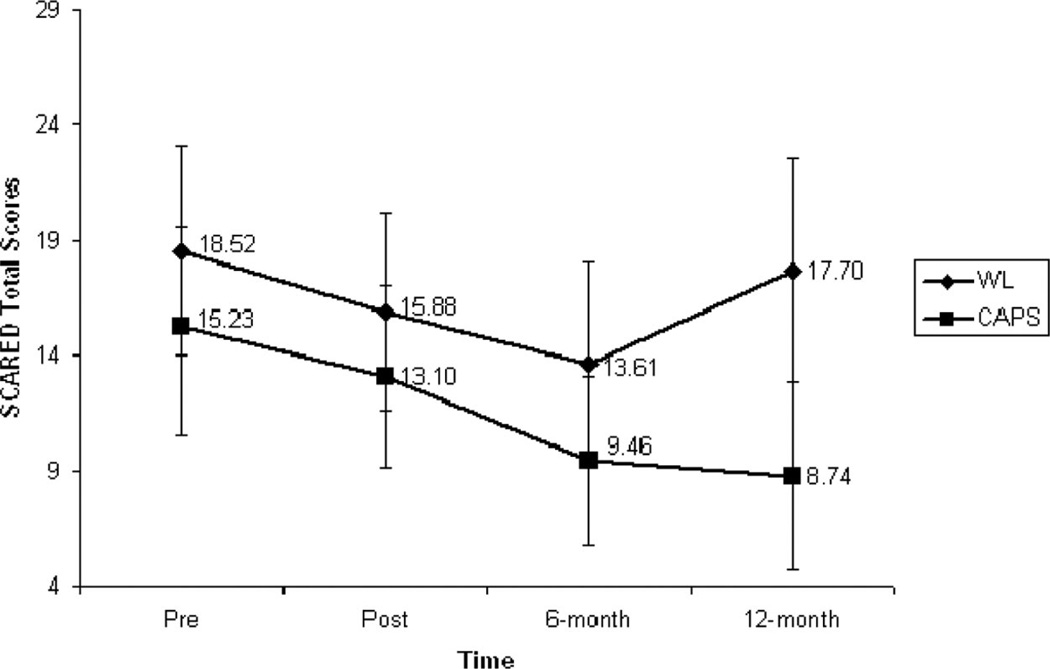
Means, standard deviations, and effect sizes on the ADIS–C/P clinical severity rating (CSR) and child and parent SCARED are presented in Table 4. The efficiency of MI estimation was over .98 for each variable. Table 4 shows the program effects for the ANCOVA from MI for each outcome at each time point. I included the baseline score and Baseline × Group interaction in all of the ANCOVA models. None of the interactions were significant, meaning that the program effect was homogeneous, not dependent on the baseline scores. ANCOVA indicated significant program effects on the 6-month and 12-month follow-up measures of severity of anxiety disorders based on ADIS–C/P. Another significant program effect was found for parent-report SCARED at the 12-month follow-up.
Table 4.
