Abstract
Background
Median sternotomy can weaken the upper abdominal wall and result in subxiphoid incisional hernia. We evaluated risk factors associated with the development of subxiphoid incisional hernias after coronary artery bypass grafting (CABG).
Materials and Methods
Of 1,656 isolated CABGs performed between January 2001 and July 2010, 1,599 patients who were completely followed up were analyzed. The mean follow-up duration was 49.5±34.3 months. Subxiphoid incisional hernia requiring surgical repair developed in 13 patients (0.8%). The hernia was diagnosed 16.3±10.3 months postoperatively, and hernia repair was performed 25.0±26.1 months after the initial operation. Risk factors associated with the development of subxiphoid incisional hernia were analyzed with the Cox proportional hazard model.
Results
Five-year freedom from the hernia was 99.0%. Univariate analysis revealed that female sex (p=0.019), height (p=0.019), body surface area (p=0.046), redo operation (p=0.012), off-pump CABG (p=0.049), a postoperative wound problem (p=0.041), postoperative bleeding (p=0.046), and low cardiac output syndrome (p<0.001) were risk factors for the development of the hernia. Multivariable analysis showed that female sex (p=0.01) and low cardiac output syndrome (p<0.001) were associated with subxiphoid hernia formation.
Conclusion
Female sex and postoperative low cardiac output syndrome were risk factors of subxiphoid hernia. Therefore, special attention is needed for patients with high-risk factors.
Keywords: Hernia, Coronary artery bypass, Sternotomy
INTRODUCTION
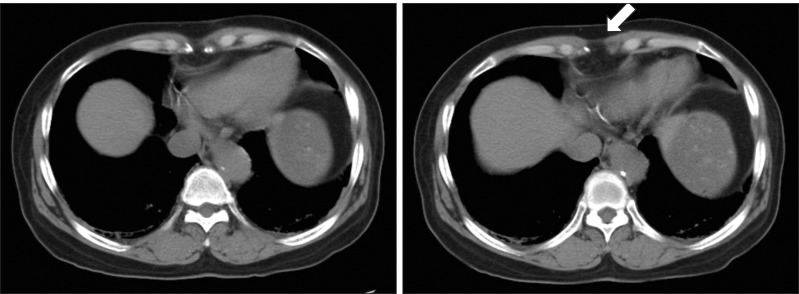
A median sternotomy that extends toward the epigastric area can weaken the upper abdominal wall and result in the development of subxiphoid incisional hernia (Fig. 1). Reported incidence of subxiphoid incisional hernia has ranged from 1% to 4.2% [1,2]. The subxiphoid hernia is known for its repair complexities and high recurrence rate because the subxiphoid area is a complex structure consisting of boney structures, the rectus abdominis muscles, linea alba, and the diaphragm [1-5]. Few studies have reported on subxiphoid incisional hernia while numerous studies that focused on abdominal incisional hernias have been reported [6-8]. We evaluated the risk factors associated with the development of subxiphoid incisional hernia in patients who underwent coronary artery bypass grafting (CABG).
Fig. 1.
Subxiphoid incisional hernia on computed tomography (CT) image. There is a fascial defect that resulted in the hernia at the subxiphoid area on the CT scan (arrow).
MATERIALS AND METHODS
1) Patient characteristics
Between January 2000 and July 2010, 1,656 patients underwent isolated CABG in our institution. Among them, 1,599 patients (male:female=1,136:463) who were followed up completely were enrolled in the present study. The mean age was 63.6±9.2 years and mean body mass index (BMI) was 24.8±2.9 kg/m2. During the study period, the fascial layer was closed by a continuous suture (1-0 Vicryl; Ethicon, Somerville, NJ, USA) and was reinforced by additional multiple 1-0 silk interrupted sutures.
