Abstract
Substance use disorders are associated with psychopathy, a personality disorder that is heterogeneous in both adults and youth; secondary variants of psychopathy with comorbid psychopathology and primary variants without comorbidity show distinct correlates and outcomes. In adult criminal populations, secondary variants report greater substance abuse compared with primary variants. The primary aim of this study is to replicate and extend these findings to a juvenile offender population. Compared with primary variants of juvenile psychopathy, secondary variants (a) reported significantly more frequent substance—particularly alcohol—use within the six months prior to incarceration (d = .43), (b) were almost twice as likely to abuse substances while incarcerated, and (c) were more likely to be diagnosed with a current DSM-IV substance use disorder. Practical implications for working with justice-involved youth are discussed.
Keywords: psychopathy, juvenile psychopathy, substance abuse and dependence, alcohol, juvenile offenders
Psychopathy is a personality disorder characterized by such traits as superficial charm, pathologic egocentricity, untruthfulness and insincerity, and a lack of remorse or shame (Cleckley, 1941). Although not formally recognized by the DSM-IV, psychopathy is a personality disorder typically studied among adult criminal offenders. However, research paradigms have begun to identify developmental precursors in childhood and adolescence (see Frick, 1995; 2006; Lynam, 1996). Similar to adults, psychopathic traits in youth identify those at risk for antisocial and violent behavior, who show deficits in emotional and fearful responding (see Frick & Marsee, 2006). Traditional theoretical perspectives on psychopathy view these individuals as a largely homogeneous group, as evidenced by many of the diagnostic measures used to classify them (Andershed, Kerr, Stattin, & Levander, 2002; Hare, 2003; Forth, Kosson, & Hare, 2003; Lynam, 1997). However, the traditional conceptualization of psychopathy as a unitary construct has been challenged, highlighting evidence of measurable heterogeneity among individuals classified as ‘psychopaths’ (see Skeem, et al., 2003).
Connecting Psychopathy Variants to Psychopathology and Trauma Exposure
There is growing empirical support for heterogeneity among both adolescents and adults scoring high on measures of psychopathy. Such research paradigms are rooted in theory that posits phenomenological distinctions between variants of psychopathy.1 The prevailing conceptualization is that of Karpman (1948; 1955), who discriminates between psychopathy subtypes based on their experiences of underlying neurotic conflict. Specifically, Karpman (1955) posits that the primary psychopathy variant is characterized by a general lack of emotion and anxiety, while the secondary variant is emotionally reactive, principally as a result of high anxiety levels. Schmitt and Newman (1999) examined the association between Psychopathy Checklist (PCL-R; Hare, 1991) scores—the most widely used measure of psychopathy—and features of anxiety (including neuroticism and fear) in adult offenders and found weak and mostly non-significant correlations between psychopathy and anxiety constructs (see also Hare 2003). The authors interpreted these findings as evidence that the psychopathy construct and anxiety are essentially independent, which counters the “traditional belief that all psychopathic individuals are low-anxious” (p. 353) and offers support for Karpman’s (1955) theory. Indeed, the acceptance of this perspective is evidenced by several empirical studies that attempt to delineate psychopathy variants utilizing symptoms of anxiety as the main distinguishing factor (Falkenbach, Poythress, & Creevy, 2008; Kosson & Newman, 1995; Lee, Salekin, & Iselin, 2010; Skeem, Johansson, Andershed, Kerr, & Louden, 2007; Tatar, Cauffman, Kimonis, & Skeem, in press).
Although several theoretical perspectives agree that anxiety is a key distinction between psychopathy variants, others highlight alternative distinguishing characteristics such as dissociative experiences (Porter, 1996), behavioral inhibition/activation (Lykken, 1995), and social withdrawal (Blackburn, 1975). These perspectives also posit etiological distinctions that center on the relative contributions of nature versus nurture—theoretically, primary psychopathy is primarily inborn, whereas the secondary variant develops through environmental insult, particularly competitive disadvantage (Mealey, 1995), childhood abuse and neglect (Karpman, 1955), and traumatic experiences (Porter, 1996). Karpman (1948) theorized that exposure toearly abusive experiences resulted in hostility in the child that disturbed the functioning of an otherwise intact conscience. The few studies that compare trauma and maltreatment histories among psychopathy variants are generally consistent with this perspective (adult populations, for a review see Skeem, Poythress, Edens, Lilienfeld, & Cale, 2003; juvenile offenders, Tatar, et al., in press; Vaughn, et al., 2009). The idea that trauma and abuse provide the necessary conditions for the development of secondary psychopathy is especially relevant to incarcerated adult and juvenile populations who show high rates of such childhood adversity (Cauffman, Feldman, Waterman & Steiner, 1998; Smith & Thornberry, 1995; Weeks & Widom, 1998). Indeed, several studies link reports of childhood abuse and neglect to higher scores on measures of psychopathy (Campbell, Porter, & Santor, 2004; Forth & Burke, 1998; Krischer, & Sevecke, 2008; Lang, af Klinteberg, & Alm, 2002; Marshall & Cooke, 1995; Weiler & Widom, 1996), with stronger associations noted for general antisocial deviance features of psychopathy (factor 2; i.e., irresponsibility, childhood and adult criminal behavior) rather than emotional detachment (factor 1; i.e., callousness, lack of empathy/guilt, grandiosity and manipulativeness) per se (Poythress, Skeem, & Lilienfeld, 2006, Krischer, & Sevecke, 2008; O’Neill, Lidz, & Heilbrun, 2003).
Some cluster-analytic research finds that high-anxious secondary variants also experience greater comorbid psychopathology—particularly depression (Haapasalo and Pulkkinen 1992; Alterman, McDermott et al. 1998; incarcerated youth, Kimonis, Skeem et al. in press), post-traumatic stress symptomatology (incarcerated youth, Tatar, Cauffman et al. in press), anger/hostility (Hicks, Markon, Patrick, Krueger, & Newman, 2004; incarcerated youth, Kimonis, Skeem, Cauffman, & Dmitrieva, in press), and symptoms of attention-deficit hyperactivity disorder (Hundt, Kimbrel, Mitchell, & Nelson-Gray, 2008; incarcerated youth, Vaughn, Edens, Howard, & Smith, 2009), compared with their low-anxious counterparts—but not dissociative experiences (Poythress, Skeem, & Lilienfeld, 2006; Tatar, et al., in press). This research offers promising evidence for the existence of multiple variants of psychopathy that can be distinguished according to the presence of various forms of comorbid psychopathology.
Psychopathy Variants and Substance Abuse
In The Mask of Sanity, Cleckley (1976) wrote that “although some psychopaths do not drink at all and others drink rarely, considerable overindulgence in alcohol is very often prominent in the life story” (p. 355). Substance use disorders are moderately associated with psychopathy in adolescents and adults, with some researchers reporting stronger associations for the antisocial deviance dimension of the two-factor model of psychopathy (for a review, see Taylor & Lang, 2006), and others reporting similar associations across dimensions of the three-factor model (e.g., YPI, Hillege, Das, & de Ruiter, 2010). There is growing support for greater substance abuse pathology in adult secondary variants of psychopathy (Vassileva, Kosson et al. 2005; Skeem, Johansson et al. 2007; Swogger and Kosson 2007). For example, Vassileva and colleagues (2005) found that the high-anxious psychopathic (secondary) cluster—identified through cluster analysis of scores on psychopathy, anxiety, and DSM-IV diagnoses of alcohol and substance abuse disorders—presented with more severe alcohol and substance abuse pathology than all remaining clusters, including the primary psychopathy cluster. These findings were replicated in a more recent study using a similar analytic strategy (Swogger & Kosson, 2007). Of course, some may argue that such findings are less than compelling, considering the use of substance pathology to help discriminate subtypes, as cluster analytic strategies are designed to obtain significant group differences on as many characteristics as possible. However, another study used only psychopathy and trait anxiety scores to cluster psychopathic offenders, and also found significantly more alcohol and drug pathology amongst adultsecondary variants than primary variants or comparison offenders (Skeem, Johansson, Andershed, Kerr, & Eno Louden, 2007).
