Abstract
The deterioration of skeletal muscle with advancing age has long been anecdotally recognized and has been of scientific interest for more than 150 years. Over the past several decades, the scientific and medical communities have recognized that skeletal muscle dysfunction (e.g., muscle weakness, poor muscle coordination, etc.) is a debilitating and life-threatening condition in the elderly. For example, the age-associated loss of muscle strength is highly associated with both mortality and physical disability. It is well-accepted that voluntary muscle force production is not solely dependent upon muscle size, but rather results from a combination of neurologic and skeletal muscle factors, and that biologic properties of both of these systems are altered with aging. Accordingly, numerous scientists and clinicians have used the term “muscle quality” to describe the relationship between voluntary muscle strength and muscle size. In this review article, we discuss the age-associated changes in the neuromuscular system—starting at the level of the brain and proceeding down to the subcellular level of individual muscle fibers—that are potentially influential in the etiology of dynapenia (age-related loss of muscle strength and power).
Keywords: Sarcopenia, Dynapenia, Muscle, Strength, Weakness, Aging
Introduction
In 2006, there were 37.3 million adults over the age of 65 years living in the USA [1], and it is expected that this number will double by the year 2050. Among these individuals, it is estimated that 42% have limitations in performing one or more daily tasks (e.g., walking two to three blocks, transferring from sitting to standing) that are essential for maintaining physical independence [1]. While the causes of physical disability are multifactorial, it is well established that contributing factors associated with age-related physical disability are low levels of voluntary muscle strength and power [2–7]. Indeed, over the past several decades, the scientific and medical communities have recognized that both skeletal muscle wasting and weakness are a debilitating—and even life-threatening—condition in older persons [8].
It was originally thought that the loss of skeletal muscle mass largely explained the muscle weakness observed in older adults [9]; however, recent longitudinal data suggest that other physiologic factors—independent of tissue size— play an important role in muscle weakness. Specifically, data from the Health ABC study indicate that the decline in muscle strength is much more rapid than the concomitant loss of muscle mass and that the change in quadriceps muscle area only explains ∼6–8% of the between-subject variability in the change in knee extensor muscle strength [10]. Moreover, maintaining or gaining muscle mass does not prevent aging-related declines in muscle strength [10]. Accordingly, these findings indicate that the loss of muscle strength in older adults is weakly associated with the loss of lean body mass. Our findings using animal models of aging and experimental disuse models of muscle weakness (e.g., cast immobilization and unilateral lower limb suspension) also suggest that the relative contribution of muscle atrophy to the disuse-induced muscle weakness is only modest [11–13]. In recent years, we have attempted to highlight the paucity of knowledge and our lack of understanding of the mechanisms of weakness in the elderly, and in 2008, a new term to more accurately define the loss of muscle strength with age was coined: dynapenia [14].
Numerous scientists and clinicians have used the term “muscle quality”—and other related terms such as specific force—to describe the relationship between voluntary muscle strength and muscle size (i.e., decreased muscle quality is indicative of lower muscle strength relative to muscle size) [2, 10, 15–24]. Recent longitudinal data from the Health ABC study of more than 1,600 older adults indicate that knee extensor muscle quality—as defined above—decreases at a staggering rate of ∼2.5%/year (in contrast to muscle cross-sectional area decreasing at a rate of ∼1%/year) [10]. Similar findings have also been observed in cross-sectional studies [2]. These findings further indicate that changes in neurological function and/or the intrinsic force-generating properties of skeletal muscle contribute to dynapenia in older adults. These potential contributors to reduced muscle quality are numerous and likely even vary within the context of specific tasks. In general though, the mechanisms determining muscle quality largely arise from two factors: (1) neurological and (2) skeletal muscle properties, as it is well known that the output from these sources controls muscle force production. Specifically, within the neuromuscular system, there are several potential sites affecting muscle quality, such as excitatory drive to the lower motor neurons, α-motor neuron excitability, neuromuscular transmission, and excitation–contraction (E–C) coupling [25]. In this review article, starting at the level of the brain and proceeding down to the muscle fiber level, we will discuss and describe the potential physiological factors leading to reductions in muscle quality in older adults.
Effects of aging on the mechanisms determining optimal force output
Neural contributors to force generation
In this section, we will discuss age-related changes in central (voluntary) activation, followed by discussing the effects of aging on supraspinal and spinal form and function.
Age-related changes in central (voluntary) activation
As stated earlier, aging is commonly associated with muscle weakness. This loss of muscle strength is likely due to a wide variety of physiologic reasons, including reductions in muscle mass and changes in the excitation–contraction coupling process. However, it is also probable that a portion of the strength loss is attributable to the nervous systems ability—or lack thereof—to fully activate skeletal muscle. Thus, it is imperative that scientists and clinicians understand the role of the central nervous system in mediating the muscle weakness observed with advancing age.
There is evidence to suggest that aging results in impaired agonist activation and/or increased antagonistic coactivation [26]; however, age-related differences in voluntary activation appear to vary between muscle groups. Prior to more fully discussing the effects of aging on voluntary activation, we will first provide a brief overview of the assessment of voluntary activation. A voluntary effort, or a voluntary contraction of a muscle, comprises the recruitment of motor neurons, and hence muscle fibers, by increased descending drive. Hence, with an increased force of contraction, there is increased activation of neurons in the primary motor cortex with increased firing of corticospinal neurons [27]. Increased descending drive recruits greater numbers of motor neurons in the spinal cord. While there are many influences on motor neurons during voluntary contractions, such as excitatory and inhibitory sensory feedback, and alterations in motor neuron properties that may make them more or less responsive to synaptic input [28], descending drive from the motor cortex is the major determinant of the timing and strength of voluntary contractions. Voluntary activation is commonly assessed using the interpolated twitch method, or a derivative thereof (e.g., central activation ratio) [29–32]. Here, the motor nerve to the muscle is electrically stimulated during a voluntary effort. During maximal voluntary efforts, any increment in force evoked by a stimulus indicates that voluntary activation is less than 100%. That is, some motor units are not recruited or are not firing fast enough to produce fused contractions [33]. The extra force evoked by stimulation during contraction can be quantified by comparison to the force produced by the whole muscle. Thus, voluntary activation represents the proportion of maximal possible muscle force that is produced during a voluntary contraction. Measurement of voluntary activation does not quantify the descending drive reaching the motor neurons, nor whether motor neuron firing rates are maximal, nor does it take into account the source of drive to the motor neurons [30].
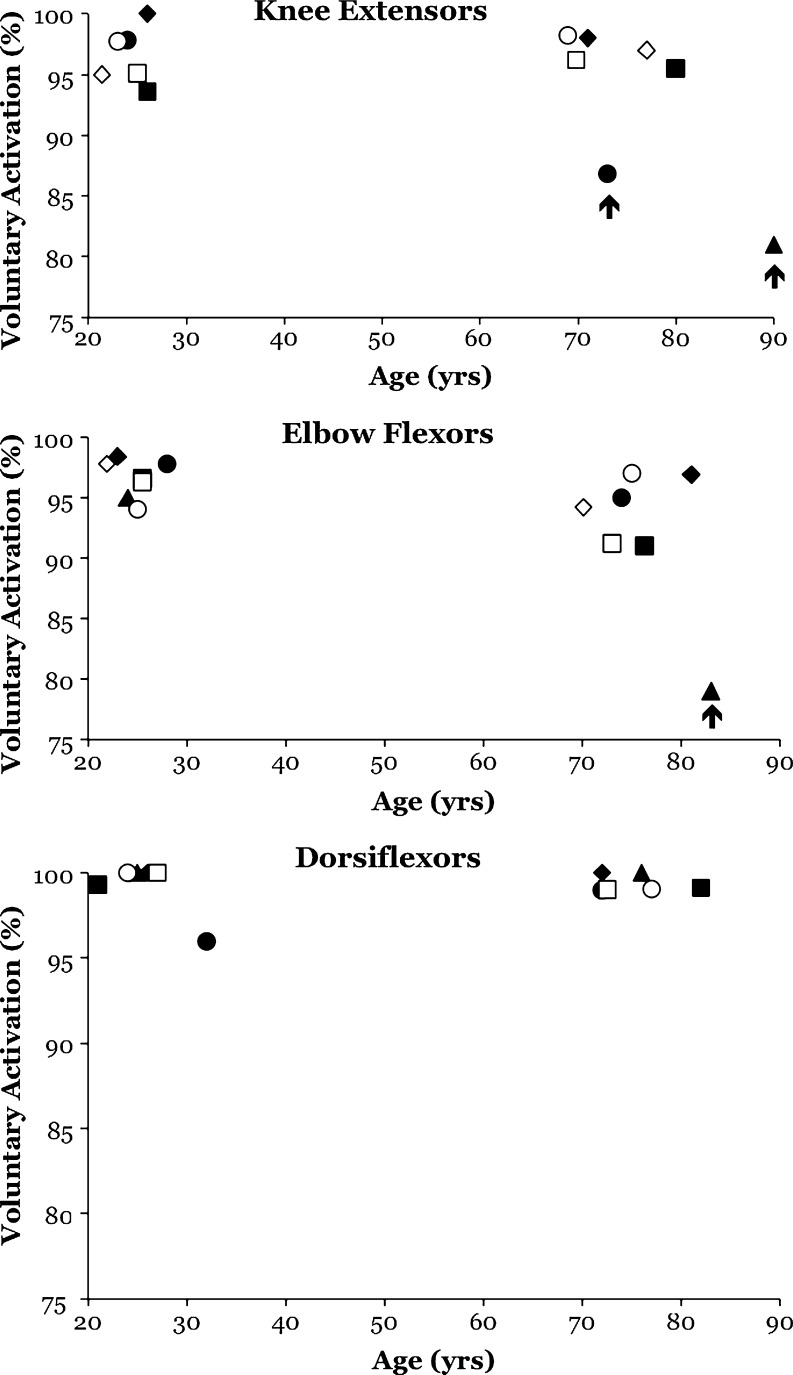
There are equivocal reports in the literature on whether or not advancing age reduces voluntary activation capacity [34–53] (for review, see [2]). A synthesis of the literature provides some insight into potential explanations of these equivocal reports. Specifically, several studies examining the effect of age on voluntary isometric activation of the knee extensors (Fig. 1a) and the elbow flexors (Fig. 1b) suggest that older adults, particularly those greater than 70–75 years of age, exhibit a decrease in voluntary activation, whereas investigations on the age-related changes in voluntary activation of the dorsiflexors yield null findings (Fig. 1c). Due to the functional differences between these muscles, as well as differences in their physiologic profiles (e.g., motor unit innervations and fiber-type characteristics), these muscle group-specific effects are not overly surprising. We should note that three studies indicating a dramatic impairment in voluntary activation are highlighted with an arrow in Fig. 1. Two of these (Fig. 1a) relate to the knee extensor muscles and one relates to the elbow flexors (Fig. 1b). With regards to the knee extensors, a number of reports show no differences between old and young adults, but two reports stand out as showing a deficit in voluntary activation with aging (Fig. 1a, vertical arrows) [40, 42, 50]. One of these represents data from the oldest known cohort of individuals that has been examined to date (n = 11, age range 85–97 years) [40], and this observation suggests that deficits in the neural drive can contribute to much of the muscle weakness observed in the very elderly—at least in the knee extensor muscles. The second of the highlighted studies deserves particular attention because it is the largest to date (young adults: n = 46, 18–32 years; older adults: n = 46, 64–84 years) [50]. Here, the voluntary activation of older adults was calculated to produce 87% of maximal muscle force in comparison to 98% maximal force produced by younger subjects. With regards to the elbow flexors, one study is highlighted as this study averaged voluntary activation across numerous trials (as opposed to a single best trial or two) and thus provides some evidence that voluntary activation is less consistent across trials in older men compared to younger men [42]. Together, these studies provide proof of principle that older adults likely exhibit impairments in voluntary activation and that this likely varies with the specifics of a given task and the muscle group being examined.
Fig. 1.
Age-related changes in voluntary activation (a measure of how much of a muscle’s possible force is produced by a voluntary contraction) is muscle group specific. Studies quantifying age-related differences in voluntary activation of the knee extensors (a), elbow flexors (b), and ankle dorsiflexors (c) during isometric contractions. Selected studies have been highlighted with an arrow pointing to them (see main text for further discussion on these specific papers). Data points in a correspond to the following articles: filled circles: [50], filled squares: [48], filled diamonds: [35], filled triangle: [40], open circles: [51], open squares: [36], open diamonds: [46]. Data points in b correspond to the following articles: filled circles: [38], filled squares: [34], filled diamonds: [45], filled triangle: [42], open circles: [52], open squares: [41], open diamonds: [53]. Data points in c correspond to the following articles: filled circles: [43], filled squares: [38], filled diamonds: [47], filled triangle: [44], open circles: [49], open squares: [37]. Reprinted with permission from [233]
Age-related changes in supraspinal properties
The neurons in the premotor and primary motor cortex form a complex network of glutamatergic interneurons, afferent projections, and pyramidal neurons that project to the striatum and spinal cord, among other areas of the central nervous system. Although it is often widely assumed that there is a progressive decay in the number of primary motor cortex (M1) neurons in normal aging, it does not appear that an actual decrease in cortical neurons occurs [54, 55]. However, there are substantial morphometric changes in the motor cortex that do occur with normal aging. For example, cadaveric dissections from humans who died without neurological signs suggest that individuals over 65 years of age exhibit a 43% volumetric reduction in the premotor cortex neuron cell body size in comparison to adults younger than 45 years [54], which have more recently been corroborated in living humans using high-resolution magnetic resonance imaging [56]. Furthermore, there is also evidence to suggest that age-related differences exist in mass of white matter and of myelinated nerve fiber length with individuals losing ∼45% of the total length of the myelinated fibers, mostly in the smallest white matter nerve fibers [57]. Also, cross-sectional studies further suggest that aging disrupts the integrity of white matter [58]. Functionally, it appears that these changes due to aging would affect the connectivity of the cortex with itself as well as the rest of the central nervous system.