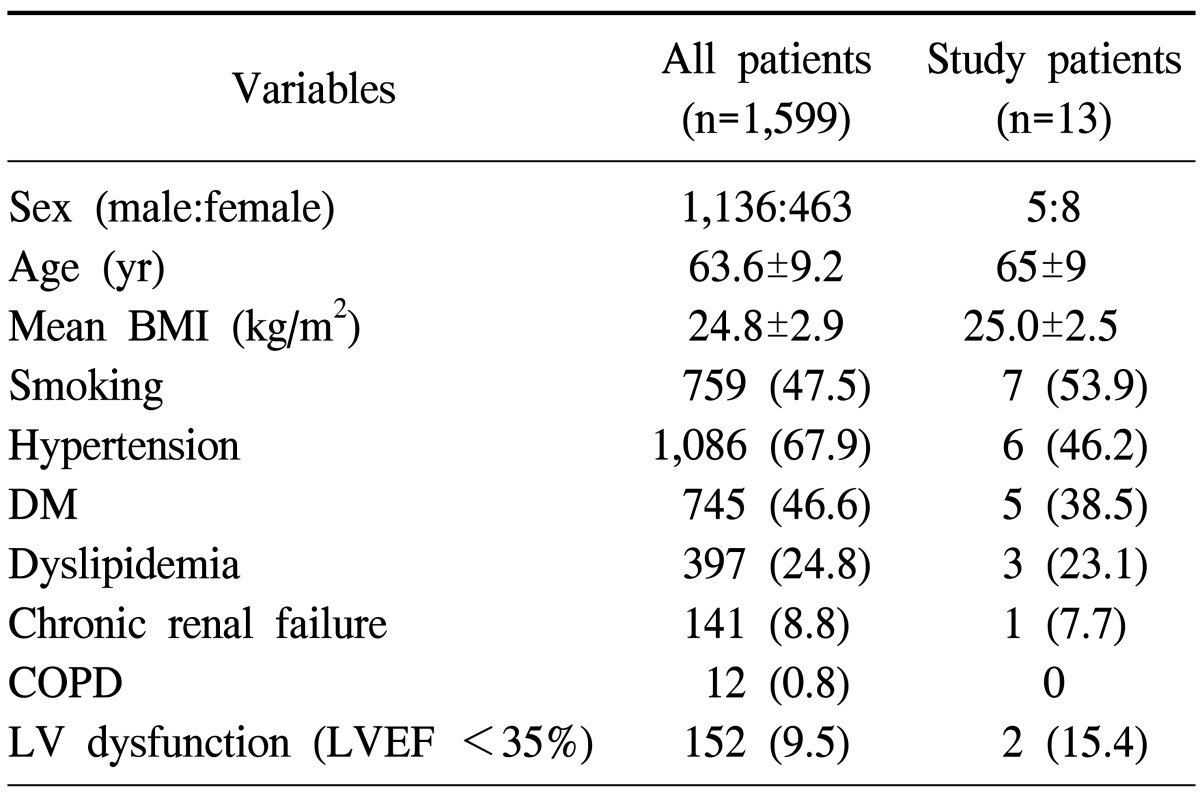
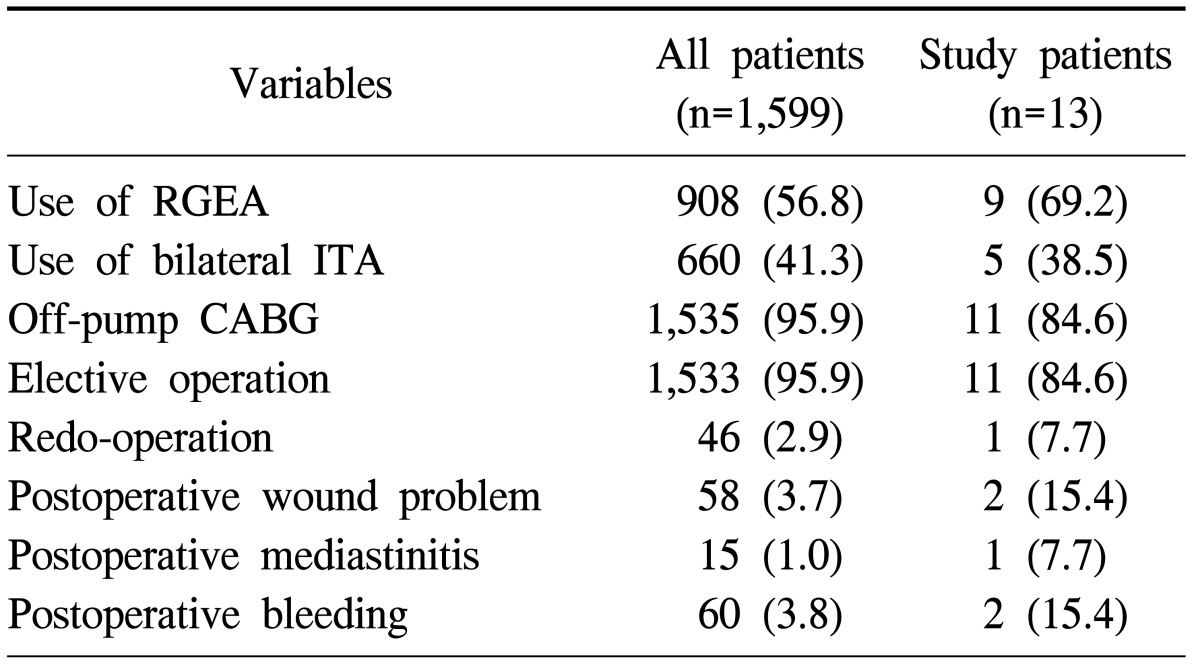
Patients showed various comorbidities, such as hypertension (1,086, 67.9%), diabetes mellitus (745, 46.6%), and dyslipidemia (397, 24.8%) (Table 1). Forty-six patients (2.9%) had a history of prior cardiac surgery. Postoperative wound problems developed in 58 patients (3.63%), including postoperative mediastinitis in 15 patients (0.94%). Sixty patients (3.75%) underwent reoperation for bleeding control due to postoperative bleeding (Table 2).
Table 1.
Patient characteristics
Values are presented as mean±standard deviation or number (%).
BMI, body mass index; DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; LV, left ventricle; LVEF, left ventricular ejection fraction.
Table 2.
Operative and postoperative data
Values are presented as number (%).
RGEA, right gastroepiploic artery; ITA, internal thoracic artery; CABG, coronary artery bypass graft surgery.
2) Clinical follow-up
Patients underwent regular postoperative follow-up through the outpatient clinic at 3-month or 4-month intervals. Routine physical examination including surgical wound observation was performed at the outpatient clinic. The mean follow-up duration was 49.5±34.3 months.
3) Statistical analysis
Statistical analysis was performed using the SPSS ver. 19.0 (SPSS Inc., Chicago, IL, USA). Patient demographic and clinical data that was considered as having an association with the development of subxiphoid hernia were analyzed using the Cox proportional hazard model. Preoperative risk factors such as sex, age, BMI, smoking, hypertension, diabetes mellitus, chronic renal failure, dyslipidemia, chronic renal failure, preoperative left ventricular dysfunction (ejection fraction <30%), chronic obstructive pulmonary disease, and prior surgical history were included in the analysis. Operation-related factors such as use of the right gastroepiploic artery (RGEA) graft, use of the bilateral internal thoracic artery graft, use of cardiopulmonary bypass, and emergent or urgent surgery were incorporated. Presence of wound problems including mediastinitis, reoperation for bleeding control, and postoperative low cardiac output syndrome (LCOS) were also included in the analysis.
Low cardiac output syndrome was defined as the need for a postoperative intraaortic balloon pump or inotropic support for longer than 30 minutes at the intensive care unit to maintain the systolic blood pressure (>90 mmHg) and the cardiac index (>2.2 L/min/m2) [9].
Multivariable analysis was performed with the univariate variables whose p-values were less than 0.1. A p-value of less than 0.05 was considered to be statistically significant.