We are aware of only two studies to date that examine differences in substance abuse pathology among juvenile variants of psychopathy (Vaughn, et al., 2009; Wareham, Dembo, Poythress, Childs, & Schmeidler, 2009). Using a sample of incarcerated juvenile offenders, Vaughn and colleagues (2009) distinguished psychopathy variants using various psychiatric characteristics (i.e. anxiety, depression, PTSD, ADHD) within a finite mixture modeling approach, which produced two distinct classes. Using a retrospective self-report measure, they found that secondary variants reported greater co-occurring substance use in the previous year, and also scored higher on measures of psychopathology, compared with primary variants and non-psychopathic classes. Another study by Wareham, Dembo, Poythress, Childs, and Schmeidler (2009) used latent class analysis to identify psychopathy variants within a sample of incarcerated boys and girls. While their cluster analysis produced a theoretically coherent primary variant of psychopathy, they had greater difficulty in establishing a comparable secondary group. Nevertheless, they found that the high-anxious, moderately psychopathic group reported the greatest frequency of substance abuse prior to incarceration and more drug use at a one-year follow-up. However, neither study included a clear indicator of the relative severity of the participants’ substance abuse problems (i.e. clinical diagnosis). In other words, it is difficult to determine from either study whether the participants’ substance use represented clinically significant pathology. The present study fills this important gap in the literature by conducting an in-depth assessment of pre-incarceration and facility-based substance use in a sample of juvenile offenders that includes a diagnostic clinical interview. We also used multiple reports of substance abuse activity (retrospective report, prospective report, and DSM-IV diagnosis) to allow for a more comprehensive picture of the possible association between substance-related problems and secondary psychopathy.
The Present Study
Preliminary research suggests that co-occurring problems may be more prevalent in secondary variants of psychopathy in incarceration settings; however, there has been relatively little study of substance-related disorders in juvenile psychopathy variants. The present study moves the field forward by improving the identification of youthful offenders at greatest risk for substance-related problems and informing our understanding of the correlates and functions of substance use for subgroups of incarcerated youth that can be targeted within intervention. Specifically, we address whether secondary variants of juvenile psychopathy report greater alcohol and drug abuse prior to (Aim 1) and during incarceration (Aim 2), compared with primary variants and nonpsychopathic comparison youth. In addition, our third aim is to examine whether secondary variants are more likely to meet diagnostic criteria for a DSM-IV substance abuse or dependence disorder—both past and present—than primary and comparison youth. Consistent with prior research, it is hypothesized that secondary variants will report greater substance use and show a higher likelihood of substance abuse pathology both inside and outside of the incarceration context, than primary or comparison youth. An important strength of this study is its use of a cluster-analytic strategy to delineate juvenile psychopathy variants. This analytic technique establishes more confidence in defined groups than simpler a priori strategies, such as median splits (see Whiteman & Loken, 2006). Model-based cluster (MBC) analysis also is conducted without inclusion of substance abuse pathology, allowing for a more independent examination of the connection between psychopathy variants and alcohol and drug use.
Method
Participants
Participants include 373 male juvenile offenders between the ages of 14 and 17 years (M = 16.42, SD = .79; see Table 1) housed in a secure confinement facility in Southern California. The majority (94%; n = 350) of youth were from ethnic minority backgrounds (53% Hispanic, 29% African American, and 12% other [bi- or multi-racial]), whereas only 6% of the sample was Caucasian. The ethnic composition of this sample is representative of youth incarcerated in this region of the US (Snyder & Sickmund, 2006). The majority of juveniles were sentenced for violent (e.g., murder, rape, robbery, aggravated assault) committing offenses (69%, n = 258).
Table 1.
Descriptive Statistics and Zero-order Correlations among Main Study Variables
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Psychopathy | -- | .26** | .08 | .10 | .11* | .13* | .21** | .26** | .22** | .42** | .21** | .17** |
| 2. Anxiety | -- | -- | .27** | .52** | .42** | .54** | .36** | .51** | .44** | .34** | .09 | .01 |
| 3. Maltreatment History | -- | -- | -- | .10* | .12* | .13** | .16** | .16** | .14** | .18** | .17** | .06 |
| 4. CES-D Total | -- | -- | -- | -- | .61** | .73** | .43** | .49** | .46** | .36** | .09 | .08 |
| 5.Withdrawn/Depressed | -- | -- | -- | -- | -- | .65** | .46** | .44** | .55** | .32** | .04 | −.01 |
| 6. Anxious/Depressed | -- | -- | -- | -- | -- | -- | .55** | .63** | .58** | .35** | .09 | .05 |
| 7. Thought Problems | -- | -- | -- | -- | -- | -- | -- | .54** | .41** | .39** | .15** | .06 |
| 8. Attention Problems | -- | -- | -- | -- | -- | -- | -- | -- | .62** | .49** | .18** | .11* |
| 9. Social Problems | -- | -- | -- | -- | -- | -- | -- | -- | -- | .35** | .11* | −.01 |
| 10. Anger | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .27** | .22** |
| 11. Pre-Incarceration Substance Use |
-- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .16** |
| 12. Institutional Substance Use | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Descriptives | ||||||||||||
| Mean | 118.14 | 6.85 | 1.52 | 17.18 | 4.70 | 6.04 | 2.47 | 5.35 | 3.21 | 89.25 | 5.34 | .80 |
| SD | (20.26) | (5.18) | (1.56) | (8.83) | (2.40) | (4.45) | (2.23) | (3.22) | (2.01) | (16.59) | (1.94) | (1.52) |
| Range | 59-174 | 0-27 | 0-7 | 0-48 | 0-11 | 0-23 | 0-13 | 0-16 | 0-10 | 51-140 | 0-7 | 0-11.25 |
| Skewness | −.15 | 1.02 | 1.00 | .63 | .25 | .92 | 1.24 | .46 | .62 | −.05 | −1.69 | 2.73 |
| Skewness SE | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) | (.13) |
| Kurtosis | .04 | .92 | .42 | .05 | −.39 | .69 | 2.08 | −.31 | .10 | −.60 | 1.76 | 9.44 |
| Kurtosis SE | (.26) | (.26) | (.25) | (.25) | (.25) | (.25) | (.25) | (.25) | (.25) | (.25) | (.25) | (.25) |
| Alpha | .90 | .85 | .64 | .82 | .61 | .81 | .66 | .73 | .53 | .90 | .65 | .59 |
| Mean inter- item correlations |
.16 | .10 | .22 | .15 | .19 | .20 | .23 | .20 | .13 | .22 | .22 | .12 |
Note. p < .05
p < .01
p < .001. CES-D = Center for Epidemiological Studies Depression Scale. Substance abuse variables reported in this table are for frequency of use. SE = Standard error.
Study Design
All study procedures were approved by the University Institutional Review Board and the Department of Corrections and Rehabilitation. In addition, a Certificate of Confidentiality was secured by the Department of Health and Human Services to ensure that the information disclosed by the youths remained confidential. All youth between the ages of 14 and 17 years who were newly admitted to the facility, or returning on a new offense, were eligible to enroll in the study. Ninety seven percent of parents/guardians contacted consented to their child’s participation in the study; the youth assent rate was 96%. Within 48 hours of arrival to the facility, youth completed a two-hour baseline interview, consisting of a diagnostic assessment and a battery of developmental, behavioral, emotional, and attitudinal measures. Youth also completed weekly and monthly follow-up interviews (i.e., weeks 2, 3, 4, and month 2) consisting of the same measures completed at baseline, as well as several supplemental questionnaires, as the broader study assessed adjustment to incarceration.
Measures
Demographic information
Participants self-reported their age, ethnicity, and whether they had been to the facility before.
Measures described below are categorized into clustering measures used in MBC to identify clusters, measures used to support the external validity of the resultant clusters based on theoretical conceptualizations of psychopathy variants, and outcome measures used to test the study aims.