Mean Scores and Standard Deviations on Anxiety Measures and Analyses of Covariance Results for Program Effects
| Group | |||||||
|---|---|---|---|---|---|---|---|
| CAPS | WL | ||||||
| Measure | M | SD | M | SD | t | p | Cohen’s d |
| ADIS–C/P CSR | |||||||
| Preintervention | 2.10 | 0.85 | 2.15 | 0.67 | |||
| Postintervention | 1.65 | 1.00 | 2.05 | 1.85 | −1.00 | .32 | 0.34 |
| 6-month follow-up | 1.47 | 0.74 | 2.56 | 1.54 | −2.82 | .01 | 1.03 |
| 12-month follow-up | 0.94 | 0.85 | 3.24 | 1.56 | −4.78 | .001 | 1.99 |
| SCARED, child | |||||||
| Preintervention | 24.70 | 14.61 | 24.39 | 10.24 | |||
| Postintervention | 19.32 | 12.16 | 19.43 | 12.18 | −0.10 | .92 | 0.03 |
| 6-month follow-up | 17.39 | 10.50 | 16.60 | 9.79 | 0.18 | 1.0 | 0.00 |
| 12-month follow-up | 17.28 | 11.80 | 19.16 | 9.62 | −0.58 | .57 | 0.27 |
| SCARED, parent | |||||||
| Preintervention | 15.23 | 7.97 | 18.52 | 11.89 | |||
| Postintervention | 13.10 | 9.05 | 15.88 | 9.69 | −0.29 | .77 | 0.11 |
| 6-month follow-up | 9.46 | 8.33 | 13.61 | 10.15 | −0.74 | .47 | 0.36 |
| 12-month follow-up | 8.74 | 9.31 | 17.70 | 11.03 | −2.02 | .05 | 0.82 |
Note. CAPS = Coping and Promoting Strength program group; WL = wait list group; ADIS–C/P CSR = Anxiety Disorders Interview Schedule for DSM–IV—Child Version clinical severity rating; SCARED = Screen for Child Anxiety Related Emotional Disorders. Following Rosenthal’s (1994) suggestion, Cohen’s d can be calculated as , where n1 and n2 are the sample sizes for the program and self-study groups, respectively. For mixed models for longitudinal data, the degree of freedom is based on Satterthwaite’s approximation that accounts for random effects in calculating standard errors (see Little, Miliken, Stroup, & Wolfinger, 1996). When the means are in the wrong direction, p = 1.0 and d = 0.
The mixed model analyses examined the linear trend of the outcome variables across the entire study period. There were significant Intervention Group × Time interaction effects on (a) ADIS–C/P CSR scores (b = −0.74, SEb = 0.13), confidence interval = (−.96, −.52), t(118) = −5.79, p < .001, and (b) parent reports on SCARED total scores (b = −1.79, SEb = 0.97), confidence interval = (−3.41, −.17), t(118) = 1.84, p < .05. Figures 3 and 4 illustrate the changes over time across groups for these two variables, respectively, using the means from the imputed data. Both findings indicated that children’s anxiety levels were reduced linearly over time for the CAPS group but not for the WL group.
Figure 3.
Changes on the Anxiety Disorders Interview Schedule for DSM–IV Child Version (ADIS-C/P) clinical severity rating (CSR) over time for the Coping and Promoting Strength program (CAPS) and wait list (WL) groups.
Figure 4.
Changes on the Screen for Child Anxiety Related Emotional Disorders (SCARED) Parent Version total scores over time for the Coping and Promoting Strength program (CAPS) and wait list (WL) groups.
Intervention Satisfaction
Parent mean ratings on the satisfaction questionnaire items (see Table 5 and Table 6) indicated that parental satisfaction was high.
Table 5.
Parental Responses on the Treatment Satisfaction Questionnaire (N = 17)
| Intervention components | M score |
|---|---|
| Talking to a professional | 1.13 |
| Talking to my therapist | 1.19 |
| Factual information on stress, worries | 1.38 |
| Information on helpful and unhelpful thoughts | 1.38 |
| Information on facing challenges | 1.38 |
| Information on problem-solving skills | 1.44 |
| Information on communication skills | 1.56 |
| Information on parenting | 1.56 |
| Activities done in session | 1.63 |
| Session handouts | 1.88 |
| Out of session assignments | 1.94 |
| Information on relaxation skills | 2.00 |
| Daily diaries | 2.63 |
| Satisfaction with intervention | |
| Overall, how satisfied were you with the program?a | 6.19 |
| Degree program helped family cope better with stress?a | 6.06 |
| Would you recommend the program to others?a | 6.31 |
Note. Unless otherwise noted, parents answered on a scale of 1= very helpful to 5= very unhelpful.
Response to the item was made on a scale of 1= not at all satisfied to 7= very satisfied.
Table 6.