In addition to morphometric changes, there has long been interest regarding the neurochemical changes within the basal ganglia that can be attributed to aging. This interest was largely driven by the hypothesis that changes in neurotransmitters and their receptors may be attributed to decreases in cognitive as well as motor functions. Certainly, it has been shown that impaired neurotransmission is responsible for at least some age-related behavioral abnormalities [59], including the serotonergic [60, 61], cholinergic [62], adrenergic [61], dopaminergic [63–66], GABAergic [63, 65], and glutamatergic systems [63, 65]. Reductions in neurotrophic factors have been shown within the motor cortex as well [67]. Age-related changes in the dopaminergic system are perhaps the best understood from work on different neurological conditions such as Parkinson’s disease. Older adults have been reported to exhibit reduced dopamine transporter availability [68], and animal findings show that older rodents have decreased dopamine (D2) receptors [69].
Aging also affects motor cortical properties at the systems level. Specifically, aging has been shown to result in decreased cortical excitability [70–73], increased activation in areas of sensorimotor processing and integration [74–76], and reduced cortical plasticity [77, 78]. In the following exposition, we will briefly summarize some of the evidence indicating these pertinent changes.
The effect of aging on cortical excitability is most commonly examined using paired-pulse transcranial magnetic stimulation (TMS), which also allows for the assessment of intracortical excitability [79, 80]. More specifically, paired-pulse TMS permits the assessment of short- and long-interval intracortical inhibition, which is generally thought to be mediated by gamma-aminobutyric acid (GABA) type A [81, 82] and B [81, 83] receptors, respectively (GABAA, GABAB). Additionally, intracortical facilitation—a measure that is mediated by excitatory glutamatergic interneurons and N-methyl-d-aspartate (NMDA) receptors [82, 84, 85]—can also be quantified. A recent investigation on age-related changes in intracortical facilitatory and inhibitory properties using paired-pulse TMS suggests that middle-aged adults exhibit reduced cortical excitability in comparison to younger adults, as it has been observed that individuals in their late 50s and early 60s exhibit more intracortical inhibition and less intracortical facilitation than adults in their 20s [70]. Our recent findings in the elderly (mean age of 71 years) support these previous data, as we have observed that older adults exhibit substantially more intracortical inhibition and less intracortical facilitation in comparison to young adults under resting conditions, but that when these data were elicited during a submaximal contraction these differences disappeared [73]. Collectively, these findings suggest that aging results in cortical atrophy, altered neurochemistry, and reduced motor cortical excitability, all of which could be mechanistically link to impairments in voluntary activation capacity and contribute to age-related reductions in motor performance.
Age-related changes in spinal properties and the neuromuscular junction
The neuromuscular system is comprised of individual motor units, with the neuromuscular junction serving as the communication bridge between the nerve terminal and the muscle fibers they innervate. While the motor neuron and its behavior are the “final common pathway” for all motor commands, each motor neuron typically has 50,000 synapses to convey these commands [86] and can thus be influenced by numerous factors. It is well known that motor unit recruitment is primarily regulated on a biophysical basis with low-threshold motoneurons being recruited first [87]. However, in addition to the size principle of recruitment, discharge patterns of motor neurons are influenced by both the characteristics of their presynaptic input and their intrinsic properties. For instance, the discharge properties of motor neurons can be influenced by their prominent post-spike after hyperpolarization [88], their “bistable” behavior [89], as well as persistent inward currents. This phenomenon is thought to be explained from dendrite properties known as the persistent inward currents that act to amplify synaptic input [89, 90]. Motor units demonstrate numerous age-related adaptations, including changes in morphology, behavior, and electrophysiology. With regards to changes in morphology, advancing age is thought to result in a reduced motor unit number as well as an increased number of fibers per motor unit (increased innervation ratio) due to the compensatory collateral sprouting by surviving neurons [91–94]. Aging also elicits remodeling of the neuromuscular junctions endplate. Specifically, aged neuromuscular junctions exhibit elevations in presynaptic nerve terminal branching, and in the post-synaptic distribution of receptor sites for neurotransmitter [95–100]. Interestingly, recent evidence indicates that disuse further compounds these age-associated changes as muscle unloading was observed to result in significant remodeling of aged rats neuromuscular junction, but not in those of young, healthy rats [99]. Accordingly, these findings may indicate that the combination of aging and disuse, at least among aged rats, results in partial denervation leading to morphological remodeling of the neuromuscular junction [101].
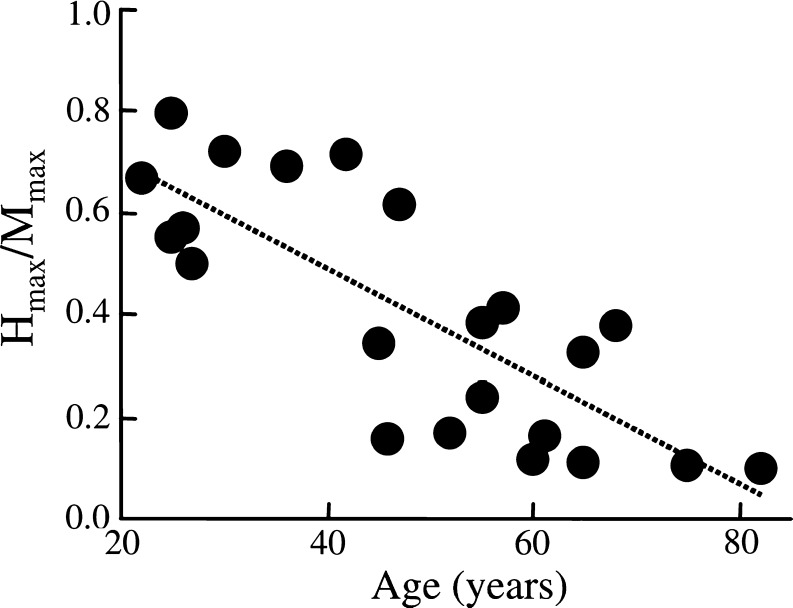
Aging has also been shown to result in changes in spinal excitability. For example, Kido and colleagues reported that both the maximum soleus H-reflex (H-max, a measure of global spinal excitability) and the maximum soleus M-wave (M-max, also known as the compound muscle action potential or CMAP) decrease gradually with age, with the decrease in the H-max being more pronounced (reduced H-max to M-ma ratio; Fig. 2). The H-reflex only provides a global measure of spinal excitability, as it can be modulated by a number of potential factors (e.g., presynaptic inhibition, variation in the amount of neurotransmitter released by the Ia terminal, fluctuations in the membrane potential arising, alterations in the intrinsic properties in the motoneurons, etc.). As such, the aforementioned findings suggest that overall spinal excitability is depressed in older adults. However, others have observed that heteronymous facilitation [102] and oligosynaptic reflexes [2] also decrease with age, which provides collective evidence that there is a general decrease in the excitability of spinal reflexes with age.
Fig. 2.
Age-related decline in the human soleus muscles H-max to M-max ratio suggesting that advancing age results in a decrease in global spinal excitability. Data were obtained during standing while the muscle was activated at an intensity equal to 15% of its maximum voluntary contraction. Reprinted with permission from [234]
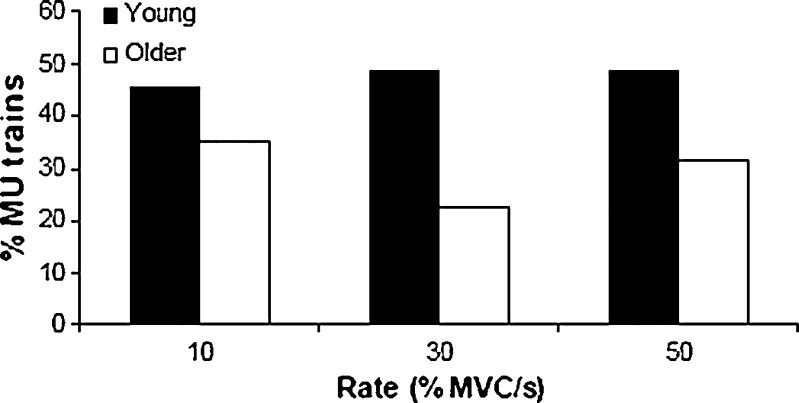
The end result of the morphological and physiological adaptations in motor units with aging is alterations in the behavioral discharge properties of motor units. For instance, older adults have been reported to exhibit mean motor unit firing rates of the tibialis anterior across a variety of contraction intensities that are ∼30–35% lower than young adults [103], and the maximum motor unit firing rate of an intrinsic hand muscle is also comparably reduced [103]. These lower firing rates appear to be largely inter-related to the longer twitch contraction durations in older muscle, which further illustrates the critical integrative control processes involved between the nervous and muscular systems as it relates to overall neuromuscular function. More recent evidence suggests that more subtle age-related differences exist in motor unit behavior. Specifically, older adults have been reported to exhibit a greater variability in motor unit discharge rates that appears to largely influence their ability to maintain steady forces [104], and the occurrence of motor unit doublet discharges is lower in older adults (Fig. 3) [105].
Fig. 3.
Percentage of motor unit trains in which doublets were observed in young (black) and older (white) individuals at three rates of force production. There were no significant differences among rates of force production, but significant differences between groups were found, indicating that the young subjects tended to display more doublet discharges. Reprinted with permission from [105]
Collectively, these findings suggest that aging results in morphological changes in motor units, including an actual reduction in functional motor units. A change of this nature (i.e., loss of motor units resulting in some muscle fibers not undergoing re-innervation) would theoretically result in a reduction in muscle quality. Additionally, age-related changes in spinal properties and the neuromuscular junction, such as decreased spinal excitability and a reduction in maximal motor unit discharge rates, may contribute to impairments in voluntary activation capacity (and thus reduced muscle quality).
Muscular contributors to force generation
In this section, we will discuss age-related changes in muscular properties as it relates to muscle size and composition, excitation–contraction coupling, and crossbridge function and energetics.
Age-related changes in muscle size and composition
Much atrophy undoubtedly occurs with advancing age. In fact, data from the Health, Aging, and Body Composition (Health ABC) Study—which followed 1,678 older adults between 70 and 79 years of age longitudinally over a 5-year period—indicate that, on average, older men lose approximately 1% of their thigh muscle area per year and older women lose approximately 0.65% of their thigh muscle area per year [10]. With this stated, it should be noted that there is a large between-subject variability in the degree of atrophy observed with aging, and some older adults appear to exhibit no or nominal losses in muscle mass [10]. To study the effects of increasing age on human skeletal muscle size and composition, Lexell et al. examined 15-μm cross sections of autopsied whole vastus lateralis muscle from 43 previously physically healthy men between 15 and 83 years of age [106]. They reported that age-related muscle atrophy begins during the third decade of life and accelerates thereafter. The observed atrophy appeared to be primarily caused by a loss of fibers, with no predominant effect on any fiber type, and to a lesser extent by a reduction in fiber size—predominantly type II fibers. This finding was later corroborated by Lee and colleagues who reported that aging resulted in a decreased fiber area percentage, fiber number percentage, and mean fiber area of type IIA and IIB muscle fibers, but that type I fibers increased in area and number but not in size [107]. Moreover, the type II fibers appeared morphologically smaller and flatter, which is consistent with other reports suggesting pathological abnormalities in aged human muscle fibers such as central nuclei, ring fibers, fiber splitting, scattered highly atrophic fibers, moth-eaten fibers, and even vacuoles [108]. Hence, as both the size and structure of a muscle deteriorate, the force-generating capacity is influenced.