RESULTS
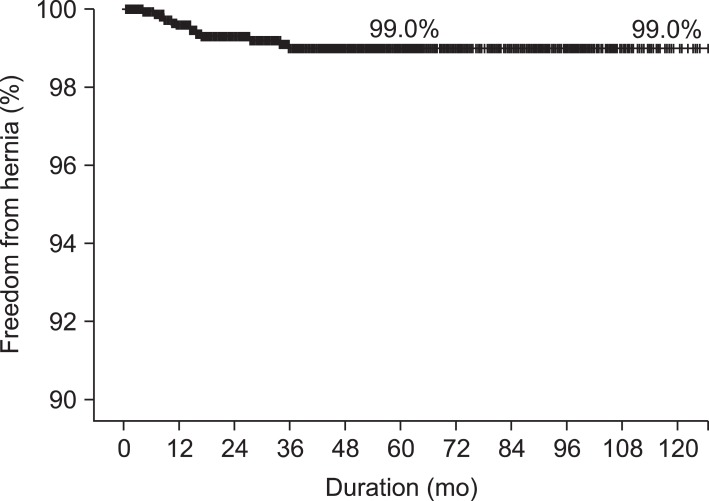
A subxiphoid incisional hernia requiring surgical repair developed in 13 patients (0.81%). It was diagnosed 16.3±10.3 months postoperatively, and hernia repair was performed 25.0±26.1 months after the initial operation. Once patients were diagnosed with an incisional hernia, they were referred to a general surgeon. Operations for the hernia were electively performed after examination by a general surgeon. All 13 patients underwent hernia repair using polyprolene mesh such as Marlex mesh (Phillips, Bartlesville, OK, USA) or Prolene mesh (Ethicon, Somerville, NJ, USA). None of the patients suffered from recurrence of subxiphoid hernia. Five-year and ten-year freedom from subxiphoid incisional hernia were 99.0% and 99.0%, respectively. In all 13 cases, the hernia had developed within five years after the surgery (Fig. 2).
Fig. 2.
Kaplan-Meier curve of freedom from subxiphoid incisional hernia. Five- and ten-year freedom from subxiphoid incisional hernias was 99.0% and 99.0%, respectively. All subxiphoid incisional hernias developed within 5 years after surgery.
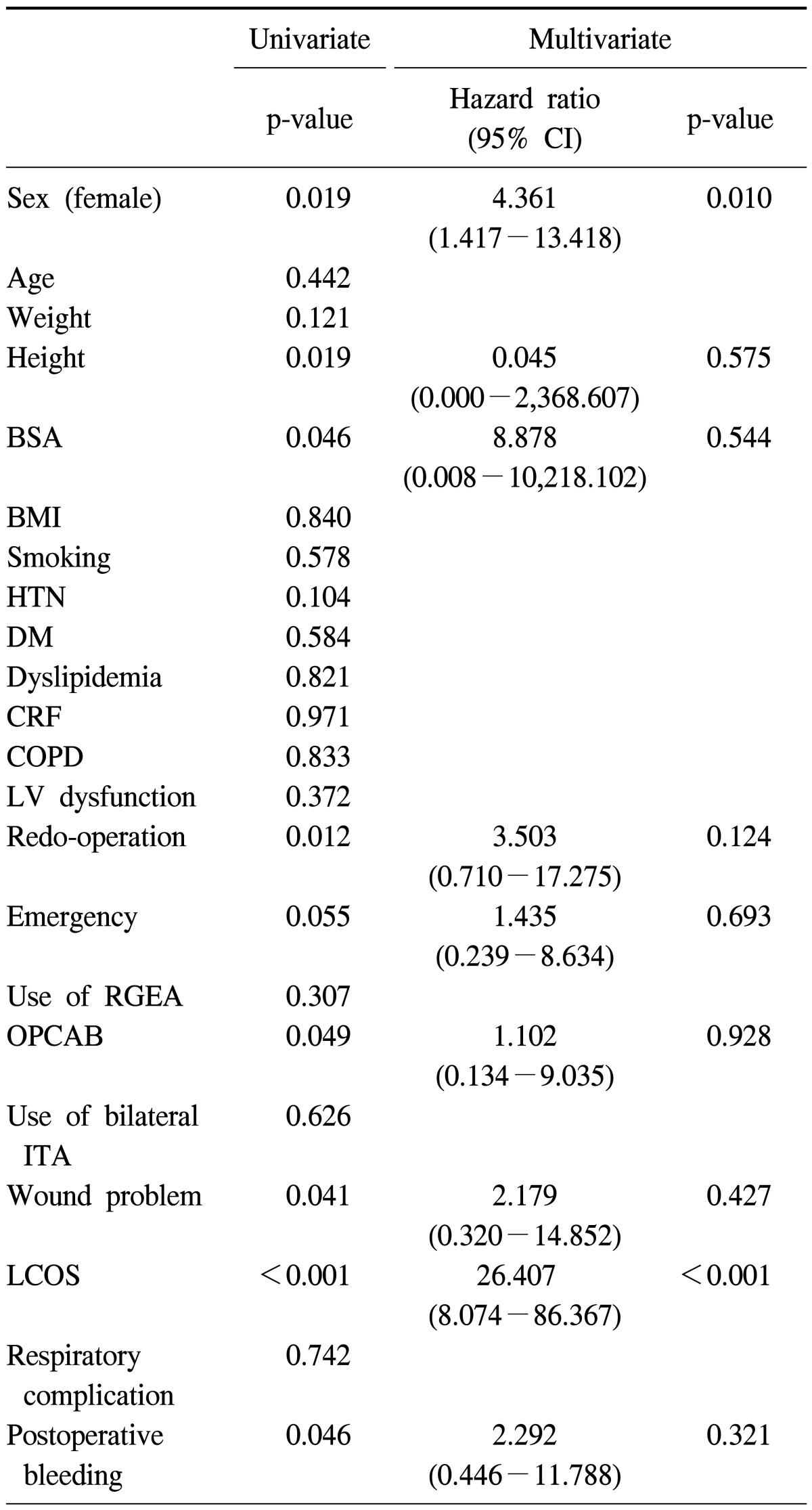
Univariate analyses revealed that female sex (p=0.019), height (p=0.019), body surface area (p=0.046), redo operation (p=0.012), off-pump CABG (p=0.049), a postoperative wound problem (p=0.041), postoperative bleeding reoperation (p= 0.046), and LCOS (p<0.001) were related to the development of subxiphoid incisional hernia (Table 3). On multivariable analysis, female sex (relative risk, 4.361; p=0.01) and postoperative LCOS (relative risk, 26.407; p<0.001) increased the risk of subxiphoid hernia.
Table 3.
Analysis of risk factors for the development of subxiphoid incisional hernia using the Cox proportional hazard model
