Abstract
Abdominal aortic occlusion (AAO) caused by detachment of cardiac myxoma (CM) is a very rare complication in patients with CM. Although the nature of CMs has been well established, detachment of CM may cause unexpected serious complications such as vicious embolic events. Actually, in several cases of AAO caused by detachment of CM, it has been reported that CM fragments easily migrated to the brain, heart, and lungs, and caused lifelong neurological complications despite appropriate surgical therapy. Herein, we report a case of a patient with AAO caused by detachment of CM who underwent CM excision and abdominal aortic thromboembolectomy. Additionally, we have presented the preoperative and postoperative images using 64-multidetector computed tomography.
Keywords: Aorta, surgery; Myxoma; Aorta, abdominal
CASE REPORT
A 41-year-old female patient presented to the emergency room with sudden weakness of the legs that began one hour previously. She had been healthy except for a history of hypertension. The initial heart rate was at 75 beats/min and blood pressure was at 101/63 mmHg. She had cold and mottled lower extremities. Cardiac auscultation revealed an audible diastolic murmur. In addition, the femoral, popliteal, and dorsalis pedis arterial pulses were markedly diminished bilaterally. A 12-lead electrocardiogram and chest X-ray were normal. A conventional chest computed tomography (CT) scan revealed a low attenuation thrombus-like mass in the left atrium (Fig. 1A). A 64-multidetector computed tomography (64-MDCT) angiography of the lower extremities was performed. Three-dimensional, volume-rendering images of 64-MDCT angiography revealed total occlusion of the infrarenal abdominal aorta up to the bilateral common iliac arteries and reduced blood flow in the bilateral anterior and posterior tibial arteries (Fig. 2A). Transthoracic echocardiography revealed a mobile 44×26 mm mass that was attached to the left interatrial septum and that moved through the mitral valve during diastole. We planned an urgent cardiac myxoma (CM) excision and abdominal aortic thromboembolectomy. We performed antegrade and retrograde transfemoral thromboembolectomy using Fogarty catheters, which were passed through both common femoral arteries to restore the patency in the bilateral lower extremities. Large numbers of embolic fragments were extracted from both the femoral arteriotomy sites. Embolic fragments had gelatinous features and were mixed with the thrombus. Both the dorsalis pedis arterial pulsations and vascular Doppler flow signals were restored immediately after arteriotomy closure. We then performed a sternotomy and removed the CM through the left atrium. The atrial septal defect which was created for mass excision, was covered with an autologous pericardial patch. The mass to be excised was attached to the inferior margin of the fossa ovalis. The macroscopic specimen showed a nodular outer surface measuring 67×58×45 mm and contained multiple hemorrhagic spotted areas (Fig. 1B). The histopathologic report confirmed the diagnosis of a cardiac myxoma and detached myxoma fragments. We used intravenous unfractionated heparin therapy for 7 days to maintain the activated partial thromboplastin time between 55 and 60 seconds. After 10 days, she was discharged without any vascular or neurological complications. One month after surgery, a follow-up 64-MDCT of the lower extremity was performed. A volume-rendering image of the 64-MDCT angiography revealed patent blood flow in the distal abdominal aorta, and the bilateral common iliac and tibial arteries (Fig. 2B).
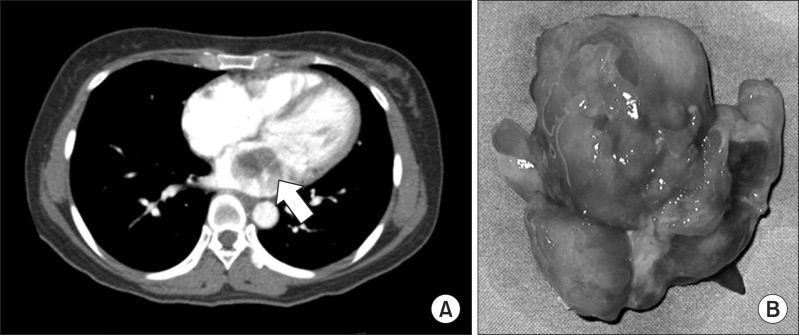
Fig. 1.
(A) Conventional chest computed tomography scan revealed a slow attenuation mass lesion in the left atrium (arrow). (B) Postoperative gross findings of cardiac myxoma.
Fig. 2.