There are many interacting factors leading to muscle wasting in older adults, and they often present themselves concurrently (for review, see [109]). Changes in muscle protein metabolism have been proposed as an explanatory factor in muscle wasting in older adults, as the balance between protein synthesis and degradation is largely responsible for the maintenance of lean mass [110]. However, recent findings suggest that basal muscle protein synthesis rates do not differ between young and old adults [111–116], and today, it is generally accepted that the difference in fasted rates of muscle protein synthesis or breakdown are not altered in healthy older adults [110]. Current hypotheses related to causative factors affecting muscle protein turnover surround the concept of older adults being resistant to anabolic stimuli, such as that associated with feeding, insulin, or physical activity. For example, while the ingestion or infusion of large quantities of amino acids/protein (∼30–40 g) yields similar increases in muscle protein synthesis in both young and older individuals [114, 117–122], recent studies indicate that older adults exhibit a diminished accretion of muscle proteins after the ingestion of smaller amounts of essential amino acids (6–15 g) [112, 113]. Similarly, several recent studies have reported a blunted muscle protein synthesis response following an acute bout of resistance exercise in older subjects [123–125]. These effects are likely due to deficits in the mammalian target of rapamycin signaling pathway [111, 126], extracellular-related kinase 1/2 signaling pathway [127], and/or upregulation of the ubiquitin proteasome pathway in the elderly [128].
In addition, an increasing number of investigations report an age-related decline in autophagy (for recent reviews, c.f. [129, 130]). Sometimes referred to as “cell death type II,” autophagy is a process of cell and organelle degradation similar to, but distinct from, apoptosis [131, 132]. Although it can contribute to cell death in a number of situations (e.g., starvation, growth factor deprivation), autophagy also serves valuable housekeeping functions in normal, healthy cells by removing damaged or dysfunctional organelles [132]. This latter function is often referred to as macroautophagy, and recent evidence suggests that this process is lost or impaired in aging muscles. It is hypothesized that impaired autophagy leads to the accumulation of dysfunctional, damaged proteins, lipids, and nucleic acids that function at a suboptimal level. Dysfunctional contractile proteins, for example, might produce less force than normal ones and, thus, could contribute to impaired muscle quality. Moreover, the accumulation of these damaged cellular components may initiate cellular apoptosis, leading to a loss of muscle mass, thus contributing to sarcopenia. In support of this hypothesis, caloric restriction has been shown to restore markers of autophagy in skeletal muscle [132] and preserve muscle size and function [133, 134].
In addition to muscle size and anatomical structure, aged muscle also appears to differ in other compositional manners. For instance, over the past decade, numerous studies have reported that aging increases the adipocyte content between muscle groups (intermuscular adipose tissue) and between muscle fascicles (intramuscular adipose tissue) [10, 92, 93, 135, 136]. The earliest of these studies suggested that greater muscle fat content was associated with reduced muscle strength [135], suggesting a potential mechanistic link between increases in fat infiltration in muscle and muscle weakness. Indeed, cytokine production from adipose tissue has been linked to depressed muscle force production [94, 137], thus providing a theoretical basis to this assertion. However, more recent longitudinal data have failed to observe a direct relationship between increased levels of intermuscular adipose tissue and strength loss with age [10].
Age-related changes in contractile filaments
As noted, age-related declines in muscular force production were considered to be solely a function of reduced muscle mass for some time. It is no surprise then, that substantial attention has been devoted to age-related changes in the contractile proteins actin and myosin, which make up the majority of the volume of a skeletal muscle cell. Although sarcomeric actin seems to be quite uniform across muscle cells, myosin, in particular the myosin heavy chain (MHC), is not. In fact, muscle cells (fibers) are frequently differentiated by which isoform(s) of myosin they express. These different myosin isoforms are associated with different levels of ATP consumption—type I (i.e., slow) consume less ATP than type II (i.e., fast) isoforms at maximum levels of contractile activation [138–142]. Studies suggest that metabolic cost of type I < type IIa < type IIx < type IIb fibers. While humans do not express type IIb myosin, this pattern appears to hold for the three principal isoforms expressed in human muscle. Aging is associated with a loss of skeletal muscle mass (sarcopenia), and since actin and myosin are the predominant proteins in skeletal muscle, an overall loss in these proteins is observed with aging [143–146].
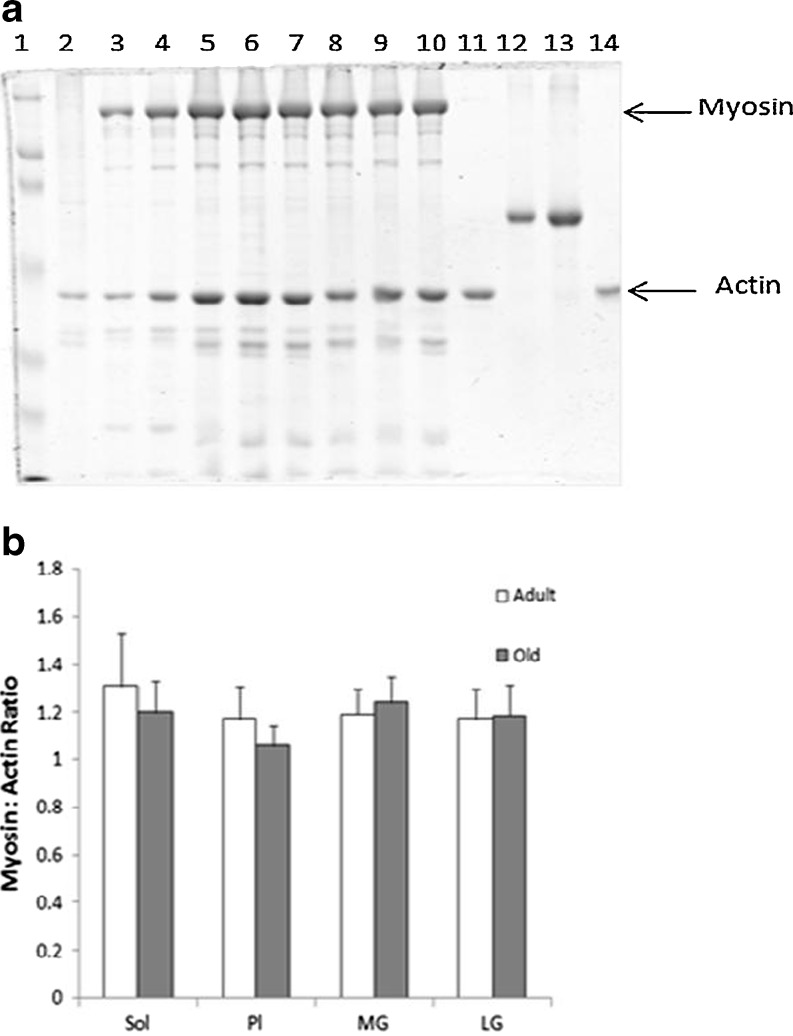
Some investigators have reported an age-related decline in the myosin/actin ratio in rat muscles [146], which might be expected to alter force production, as has been suggested in studies of disuse and microgravity [147, 148]. Of note, this change occurred in the semimembranosus, but not the soleus muscle, and was observed only in very old, but not old animals [146]. Our own data from aging, but not very old, rats indicate no significant changes in this ratio in any of the principal plantar flexor muscles (Fig. 4), further suggesting that this change may be muscle specific.
Fig. 4.
Lack of difference in myosin/actin ratio between adult (6–8 months) and old (24 months) muscles. a Representative Coomassie-stained gel. Lane 1, molecular weight markers; lane 2, myofibrillar fraction from a previous experiment for positive control; lanes 11 and 14, actin standards of 2.0 and 1.0 μg, respectively; lanes 12 and 13, BSA standards of 2.5 and 5 μg, respectively; lanes 3 and 4, adult and old soleus; lanes 5 and 6, adult and old plantaris; lanes 7 and 8, adult and old medial gastrocnemius; lanes 9 and 10, adult and old lateral gastrocnemius. b Mean (±SE) myosin/actin ratio for adult and old muscles (n = 8/group). Unpublished data from Russ Laboratory
In addition to loss of muscle mass, aging is also generally associated with a shift in fiber type. Although not universal, most studies of aging muscle reflect a shift in overall muscle phenotype from faster to slower MHC, such that a larger proportion of the remaining contractile mass is composed of slower MHC isoforms [149, 150]. Consistent with a slower overall muscle phenotype are observations of reduced potentiation in aged skeletal muscle [151–153]. This shift is believed to be the result of both greater atrophy of type II fibers as well as a relatively small loss of fast, type II fibers [106, 154, 155]. Such a shift may inherently alter muscle quality, as the specific tension of type II fibers is greater than that of type I fibers [156, 157]. Although the underlying mechanisms are not entirely clear, apoptotic loss of the α-motor neurons has been implicated [91, 158, 159]. A decline in overall habitual physical activity has been shown to occur with increasing age, but MHC changes due to disuse and detraining are typically observed to be the opposite of those seen with aging (i.e., from slower to faster isoforms).
In addition to the absolute amount of contractile protein, some investigators have reported age-related functional impairments of these proteins within single fibers [160] and even at the level of isolated myosin molecules [161, 162]. Lowe and colleagues demonstrated a reduction in the number of strongly bound crossbridges in maximally activated fibers of aged vs. young rats using electron paramagnetic resonance [97, 163, 164]. These functional deficits may be the result of a reduced mixed muscle protein and MHC turnover [165–168], which could in turn contribute to the accumulation of post-translational modifications that impair crossbridge function. These findings are also consistent with the role of age-related impairments of autophagy described earlier in this paper.
Finally, the thin filaments also contain tropomyosin and the troponin isoforms. Although these regulatory proteins are not part of the actin–myosin crossbridge, they are critical in opening up the myosin binding site on actin, which makes crossbridge formation possible. If either tropomyosin or troponin are not functioning properly, it is possible that fewer crossbridges will form (in effect reducing the calcium sensitivity of the muscle), generating less force which would result in reduced muscle quality [169]. Recent proteomics studies have suggested that increased age is associated with reduced expression of these proteins and increased post-translational modifications (e.g., nitration) [170–172], either of which could impair protein function. These proteins have received much less attention in the aging literature than the contractile proteins, and this area clearly needs more study in the future.
Age-related changes in muscular force transmission
Although actin and myosin are proteins responsible for the generation of muscular force (via the crossbridge cycle), functional force needs to be effectively transmitted to produce optimal function. Much force transmission in skeletal muscle takes place through a complex array of cytoskeletal proteins, and it is possible that deficiencies in these cytoskeletal proteins could reduce muscle quality by impairing force transmission. This topic has been largely unexplored, despite evidence from knockout animals that loss of at least one cytoskeletal protein, desmin, is associated with reduced muscle quality [173–176]. However, the few existing studies indicate that, if anything, desmin is increased with aging [145, 177, 178]. Interestingly, one group [179] has reported increased specific force in muscles from desmin knockout mice, speculating that desmin acts a “viscous element that dissipates mechanical energy.” If this is the case, then an age-associated increase in desmin could indeed contribute to impaired muscle quality with aging. Clearly, much further work needs to be done to explore the potential role of cytoskeletal changes in aging muscle function.
Age-related changes in excitation–contraction coupling
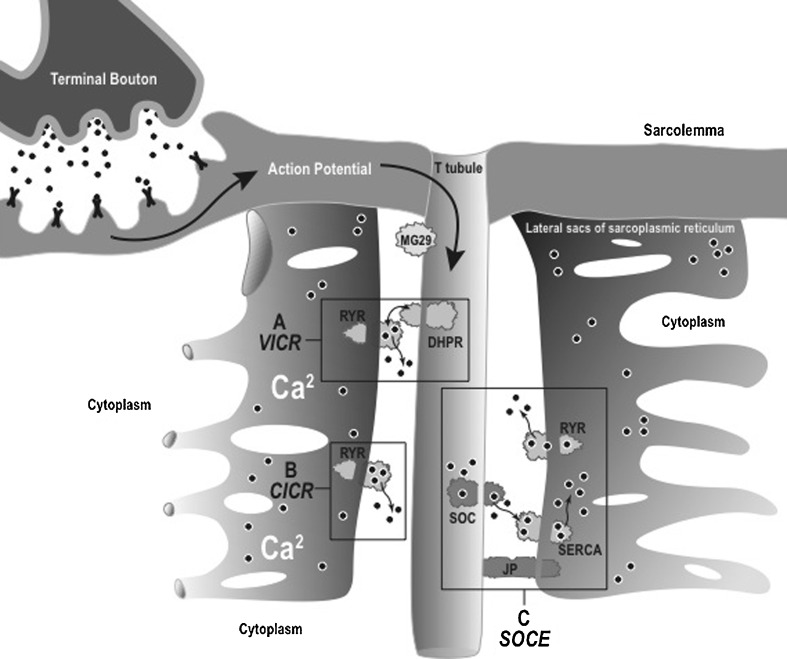
Excitation–contraction coupling (E−CC) converts the neural signal for muscle activation (muscle action potential) into muscle contraction and force development through a series of biophysical steps (Fig. 5). Briefly, the action potential spreads throughout the muscle via the t-tubular system, activating the voltage-sensitive dihydropyridine receptors (DHPRs), which subsequently open the ryanodine receptors (RYRs; Ca2+ release channels). This releases Ca2+ from its membranous storage area known (the sarcoplasmic reticulum (SR)). The newly released Ca2+ binds to troponin C which promotes crossbridge formation and force production. The Ca2+ is then returned to the SR by the sarcoplasmic reticulum Ca2+ pump (SR-ATPase) [180].
Fig. 5.