Clustering Measures
Psychopathy
The Youth Psychopathic Traits Inventory (YPI; Andershed, Kerr, Stattin, & Levander, 2002) is a 50-item self-report measure of psychopathic traits that was administered at the week 3 assessment. The YPI was developed in a community-based sample of youth with an aim to capture core affective and interpersonal personality features of psychopathy to the exclusion of the “more behavioral consequences of psychopathic personality traits” (Andershed, Kerr et al., 2002, p. 135), or antisocial deviance and criminal behavior that some believe develop downstream from such traits (Skeem and Cooke 2010; Skeem and Cooke 2010) (cf. Hare and Neumann 2010). The items of the YPI were written to assess ten target traits/scales in a relatively comprehensive (5 items per trait) and indirect, nontransparent manner (e.g., “I usually feel calm when other people are scared”). Prior factor analytic research supports a three-factor structure in which each higher-order factor is composed of several lower-order scales (in parentheses): Grandiose-Manipulative (i.e., interpersonal traits: dishonest charm, grandiosity, lying, manipulation), Callous-Unemotional (affective traits: remorselessness, callousness, unemotionality), and Impulsive-Irresponsible (lifestyle traits: impulsiveness, irresponsibility, thrill seeking) (Andershed, Kerr et al. 2002; Poythress, Dembo et al. 2006; Declercq, Markey et al. 2009). The YPI correlates modestly with the Psychopathy Checklist: Youth Version (PCL:YV, r=.35, Forth, Kosson et al. 2003), with low to modest correlations with a variety of self-report conduct problem indices, supporting its convergent validity (Cauffman, Kimonis, Dmitrieva, & Monahan, 2009). In the current sample, the YPI total and factor scores demonstrated adequate internal consistency (total score α = .90; factor scores ranging from .71 [CU] to .89 [GM]).
Anxiety
The Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1985; 2000) is a standardized measure designed to assess anxiety in youth between the ages of 6 and 19. The RCMAS has 37 items divided into four scales: Physiological Anxiety (10 items; e.g., “Often I feel sick in my stomach,” α = .64), Worry/Oversensitivity (11 items; e.g., “I worry about what is going to happen,” α = .76), Social Concerns/Concentration (7 items; “A lot of people are against me,” α = .68), and a Lie Scale (9 items; e.g., “I never get angry,” not included in analyses). The child responds to each question with a “Yes” or “No” answer. The RCMAS is internally consistent (α =.85, Reynolds and Richmond 1985) and possesses moderate test–retest reliability over a 9-month period (r= .63, Reynolds 1981). It is significantly more strongly associated with other measures of anxiety (e.g., the State–Trait Anxiety Inventory for Children, r = .88) than it is with measures of depression (e.g., Child Depression Inventory), providing some support for its construct validity (e.g., Muris, Merckelbach, Ollendick, King, & Bogie, 2002).
External Validation Measures
Maltreatment History
The Life Events Scale (Gil-Rivas, 2003) consists of a list of 32 stressful life events. The youth is asked to endorse which of these events he has ever experienced in his lifetime. Maltreatment history was computed by totaling the seven items tapping parental absence, domestic violence exposure, parental neglect, and physical, emotional, and sexual abuse (two items) (α = .64).
Depression
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) is a 20-item self-report measure of depressed mood, lack of positive affect, somatic symptoms, and interpersonal difficulties. While high scores on the measure do not officially warrant a diagnosis, studies have shown that scores of 16 and over are considered as a caution for follow-up on diagnostic interview for possible diagnosis of depression (Radloff, 1977). Each item (e.g., In the past week, I could not shake the blues even with help) on the scale is rated on a 4-point Likert-type scale, specifying the frequency with which the symptom was experienced by the youth (0 = rarely; 1 = some or a little of the time; 2 = occasionally, and 3 = most or all of the time). A total score was computed by summing all 20 items rated at baseline, with higher scores indicative of more depressive symptomatology (α = .82). Previous research has shown that the CES-D is moderately stable over several weeks (r = 0.57, Radloff 1977).
Psychiatric Symptomatology
The 112-item Child Behavior Checklist Youth Self Report (CBCL-YSR; Achenbach, 1991) was used to assess psychiatric symptoms. The withdrawn/depressed (7 items, e.g., I cry a lot), anxious/depressed (16 items), thought problems (7 items, e.g., I have thoughts that other people would think are strange), attention problems (9 items, e.g., I have trouble concentrating or paying attention), and social problems (8 items, e.g., I don’t get along with other kids) subscales rated at baseline were used. The internal consistencies of CBCL scales are reported in Table 1.
Anger
The Novaco Anger Scale (NAS; Novaco, 2003) is a 48-item self-report measure of various dimensions of anger. The NAS utilizes a 3-point response scale (1 = never true; 2 = sometimes true; 3 = always true) such that higher scores reflect greater anger. The total score rated at baseline (α = .90) was used in the current study with higher scores indicative of greater anger. The NAS is highly correlated with several other measures of anger, such as the Buss-Durkee Hostility Total score (r = .82), Caprara Scales of Irritability (r = .78) and Rumination (r = .69), Cook-Medley Hostility (r = .68), and the STAXI Trait Anger Scale (r = .84) (Novaco 2003).
Outcome Measures
Substance Abuse
Youth were asked to self-report their personal histories of pre-incarceration (history of substance use) and institutional (within-facility) substance use using an adapted version of a scale developed by Stice, Barrera, and Chassin (1993). At the baseline interview, youth reported on their frequencies (0=never, 1=once every few months, 2=once a month, 3=once every two weeks, 4=once a week, 5=more than once a week, 6=daily, 7=twice a day) of alcohol, marijuana, inhalants, or other drug use (i.e., stimulants, hallucinogens, prescription medications), separately, within the six months prior to facility entry (pre-incarceration). Higher scores on this scale were indicative of more substance use within the six month period prior to incarceration.
Prevalence of institutional substance use was recorded as a dichotomous endorsement (1=Yes, 0=No) and affirmative responses were collapsed across each of the four substance types (alcohol, marijuana, inhalants, or other drug) and each follow-up assessment (weeks 2, 3, 4, month 2) to compute the prevalence of any substance use during the entire period of incarceration (1=Yes, 0=No). Youth were also asked to report on the frequency of use of each of the four substance types within the institution using an open-ended response (e.g., used alcohol five times in the past week). To provide a measure of the average frequency of any type of substance use during the entire period of incarceration, frequency responses for each of the four substance types (alcohol, marijuana, inhalants, or other drug) and follow-up assessments (weeks 2, 3, 4, month 2) were averaged.
Though there appears to be some level of disagreement within the literature, several research studies have supported the validity and temporal consistency of adolescent self-reports of substance use as a measure of actual behavior (i.e., Needle, McCubbin et al. 1983; Oetting and Beauvais 1990; Winters, Stinchfield et al. 1991). In fact, research utilizing drug testing procedures as corroborating evidence for youth’s self-reported substance abuse have often observed moderate levels of agreement between these measures (e.g., κ=.48-.60, self-report and urinalysis for marijuana, Harrison, Martin et al. 2007). Although there may be concerns regarding the validity of self-reports of substance use amongst incarcerated populations, considering the possible consequences of discovery, research has also supported the relative accuracy of these reports, particularly when compared to individuals in other high-risk settings (Hser, Maglione et al. 1999).
In addition, the presence or absence of alcohol and other substance related diagnoses were measured using the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime version (K-SADS-PL; Kauffman, Birmaher, Brent, Rao, Flynn, et al., 1997). The K-SADS-PL is a semi-structured diagnostic interview designed to assess current and past episodes of psychopathology in children and adolescents according to DSM-IV criteria. Prior to administering the diagnostic interview for data collection, interviewers completed an extensive training that involved rating tape-recorded K-SADS-PL interviews conducted by an experienced clinician. There was excellent interrater agreement (κ = .80, p < .001). The substance abuse supplement of the K-SADS-PL assesses DSM-IV diagnostic criteria for alcohol and other substance (marijuana, cocaine, heroin, opiates, polysubstance, etc.) abuse and dependence disorders, both at any point in the past and for current presentation. For the purposes of the present study, the presence of alcohol and substance abuse pathology was recorded dichotomously to indicate whether (1=Yes) or not (0=No) the participant met DSM-IV diagnostic criteria.
Control Variable
Time incarcerated
Because longer exposure to the incarceration setting permits greater opportunity for institutional offending, we controlled for time spent in the facility. Thus, in analyses of institutional substance abuse, time incarcerated was used as a control variable. It was calculated as the proportion of time that a youth remained in the study. There was no significant difference between primary/secondary variants and nonpsychopathic comparison youth on time spent incarcerated.