CI, confidence interval; BSA, body surface area; BMI, body mass index; HTN, hypertension; DM, diabetes mellitus; CRF, chronic renal failure; COPD, chronic obstructive pulmonary disease; LV, left ventricle; RGEA, right gastroepiploic artery; OPCAB, off-pump coronary artery bypass; ITA, internal thoracic artery; LCOS, low cardiac output syndrome.
DISCUSSION
The present study produced two findings: subxiphoid incisional hernia requiring surgical repair developed in 0.8% of patients who underwent isolated CABG, and female sex and postoperative LCOS were associated with the development of subxiphoid incisional hernia.
Subxiphoid incisional hernia is usually associated with median sternotomy [3]. Subxiphoid incisional hernias have been known as difficult lesions to repair and have shown a high recurrence rate owing to the anatomical complexity of the subxiphoid area [2-5]. Incidences of subxiphoid incisional hernias associated with median sternotomy have been reported as between 1% and 4.2%, and a majority of the hernias have been reported to have developed within 2 to 3 years after surgery [2-5]. As complex cardiac surgical procedures associated with prolonged operation time were reported as risk factors of sternal wound infection [10], we limited the study population to only include patients who underwent isolated CABG. Patients who underwent valve surgery and CABG/valve surgery were excluded in the analysis to minimize the effect of procedure type and operation time. In the present study, subxiphoid incisional hernia requiring surgical repair developed in 0.8% of patients who underwent isolated CABG, and all subxiphoid hernias were detected within 5 postoperative years.