Graphical illustration of the excitation–contraction coupling process. VICR voltage-induced calcium release, CICR calcium-induced calcium release, SOCE store-operated calcium entry, RYR ryanodine receptor, DHPR dihydropyridine receptor, SERCA sarcoplasmic/endoplasmic reticulum calcium ATPase, JP juntophilin
Reuptake of Ca2+, in and of itself, contributes more to force relaxation than force generation. Thus, age-associated impairments of reuptake, if present, are more likely to play a significant role in phenomena such as task performance (i.e., motor coordination) and muscle fatigue than in weakness. However, impaired Ca2+ reuptake could lead to unwanted elevations of intramyocellular Ca2+ that could activate specific proteases (e.g., calpains). Although the main myofibrillar proteins actin and myosin are not believed to be substrates for calpains, many of the cytoskeletal elements that anchor the myofibrillar proteins are. Thus, increased calpain activity could disrupt myofibrillar integrity of the myofibrils, making them susceptible to degradation by the ubiquitin–proteasome system (for recent reviews, c.f. [181, 182]). In addition, elevated Ca2+ could activate several cell signaling pathways that could contribute to weakness by inducing muscle cell apoptosis [181]. Several investigators have reported reduced SR Ca2+ reuptake with aging [13, 183, 184], although if SR Ca2+ release declines with age as well (see below), this may not be a major issue, as there may be no net increase in calcium. The rest of this section will focus on SR Ca2+ release, as this is the aspect of E–CC most directly related to force production, and thus weakness.
The description of E–CC above outlines the predominant mechanism of Ca2+ release in skeletal muscle, also referred to as voltage-induced calcium release (VICR) and does not require transmembrane movement of extracellular calcium [185]. However, Ca2+-induced calcium release (CICR), which predominates in cardiac muscle, has also been shown to occur in skeletal muscle [186–188]. In this process, direct entry of extracellular Ca2+ into the myoplasm via activation of DHPRs that are not associated with RyRs occurs and triggers further mobilization of intracellular Ca2+ stores by activating RyRs. It has been suggested that this CICR may amplify the effects of VICR [189]. Finally, store-operated calcium entry (SOCE) is thought to serve to renew depleted Ca2+ in the SR via the opening of plasma membrane-located store-operated Ca2+ channels [190]. This allows extracellular Ca2+ to accumulate in the cytoplasm in order replenish SR Ca2+ [191]. Theoretically, disruption at any point in the E–CC process can prevent optimal activation of muscle mass and thus reduce muscle quality.
Impairments in SR Ca2+ release have been suggested to explain deficits of muscle quality in aged muscle [192–195], and in this regard, the role of Osvaldo Delbono must be acknowledged. Arguably, the idea that changes in E–CC were contributing to age-related weakness began with his reports of “excitation-calcium release uncoupling” in single fibers from aged human muscles [196]. Perhaps the most obvious mechanism for “uncoupling” of E–CC to account for loss of force production would be a reduction in the expression of the principal proteins in VICR. Although some early work indicated that RYR expression might be reduced with age, at least in fast muscles [194], a number of studies have not supported this hypothesis [184, 197–199]. There is more support for the age-related loss of DHPR (particularly the α-1s subunit), such that a greater number of RYRs are not associated with DHPR, causing the uncoupling and disrupting the VICR process [199–201]. More recently, attention has been focused on the β-1a subunit of the DHPR. This subunit has roles in chaperoning the α-1s subunit to the t-tubule membrane and regulating Ca2+ current [202–204]. It also interacts directly with RyR [205] and may impair E–CC by binding to charged residues on RyR [206]. Taylor et al. determined that DHPR-β1a increases significantly with age in fast, slow, and mixed murine muscle fibers and that overexpression of the subunit results in a decrease in α-1s subunits and a decline in specific force [207]. Finally, Payne et al. found that RNA inhibition of DHPR-β1a expression in FDB muscles of young and old mice caused a significant reduction of charge movement in young mice, but restored charge movement to young control levels in old mice [208].
Although the case for alterations of DHPR contributing to the age-related decline in muscle quality is compelling, other processes may be impaired as well. Data from our laboratory [13] and others [184] suggest that aging may impair SR calcium release, independent of DHPR function. In these experiments, the RYR was stimulated directly through pharmacological means in an SR vesicle preparation. Thus, SR function was compromised. Interestingly, we found that the older muscles also exhibited a reduced RYR–FKBP binding [13]. FKBP is a small immunophilin known to associate with the RYR, and reduced RYR–FKBP interaction has been linked to reduced muscle quality and impaired calcium release in models of aging, heart failure, and exhaustion [209–211]. While the cause of the reduced protein–protein interaction has not been definitively identified, data suggest that an age-related increase in RYR oxidation may be at work [209, 210]. Such a modification may be the result of reduced protein turnover with increasing age, allowing for greater accumulation of post-translational modifications such as oxidation [212]. Again, impaired autophagy may contribute to the problem, as oxidized RYR may not be removed and thus dysfunctional RYR will accumulate. Given that normal turnover of RYR is more rapid than that of myosin [212, 213], it could be that impaired autophagy may affect RYR earlier in the aging process than it does myosin.
Investigators have also begun examining a potential role for SR-related proteins that are not directly involved in SR Ca2+ release, with much attention given to junctophilin and mitsugumin 29 (MG29). These proteins are both associated with the triadic junctions between the t-tubules and terminal cisternae, and both appear necessary for normal triad organization and optimal E–CC [214–218]. Interestingly, MG29 has been linked to SOCE and has been shown to decline with aging [191, 195], and may contribute to the fragmentation of the SR, resulting in fragments of Ca2+-containing SR disconnected from the t-tubule membranes [219]. It has been hypothesized that this fragmentation occurs in a subpopulation of fibers that became at least partially dependent on extracellular Ca2+ for SR Ca2+. This phenomenon essentially shifts the E–CC mechanism from VICR to CICR [220]. Muscles containing higher percentages of such fibers dependent on SOCE would be at a force-generating disadvantage compared to normal skeletal muscle fibers that are not dependent upon the influx of Ca2+ from the t-tubule, particularly if the SR were depleted of Ca2+. The role for an age-associated decline in SOCE in impaired muscle quality remains unclear, however, as others have not found that age adversely affects either SOCE or calcium stores [208], and the conditions under which impairments in SOCE may affect force (i.e., prolonged, high-rate stimulation with long-duration pulses) may not occur during normal muscle function [221].
Because of the role of E–CC in linking neural signals to muscular responses, it is not surprising that a direct biochemical interaction between muscle and nerve may influence E–CC. There is evidence to suggest that muscle-specific IGF-1 may act in a paracrine, retrograde manner to preserve motor neuron function [222, 223]. This in turn is thought to lead to the preservation of E–CC and muscle quality [223, 224], possibly through the regulation of DHPR expression [225]. However, questions regarding the exact mechanisms and outcomes of IGF-1 overexpression remain [201].
Finally, it is worth noting that age-related changes in membrane composition of the SR itself may occur. While much attention has been focused on the age-related alterations of the proteins associated with the SR, it is well known that the function of integral membrane proteins is affected by the composition of the membranes in which they are situated [226–229]. Investigation along these lines has been quite limited. However, age-related changes in the SR phospholipid and fatty acid composition have been demonstrated [230, 231]. The contribution of such alterations in membrane composition on age-related changes in muscle function has not been characterized, but at least one group has observed an increased susceptibility to heat inactivation of SERCA function in the SR of aging rats [230].
Future directions
Muscle weakness is undoubtedly a debilitating and life-threatening condition in the elderly as it is highly associated with both mortality and physical disability. As argued in this article, voluntary muscle force production is not solely dependent upon muscle size, but rather results from a combination of neurologic and skeletal muscle factors, and that biologic properties of both of these systems are altered with aging. The scientific and medical communities have made substantial progress in recent years on developing a better understanding of the clinical significance of muscle weakness in older adults and the physiological mechanisms involved in muscle weakness; however, there is still substantial progress that needs to be made. For example, virtually all studies conducted to date examining age-related mechanisms of muscle weakness have used cross-sectional study designs. Unfortunately, delineating the true cause and effect relationships with designs of this nature—and thus determining the mechanistic underpinnings of muscle weakness in older adults—is difficult. Accordingly, longitudinal studies are needed, or at a minimum, case–control studies whereby healthy older adults are compared to older adults with low levels of muscle strength are needed. Experiments of this nature would help determine the relative contribution of the various segmental components of the neuromuscular system associated with muscle weakness and thereby identify potential therapeutic targets.
Acknowledgments
This work was support in part by Award Number R15HD065552 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development to BC Clark. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health. The authors would like to thank Danette Pratt, a Biomedical Illustrator in the Office of Communication at the Ohio University Heritage College of Osteopathic Medicine, for developing Fig. 5 depicting the excitation–contraction coupling process. The authors declare that they have no conflict of interest. The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle [232].
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Drs. Russ and Clark contributed equally to this article.
Contributor Information
David W. Russ, Email: russd@ohio.edu
Brian C. Clark, Email: clarkb2@ohio.edu
References
- 1.Federal Interagency Forum on Aging-Related Statistics . Older Americans 2008: key indicators of well-being. Washington: U.S. Government Printing Office; 2008. [Google Scholar]
- 2.Brooke JD, et al. Aging of human segmental oligosynaptic reflexes for control of leg movement. Neurobiol Aging. 1989;10:721–725. doi: 10.1016/0197-4580(89)90009-2. [DOI] [PubMed] [Google Scholar]
- 3.Cesari M, et al. Skeletal muscle and mortality results from the InCHIANTI Study. J Gerontol A Biol Sci Med Sci. 2009;64:377–384. doi: 10.1093/gerona/gln031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manini TM, et al. Knee extension strength cutpoints for maintaining mobility. J Am Geriatr Soc. 2007;55:451–457. doi: 10.1111/j.1532-5415.2007.01087.x. [DOI] [PubMed] [Google Scholar]
- 5.Newman AB, et al. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci. 2006;61:72–77. doi: 10.1093/gerona/61.1.72. [DOI] [PubMed] [Google Scholar]
- 6.Visser M, et al. Skeletal muscle mass and muscle strength in relation to lower-extremity performance in older men and women. J Am Geriatr Soc. 2000;48:381–386. doi: 10.1111/j.1532-5415.2000.tb04694.x. [DOI] [PubMed] [Google Scholar]
- 7.Visser M, et al. Change in muscle mass and muscle strength after a hip fracture: relationship to mobility recovery. J Gerontol A Biol Sci Med Sci. 2000;55:M434–M440. doi: 10.1093/gerona/55.8.M434. [DOI] [PubMed] [Google Scholar]