Results
Descriptive statistics were performed on the clustering variables to determine their distributions. YPI (psychopathy) factor scores were normally distributed, although anxiety subscales were positively skewed, with most youth scoring at the lower end of the distribution. YPI factor scores were modestly positively correlated with anxiety scores (average r = .20, p < .01); associations between psychopathy and anxiety total scores were not significantly different between African American (r = .27, p < .01) and Hispanic offenders (r = .27, p < .001)2. As shown in Table 1, pre-incarceration and institutional substance use were positively associated with psychopathy scores, but were uncorrelated with anxiety.
Consistent with prior empirical studies of psychopathy variants (Hicks, Markon et al. 2004; Skeem, Johansson et al. 2007; Hicks, Vaidyanathan et al. 2010; Kimonis, Skeem et al. in press; Tatar, Cauffman et al. in press), we first used model-based cluster analysis (MBC; Banfield and Raftery 1993) to determine whether primary and secondary variants of juvenile psychopathy can be identified in a subsample of male juvenile offenders scoring high on a measure of psychopathy. To validate the resultant clusters we used multivariate analyses of variance (MANOVA) and analyses of variance (ANOVA) to compare them on theoretically relevant factors not used to derive them, namely maltreatment history and psychiatric symptomatology, predicting that secondary variants will show greater levels of each than primary variants. To address the primary aim—whether secondary variants of juvenile psychopathy report greater pre-incarceration substance abuse compared with primary variants and nonpsychopathic comparison youth—we used ANOVA and MANOVA. To address the second aim—to test for differences in institutional substance use—we used chi-square and logistic regression analyses (for dichotomous prevalence outcomes), and ANCOVA/ MANCOVA (for continuous frequency outcomes). Finally, to address the third study aim— differences in alcohol and substance abuse/dependence pathology—we used logistic regression analyses.
Cluster Derivation
Although we recognize that the most compelling data suggest that psychopathy is a dimensional trait rather than a taxon (Lilienfeld 1994; Lilienfeld 1998; Edens, Marcus et al. 2006; Marcus, Lilienfeld et al. 2006) (cf. Harris, Rice et al. 1994), we used a threshold score to select youth because our interest was in identifying those with substantial psychopathic traits. Thus, to derive clusters of primary and secondary variants of psychopathy, those scoring greater than 121.5 on the YPI (n= 165) were selected for analyses. While the YPI does not have an established cut score for classifying youth as psychopathic, a score of 121.5 was found to correspond to a PCL:YV score of 30 (the traditional cut-off) in a large sample (N = 1,171) of adolescent male offenders (Cauffman, Kimonis et al. 2009). We focused on youth with high scores on the YPI (rather than all youthful offenders) to permit comparison of the results with prior studies of adult (Hicks, et al., 2004; Skeem, et al., 2007) and juvenile variants of psychopathy (Kimonis, Skeem et al. in press). The remaining youth (n = 208) with YPI total scores of 121.5 and below were used as a comparison group. Relative to the nonpsychopathic comparison subsample (n = 208), the group scoring high on the YPI (i.e., clustering subsample, n = 165) obtained significantly higher scores on the RCMAS, and was more likely to have a property-related committing offense. However, among the clustering subsample YPI total scores were not significantly associated with anxiety scores (r = .12), although there was a significant positive association for comparison youth (r = .26, p < .001).
MBC was performed using SPLUS 7.0 (Insightful Corporation 1988-2005), the mclust library (Fraley and Raftery 2002; Fraley and Raftery 2002; Fraley and Raftery 2008), and the expectation maximization (EM) algorithm. MBC reduces some of the uncertainties inherent in common clustering methods by testing the relative fit of ten models that vary in their assumptions about the structure of the data. More detailed discussions of MBC are provided by Hicks et al. (2004) and Skeem et al. (2007). Youths’ Z scores (based on the psychopathic subsample) on the three higher-order factors of the YPI and the RCMAS were used as clustering variables. According to BIC values generated by MBC, models that specified one cluster fit relatively poorly, indicating there were subgroups of youth scoring high on psychopathy with distinctive trait patterns. The best-fitting model was a two-cluster solution (cluster 1, n = 122; cluster 2, n = 43) with equal shape, equal volume, and diagonal orientation (BIC = −5236). The average classification certainty, or posterior probability that an individual was correctly assigned to a cluster, was high at 99.9%. Three-quarters of the sample had a fairly high (> 97.5%) probability of correct assignment to a cluster suggesting confidence in this clustering solution.3
Description of Clusters
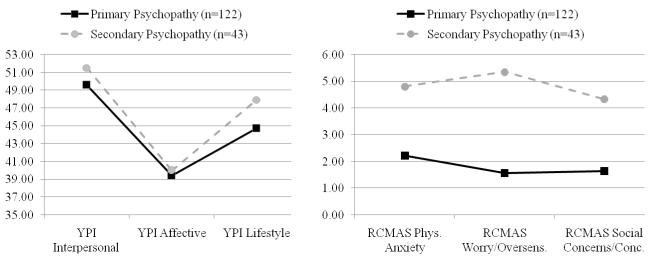
Using t-tests, the two clusters (C1, n = 122; C2, n = 43) were compared on total and factor scores of the YPI and the RCMAS for descriptive purposes (see Figure 1). The second cluster (n = 43), which was labeled ‘secondary,’ reported significantly greater anxiety (physiological, t(163) = −8.59; worry, t(163) = −13.61; and social concerns/concentration, t(163) = −11.92; all p’s < .001), higher total YPI (t(163) = −3.31; p < .001) and Impulsive-Irresponsible lifestyle factor scores (t(163) = −3.70; p < .001), but not Callous-Unemotional or Grandiose-Manipulative scores, compared with the first cluster (n = 122) that was labeled ‘primary.’ The low psychopathy scoring comparison youth were significantly less anxious (M = 6.07, SE = .32) than secondary variants (M = 14.50, SE = .67; F(2,352) = 74.36, p < .001, η2 = .30), whose average score fell in the subclinical range (corresponding to a t-score falling between 60 and 61; Reynolds & Richmond, 2000); however, their anxiety scores did not differ significantly from primary variants (M = 5.43, SE =.39).
Figure 1.
Mean scores for psychopathy variants on clustering variables from the Youth Psychopathic Traits Inventory (YPI) and the Revised Child Manifest Anxiety Scale (RCMAS). Secondary variants scored significantly higher across anxiety factor scores and on the impulsive-irresponsible lifestyle factor of the Youth Psychopathic Traits Inventory, but not interpersonal and affective factors, compared with primary variants.
Validating Clusters: Maltreatment and Psychiatric Symptomatology
The resulting clusters were validated by comparing them on theoretically-relevant dimensions not used to derive them. Since validation variables were significantly correlated (r = .32 to .73) a MANOVA was conducted to compare groups, with ANOVA follow-up tests using the Bonferroni correction (.025 level). Consistent with expectations, secondary variants scored significantly higher on each measure of psychiatric symptomatology compared with primary variants and comparison youth (Λ = 0.81, F (14,728) = 5.86, p < .001, d = .67).
Secondary variants also reported significantly more maltreatment (F(2,371) = 5.64, p < .01, d = .35) compared with primary variants and comparison youth. Altogether, these results suggest that the two clusters are meaningfully related to variables that are theoretically relevant to distinguishing between primary and secondary psychopathy, consistent with their external validity.