A previous study showed that obesity (BMI >30 kg/m2) increased the risk of sternal wound complications and subxiphoid hernia [3]. In the present study, we did not find the BMI to be a risk factor because the BMI of all the patients including the patients with subxiphoid hernia were 24.8±2.9 kg/m2 and 25.0±2.5 kg/m2, respectively. We investigated the risk factors for the development of incisional hernia after cardiac surgery among the common risk factors for sternal wound infection, such as old age, female sex, obesity, diabetes, chronic obstructive pulmonary disease, bilateral use of the internal thoracic artery, LCOS, and re-exploration for bleeding [10-13]. Female sex has been reported to be an independent risk factor for CABG and the higher morbidity in female patients was suggested to be associated with the higher proportion of women with diabetes and obesity who undergo this procedure [14-17]. Low cardiac output syndrome was also a risk factor of deep sternal infection [12,13]. As subxiphoid incisional hernia is a problem for wound healing, the negative effects of postoperative LCOS on wound the healing process may increase the risk of subxiphoid incisional hernia. In the present study, female sex and postoperative LCOS were identified as risk factors for incisional hernia.
The development of subxiphoid incisional hernia was explained by fascial dehiscence, which develops from a weakness in the soft tissue structures as well as from distraction mediated by the xiphoid region's osseous geometry [18]. Subxiphoid incisional hernia is obviously related to median sternotomy. However, variables commonly considered to be risk factors for wound complications were not demonstrated to be significant in this study. The use of RGEA, which required a long incision extended toward the abdomen area and the peritoneal opening, was also shown to be an insignificant factor for the development of the hernia. Although previous studies have reported high recurrence rates after the repair of subxiphoid incisional hernia (24% to 44%) [3,19,20], no recurrence was observed in this study. Currently, we are applying multiple interrupted sutures at the fascia layer of the subxiphoid area to prevent development of incisional hernia.
There are limitations to the present study. First, it was a retrospective study in a single institution. Second, the analysis was performed in a limited sample population who underwent isolated CABG. Therefore, it is difficult to generalize this result to patients who have undergone other cardiac surgical procedures. Third, we were not able to perform physical examinations for all the patients to detect subxiphoid incisional hernia. Thus, the incidence of development of subxiphoid incisional hernia might be underestimated.
CONCLUSION
In this study, female sex and postoperative LCOS showed an increased risk of subxiphoid incisional hernia. It is recommended that the surgeon pay attention when performing wound closures for high-risk patients and consider the possibility of subxiphoid hernia development during the follow-up period.
Footnotes
This article was presented at the 42nd Autumn Academic Meeting of the Korean Society for Thoracic and Cardiovascular Surgery.