- 8.von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachex Sarcopenia Muscle. 2010;1:129–133. doi: 10.1007/s13539-010-0014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grimby G, Saltin B. The ageing muscle. Clin Physiol. 1983;3:209–218. doi: 10.1111/j.1475-097X.1983.tb00704.x. [DOI] [PubMed] [Google Scholar]
- 10.Delmonico MJ, et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90:1579–1585. doi: 10.3945/ajcn.2009.28047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark BC, et al. Adaptations in human neuromuscular function following prolonged unweighting: II. Neurological properties and motor imagery efficacy. J Appl Physiol. 2006;101:264–272. doi: 10.1152/japplphysiol.01404.2005. [DOI] [PubMed] [Google Scholar]
- 12.Clark BC, Fernhall B, Ploutz-Snyder LL. Adaptations in human neuromuscular function following prolonged unweighting: I. Skeletal muscle contractile properties and applied ischemia efficacy. J Appl Physiol. 2006;101:256–263. doi: 10.1152/japplphysiol.01402.2005. [DOI] [PubMed] [Google Scholar]
- 13.Russ DW, et al. Ageing, but not yet senescent, rats exhibit reduced muscle quality and sarcoplasmic reticulum function. Acta Physiol. 2011;201:391–403. doi: 10.1111/j.1748-1716.2010.02191.x. [DOI] [PubMed] [Google Scholar]
- 14.Clark BC, Manini TM. Sarcopenia =/= dynapenia. J Gerontol A Biol Sci Med Sci. 2008;63:829–834. doi: 10.1093/gerona/63.8.829. [DOI] [PubMed] [Google Scholar]
- 15.Tomas MT, et al. Body composition, muscle strength, functional capacity, and physical disability risk in liver transplanted familial amyloidotic polyneuropathy patients. Clin Transpl. 2011;25:E406–E414. doi: 10.1111/j.1399-0012.2011.01436.x. [DOI] [PubMed] [Google Scholar]
- 16.Scott D, et al. Statin therapy, muscle function and falls risk in community-dwelling older adults. QJM. 2009;102:625–633. doi: 10.1093/qjmed/hcp093. [DOI] [PubMed] [Google Scholar]
- 17.Delmonico MJ, et al. Association of the ACTN3 genotype and physical functioning with age in older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1227–1234. doi: 10.1093/gerona/63.11.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reid KF, et al. Lower extremity power training in elderly subjects with mobility limitations: a randomized controlled trial. Aging Clin Exp Res. 2008;20:337–343. doi: 10.1007/bf03324865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park SW, et al. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care. 2007;30:1507–1512. doi: 10.2337/dc06-2537. [DOI] [PubMed] [Google Scholar]
- 20.Brooks N, et al. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int J Med Sci. 2007;4:19–27. doi: 10.7150/ijms.4.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodpaster BH, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–1064. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- 22.Kostek MC, et al. Muscle strength response to strength training is influenced by insulin-like growth factor 1 genotype in older adults. J Appl Physiol. 2005;98:2147–2154. doi: 10.1152/japplphysiol.00817.2004. [DOI] [PubMed] [Google Scholar]
- 23.Katsiaras A, et al. Skeletal muscle fatigue, strength, and quality in the elderly: the Health ABC Study. J Appl Physiol. 2005;99:210–216. doi: 10.1152/japplphysiol.01276.2004. [DOI] [PubMed] [Google Scholar]
- 24.Newman AB, et al. Strength and muscle quality in a well-functioning cohort of older adults: the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:323–330. doi: 10.1046/j.1532-5415.2003.51105.x. [DOI] [PubMed] [Google Scholar]
- 25.Bigland-Ritchie B. Muscle fatigue and the influence of changing neural drive. Clin Chest Med. 1984;5:21–34. [PubMed] [Google Scholar]
- 26.Klass M, Baudry S, Duchateau J. Voluntary activation during maximal contraction with advancing age: a brief review. Eur J Appl Physiol. 2007;100:543–551. doi: 10.1007/s00421-006-0205-x. [DOI] [PubMed] [Google Scholar]
- 27.Ashe J. Force and the motor cortex. Behav Brain Res. 1997;87:255–269. doi: 10.1016/S0166-4328(97)00752-3. [DOI] [PubMed] [Google Scholar]
- 28.Rekling JC, et al. Synaptic control of motoneuronal excitability. Physiol Rev. 2000;80:767–852. doi: 10.1152/physrev.2000.80.2.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Behm D, Power K, Drinkwater E. Comparison of interpolation and central activation ratios as measures of muscle inactivation. Muscle Nerve. 2001;24:925–934. doi: 10.1002/mus.1090. [DOI] [PubMed] [Google Scholar]
- 30.Gandevia SC. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev. 2001;81:1725–1789. doi: 10.1152/physrev.2001.81.4.1725. [DOI] [PubMed] [Google Scholar]
- 31.Kent-Braun JA. Noninvasive measures of central and peripheral activation in human muscle fatigue. Muscle Nerve Suppl. 1997;5:S98–S101. doi: 10.1002/(SICI)1097-4598(1997)5+<98::AID-MUS23>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 32.Kent-Braun JA, Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19:861–869. doi: 10.1002/(SICI)1097-4598(199607)19:7<861::AID-MUS8>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 33.Merton PA. Voluntary strength and fatigue. J Physiol. 1954;123:553–564. doi: 10.1113/jphysiol.1954.sp005070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bilodeau M, et al. Fatigue of elbow flexor muscles in younger and older adults. Muscle Nerve. 2001;24:98–106. doi: 10.1002/1097-4598(200101)24:1<98::AID-MUS11>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 35.Callahan DM, Foulis SA, Kent-Braun JA. Age-related fatigue resistance in the knee extensor muscles is specific to contraction mode. Muscle Nerve. 2009;39:692–702. doi: 10.1002/mus.21278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cannon J, et al. Comparative effects of resistance training on peak isometric torque, muscle hypertrophy, voluntary activation and surface EMG between young and elderly women. Clin Physiol Funct Imaging. 2007;27:91–100. doi: 10.1111/j.1475-097X.2007.00719.x. [DOI] [PubMed] [Google Scholar]
- 37.Chung LH, Callahan DM, Kent-Braun JA. Age-related resistance to skeletal muscle fatigue is preserved during ischemia. J Appl Physiol. 2007;103:1628–1635. doi: 10.1152/japplphysiol.00320.2007. [DOI] [PubMed] [Google Scholar]
- 38.Connelly DM, et al. Motor unit firing rates and contractile properties in tibialis anterior of young and old men. J Appl Physiol. 1999;87:843–852. doi: 10.1152/jappl.1999.87.2.843. [DOI] [PubMed] [Google Scholar]
- 39.De Serres SJ, Enoka RM. Older adults can maximally activate the biceps brachii muscle by voluntary command. J Appl Physiol. 1998;84:284–291. doi: 10.1063/1.368025. [DOI] [PubMed] [Google Scholar]
- 40.Harridge SD, Kryger A, Stensgaard A. Knee extensor strength, activation, and size in very elderly people following strength training. Muscle Nerve. 1999;22:831–839. doi: 10.1002/(SICI)1097-4598(199907)22:7<831::AID-MUS4>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 41.Hunter SK, et al. Recovery from supraspinal fatigue is slowed in old adults after fatiguing maximal isometric contractions. J Appl Physiol. 2008;105:1199–1209. doi: 10.1152/japplphysiol.01246.2007. [DOI] [PubMed] [Google Scholar]
- 42.Jakobi JM, Rice CL. Voluntary muscle activation varies with age and muscle group. J Appl Physiol. 2002;93:457–462. doi: 10.1152/japplphysiol.00012.2002. [DOI] [PubMed] [Google Scholar]
- 43.Kent-Braun JA, Ng AV. Specific strength and voluntary muscle activation in young and elderly women and men. J Appl Physiol. 1999;87:22–29. doi: 10.1152/jappl.1999.87.1.22. [DOI] [PubMed] [Google Scholar]
- 44.Klass M, Baudry S, Duchateau J. Aging does not affect voluntary activation of the ankle dorsiflexors during isometric, concentric, and eccentric contractions. J Appl Physiol. 2005;99:31–38. doi: 10.1152/japplphysiol.01426.2004. [DOI] [PubMed] [Google Scholar]
- 45.Klein CS, Rice CL, Marsh GD. Normalized force, activation, and coactivation in the arm muscles of young and old men. J Appl Physiol. 2001;91:1341–1349. doi: 10.1152/jappl.2001.91.3.1341. [DOI] [PubMed] [Google Scholar]
- 46.Knight CA, Kamen G. Adaptations in muscular activation of the knee extensor muscles with strength training in young and older adults. J Electromyogr Kinesiol. 2001;11:405–412. doi: 10.1016/S1050-6411(01)00023-2. [DOI] [PubMed] [Google Scholar]
- 47.Lanza IR, Russ DW, Kent-Braun JA. Age-related enhancement of fatigue resistance is evident in men during both isometric and dynamic tasks. J Appl Physiol. 2004;97:967–975. doi: 10.1152/japplphysiol.01351.2003. [DOI] [PubMed] [Google Scholar]
- 48.Roos MR, et al. Quadriceps muscle strength, contractile properties, and motor unit firing rates in young and old men. Muscle Nerve. 1999;22:1094–1103. doi: 10.1002/(SICI)1097-4598(199908)22:8<1094::AID-MUS14>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 49.Simoneau E, Martin A, Van Hoecke J. Muscular performances at the ankle joint in young and elderly men. J Gerontol A Biol Sci Med Sci. 2005;60:439–447. doi: 10.1093/gerona/60.4.439. [DOI] [PubMed] [Google Scholar]
- 50.Stevens JE, et al. Are voluntary muscle activation deficits in older adults meaningful? Muscle Nerve. 2003;27:99–101. doi: 10.1002/mus.10279. [DOI] [PubMed] [Google Scholar]
- 51.Wilder MR, Cannon J. Effect of age on muscle activation and twitch properties during static and dynamic actions. Muscle Nerve. 2009;39:683–691. doi: 10.1002/mus.21233. [DOI] [PubMed] [Google Scholar]
- 52.Yue GH, et al. Older adults exhibit a reduced ability to fully activate their biceps brachii muscle. J Gerontol A Biol Sci Med Sci. 1999;54:M249–M253. doi: 10.1093/gerona/54.5.M249. [DOI] [PubMed] [Google Scholar]
- 53.Yoon T, De-Lap BS, Griffith EE, Hunter SK. Age-related muscle fatigue after a low-force fatiguing contraction is explained by central fatigue. Muscle Nerve. 2007;37:457–466. doi: 10.1002/mus.20969. [DOI] [PubMed] [Google Scholar]
- 54.Haug H, Eggers R. Morphometry of the human cortex cerebri and corpus striatum during aging. Neurobiol Aging. 1991;12:336–338. doi: 10.1016/0197-4580(91)90013-A. [DOI] [PubMed] [Google Scholar]
- 55.Ward NS. Compensatory mechanisms in the aging motor system. Ageing Res Rev. 2006;5:239–254. doi: 10.1016/j.arr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 56.Salat DH, et al. Thinning of the cerebral cortex in aging. Cereb Cortex. 2004;14:721–730. doi: 10.1093/cercor/bhh032. [DOI] [PubMed] [Google Scholar]
- 57.Marner L, et al. Marked loss of myelinated nerve fibers in the human brain with age. J Comp Neurol. 2003;462:144–152. doi: 10.1002/cne.10714. [DOI] [PubMed] [Google Scholar]
- 58.Madden DJ, et al. Diffusion tensor imaging of adult age differences in cerebral white matter: relation to response time. Neuroimage. 2004;21:1174–1181. doi: 10.1016/j.neuroimage.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 59.Carlsson A. Treatment of Parkinson’s with L-DOPA. The early discovery phase, and a comment on current problems. J Neural Transm. 2002;109:777–787. doi: 10.1007/s007020200064. [DOI] [PubMed] [Google Scholar]
- 60.Morgan DG, May PC, Finch CE. Dopamine and serotonin systems in human and rodent brain: effects of age and neurodegenerative disease. J Am Geriatr Soc. 1987;35:334–345. doi: 10.1111/j.1532-5415.1987.tb04641.x. [DOI] [PubMed] [Google Scholar]
- 61.Bigham MH, Lidow MS. Adrenergic and serotonergic receptors in aged monkey neocortex. Neurobiol Aging. 1995;16:91–104. doi: 10.1016/0197-4580(95)80012-G. [DOI] [PubMed] [Google Scholar]
- 62.Bartus RT, et al. The cholinergic hypothesis of geriatric memory dysfunction. Science. 1982;217:408–414. doi: 10.1126/science.7046051. [DOI] [PubMed] [Google Scholar]
- 63.Segovia G, et al. Glutamatergic neurotransmission in aging: a critical perspective. Mech Ageing Dev. 2001;122:1–29. doi: 10.1016/S0047-6374(00)00225-6. [DOI] [PubMed] [Google Scholar]
- 64.Roth GS. Age changes in signal transduction and gene expression. Mech Ageing Dev. 1997;98:231–238. doi: 10.1016/S0047-6374(97)00110-3. [DOI] [PubMed] [Google Scholar]
- 65.Mora F, Segovia G, Del Arco A. Glutamate–dopamine–GABA interactions in the aging basal ganglia. Brain Res Rev. 2008;58:340–353. doi: 10.1016/j.brainresrev.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 66.Roth GS, Joseph JA. Cellular and molecular mechanisms of impaired dopaminergic function during aging. Ann N Y Acad Sci. 1994;719:129–135. doi: 10.1111/j.1749-6632.1994.tb56824.x. [DOI] [PubMed] [Google Scholar]