First Aim: To Test Whether Secondary Variants Report Greater Pre-Incarceration Substance Use than Primary Variants and Comparison Youth
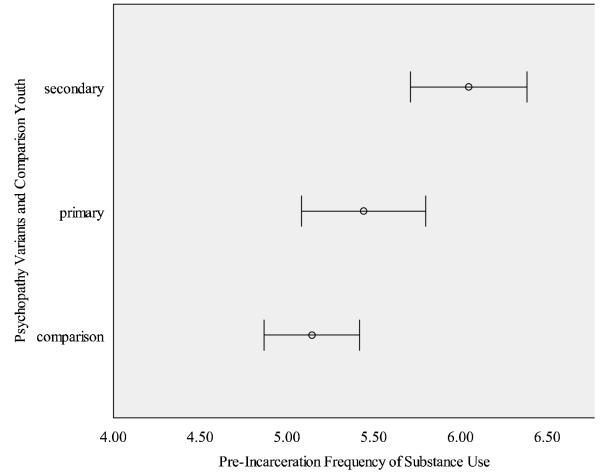
A one way ANOVA revealed a significant difference between groups in their frequency of substance use in the six months prior to incarceration (F(2,369) = 4.07, p < .05, d = .30). Planned contrasts revealed that primary variants differed significantly from secondary variants (t(132) = 2.46, p < .05, d = .43); Secondary variants also differed significantly from comparison youth (t(108) = 4.15, p < .001, d = .80). On average, secondary variants reported the greatest frequency of pre-incarceration substance use (M = 6.05(1.08) [corresponding to a daily frequency], 95% CI [5.71, 6.38]), followed by primary variants (M = 5.44 (2.00), 95% CI [5.08, 5.80]) and comparison youth (M = 5.14 (2.02), 95% CI [4.87, 5.42]), the latter two both reporting a frequency of between once per week and daily use (see Figure 2).
Figure 2.
Frequency of self-reported pre-incarceration alcohol and drug use among primary and secondary psychopathy variants and comparison youth.
To compare groups on the frequency of specific types of substance abuse prior to incarceration, a MANOVA was conducted. Results revealed a significant difference between groups (Λ = 0.95, F(8,690) = 2.33, p < .05, d = .33), with significant differences for alcohol (F(2,348) = 6.31, p < .01, d = .38) and other drug use (F(2,348) = 4.37, p < .05, d = .32), specifically, but not marijuana or inhalant use. Posthoc tests using the Tukey procedure revealed that secondary variants reported significantly more alcohol use (M = 5.08, SE = .35 [more than once per week], 95% CI [4.40, 5.76]) than primary variants (M = 4.03, SE = .21 [once a week], 95% CI [3.62, 4.44]) and comparison youth (M = 3.73 [between once a week and once every two weeks], SE = .16, 95% CI [3.42, 4.04]). Secondary variants also reported significantly more (M = 3.63, SE = .41, 95% CI [2.82, 4.43]) other drug use than comparison youth (M = 2.30, SE = .18, 95% CI [1.93, 2.66]), but not primary variants (M = 2.58, SE = .25 [between once every two weeks and once a month], 95% CI [2.10, 3.06]). There were no significant differences between primary variants and comparison youth.
Second Aim: To Test Whether Secondary Variants Report Greater Institutional Substance Abuse than Primary Variants and Comparison Youth
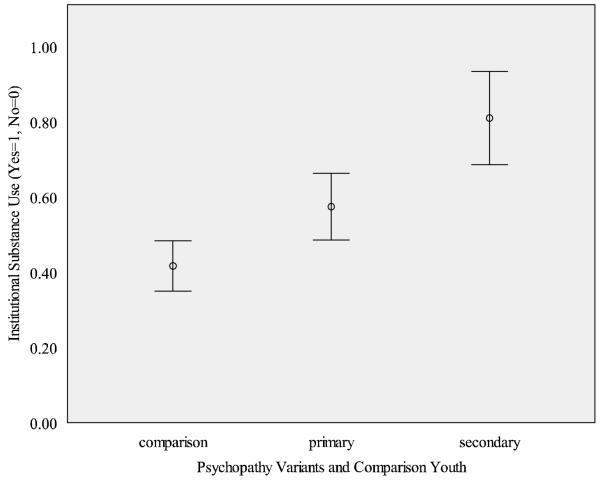
The results of a logistic regression analysis, controlling for time incarcerated in the first step and entering cluster membership as a categorical predictor in the second step, revealed that the odds of using any substances while incarcerated was almost two times greater for the secondary group than the primary group (OR = 1.85, Std. B = .62, p < .01, 95% CI [1.17, 2.94]), and more than five times greater than the comparison group (OR = 5.41, Std. B = 1.69, p < .001, 95% CI [2.36, 12.42]). The percentage of youth in each group reporting substance abuse while incarcerated is depicted in Figure 3 (secondary, 81% vs. primary, 57% vs. comparison, 42%; χ2(2,373) = 24.41, p < .001, η2 = .25).
Figure 3.
Prevalence of institutional alcohol and drug use among primary and secondary psychopathy variants and comparison youth.
Results of a one-way ANCOVA revealed a difference between groups in their average weekly frequency of institutional substance use, after controlling for time incarcerated (F(2,361) = 2.80, p = .06, d = .25). Although not a statistically significant difference, secondary variants reported the greatest average weekly frequency of substance use while incarcerated (M = 1.20 uses per week, SE = .24, 95% CI [.74, 1.67]), followed by primary variants (M = .92, SE = .14, 95% CI [.65, 1.19]) and comparison youth (M = .65, SE = .11, 95% CI [.44, .86]).
To compare variants on their frequency of specific types of institutional substance use, a MANCOVA was conducted controlling for time in the institution, which revealed differences by group (Λ = 0.96, F(8,716) = 1.92, p = .05, d = .29). Groups differed significantly on average weekly frequency of institutional alcohol (F(2,361) = 3.27, p < .05, d = .27) and marijuana use (F(2,361) = 3.05, p < .05, d = .26), but not inhalant or other drug use. Planned contrasts revealed that secondary variants reported significantly more alcohol and marijuana use (M = .16, SD = .39 and M = 1.42, SD = 3.35, respectively) than comparison youth (M = .05, SD = .22 and M = .55, SD = 1.70, respectively), but not primary variants (M = .13, SD = .48 and M = .79, SD = 1.93, respectively). Primary variants also reported significantly more alcohol use than comparison youth, after controlling for time spent incarcerated (all p<.05).
Third Aim: To Test Whether Secondary Variants Are More Likely to Meet DSM-IV Diagnostic Criteria for an Alcohol or Substance Related Disorder (Current and Past)
To examine group differences in both past and present alcohol and substance use pathology assessed from the DSM-IV interview, logistic regression was conducted. Results for past substance use pathology revealed that secondary variants were more likely than the comparison group (OR = 5.56, b = 1.72, p < .01, 95% CI [1.91, 16.22]) and the primary group (OR = 2.91, b = 1.07, p = .06, 95% CI [.96, 8.83]) to meet diagnostic criteria for an alcohol or drug abuse/dependence diagnosis at any time in the past. Results were significant for alcohol abuse (OR = 2.20, b = .79, p < .05, 95% CI [1.15, 4.21]), and alcohol (OR = 3.30, b = 1.20, p < .001, 95% CI [1.71, 6.38]) and drug dependence (OR = 3.86, b = 1.35, p < .001, 95% CI [1.88-7.95]). Secondary variants were over four times (OR = 4.40, b = 1.48, p < .01, 95% CI [1.53, 12.65]) more likely than both primaries and comparisons to have met diagnostic criteria for a substance-related disorder in the past.
With regard to current diagnosis, secondary variants were more likely than primary variants (OR = 2.24, b = .81, p < .05, 95% CI [1.11, 4.54]) and the control group (OR = 1.94, b = .66, p = .053, 95% CI [.99, 3.78]) to meet diagnostic criteria for an alcohol or substance use disorder. The secondary variant was over two times (OR = 2.05, b = .72, p < .05, 95% CI [1.08, 3.90]) more likely than the primary or comparison youth to meet diagnostic criteria. This difference was significant for alcohol abuse (OR = 2.62, b = .96, p < .05, 95% CI [1.21, 5.64]) and dependence (OR = 3.34, b = 1.21, p < .01, 95% CI [1.53, 7.32]), but not drug abuse/dependence.
Discussion
The results of the current study of juvenile offenders are consistent with prior adult research showing that secondary variants of psychopathy are at increased risk for co-occurring disorders. A salient set of findings emerging from our analyses indicates that, when compared to primary variants of juvenile psychopathy without comorbid psychopathology, secondary variants with comorbid psychopathology: (a) reported significantly more frequent use of substances within the six months prior to incarceration—particularly alcohol, (b) were significantly more likely to use substances while incarcerated, and (c) were significantly more likely to meet diagnostic criteria for a current DSM-IV alcohol abuse/dependence disorder; these effects were medium in magnitude (Cohen 1988; Wickens 1989). Attesting to the validity of the identified clusters, secondary variants also reported more maltreatment and internalizing problems than the comparison groups, consistent with theoretical conceptualizations (see Poythress & Skeem, 2005; Skeem et al., 2003).