Sample Parental Responses on the Treatment Satisfaction Questionnaire
| Question | Sample parent response |
|---|---|
| What was the most helpful part of the program? | “communication and problem solving skills” |
| “identifying stressors and having concrete approaches”…“it gave us a vocabulary with which to discuss anxiety and some skills to use” | |
| “facing challenges, using rewards, helpful and unhelpful thoughts” | |
| What was the least helpful part of the program? | “the daily diaries” |
| “relaxation exercises” | |
| Suggestions for how to make the CAPS program better? | “involve extended family when in same household” |
| “focus a little more on parenting skills” |
Note. CAPS = Coping and Promoting Strength.
Discussion
The results of the present study indicated that a brief (6- to 8-session) family-based preventive intervention reduced the 1-year incidence of anxiety disorders and significantly reduced levels of anxiety symptomatology in the offspring of parents with anxiety disorders. This study represents the first published effort to prevent the onset of anxiety disorders among this population. The positive results were consistent across both independent evaluators and parent reports; however, child self-reports of anxiety did not differ in the intervention and WL groups. Parent levels of satisfaction with the intervention were high, and most families completed all of the sessions offered, suggesting families were engaged in the program and perceived it to be beneficial. Although this study was small in scope and requires replication, the findings highlight the promise and potential of prevention efforts for ameliorating the psychological and economic costs of anxiety disorders in this high-risk population.
Incidence of Anxiety Disorders
A primary goal of prevention science is to reduce the incidence of disorder or disease. Although there are no published data on 1-year incidence rates of anxiety disorders among offspring of parents with anxiety disorders, findings in the present study suggest this rate may be as high as 30% (among predominantly high-income Caucasian volunteer samples). More important, the preventive intervention developed and tested in this study appeared to reduce this 1-year rate. Although it is also possible that the WL condition had a negative impact rather than the intervention having a preventive effect, given that no iatrogenic effects of WL controls have been reported in the literature, this hypothesis seems unlikely. The high incidence rate of anxiety disorders in the WL group may be an aberration given the small sample; however, this rate is much lower than prevalence rates of anxiety disorders in this high-risk population. The high rate of anxiety disorders in the WL group may also be a function of the fact that many offspring had subclinical anxiety at baseline and were likely on a trajectory for developing an anxiety disorder. Regardless, the data confirm the vulnerability of these offspring and the need for preventive interventions.
Severity of Anxiety Symptomatology
Elevated levels of anxiety symptoms among youth are considered a key risk factor for anxiety disorders (see Spence, 2001). On the basis of parent and IE evaluations, this intervention significantly reduced anxiety symptoms over 1 year relative to the WL group. Effect sizes were generally moderate to large. Specifically, on the parent-report SCARED, children’s levels of anxiety symptoms dropped by approximately 40% for families randomized to the CAPS group but were relatively unchanged in the WL group over 1 year. In contrast to parent and IE reports, child reports of anxiety symptoms were not statistically different between groups, although the effect size at the 1-year assessment mirrored that of other prevention trials (Beardslee et al., 2003). In addition to the small sample size and limited power to detect differences, there may be several other reasons for this finding. First, it is possible that the intervention had no impact on children’s perceptions of their own anxiety symptoms. Parents’ reports may also have been biased (i.e., those in CAPS may have underreported symptoms and those in the WL group may have overreported), and IEs may have been influenced by parents’ reports of their child’s anxiety. It is also possible that children’s reports of subjective anxiety at this age or at subclinical levels are less valid and thus did not reflect intervention effects. Indeed, large effect sizes based on parent reports of anxiety are not unique to this study and mirror those found in other anxiety trials (e.g., Silverman et al., 1999).
On the basis of continuous data of anxiety symptoms, the effects of the intervention appeared to have the greatest impact over time (i.e., at 6 months and 1 year). The absence of change on continuous measures at the postintervention assessment can be interpreted in several ways. As with most preventive interventions, effects are generally expected to have maximal impact over many years and, consistent with this expectation, the largest effects were seen at the 1-year assessment (for all informants). The timing of the postintervention assessment may have been too close to the baseline assessment for significant changes in anxiety symptoms to occur.