- 67.Hayashi M, Yamashita A, Shimizu K. Somatostatin and brain-derived neurotrophic factor mRNA expression in the primate brain: decreased levels of mRNAs during aging. Brain Res. 1997;749:283–289. doi: 10.1016/S0006-8993(96)01317-0. [DOI] [PubMed] [Google Scholar]
- 68.Volkow ND, et al. Dopamine transporters decrease with age. J Nucl Med. 1996;37:554–559. [PubMed] [Google Scholar]
- 69.Joseph JA, et al. Age-related changes in the nigrostriatum: a behavioral and biochemical analysis. J Gerontol. 1978;33:643–649. doi: 10.1093/geronj/33.5.643. [DOI] [PubMed] [Google Scholar]
- 70.Kossev AR, et al. Increased intracortical inhibition in middle-aged humans; a study using paired-pulse transcranial magnetic stimulation. Neurosci Lett. 2002;333:83–86. doi: 10.1016/S0304-3940(02)00986-2. [DOI] [PubMed] [Google Scholar]
- 71.Sale MV, Semmler JG. Age-related differences in corticospinal control during functional isometric contractions in left and right hands. J Appl Physiol. 2005;99:1483–1493. doi: 10.1152/japplphysiol.00371.2005. [DOI] [PubMed] [Google Scholar]
- 72.Smith AE, et al. Age-related changes in short-latency motor cortex inhibition. Exp Brain Res. 2009;198:489–500. doi: 10.1007/s00221-009-1945-8. [DOI] [PubMed] [Google Scholar]
- 73.McGinley M, et al. Older adults exhibit more intracortical inhibition and less intracortical facilitation than young adults. J Am Osteopathic Assoc. 2010;45:671–678. doi: 10.1016/j.exger.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Heuninckx S, et al. Neural basis of aging: the penetration of cognition into action control. J Neurosci. 2005;25:6787–6796. doi: 10.1523/JNEUROSCI.1263-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Naccarato M, et al. Does healthy aging affect the hemispheric activation balance during paced index-to-thumb opposition task? An fMRI study. Neuroimage. 2006;32:1250–1256. doi: 10.1016/j.neuroimage.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 76.Rowe JB, et al. Aging is associated with contrasting changes in local and distant cortical connectivity in the human motor system. Neuroimage. 2006;32:747–760. doi: 10.1016/j.neuroimage.2006.03.061. [DOI] [PubMed] [Google Scholar]
- 77.Fathi D, et al. Effects of aging on the human motor cortical plasticity studied by paired associative stimulation. Clin Neurophysiol. 2010;121:90–93. doi: 10.1016/j.clinph.2009.07.048. [DOI] [PubMed] [Google Scholar]
- 78.Sawaki L, et al. Age-dependent changes in the ability to encode a novel elementary motor memory. Ann Neurol. 2003;53:521–524. doi: 10.1002/ana.10529. [DOI] [PubMed] [Google Scholar]
- 79.Kobayashi M, Pascual-Leone A. Transcranial magnetic stimulation in neurology. Lancet Neurol. 2003;2:145–156. doi: 10.1016/S1474-4422(03)00321-1. [DOI] [PubMed] [Google Scholar]
- 80.McGinley MP, Clark BC. Transcranial magnetic stimulation and the human neuromuscular system. In: Costa A, Villalba E, editors. Horizons in neuroscience research. Hauppauge: Nova Science; 2011. pp. 69–88. [Google Scholar]
- 81.Florian J, et al. Inhibitory circuits and the nature of their interactions in the human motor cortex—a pharmacological TMS study. J Physiol. 2008;586:495–514. doi: 10.1113/jphysiol.2007.142059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ziemann U. Pharmacology of TMS. Suppl Clin Neurophysiol. 2003;56:226–231. doi: 10.1016/S1567-424X(09)70226-0. [DOI] [PubMed] [Google Scholar]
- 83.McDonnell MN, Orekhov Y, Ziemann U. The role of GABA(B) receptors in intracortical inhibition in the human motor cortex. Exp Brain Res. 2006;173:86–93. doi: 10.1007/s00221-006-0365-2. [DOI] [PubMed] [Google Scholar]
- 84.Reis J, et al. Contribution of transcranial magnetic stimulation to the understanding of cortical mechanisms involved in motor control. J Physiol. 2008;586:325–351. doi: 10.1113/jphysiol.2007.144824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ziemann U. TMS and drugs. Clin Neurophysiol. 2004;115:1717–1729. doi: 10.1016/j.clinph.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 86.Powers RK, Binder MD. Input–output functions of mammalian motoneurons. Rev Physiol Biochem Pharmacol. 2001;143:137–263. doi: 10.1007/BFb0115594. [DOI] [PubMed] [Google Scholar]
- 87.Henneman E, Somjen G, Carpenter DO. Excitability and inhibitability of motoneurons of different sizes. J Neurophysiol. 1965;28:599–620. doi: 10.1152/jn.1965.28.3.599. [DOI] [PubMed] [Google Scholar]
- 88.Powers RK, Turker KS, Binder MD. What can be learned about motoneurone properties from studying firing patterns? Adv Exp Med Biol. 2002;508:199–205. doi: 10.1007/978-1-4615-0713-0_24. [DOI] [PubMed] [Google Scholar]
- 89.Heckman CJ. Active conductances in motoneuron dendrites enhance movement capabilities. Exerc Sport Sci Rev. 2003;31:96–101. doi: 10.1097/00003677-200304000-00008. [DOI] [PubMed] [Google Scholar]
- 90.Heckman CJ, Lee RH, Brownstone RM. Hyperexcitable dendrites in motoneurons and their neuromodulatory control during motor behavior. Trends Neurosci. 2003;26:688–695. doi: 10.1016/j.tins.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 91.Tomlinson BE, Irving D. The numbers of limb motor neurons in the human lumbosacral cord throughout life. J Neurol Sci. 1977;34:213–219. doi: 10.1016/0022-510X(77)90069-7. [DOI] [PubMed] [Google Scholar]
- 92.Siu PM, Alway SE. Response and adaptation of skeletal muscle to denervation stress: the role of apoptosis in muscle loss. Frontiers Biosci: J Virtual Libr. 2009;14:432–452. doi: 10.2741/3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vandervoort AA. Aging of the human neuromuscular system. Muscle Nerve. 2002;25:17–25. doi: 10.1002/mus.1215. [DOI] [PubMed] [Google Scholar]
- 94.Deschenes MR, et al. Remodeling of the neuromuscular junction precedes sarcopenia related alterations in myofibers. Exp Gerontol. 2010;45:389–393. doi: 10.1016/j.exger.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Andonian MH, Fahim MA. Effects of endurance exercise on the morphology of mouse neuromuscular junctions during ageing. J Neurocytol. 1987;16:589–599. doi: 10.1007/BF01637652. [DOI] [PubMed] [Google Scholar]
- 96.Courtney J, Steinbach JH. Age changes in neuromuscular junction morphology and acetylcholine receptor distribution on rat skeletal muscle fibres. J Physiol. 1981;320:435–447. doi: 10.1113/jphysiol.1981.sp013960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Oda K. Age changes of motor innervation and acetylcholine receptor distribution on human skeletal muscle fibres. J Neurol Sci. 1984;66:327–338. doi: 10.1016/0022-510X(84)90021-2. [DOI] [PubMed] [Google Scholar]
- 98.Robbins N, Fahim MA. Progression of age changes in mature mouse motor nerve terminals and its relation to locomotor activity. J Neurocytol. 1985;14:1019–1036. doi: 10.1007/BF01224810. [DOI] [PubMed] [Google Scholar]
- 99.Deschenes MR, Wilson MH. Age-related differences in synaptic plasticity following muscle unloading. J Neurobiol. 2003;57:246–256. doi: 10.1002/neu.10271. [DOI] [PubMed] [Google Scholar]
- 100.Fahim MA, Robbins N. Ultrastructural studies of young and old mouse neuromuscular junctions. J Neurocytol. 1982;11:641–656. doi: 10.1007/BF01262429. [DOI] [PubMed] [Google Scholar]
- 101.Deschenes MR. Motor unit and neuromuscular junction remodeling with aging. Curr Aging Sci. 2011;4:209–220. doi: 10.2174/1874609811104030209. [DOI] [PubMed] [Google Scholar]
- 102.Morita H, et al. Progressive decrease in heteronymous monosynaptic Ia facilitation with human ageing. Exp Brain Res Experimentelle Hirnforschung Experiment Cerebrale. 1995;104:167–170. doi: 10.1007/BF00229867. [DOI] [PubMed] [Google Scholar]
- 103.Kamen G, et al. Motor unit discharge behavior in older adults during maximal-effort contractions. J Appl Physiol. 1995;79:1908–1913. doi: 10.1152/jappl.1995.79.6.1908. [DOI] [PubMed] [Google Scholar]
- 104.Tracy BL, et al. Variability of motor unit discharge and force fluctuations across a range of muscle forces in older adults. Muscle Nerve. 2005;32:533–540. doi: 10.1002/mus.20392. [DOI] [PubMed] [Google Scholar]
- 105.Christie A, Kamen G. Doublet discharges in motoneurons of young and older adults. J Neurophysiol. 2006;95:2787–2795. doi: 10.1152/jn.00685.2005. [DOI] [PubMed] [Google Scholar]
- 106.Lexell J, Taylor CC, Sjostrom M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J Neurol Sci. 1988;84:275–294. doi: 10.1016/0022-510X(88)90132-3. [DOI] [PubMed] [Google Scholar]
- 107.Lee WS, et al. Age-associated decrease of type IIA/B human skeletal muscle fibers. Clin Orthop Relat Res. 2006;450:231–237. doi: 10.1097/01.blo.0000218757.97063.21. [DOI] [PubMed] [Google Scholar]
- 108.Jakobsson F, Borg K, Edstrom L. Fibre-type composition, structure and cytoskeletal protein location of fibres in anterior tibial muscle. Comparison between young adults and physically active aged humans. Acta Neuropathol. 1990;80:459–468. doi: 10.1007/BF00294604. [DOI] [PubMed] [Google Scholar]
- 109.Lenk K, Schuler G, Adams V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachex Sarcopenia Muscle. 2010;1:9–21. doi: 10.1007/s13539-010-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fry CS, Rasmussen BB. Skeletal muscle protein balance and metabolism in the elderly. Curr Aging Sci. 2011;4:260–268. doi: 10.2174/1874609811104030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cuthbertson D, et al. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J. 2005;19:422–424. doi: 10.1096/fj.04-2640fje. [DOI] [PubMed] [Google Scholar]
- 112.Katsanos CS, et al. Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am J Clin Nutr. 2005;82:1065–1073. doi: 10.1093/ajcn/82.5.1065. [DOI] [PubMed] [Google Scholar]
- 113.Katsanos CS, et al. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am J Physiol Endocrinol Metab. 2006;291:E381–E387. doi: 10.1152/ajpendo.00488.2005. [DOI] [PubMed] [Google Scholar]
- 114.Volpi E, et al. Oral amino acids stimulate muscle protein anabolism in the elderly despite higher first-pass splanchnic extraction. Am J Physiol. 1999;277:E513–E520. doi: 10.1152/ajpendo.1999.277.3.E513. [DOI] [PubMed] [Google Scholar]
- 115.Volpi E, et al. The response of muscle protein anabolism to combined hyperaminoacidemia and glucose-induced hyperinsulinemia is impaired in the elderly. J Clin Endocrinol Metabol. 2000;85:4481–4490. doi: 10.1210/jc.85.12.4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Volpi E, et al. Basal muscle amino acid kinetics and protein synthesis in healthy young and older men. JAMA. 2001;286:1206–1212. doi: 10.1001/jama.286.10.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rasmussen BB, Wolfe RR, Volpi E. Oral and intravenously administered amino acids produce similar effects on muscle protein synthesis in the elderly. J Nutr Health Aging. 2002;6:358–362. [PMC free article] [PubMed] [Google Scholar]
- 118.Paddon-Jones D, et al. Amino acid ingestion improves muscle protein synthesis in the young and elderly. Am J Physiol Endocrinol Metab. 2004;286:E321–E328. doi: 10.1152/ajpendo.00368.2003. [DOI] [PubMed] [Google Scholar]
- 119.Paddon-Jones D, et al. Differential stimulation of muscle protein synthesis in elderly humans following isocaloric ingestion of amino acids or whey protein. Exp Gerontol. 2006;41:215–219. doi: 10.1016/j.exger.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 120.Rennie MJ, et al. Muscle protein synthesis measured by stable isotope techniques in man: the effects of feeding and fasting. Clin Sci. 1982;63:519–523. doi: 10.1042/cs0630519. [DOI] [PubMed] [Google Scholar]
- 121.Volpi E, et al. Exogenous amino acids stimulate net muscle protein synthesis in the elderly. J Clin Invest. 1998;101:2000–2007. doi: 10.1172/JCI939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Volpi E, et al. Essential amino acids are primarily responsible for the amino acid stimulation of muscle protein anabolism in healthy elderly adults. Am J Clin Nutr. 2003;78:250–258. doi: 10.1093/ajcn/78.2.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sheffield-Moore M, et al. Mixed muscle and hepatic derived plasma protein metabolism is differentially regulated in older and younger men following resistance exercise. Am J Physiol Endocrinol Metab. 2005;288:E922–E929. doi: 10.1152/ajpendo.00358.2004. [DOI] [PubMed] [Google Scholar]