Before interpreting the results further, we acknowledge several study limitations. First, the current study is limited to serious male juvenile offenders and findings may not generalize to female or community samples or to juvenile offenders with less serious histories of offending. That is, this study employed an adolescent offender sample housed in a secure facility, the majority of which were sentenced for a violent committing offense. Indeed, average YPI scores were fairly high in this sample and our use of a cut score extrapolated from a more heterogeneous sample of boys adjudicated of a felony offense—with a greater proportion of drug offenders (capped at 15%, Schubert, Mulvey et al. 2004 vs. 4%, present study)—resulted in a large proportion of youth falling in the “psychopathic” range for inclusion in the cluster analysis. While our use of a cut score to designate youth with substantial psychopathic traits on the YPI is contradictive to the most compelling data suggesting that these traits are dimensional (e.g., Edens, Marcus et al. 2011) and may limit the generalizability of our findings to other samples or studies using continuous analytic approaches, it allowed us to identify clusters of similar youth to permit comparisons of our results with prior studies of adults (e.g., Skeem, et al., 2007) and was guided by empirical research with adolescent male offenders (Cauffman, et al., 2009).
Second, the sample consisted of predominately ethnic minority youth (72%), particularly those of Hispanic descent (47%), a population for which validation studies of the YPI have yet to be conducted. While this is an important strength, given the relative lack of research on minority populations, it also limits the generalizability of findings to less ethnically heterogeneous populations. However, associations among YPI and RCMAS measures were not significantly different between the two primary racial/ethnic groups (Black and Hispanic) included in this study. Third, it is possible that certain personality traits that are characteristic of secondary psychopathy (e.g., negative emotionality) contribute to both substance abuse and to the tendency to report relatively mild levels of past parental mistreatment (e.g., criticism) as abusive. Fourth, since our indices of substance abuse within the facility relied on self-reported behavior, coupled with the fact that such activity would result in considerable sanctions from facility staff, it is possible that there was some degree of underreporting of substance abuse activity. However, despite this possibility, we did observe a fairly high proportion of youth reporting substance abuse within the facility (45.6%), which suggests that youth in the present study were largely willing to disclose this type of information. In addition, since this type of activity is likely to go undetected within the facility, relying on institutional reports of substance abuse would result in further loss of information, suggesting that self-report would be an optimal strategy. Finally, we studied a limited number of risk factors for substance abuse and dependence. We acknowledge that there are many other risk factors for adolescent substance use, including peer, environmental, and family factors, such as a family history of substance abuse, that were not tested in the present study and should be incorporated into studies seeking to obtain a more comprehensive understanding of this phenomenon. With these limitations in mind, we offer our interpretations of the results.
Juvenile offenders scoring high on a measure of psychopathy, the Youth Psychopathic Traits Inventory (YPI), reported significantly greater substance abuse than nonpsychopathic juvenile offenders. In a Dutch non-referred sample of adolescents (N = 776), Hilege and colleagues similarly found that youth scoring high on the YPI self-reported greater alcohol and drug use (Hilege, Das, & de Ruiter, 2010). Consistently, many studies have documented a link between psychopathic traits and substance use among juvenile and adult offender samples (adults, Coid et al., 2009; Walsh, Allen, & Kosson, 2007; youth, Campbell, et al., 2004; Corrado et al., 2004; Mailloux, Forth, & Kroner, 1997) (see also Hemphill, Hart, & Hare, 1994; Taylor & Lang, 2006; Rutherford, Alterman, & Cacciola, 2000). In his writing, Lykken (1995) explained that “in keeping with their propensity for risk-taking, psychopaths are more likely to abuse alcohol and especially stimulant drugs such as cocaine than is the average citizen” (p. 142). Importantly, much of this body of research links alcohol and drug abuse or dependence disorders to antisocial deviance (factor 2) traits, specifically (e.g., Smith & Newman, 1990)—the dimension of psychopathy used by several researchers as a proxy for secondary psychopathy, and which has a strong relationship with the externalizing dimension of psychopathology (r = .84)—a common factor underlying conduct disorder, adult antisocial behavior, substance use/abuse, and disinhibitory personality traits, that is largely genetically mediated (Krueger et al., 2002; Patrick, Hicks, Krueger, & Lang, 2005).
Several studies on variants of adult psychopathy have documented higher rates of substance abuse among secondary variants compared with primary variants (Alterman et al., 1998; Bagley, Abramowitz, & Kosson, 2009; Blackburn, 1998; Hicks, Vaidyanathan, & Patrick, 2010; Swogger & Kosson, 2007; Vassileva et al., 2005); Vaughn and colleagues (2009) were the first to document a similar pattern in juvenile variants of psychopathy (see also Wareham et al., 2009). They found that high-anxious secondary variants reported the greatest rates of past year substance use. The present study is the first to also examine differences between juvenile psychopathy variants in their patterns of institutional substance use, their use of specific substances, and their rates of clinical diagnoses for substance-related disorders. We found that juvenile offenders scoring high on a measure of psychopathy with comorbid psychopathology reported significantly greater substance abuse prior to entering the facility and were more likely to meet diagnostic criteria for a current substance-related disorder, compared with psychopathic youth without comorbidity. Primary variants were less likely than secondary variants to use substances during their first eight weeks of incarceration, but when they did they used at a comparable frequency to secondary variants (i.e., once per week). With regard to their use of specific types of substances, secondary variants reported significantly greater use of alcohol in the six months prior to facility entry—but comparable use within the facility—compared with primary variants. Variants did not differ significantly in their use of marijuana and harder drugs. Importantly, differences between variants could not be attributed to anxiety as this variable was uncorrelated with substance use in the current sample.
We found a modest association between psychopathy and anxiety scores. Although a wealth of evidence from the psychopathy literature has observed a negative relation between these features (e.g. Frick, O’Brien, Wootton, & McBurnett, 1994; Murrie & Cornell, 2000; Schmitt & Newman, 1999), in a delinquent adolescent sample Kosson and colleagues also found a comparable significant positive association between anxiety and PCL:YV scores (r = .25; Kosson, Cyterski et al. 2002). Whereas these authors interpreted the finding to reflect the possibility that youth—compared with adults—high on psychopathic traits had not yet “developed the same impenetrable mask of sanity” (p. 106), others have questioned the validity of juvenile psychopathy measures that correlate positively with anxiety (Skeem and Cauffman 2003). Still others argue that aspects of neuroticism and anxiety-like characteristics may accompany psychopathy at earlier developmental stages, and may become embedded within the expression of psychopathy later (Salekin, Leistico, Trobst, Schrum, & Lochman, 2005). The greater levels of anxiety observed in secondary variants in the present study is consistent with a large and growing body of empirical literature on primary and secondary psychopathy. However, it is important to note that alternative perspectives in the field are that psychopathy variants do not exist and that anxiety is not a distinguishing factor between them.
The findings of the current study help inform our understanding of the function that substance use plays in the lives of secondary variant youths. Secondary variants in the current study reported the greatest rates of maltreatment, and prior research with this sample also found higher rates of trauma exposure and PTSD symptoms relative to primary variants and comparison youth (Tatar, Cauffman et al. in press). Similarly, Hicks et al. (2010) found that adult female secondary variants reported greater exposure to traumatic events, particularly childhood physical abuse, and greater symptoms of PTSD. Importantly, stressful or traumatic events increase adolescents’ risk for developing substance use problems (Kilpartick et al., 2000), with the number of stressful events experienced being positively related to the initiation and continuation of substance use (Wills et al., 2001). Comorbid psychiatric factors have also long been recognized as contributing factors to adolescent alcohol/other drug use (Deas & Thomas, 2002); secondary variants reported greater psychiatric symptoms along with co-occurring substance problems. Of course, these factors exist in the general adolescent population, but they are present at much higher levels among high-risk youth (Teplin 2002), such as the incarcerated youth in the present study.