Intervention Satisfaction
Parental satisfaction with the intervention was high. The majority of parents rated the following skills as very helpful (i.e., 1 on the 5-point scale): talking to a professional (70%), talking to their therapist (70%), information on facing challenges (60%), factual information on stress and worries (55%), information on helpful and unhelpful thoughts (55%), information on problem solving (55%), and information on parenting (50%). The intervention components with the lowest ratings were session handouts (35%), out-of-session assignments (30%), information on relaxation (30%), and daily diaries (10%).
Although formal dismantling studies are needed to clarify which intervention ingredients are critical, the satisfaction and attendance data suggest the majority of skills were perceived as beneficial. Future studies are needed to examine whether the hypothesized changes in the proximal outcomes accounted for changes in the distal outcomes (i.e., reductions in anxiety symptoms and disorders; see Figure 1). These analyses will further refine the intervention and theoretical model. Also awaiting future studies are questions related to costs and benefits. The cost of the current intervention associated with the individual format (versus a group format), length (i.e., number of sessions), and delivery method (face to face with each family vs. child or parent only vs. a Web-based intervention) must be compared with alternatives and submitted to a cost–benefit analysis. For instance, although the length of the current intervention was considerably shorter than the time involved in anxiety treatments, a longer intervention may have had more powerful effects. Alternatively, similar effects may have been found with a shorter intervention.
Limitations
The sample size was small, limiting power to detect small intervention effects (e.g., potentially in child reports of anxiety and postintervention) and restricting the number and type of analyses that could be performed, including the examination of moderators and mediators of intervention response. Comparisons between the two groups on key baseline demographic and clinical characteristics indicated that randomization worked, minimizing threats to the internal validity and increasing confidence in the main findings. However, examining whether the intervention’s impact varied as a function of baseline demographic or clinical variables (e.g., child gender, parental diagnosis, or anxiety severity) will be important for future, larger studies and to help determine for whom this intervention may be most useful. For instance, attrition analyses revealed that the 7 families who dropped from the study included younger children and the parents were more often in psychiatric treatment compared with the families who remained in the study. Although this number is small, it is possible that the intervention is less relevant for younger children or more of a burden for parents trying to manage their own treatment. Another limitation of the current study is the use of a WL control group. The WL condition raises questions about the specificity of the intervention and prohibits claims that the current intervention’s content, length, or format is superior to another. Moreover, because the ADIS (i.e., interview to determine parental diagnosis) and therapy sessions were not videotaped, confirmation about the reliability of parental diagnoses and the quality of adherence to the intervention are uncertain and remain for a future study. Finally, the sample of volunteers was predominantly Caucasian, two-parent families with high incomes, thus limiting the generalizability of findings to this population.
Clinical Implications and Future Directions
Overall, results indicated that a time-limited family-based intervention has the potential to lower the incidence of child anxiety disorders and reduce anxiety symptoms. For families, the findings have the potential to reduce the psychological and economic burden of illness. Although there are several models of preventive interventions (Mrazek & Haggerty, 1994), the current study fills a gap in the literature because it is the first published randomized controlled trial attempting to reduce the incidence of anxiety disorders among the offspring of parents with anxiety disorders. Although replication is warranted and future studies are needed to follow youth for longer periods of time to identify if the intervention has a long-term impact, these results provide information to clinicians working with parents with anxiety disorders and to policymakers (or third-party payors) regarding additional options for how to prevent anxiety disorders in at-risk youth.