- 124.Kumar V, et al. Age-related differences in the dose–response relationship of muscle protein synthesis to resistance exercise in young and old men. J Physiol. 2009;587:211–217. doi: 10.1113/jphysiol.2008.164483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mayhew DL, et al. Translational signaling responses preceding resistance training-mediated myofiber hypertrophy in young and old humans. J Appl Physiol. 2009;107:1655–1662. doi: 10.1152/japplphysiol.91234.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Guillet C, et al. Impaired anabolic response of muscle protein synthesis is associated with S6K1 dysregulation in elderly humans. FASEB J. 2004;18:1586–1587. doi: 10.1096/fj.03-1341fje. [DOI] [PubMed] [Google Scholar]
- 127.Drummond MJ, et al. Skeletal muscle protein anabolic response to resistance exercise and essential amino acids is delayed with aging. J Appl Physiol. 2008;104:1452–1461. doi: 10.1152/japplphysiol.00021.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Altun M, et al. Muscle wasting in aged, sarcopenic rats is associated with enhanced activity of the ubiquitin proteasome pathway. J Biol Chem. 2010;285:39597–39608. doi: 10.1074/jbc.M110.129718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Eskelinen EL, Saftig P. Autophagy: a lysosomal degradation pathway with a central role in health and disease. Biochim Biophys Acta. 2009;1793:664–673. doi: 10.1016/j.bbamcr.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 130.Rajawat YS, Hilioti Z, Bossis I. Aging: central role for autophagy and the lysosomal degradative system. Ageing Res Rev. 2009;8:199–213. doi: 10.1016/j.arr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 131.McMullen CA, et al. Age-related changes of cell death pathways in rat extraocular muscle. Exp Gerontol. 2009;44:420–425. doi: 10.1016/j.exger.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wohlgemuth SE, et al. Skeletal muscle autophagy and apoptosis during aging: effects of calorie restriction and life-long exercise. Exp Gerontol. 2010;45:138–148. doi: 10.1016/j.exger.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lee CM, et al. Influences of caloric restriction on age-associated skeletal muscle fiber characteristics and mitochondrial changes in rats and mice. Ann N Y Acad Sci. 1998;854:182–191. doi: 10.1111/j.1749-6632.1998.tb09901.x. [DOI] [PubMed] [Google Scholar]
- 134.Marzetti E, et al. Sarcopenia of aging: underlying cellular mechanisms and protection by calorie restriction. Biofactors. 2009;35:28–35. doi: 10.1002/biof.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Goodpaster BH, et al. Skeletal muscle attenuation determined by computed tomography is associated with skeletal muscle lipid content. J Appl Physiol. 2000;89:104–110. doi: 10.1152/jappl.2000.89.1.104. [DOI] [PubMed] [Google Scholar]
- 136.Kurz MJ, Stergiou N. The aging human neuromuscular system expresses less certainty for selecting joint kinematics during gait. Neurosci Lett. 2003;348:155–158. doi: 10.1016/S0304-3940(03)00736-5. [DOI] [PubMed] [Google Scholar]
- 137.Christie A, Kamen G. Short-term training adaptations in maximal motor unit firing rates and afterhyperpolarization duration. Muscle Nerve. 2010;41:651–660. doi: 10.1002/mus.21539. [DOI] [PubMed] [Google Scholar]
- 138.Han YS, et al. ATP consumption rate per cross bridge depends on myosin heavy chain isoform. J Appl Physiol. 2003;94:2188–2196. doi: 10.1063/1.1595709. [DOI] [PubMed] [Google Scholar]
- 139.He ZH, et al. ATP consumption and efficiency of human single muscle fibers with different myosin isoform composition. Biophys J. 2000;79:945–961. doi: 10.1016/S0006-3495(00)76349-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rivero JL, Talmadge RJ, Edgerton VR. Interrelationships of myofibrillar ATPase activity and metabolic properties of myosin heavy chain-based fibre types in rat skeletal muscle. Histochem Cell Biol. 1999;111:277–287. doi: 10.1007/s004180050358. [DOI] [PubMed] [Google Scholar]
- 141.Stienen GJ, et al. Myofibrillar ATPase activity in skinned human skeletal muscle fibres: fibre type and temperature dependence. J Physiol. 1996;493:299–307. doi: 10.1113/jphysiol.1996.sp021384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Szentesi P, et al. ATP utilization for calcium uptake and force production in different types of human skeletal muscle fibres. J Physiol. 2001;531:393–403. doi: 10.1111/j.1469-7793.2001.0393i.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.D’Antona G, et al. The effect of ageing and immobilization on structure and function of human skeletal muscle fibres. J Physiol. 2003;552:499–511. doi: 10.1113/jphysiol.2003.046276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Haddad F, Adams GR. Aging-sensitive cellular and molecular mechanisms associated with skeletal muscle hypertrophy. J Appl Physiol. 2006;100:1188–1203. doi: 10.1152/japplphysiol.01227.2005. [DOI] [PubMed] [Google Scholar]
- 145.Piec I, et al. Differential proteome analysis of aging in rat skeletal muscle. FASEB J. 2005;19:1143–1145. doi: 10.1096/fj.04-3084fje. [DOI] [PubMed] [Google Scholar]
- 146.Thompson LV, et al. Myosin and actin expression and oxidation in aging muscle. J Appl Physiol. 2006;101:1581–1587. doi: 10.1152/japplphysiol.00426.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Clark BC. In vivo alterations in skeletal muscle form and function after disuse atrophy. Med Sci Sports Exerc. 2009;41:1869–1875. doi: 10.1249/MSS.0b013e3181a645a6. [DOI] [PubMed] [Google Scholar]
- 148.Riley DA, et al. Decreased thin filament density and length in human atrophic soleus muscle fibers after spaceflight. J Appl Physiol. 2000;88:567–572. doi: 10.1152/jappl.2000.88.2.567. [DOI] [PubMed] [Google Scholar]
- 149.Klitgaard H, et al. Ageing alters the myosin heavy chain composition of single fibres from human skeletal muscle. Acta Physiol Scand. 1990;140:55–62. doi: 10.1111/j.1748-1716.1990.tb08975.x. [DOI] [PubMed] [Google Scholar]
- 150.Sullivan VK, et al. Myosin heavy chain composition in young and old rat skeletal muscle: effects of endurance exercise. J Appl Physiol. 1995;78:2115–2120. doi: 10.1152/jappl.1995.78.6.2115. [DOI] [PubMed] [Google Scholar]
- 151.Carlsen RC, Walsh DA. Decrease in force potentiation and appearance of alpha-adrenergic mediated contracture in aging rat skeletal muscle. Pflugers Archiv: Eur J Physiol. 1987;408:224–230. doi: 10.1007/BF02181463. [DOI] [PubMed] [Google Scholar]
- 152.Petrella RJ, et al. Comparison of twitch potentiation in the gastrocnemius of young and elderly men. Eur J Appl Physiol Occup Physiol. 1989;58:395–399. doi: 10.1007/BF00643515. [DOI] [PubMed] [Google Scholar]
- 153.Russ DW, et al. Contrasting influences of age and sex on muscle fatigue. Med Sci Sports Exerc. 2008;40:234–241. doi: 10.1249/mss.0b013e31815bbb93. [DOI] [PubMed] [Google Scholar]
- 154.Larsson L. Morphological and functional characteristics of the ageing skeletal muscle in man. A cross-sectional study. Acta Physiol Scand Suppl. 1978;457:1–36. doi: 10.1111/j.1748-1716.1978.tb06041.x. [DOI] [PubMed] [Google Scholar]
- 155.Lexell J, et al. Distribution of different fiber types in human skeletal muscles: effects of aging studied in whole muscle cross sections. Muscle Nerve. 1983;6:588–595. doi: 10.1002/mus.880060809. [DOI] [PubMed] [Google Scholar]
- 156.Geiger PC, et al. Maximum specific force depends on myosin heavy chain content in rat diaphragm muscle fibers. J Appl Physiol. 2000;89:695–703. doi: 10.1152/jappl.2000.89.2.695. [DOI] [PubMed] [Google Scholar]
- 157.Bodine SC, et al. Maximal force as a function of anatomical features of motor units in the cat tibialis anterior. J Neurophysiol. 1987;57:1730–1745. doi: 10.1152/jn.1987.57.6.1730. [DOI] [PubMed] [Google Scholar]
- 158.Deschenes MR. Effects of aging on muscle fibre type and size. Sports Med. 2004;34:809–824. doi: 10.2165/00007256-200434120-00002. [DOI] [PubMed] [Google Scholar]
- 159.Ulfhake B, et al. Regulation of neurotrophin signaling in aging sensory and motoneurons: dissipation of target support? Mol Neurobiol. 2000;21:109–135. doi: 10.1385/MN:21:3:109. [DOI] [PubMed] [Google Scholar]
- 160.Larsson L, Li X, Frontera WR. Effects of aging on shortening velocity and myosin isoform composition in single human skeletal muscle cells. Am J Physiol. 1997;272:C638–C649. doi: 10.1152/ajpcell.1997.272.2.C638. [DOI] [PubMed] [Google Scholar]
- 161.Hook P, Larsson L. Actomyosin interactions in a novel single muscle fiber in vitro motility assay. J Muscle Res Cell Motil. 2000;21:357–365. doi: 10.1023/A:1005614212575. [DOI] [PubMed] [Google Scholar]
- 162.Hook P, et al. In vitro motility speed of slow myosin extracted from single soleus fibres from young and old rats. J Physiol. 1999;520:463–471. doi: 10.1111/j.1469-7793.1999.00463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Lowe DA, et al. Electron paramagnetic resonance reveals age-related myosin structural changes in rat skeletal muscle fibers. Am J Physiol Cell Physiol. 2001;280:C540–C547. doi: 10.1152/ajpcell.2001.280.3.C540. [DOI] [PubMed] [Google Scholar]
- 164.Lowe DA, et al. Muscle activity and aging affect myosin structural distribution and force generation in rat fibers. J Appl Physiol. 2004;96:498–506. doi: 10.1152/japplphysiol.00842.2003. [DOI] [PubMed] [Google Scholar]
- 165.Balagopal P, et al. Effects of aging on in vivo synthesis of skeletal muscle myosin heavy-chain and sarcoplasmic protein in humans. Am J Physiol. 1997;273:E790–E800. doi: 10.1152/ajpendo.1997.273.4.E790. [DOI] [PubMed] [Google Scholar]
- 166.Koopman R, et al. Co-ingestion of protein and leucine stimulates muscle protein synthesis rates to the same extent in young and elderly lean men. Am J Clin Nutr. 2006;84:623–632. doi: 10.1093/ajcn/84.3.623. [DOI] [PubMed] [Google Scholar]
- 167.Short KR, et al. Age and aerobic exercise training effects on whole body and muscle protein metabolism. Am J Physiol Endocrinol Metab. 2004;286:E92–E101. doi: 10.1152/ajpendo.00366.2003. [DOI] [PubMed] [Google Scholar]
- 168.Welle S, Thornton C, Statt M. Myofibrillar protein synthesis in young and old human subjects after three months of resistance training. Am J Physiol. 1995;268:E422–E427. doi: 10.1152/ajpendo.1995.268.3.E422. [DOI] [PubMed] [Google Scholar]
- 169.Kawai M, Ishiwata S. Use of thin filament reconstituted muscle fibres to probe the mechanism of force generation. J Muscle Res Cell Motil. 2006;27:455–468. doi: 10.1007/s10974-006-9075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kanski J, Hong SJ, Schoneich C. Proteomic analysis of protein nitration in aging skeletal muscle and identification of nitrotyrosine-containing sequences in vivo by nanoelectrospray ionization tandem mass spectrometry. J Biol Chem. 2005;280:24261–24266. doi: 10.1074/jbc.M501773200. [DOI] [PubMed] [Google Scholar]
- 171.Capitanio D, et al. Comparative proteomic profile of rat sciatic nerve and gastrocnemius muscle tissues in ageing by 2-D DIGE. Proteomics. 2009;9:2004–2020. doi: 10.1002/pmic.200701162. [DOI] [PubMed] [Google Scholar]
- 172.Donoghue P, et al. DIGE analysis of rat skeletal muscle proteins using nonionic detergent phase extraction of young adult versus aged gastrocnemius tissue. J Proteomics. 2010;73:1441–1453. doi: 10.1016/j.jprot.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 173.Balogh J, et al. Lower active force generation and improved fatigue resistance in skeletal muscle from desmin deficient mice. J Muscle Res Cell Motil. 2003;24:453–459. doi: 10.1023/A:1027353930229. [DOI] [PubMed] [Google Scholar]
- 174.Li Z, et al. Cardiovascular lesions and skeletal myopathy in mice lacking desmin. Dev Biol. 1996;175:362–366. doi: 10.1006/dbio.1996.0122. [DOI] [PubMed] [Google Scholar]
- 175.Sam M, et al. Desmin knockout muscles generate lower stress and are less vulnerable to injury compared with wild-type muscles. Am J Physiol Cell Physiol. 2000;279:C1116–C1122. doi: 10.1152/ajpcell.2000.279.4.C1116. [DOI] [PubMed] [Google Scholar]
- 176.Wieneke S, et al. Generation of tension by skinned fibers and intact skeletal muscles from desmin-deficient mice. Biochem Biophys Res Commun. 2000;278:419–425. doi: 10.1006/bbrc.2000.3810. [DOI] [PubMed] [Google Scholar]
- 177.Ansved T, Wallner P, Larsson L. Spatial distribution of motor unit fibres in fast- and slow-twitch rat muscles with special reference to age. Acta Physiol Scand. 1991;143:345–354. doi: 10.1111/j.1748-1716.1991.tb09242.x. [DOI] [PubMed] [Google Scholar]
- 178.Russ DW, Grandy JS. Increased desmin expression in hindlimb muscles of aging rats. J Cachex Sarcopenia Muscle. 2011;2:175–180. doi: 10.1007/s13539-011-0033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Boriek AM, et al. Desmin integrates the three-dimensional mechanical properties of muscles. Am J Physiol Cell Physiol. 2001;280:C46–C52. doi: 10.1152/ajpcell.2001.280.1.C46. [DOI] [PubMed] [Google Scholar]