The distinct psychosocial histories of secondary variants set an important psychological precondition for the use of substances for self-medication reasons. Drawing on studies with adult samples, PTSD and traumatic life events influence adolescents to use substances in an effort to cope with these painful experiences (see Kilpatrick et al., 2000). This is especially the case with alcohol use (Clark et al., 1997). The self-medication hypothesis, which was first developed by Khantzian, Mack and Schatzberg (1974) and Duncan (1974), asserts that individuals’ choice of a particular drug to use does not occur by accident or coincidence. Rather, use results from psychological need, and provides, or is perceived to provide, relief from the individual’s condition—in an effort to reduce his or her distress and/or help achieve some measure of emotional stability. While Khantzian et al.’s (1974) view takes a psychodynamic approach, seeing drug users as attempting to compensate for deficient ego functioning, Duncan (1974) focused on such behavioral factors as positive reinforcement (e.g., peer approval) and negative reinforcement (e.g., reduction of negative affect). In recent years, Khantzian (1997) has revisited the self-medication hypothesis, asserting that psychiatric symptoms are key to understanding drug use disorders. Specific drugs are used to provide relief from psychological suffering, with the choice of a particular drug being based in its psychopharmacological properties. For individuals experiencing high anxiety and/or associated PTSD, central nervous system depressants, such as alcohol, produce feelings of relaxation, which may help in coping with these distressing conditions. Alcohol is also a relatively inexpensive and readily available substance for juvenile offenders, who tend to come from lower socioeconomic backgrounds. Consistently, secondary variants in the current study reported significantly greater alcohol abuse than primary variants and were more likely to meet diagnostic criteria for an alcohol abuse/dependence disorder. Similarly, in their sample of female offenders, Hicks et al. (2010) found greater alcohol use and symptoms of alcohol dependence in secondary variants compared with primary variants. Further research is clearly indicated on the “functional” relationships between emotional/psychological conditions and the use of various substances. It would appear to constitute a fertile topic for additional research involving secondary variants of psychopathic youth with comorbidity.
The combination of substance use disorders and psychopathic personality traits appears to signal greater risk for aggressive and violent outcomes. For example, Hart, Cox, and Hare (1995) found that adult psychopathic offenders housed in a state forensic hospital were more aggressive during hospitalization if they had a history of substance use disorders. In another study of adult male sexual offenders, Firestone and colleagues (1999) found that the combination of high psychopathy scores and alcohol use problems predicted greater general, violent, and sexual recidivism, compared with those offenders not showing this combination. Similarly, in a juvenile offender population, Kimonis et al. (2010) found that high-anxious secondary variants showed greater violent offending during a two-year incarceration period compared with primary variants and non-psychopathic comparison youth.
Interestingly, our analyses revealed a greater proportion of youth high on psychopathic traits classified as primary variants (n = 122) relative to secondary variants (n = 42). Although Skeem et al. (2007) also found a smaller proportion of secondary (n = 49) compared with primary variants (n = 74) in their sample of violent, long-term, adult offenders, Hicks et al. (2004) found the opposite pattern in their sample of less serious inmates housed in medium security facilities (primary vs. secondary; n = 30 vs. 66) (see also Vassileva, Kosson et al. 2005; Swogger and Kosson 2007). Still others find roughly equal proportions of primary and secondary variants (Hicks, Vaidyanathan et al. 2010; Poythress, Edens et al. 2010). A study examining serious juvenile offenders that specifically oversampled for psychopathic traits similarly found a greater proportion of primary relative to secondary variants (see also Lee, Salekin et al. 2010; n=77 vs. 39; Kimonis, Skeem et al. 2011). As such, findings suggest the prevalence of primary versus secondary variants may depend on the sample and setting studied. It is possible that social service and justice agencies may “sort” individuals who break the law into different systems, based on their perceived problems. In samples of serious offenders in criminal justice settings (i.e., the present study; Kimonis et al., 2011; Skeem et al., 2007), one might expect to find a relatively high proportion of individuals with primary psychopathic traits. In psychiatric, substance abuse, forensic, or less serious offender samples (i.e., Hicks et al., 2004; Vassileva et al., 2005), one might find a greater representation of individuals with secondary psychopathic traits. To establish prevalence rates of primary and secondary psychopathy, representative samples of individuals would need to be assessed in the setting of interest (e.g., the community, mental health settings, justice settings).
This research has important practical implications for working with juvenile offenders. First, the more extensive psychiatric problems and trauma histories reported by secondary psychopathy variants suggests the need for services that focus on problems such as negative affectivity (i.e., anxiety, depression, anger) and posttraumatic symptoms, beyond the co-occurring substance use problems that are the primary focus of traditional treatment programs targeted at substance-abusing youth. This requires that youth are first accurately identified. Assessment techniques that tap the primary-secondary psychopathy distinction are likely to be useful in identifying youth at greatest risk for problematic behaviors within the facility, and who are in greatest need of mental health services. Alarmingly, incarcerated youth are apparently reporting access to substances and secondary psychopathy variants are the most likely to seek out and use available substances. To the extent that trauma histories and related psychiatric symptoms contribute to increased risk for substance abuse, treatment of youths’ psychological problems is likely to reduce other problematic behaviors and attenuate risk for recidivism and continued substance abuse following release. Interventions may focus on identifying more positive strategies for coping with negative emotional states that stem from mental health problems related to trauma history. Greater focus on the individualized treatment needs of incarcerated youth is likely to translate into fewer future contacts with the already overburdened juvenile justice system.
Acknowledgments
We thank Richard Dembo for his helpful contribution to this manuscript and Asha Goldweber and Elizabeth Shulman for their conscientious management of this project, and our interviewers for collecting these data. Funding for this study was provided to Elizabeth Cauffman, Ph.D. from the National Institute of Mental Health (K01MH01791-01A1) and from the Center for Evidence-Based Corrections at the University of California, Irvine.
Footnotes
Our use of the term variants as opposed to subtypes is for the purpose of identifying prototypes rather than discrete categories of youth, consistent with the most compelling data suggesting that psychopathic traits are dimensional rather than a taxon (Lilienfeld 1994; Lilienfeld 1998; adults, Edens, Marcus et al. 2006; Guay, Ruscio et al. 2007; youth, Murrie, Marcus et al. 2007) (cf. adults, Harris, Rice et al. 1994; youth, Vasey, Kotov et al. 2005).
To test for the similarity in association between the two primary ethnic groups in our sample we conducted a covariance equivalence analysis (testing for equivalence of variances and covariances between groups) using manifest composite factor scores (as specified by the YPI and RCMAS measures) within multiple group structural equation models. In the first model, we specified the variances and covariances for each of the YPI and RCMAS observed factors to be unconstrained between each of the ethnic groups (allowing all free to vary) to give us a baseline model fit value with which to compare to a subsequent constrained model. This first, unconstrained model produced the following chi-square fit statistic: χ2(6) = 27.273, p < .001. We then conducted a second, constrained model (specifying each of the variances and covariances to be equal across ethnic groups). This second, constrained model produced the following chi-square fit statistic: χ2(27) = 51.737, p < .01. To determine if this change in chi-square represented a significant departure from the initial model fit, we then subtracted the baseline, unconstrained chi-square statistic and degrees of freedom from the constrained model, resulting in the following chi-square fit: χ2(21) = 24.464, p > .10. The results suggest that our assumption that the association between psychopathy and anxiety does not differ across ethnic groups is supported, which is consistent with the reported correlation values.
To validate the accuracy of group placement within the model, a second cluster analysis was conducted using mixture modeling through the Mplus software program (Muthén & Muthén, 2007). Again, a two-group solution provided the best-fitting model (BIC = 5226.8; Entropy = .82), with posterior probabilities above .90, suggesting adequate confidence in accurate group placement. Since two groups again showed the best fit in this supplemental analysis, this increases confidence that a two-group solution is the best fit for the present sample. The resulting groups revealed a somewhat larger secondary group (n = 47) and somewhat smaller primary group (n = 118). Most notably, the original 43 secondaries identified in Mclust were also assigned to the secondary group using Mplus. Thus, this “robust” secondary group was used for the remainder of the analyses.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
Contributor Information
Eva R. Kimonis, Department of Mental Health Law and Policy, University of South Florida
Joseph R. Tatar, II, Department of Psychology and Social Behavior, University of California, Irvine.