References
- 1.Losanoff JE, Basson MD, Laker S, Weiner M, Webber JD, Gruber SA. Subxiphoid incisional hernias after median sternotomy. Hernia. 2007;11:473–479. doi: 10.1007/s10029-007-0258-8. [DOI] [PubMed] [Google Scholar]
- 2.Davidson BR, Bailey JS. Incisional herniae following median sternotomy incisions: their incidence and aetiology. Br J Surg. 1986;73:995–996. doi: 10.1002/bjs.1800731216. [DOI] [PubMed] [Google Scholar]
- 3.Mackey RA, Brody FJ, Berber E, Chand B, Henderson JM. Subxiphoid incisional hernias after median sternotomy. J Am Coll Surg. 2005;201:71–76. doi: 10.1016/j.jamcollsurg.2005.01.025. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MJ, Starling JR. Repair of subxiphoid incisional hernias with Marlex mesh after median sternotomy. Arch Surg. 1985;120:1270–1271. doi: 10.1001/archsurg.1985.01390350052011. [DOI] [PubMed] [Google Scholar]
- 5.Landau O, Raziel A, Matz A, Kyzer S, Haruzi I. Laparoscopic repair of poststernotomy subxiphoid epigastric hernia. Surg Endosc. 2001;15:1313–1314. doi: 10.1007/s004640090011. [DOI] [PubMed] [Google Scholar]
- 6.Penttinen R, Gronroos JM. Mesh repair of common abdominal hernias: a review on experimental and clinical studies. Hernia. 2008;12:337–344. doi: 10.1007/s10029-008-0362-4. [DOI] [PubMed] [Google Scholar]
- 7.Franz MG. The biology of hernia formation. Surg Clin North Am. 2008;88:1–15. vii. doi: 10.1016/j.suc.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yahchouchy-Chouillard E, Aura T, Picone O, Etienne JC, Fingerhut A. Incisional hernias. I. Related risk factors. Dig Surg. 2003;20:3–9. doi: 10.1159/000068850. [DOI] [PubMed] [Google Scholar]
- 9.Rao V, Ivanov J, Weisel RD, Ikonomidis JS, Christakis GT, David TE. Predictors of low cardiac output syndrome after coronary artery bypass. J Thorac Cardiovasc Surg. 1996;112:38–51. doi: 10.1016/s0022-5223(96)70176-9. [DOI] [PubMed] [Google Scholar]
- 10.Filsoufi F, Castillo JG, Rahmanian PB, et al. Epidemiology of deep sternal wound infection in cardiac surgery. J Cardiothorac Vasc Anesth. 2009;23:488–494. doi: 10.1053/j.jvca.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Tang GH, Maganti M, Weisel RD, Borger MA. Prevention and management of deep sternal wound infection. Semin Thorac Cardiovasc Surg. 2004;16:62–69. doi: 10.1053/j.semtcvs.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Careaga Reyna G, Aguirre Baca GG, Medina Concebida LE, Borrayo Sanchez G, Prado Villegas G, Arguero Sanchez R. Risk factors for mediastinitis and sternal dehiscence after cardiac surgery. Rev Esp Cardiol. 2006;59:130–135. [PubMed] [Google Scholar]
- 13.Risk factors for deep sternal wound infection after sternotomy: a prospective, multicenter study. J Thorac Cardiovasc Surg. 1996;111:1200–1207. doi: 10.1016/s0022-5223(96)70222-2. [DOI] [PubMed] [Google Scholar]
- 14.Roques F, Nashef SA, Michel P, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–822. doi: 10.1016/s1010-7940(99)00106-2. [DOI] [PubMed] [Google Scholar]
- 15.Koch CG, Khandwala F, Nussmeier N, Blackstone EH. Gender profiling in coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;126:2044–2051. doi: 10.1016/s0022-5223(03)00955-3. [DOI] [PubMed] [Google Scholar]
- 16.Zitser-Gurevich Y, Simchen E, Galai N, Mandel M; ISCAB Consortium. Effect of perioperative complications on excess mortality among women after coronary artery bypass: the Israeli Coronary Artery Bypass Graft Study (ISCAB) J Thorac Cardiovasc Surg. 2002;123:517–524. doi: 10.1067/mtc.2002.120012. [DOI] [PubMed] [Google Scholar]
- 17.Tokmakoglu H. Operative and early results of coronary artery bypass grafting in female patients in different body mass indexes. J Cardiothorac Surg. 2010;5:119. doi: 10.1186/1749-8090-5-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Askar OM. Surgical anatomy of the aponeurotic expansions of the anterior abdominal wall. Ann R Coll Surg Engl. 1977;59:313–321. [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson BR, Bailey JS. Repair of incisional hernia after median sternotomy. Thorax. 1987;42:549–550. doi: 10.1136/thx.42.7.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Read RC, Yoder G. Recent trends in the management of incisional herniation. Arch Surg. 1989;124:485–488. doi: 10.1001/archsurg.1989.01410040095022. [DOI] [PubMed] [Google Scholar]