- 180.Di Biase V, Franzini-Armstrong C. Evolution of skeletal type e–c coupling: a novel means of controlling calcium delivery. J Cell Biol. 2005;171:695–704. doi: 10.1083/jcb.200503077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Dargelos E, et al. Calcium-dependent proteolytic system and muscle dysfunctions: a possible role of calpains in sarcopenia. Biochimie. 2008;90:359–368. doi: 10.1016/j.biochi.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 182.Goll DE, et al. Myofibrillar protein turnover: the proteasome and the calpains. J Anim Sci. 2008;86:E19–E35. doi: 10.2527/jas.2007-0395. [DOI] [PubMed] [Google Scholar]
- 183.Hunter SK, et al. Human skeletal sarcoplasmic reticulum Ca2+ uptake and muscle function with aging and strength training. J Appl Physiol. 1999;86:1858–1865. doi: 10.1152/jappl.1999.86.6.1858. [DOI] [PubMed] [Google Scholar]
- 184.Thomas MM, et al. Initiating treadmill training in late middle age offers modest adaptations in Ca2+ handling but enhances oxidative damage in senescent rat skeletal muscle. Am J Physiol Regul Integr Comp Physiol. 2010;298:R1269–R1278. doi: 10.1152/ajpregu.00663.2009. [DOI] [PubMed] [Google Scholar]
- 185.Ma J, Pan Z. Junctional membrane structure and store operated calcium entry in muscle cells. Front Biosci: J Virtual Libr. 2003;8:d242–d255. doi: 10.2741/977. [DOI] [PubMed] [Google Scholar]
- 186.Berridge MJ. Calcium oscillations. J Biol Chem. 1990;265:9583–9586. [PubMed] [Google Scholar]
- 187.Clapham DE. Calcium signaling. Cell. 1995;80:259–268. doi: 10.1016/0092-8674(95)90408-5. [DOI] [PubMed] [Google Scholar]
- 188.Pozzan T, et al. Molecular and cellular physiology of intracellular calcium stores. Physiol Rev. 1994;74:595–636. doi: 10.2466/pr0.1994.74.2.595. [DOI] [PubMed] [Google Scholar]
- 189.Rios E, Pizarro G, Stefani E. Charge movement and the nature of signal transduction in skeletal muscle excitation–contraction coupling. Annu Rev Physiol. 1992;54:109–133. doi: 10.1146/annurev.ph.54.030192.000545. [DOI] [PubMed] [Google Scholar]
- 190.Putney JW., Jr The integration of receptor-regulated intracellular calcium release and calcium entry across the plasma membrane. Curr Top Cell Regul. 1990;31:111–127. doi: 10.1016/b978-0-12-152831-7.50004-4. [DOI] [PubMed] [Google Scholar]
- 191.Zhao X, et al. Compromised store-operated Ca2+ entry in aged skeletal muscle. Aging Cell. 2008;7:561–568. doi: 10.1111/j.1474-9726.2008.00408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Boncompagni S, et al. Progressive disorganization of the excitation–contraction coupling apparatus in aging human skeletal muscle as revealed by electron microscopy: a possible role in the decline of muscle performance. J Gerontol A Biol Sci Med Sci. 2006;61:995–1008. doi: 10.1093/gerona/61.10.995. [DOI] [PubMed] [Google Scholar]
- 193.Gonzalez E, Messi ML, Delbono O. The specific force of single intact extensor digitorum longus and soleus mouse muscle fibers declines with aging. J Membr Biol. 2000;178:175–183. doi: 10.1007/s002320010025. [DOI] [PubMed] [Google Scholar]
- 194.Renganathan M, Delbono O. Caloric restriction prevents age-related decline in skeletal muscle dihydropyridine receptor and ryanodine receptor expression. FEBS Lett. 1998;434:346–350. doi: 10.1016/S0014-5793(98)01009-6. [DOI] [PubMed] [Google Scholar]
- 195.Wieslander A, et al. Biological significance of reducing glucose degradation products in peritoneal dialysis fluids. Perit Dial Int. 2000;20:S23–S27. [PubMed] [Google Scholar]
- 196.Delbono O, Renganathan M, Messi ML. Excitation–Ca2+ release–contraction coupling in single aged human skeletal muscle fiber. Muscle Nerve Suppl. 1997;5:S88–S92. doi: 10.1002/(SICI)1097-4598(1997)5+<88::AID-MUS21>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 197.Margreth A, Damiani E, Bortoloso E. Sarcoplasmic reticulum in aged skeletal muscle. Acta Physiol Scand. 1999;167:331–338. doi: 10.1046/j.1365-201x.1999.00624.x. [DOI] [PubMed] [Google Scholar]
- 198.Narayanan N, et al. Effects of aging on sarcoplasmic reticulum function and contraction duration in skeletal muscles of the rat. Am J Physiol. 1996;271:C1032–C1040. doi: 10.1152/ajpcell.1996.271.4.C1032. [DOI] [PubMed] [Google Scholar]
- 199.Wang ZM, Messi ML, Delbono O. L-type Ca(2+) channel charge movement and intracellular Ca(2+) in skeletal muscle fibers from aging mice. Biophys J. 2000;78:1947–1954. doi: 10.1016/S0006-3495(00)76742-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Delbono O. Molecular mechanisms and therapeutics of the deficit in specific force in ageing skeletal muscle. Biogerontology. 2002;3:265–270. doi: 10.1023/A:1020189627325. [DOI] [PubMed] [Google Scholar]
- 201.Moreno RJ, et al. Role of sustained overexpression of central nervous system IGF-I in the age-dependent decline of mouse excitation–contraction coupling. J Membr Biol. 2006;212:147–161. doi: 10.1007/s00232-006-0044-z. [DOI] [PubMed] [Google Scholar]
- 202.Neuhuber B, et al. Association of calcium channel alpha1S and beta1a subunits is required for the targeting of beta1a but not of alpha1S into skeletal muscle triads. Proc Natl Acad Sci USA. 1998;95:5015–5020. doi: 10.1073/pnas.95.9.5015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Strube C, et al. Reduced Ca2+ current, charge movement, and absence of Ca2+ transients in skeletal muscle deficient in dihydropyridine receptor beta 1 subunit. Biophys J. 1996;71:2531–2543. doi: 10.1016/S0006-3495(96)79446-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Gregg RG, et al. Absence of the beta subunit (cchb1) of the skeletal muscle dihydropyridine receptor alters expression of the alpha 1 subunit and eliminates excitation–contraction coupling. Proc Natl Acad Sci USA. 1996;93:13961–13966. doi: 10.1073/pnas.93.24.13961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Cheng W, et al. Interaction between the dihydropyridine receptor Ca2+ channel beta-subunit and ryanodine receptor type 1 strengthens excitation–contraction coupling. Proc Natl Acad Sci USA. 2005;102:19225–19230. doi: 10.1073/pnas.0504334102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Schredelseker J, et al. The beta 1a subunit is essential for the assembly of dihydropyridine-receptor arrays in skeletal muscle. Proc Natl Acad Sci USA. 2005;102:17219–17224. doi: 10.1073/pnas.0508710102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Taylor JR, et al. Increased Ca(V)beta(1a) expression with aging contributes skeletal muscle weakness. Aging Cell. 2009;8:584–594. doi: 10.1111/j.1474-9726.2009.00507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Payne AM, et al. Role of Ca2+, membrane excitability, and Ca2+ stores in failing muscle contraction with aging. Exp Gerontol. 2009;44:261–273. doi: 10.1016/j.exger.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Andersson DC, et al. Ryanodine receptor oxidation causes intracellular calcium leak and muscle weakness in aging. Cell Metab. 2011;14:196–207. doi: 10.1016/j.cmet.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Bellinger AM, et al. Remodeling of ryanodine receptor complex causes “leaky” channels: a molecular mechanism for decreased exercise capacity. Proc Natl Acad Sci USA. 2008;105:2198–2202. doi: 10.1073/pnas.0711074105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ward CW, et al. Defects in ryanodine receptor calcium release in skeletal muscle from post-myocardial infarct rats. FASEB J. 2003;17:1517–1519. doi: 10.1096/fj.02-1083fje. [DOI] [PubMed] [Google Scholar]
- 212.Ferrington DA, Krainev AG, Bigelow DJ. Altered turnover of calcium regulatory proteins of the sarcoplasmic reticulum in aged skeletal muscle. J Biol Chem. 1998;273:5885–5891. doi: 10.1074/jbc.273.10.5885. [DOI] [PubMed] [Google Scholar]
- 213.Papageorgopoulos C, et al. Measuring synthesis rates of muscle creatine kinase and myosin with stable isotopes and mass spectrometry. Anal Biochem. 2002;309:1–10. doi: 10.1016/S0003-2697(02)00253-1. [DOI] [PubMed] [Google Scholar]
- 214.Brandt NR, et al. The role of mitsugumin 29 in transverse tubules of rabbit skeletal muscle. Arch Biochem Biophys. 2001;385:406–409. doi: 10.1006/abbi.2000.2148. [DOI] [PubMed] [Google Scholar]
- 215.Corona BT, et al. Junctophilin damage contributes to early strength deficits and EC coupling failure after eccentric contractions. Am J Physiol Cell Physiol. 2010;298:C365–C376. doi: 10.1152/ajpcell.00365.2009. [DOI] [PubMed] [Google Scholar]
- 216.Ito K, et al. Deficiency of triad junction and contraction in mutant skeletal muscle lacking junctophilin type 1. J Cell Biol. 2001;154:1059–1067. doi: 10.1083/jcb.200105040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Nishi M, et al. Abnormal features in skeletal muscle from mice lacking mitsugumin29. J Cell Biol. 1999;147:1473–1480. doi: 10.1083/jcb.147.7.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Woo JS, et al. S165F mutation of junctophilin 2 affects Ca2+ signalling in skeletal muscle. Biochem J. 2010;427:125–134. doi: 10.1042/BJ20091225. [DOI] [PubMed] [Google Scholar]
- 219.Kurebayashi N, et al. Changes in Ca2+ handling in adult MG29-deficient skeletal muscle. Biochem Biophys Res Commun. 2003;310:1266–1272. doi: 10.1016/j.bbrc.2003.09.146. [DOI] [PubMed] [Google Scholar]
- 220.Weisleder N, et al. Muscle aging is associated with compromised Ca2+ spark signaling and segregated intracellular Ca2+ release. J Cell Biol. 2006;174:639–645. doi: 10.1083/jcb.200604166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Thornton AM, et al. Store-operated Ca2+ entry (SOCE) contributes to normal skeletal muscle contractility in young but not in aged skeletal muscle. Aging (Albany NY) 2011;3:621–634. doi: 10.18632/aging.100335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Musaro A, Dobrowolny G, Rosenthal N. The neuroprotective effects of a locally acting IGF-1 isoform. Exp Gerontol. 2007;42:76–80. doi: 10.1016/j.exger.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 223.Payne AM, et al. Motor neurone targeting of IGF-1 prevents specific force decline in ageing mouse muscle. J Physiol. 2006;570:283–294. doi: 10.1113/jphysiol.2005.100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Payne AM, et al. Motor neuron targeting of IGF-1 attenuates age-related external Ca2+-dependent skeletal muscle contraction in senescent mice. Exp Gerontol. 2007;42:309–319. doi: 10.1016/j.exger.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Delbono O. Neural control of aging skeletal muscle. Aging Cell. 2003;2:21–29. doi: 10.1046/j.1474-9728.2003.00011.x. [DOI] [PubMed] [Google Scholar]
- 226.Boesze-Battaglia K, Schimmel R. Cell membrane lipid composition and distribution: implications for cell function and lessons learned from photoreceptors and platelets. J Exp Biol. 1997;200:2927–2936. doi: 10.1242/jeb.200.23.2927. [DOI] [PubMed] [Google Scholar]
- 227.Blazyk J, Wu CJ, Wu SC. Correlation between lipid fluidity and tryptic susceptibility of Ca2+-ATPase in sarcoplasmic reticulum membranes. J Biol Chem. 1985;260:4845–4849. [PubMed] [Google Scholar]
- 228.Spector AA, Yorek MA. Membrane lipid composition and cellular function. J Lipid Res. 1985;26:1015–1035. [PubMed] [Google Scholar]
- 229.Grinna LS. Age-related alterations in membrane lipid and protein interactions: Arrhenius studies of microsomal glucose-6-phosphatase. Gerontology. 1977;23:342–349. doi: 10.1159/000212206. [DOI] [PubMed] [Google Scholar]
- 230.Ferrington DA, et al. Decreased conformational stability of the sarcoplasmic reticulum Ca-ATPase in aged skeletal muscle. Biochim Biophys Acta. 1997;1330:233–247. doi: 10.1016/S0005-2736(97)00158-2. [DOI] [PubMed] [Google Scholar]
- 231.Krainev AG, et al. Adaptive changes in lipid composition of skeletal sarcoplasmic reticulum membranes associated with aging. Biochim Biophys Acta. 1995;1235:406–418. doi: 10.1016/0005-2736(95)80030-J. [DOI] [PubMed] [Google Scholar]
- 232.von Haehling S, et al. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachex Sarcopenia Muscle. 2010;1:7–8. doi: 10.1007/s13539-010-0003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Clark BC, Taylor JL. Age-related changes in motor cortical properties and voluntary activation of skeletal muscle. Curr Aging Sci. 2011;4:193–200. doi: 10.2174/1874609811104030192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Kido A, Tanaka N, Stein RB. Spinal excitation and inhibition decrease as humans age. Can J Physiol Pharmacol. 2004;82:238–248. doi: 10.1139/y04-017. [DOI] [PubMed] [Google Scholar]