Acknowledgments
This pilot study was supported by Grant K23 MH63427-02 from the National Institute of Mental Health. I am very grateful to the following mentors: William Beardslee, Nick Ialongo, Mark Riddle, and Irwin Sandler. I also thank several postdoctoral fellows (Rachel Grover, Anu Palapattu, Julie Kingery, Candice Alfano, and Keith Herman) and all the research assistants (especially Janine Domingues) for their assistance in implementing this study. A special acknowledgement goes to Jenn-Yun Tein for her statistical support.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Beardslee WR, Gladstone TRG, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: Evidence of parental and child change. Pediatrics. 2003;112:e119–e131. doi: 10.1542/peds.112.2.e119. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM. At risk for anxiety: I. Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:918–924. doi: 10.1097/00004583-199707000-00013. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders Scale (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent DA, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM–IV. New York: Graywind; 1994. [Google Scholar]
- Capps L, Sigman M, Sena R, Henker B. Fear, anxiety, and perceived control in children of agoraphobic parents. Journal of Child Psychology and Psychiatry. 1996;37:445–452. doi: 10.1111/j.1469-7610.1996.tb01425.x. [DOI] [PubMed] [Google Scholar]
- Di Nardo P, Moras K, Barlow D, Rapee RM, Brown TA. Reliability of DSM–III–R anxiety disorder categories: Using the Anxiety Disorders Interview Schedule—Revised (ADIS–R) Archives of General Psychiatry. 1993;50:251–256. doi: 10.1001/archpsyc.1993.01820160009001. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Silverman WK, Kurtines WM. Family involvement in treating children with anxiety and phobic disorders: A look ahead. Clinical Psychology Review. 1995;15:457–473. [Google Scholar]
- Greenberg MT, Domitrovich C, Bumbarger B. The prevention of mental disorders in school-aged children: Current state of the field. Prevention & Treatment. 2001;4 Article 1a. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=pdh&AN=pre-4-1-1a&site=ehost-live. [Google Scholar]
- Hedeker D. An introduction to growth modeling. In: Kaplan D, editor. The SAGE handbook of quantitative methodology for the social sciences. Thousand Oaks, CA: Sage; 2004. pp. 215–234. [Google Scholar]
- Kashani JH, Vaidya AF, Soltys SM, Dandoy AC, Katz LM, Reid JC. Correlates of anxiety in psychiatrically hospitalized children and their parents. American Journal of Psychiatry. 1990;147:319–323. doi: 10.1176/ajp.147.3.319. [DOI] [PubMed] [Google Scholar]
- Little RC, Miliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- Merikangas KR, Dierker LC, Szatmari P. Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: A high risk study. Journal of Child Psychology and Psychiatry. 1998;39:711–720. [PubMed] [Google Scholar]
- Mrazek PJ, Haggerty RJ. Reducing risks for mental disorders: Frontiers for preventive intervention research. Washington, DC: National Academy Press; 1994. [PubMed] [Google Scholar]
- Rosenthal R. Parametric measures of effect size. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York: Russell Sage Foundation; 1994. pp. 231–244. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponses in survey. New York: Wiley; 1987. [Google Scholar]
- Silverman W, Albano A. The Anxiety Disorders Interview Schedule for Children–IV (Child and parent versions) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Kurtines WK. Childhood anxiety and phobic disorders: A pragmatic perspective. New York: Plenum Press; 1996. [Google Scholar]
- Silverman WK, Kurtines W, Ginsburg S, Weems C, Lumpkin P, White C, et al. Treating anxiety disorders in children with group cognitive– behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67:995–1003. doi: 10.1037//0022-006x.67.6.995. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. It’s about time: Using discrete-time survival analysis to study duration and the timing of events. Journal of Education Statistics. 1993;18:155–195. [Google Scholar]
- Spence S. Prevention strategies. In: Vasey MW, Dadds MR, editors. The developmental psychopathology of anxiety. New York: Oxford University Press; 2001. pp. 325–351. [Google Scholar]
- Whaley SE, Pinto A, Sigman M. Characterizing interactions between anxious mothers and their children. Journal of Consulting and Clinical Psychology. 1999;67:826–836. doi: 10.1037//0022-006x.67.6.826. [DOI] [PubMed] [Google Scholar]
- Woodruff-Borden J, Morrow C, Bourland S, Cambron S. The behavior of anxious parents: Examining mechanisms of transmission of anxiety from parent to child. Journal of Clinical Child and Adolescent Psychology. 2002;31:364–374. doi: 10.1207/S15374424JCCP3103_08. [DOI] [PubMed] [Google Scholar]