(A) Preoperative volume-rendering image of 64-multidetector computed tomography angiography demonstrated occlusion of the lower abdominal aorta (arrow) and diminished blood flow in both the lower extremities (arrow head). (B) Postoperative computed tomography revealed complete restoration of blood flow.
DISCUSSION
Atrial myxomas have been described as a proliferation of primitive mesenchymal cells that normally differentiate into endothelial and smooth muscle cells and fibroblasts. CM represents roughly 50% of all benign cardiac tumors. Cases of abdominal aortic occlusion (AAO) caused by detachment of CM have been reported sporadically and have occurred without any prodromal symptoms. Suprarenal aortic occlusion is extremely rare because of the decreasing diameter of the descending aorta [1]. Total detachment of cardiac myxoma causing saddle embolization of the abdominal aorta has also been rarely reported [1,2]. Although one study reported that the most common initial presenting symptoms of CM were related to mitral valve obstruction, the signs or symptoms of embolism were also noted frequently, with incidences ranging from 30% to 40% [3]. The central nervous system is prone to an embolic attack, and the neurologic manifestations include syncope, psychiatric presentations, headaches, and seizures [4]. The emboli generally display a prediction for the brain, but can also affect other organs such as the liver, spleen, kidney, retina, coronary arteries, and peripheral arteries [5]. CM emboli may manifest as fulminant cerebral or cerebellar infarction. Also, several case reports of AAO caused by detachment of CM have demonstrated the development of serious neurological complications such as major stroke, bowel ischemia, amputation, paraplegia, and death [2,3,5,6]. Fortunately, our patient had no neurological signs or symptoms, and hence she recovered more quickly. Both echocardiography [6] and 64-MDCT angiography help clinicians in making a precise diagnosis and therapeutic decision. Moreover, 64-MDCT may be useful to evaluate the embolic involvement in the renal, coronary, gastrointestinal, and pulmonary arterial systems even if the hemodynamic status of the patient is unstable. In the present case of AAO caused by detachment of CM, we performed preoperative and postoperative 64-MDCT angiography. Preoperative 64-MDCT angiography provided high quality anatomic information about the abdominal aorta, which made surgical decision-making easier. Postoperative 64-MDCT angiography also provided additional information regarding the flow status and residual embolic occlusion of the lower extremities. Retrograde transcatheter embolectomy is effective for sweeping embolic clumps away. Concurrent surgical removal of CM is also essential, and the results of surgical excision of an uncomplicated CM are excellent, such that the recurrence rate is only 5% [7]. In conclusion, prompt diagnosis and surgical intervention are very important in cases of AAO caused by detachment of CM because they may be beneficial for preventing neurological complications and mortality.
References
- 1.Tsao JH, Lo HC, How CK, Yen DH, Huang CI. Embolic occlusion of the aorta caused by cardiac myxoma. Resuscitation. 2010;81:511. doi: 10.1016/j.resuscitation.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Neff CM, McCowan CL. Complete aortic occlusion caused by cardiac myxoma emboli. Am J Emerg Med. 2008;26:110.e1–110.e2. doi: 10.1016/j.ajem.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 3.Pinede L, Duhaut P, Loire R. Clinical presentation of left atrial cardiac myxoma. A series of 112 consecutive cases. Medicine (Baltimore) 2001;80:159–172. doi: 10.1097/00005792-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Binning MJ, Sarfati MR, Couldwell WT. Embolic atrial myxoma causing aortic and carotid occlusion. Surg Neurol. 2009;71:246–249. doi: 10.1016/j.surneu.2007.07.062. [DOI] [PubMed] [Google Scholar]
- 5.Yadav S, Alvarez JM. Catastrophic presentation of atrial myxoma with total occlusion of abdominal aorta. Interact Cardiovasc Thorac Surg. 2009;9:913–915. doi: 10.1510/icvts.2009.212514. [DOI] [PubMed] [Google Scholar]
- 6.Coley C, Lee KR, Steiner M, Thompson CS. Complete embolization of a left atrial myxoma resulting in acute lower extremity ischemia. Tex Heart Inst J. 2005;32:238–240. [PMC free article] [PubMed] [Google Scholar]
- 7.Shavit L, Appelbaum L, Grenader T. Atrial myxoma presenting with total occlusion of the abdominal aorta and multiple peripheral embolism. Eur J Intern Med. 2007;18:74–75. doi: 10.1016/j.ejim.2006.04.020. [DOI] [PubMed] [Google Scholar]