Elizabeth Cauffman, Department of Psychology and Social Behavior, University of California, Irvine.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. University of Vermont Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Alterman AI, McDermott PA, Cacciola JS, Rutherford MJ, Boardman CR, McKay JR, Cook TG. A typology of antisociality in methadone patients. Journal of Abnormal Psychology. 1998;107:412–422. doi: 10.1037//0021-843x.107.3.412. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed., text revision American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Andershed H, Kerr M, Stattin H, Levander S. Psychopathic traits in non-referred youths: A new assessment tool. In: Blaauw E, Sheridan L, editors. Psychopaths: Current International Perspectives. Elsevier; The Hague: 2002. pp. 131–158. [Google Scholar]
- Bagley AD, Abramowitz CS, Kosson DS. Vocal affect recognition and psychopathy: converging findings across traditional and cluster analytic approaches to assessing the construct. Journal of Abnormal Psychology. 2009;118:388–398. doi: 10.1037/a0015372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banfield JD, Raftery AE. Model-based Gaussian and non-Gaussian clustering. Biometrics. 1993;49:803–821. [Google Scholar]
- Blackburn R. An empirical classification of psychopathic personality. British Journal of Psychiatry. 1975;127:456–460. doi: 10.1192/bjp.127.5.456. [DOI] [PubMed] [Google Scholar]
- Blackburn R. Psychopathy and the contribution of personality to violence. In: Millon T, Simonsen E, editors. Psychopathy: antisocial, criminal, and violent behavior. Guilford; New York: 1998. pp. 50–68. [Google Scholar]
- Campbell MA, Porter S, Santor DA. Psychopathic traits in adolescent offenders: An evaluation of criminal history, clinical, and psychosocial correlates. Behavioral Sciences & the Law. 2004;22:23–47. doi: 10.1002/bsl.572. [DOI] [PubMed] [Google Scholar]
- Cauffman E, Feldman S, Waterman J, Steiner H. Posttraumatic stress disorder among incarcerated females. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1209–1216. [PubMed] [Google Scholar]
- Cauffman E, Kimonis ER, Dmitrieva J, Monahan K. A multi-method assessment of juvenile psychopathy: Comparing the predictive utility of the PCL:YV, YPI, and NEO-PRI. Psychological Assessment. 2009;21:528–542. doi: 10.1037/a0017367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Lesnick L, Hegedus AM. Traumas and other adverse life events in adolescents with alcohol abuse and dependence. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1744–1751. doi: 10.1097/00004583-199712000-00023. [DOI] [PubMed] [Google Scholar]
- Cleckley H. The mask of sanity. C.V. Mosby; St. Louis, MO: 1941. [Google Scholar]
- Cleckley H. The mask of sanity. 5th ed C.V.: Mosby Co.; Saint Louis: 1976. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Coid JW, Yang M, Ullrich S, Roberts AD, Hare RD. Prevalence and correlates of psychopathic traits in the household population of Great Britain. International Journal of Law and Psychiatry. 2009;32:65–73. doi: 10.1016/j.ijlp.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Corrado RR, Vincent GM, Hart SD, Cohen IM. Predictive validity of the Psychopathy Checklist: Youth Version for general and violent recidivism. Behavioral Sciences and the Law. 2004;22:5–22. doi: 10.1002/bsl.574. [DOI] [PubMed] [Google Scholar]
- Deas D, Thomas S. Comorbid psychiatric factors contributing to adolescent alcohol and other drug use. Alcohol Research and Health. 2002;26:116–121. [Google Scholar]
- Declercq F, Markey S, Vandist K, Verhaeghe P. The Youth Psychopathic Trait Inventory: factor structure and antisocial behaviour in non-referred 12-17-year-olds. The Journal of Forensic Psychiatry & Psychology. 2009;20(4):577–594. [Google Scholar]
- Duncan DF. Reinforcement of drug abuse: Implications for prevention. Clinical Toxicology Bulletin. 1974;4:69–75. [Google Scholar]
- Edens JF, Marcus DK, Lilienfeld SO, Poythress NG. Psychopathic, not psychopath: Taxometric evidence for the dimensional structure of psychopathy. Journal of Abnormal Psychology. 2006;115(1):131–144. doi: 10.1037/0021-843X.115.1.131. [DOI] [PubMed] [Google Scholar]
- Edens JF, Marcus DK, Vaughn MG. Exploring the Taxometric Status of Psychopathy Among Youthful Offenders: Is There a Juvenile Psychopath Taxon? Law and Human Behavior. 2011;35:13–24. doi: 10.1007/s10979-010-9230-8. doi: 10.1007/s10979-010-9230-8. [DOI] [PubMed] [Google Scholar]
- Falkenbach D, Poythress N, Creevy C. The exploration of subclinical psychopathic subtypes and the relationship with types of aggression. Personality and Individual Differences. 2008;44:821–832. [Google Scholar]
- Firestone P, Bradford JM, McCoy M, Greenberg DM, LaRose MR, Curry S. Prediction of recidivism in incest offenders. Journal of Interpersonal Violence. 1999;14:511–531. [Google Scholar]
- Forth AE, Burke HC. Psychopathy in adolescence: Assessment, violence and developmental precursors. In: Cooke D, Forth A, Hare R, editors. Psychopathy: Theory, research and implications for society. Kluwer; Dordrecht: 1998. pp. 205–230. [Google Scholar]
- Forth AE, Kosson DS, Hare RD. The Hare Psychopathy Checklist: Youth Version. Multi-Health Systems; North Tonawanda, NY: 2003. [Google Scholar]
- Fraley C, Raftery AE. MCLUST:Software for model-based clustering, density estimation and discriminant analysis. Technical Report. 2002a Retrieved from http://www.stat.washington.edu/tech.reports.
- Fraley C, Raftery AE. Model-based clustering, discriminant analysis, and density estimation. Journal of the American Statistical Association. 2002b;380(2000) [Google Scholar]
- Fraley C, Raftery AE. The mclust02 package. 2008 from http://www.stat.washington.edu/mclust.
- Frick PJ. Callous-unemotional traits and conduct problems: A two-factor model of psychopathy in children. Issues in Criminological and Legal Psychology. 1995;24:47–51. [Google Scholar]
- Frick PJ. Developmental pathways to conduct disorder. Child and Adolescent Psychiatric Clinics of North America. 2006;15:311–331. doi: 10.1016/j.chc.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Marsee MA. Psychopathy and developmental pathways to antisocial behavior in youth. In: Patrick CJ, editor. Handbook of psychopathy. Guilford; New York: 2006. pp. 355–374. [Google Scholar]
- Frick PJ, O’Brien BS, Wootton JM, McBurnett K. Psychopathy and conduct disorders in children. Journal of Abnormal Psychology. 1994;103:700–707. doi: 10.1037//0021-843x.103.4.700. [DOI] [PubMed] [Google Scholar]
- Gil-Rivas V. Unpublished doctoral dissertation. University of California; Irvine: 2003. Parental contributions to adolescents’ psychological adjustment following the terrorist attacks of September 11, 2001. [Google Scholar]
- Guay JP, Ruscio J, Knight RA, Hare RD. A taxometric analysis of the latent structure of psychopathy: Evidence for dimensionality. Journal of Abnormal Psychology. 2007;116(4):701–716. doi: 10.1037/0021-843X.116.4.701. [DOI] [PubMed] [Google Scholar]
- Haapasalo J, Pulkkinen L. The Psychopathy Checklist and non-violent offender groups. Criminal Behaviour and Mental Health. 1992;2:315–328. [Google Scholar]
- Hare RD. The Psychopathy Checklist-Revised (PCL-R) Multi-Health Systems; Toronto, ON: 1991. [Google Scholar]
- Hare RD. The Psychopathy Checklist—Revised. 2nd ed Multi-Health Systems; Toronto: 2003. [Google Scholar]
- Hare RD, Neumann CS. The role of antisociality in the psychopathy construct: Comment on Skeem and Cooke (2010) Psychological Assessment. 2010;22:446–454. doi: 10.1037/a0013635. [DOI] [PubMed] [Google Scholar]
- Harris GT, Rice ME, Quinsey VL. Psychopathy as a taxon: Evidence that psychopaths are a discrete class. Journal of Consulting and Clinical Psychology. 1994;62:387–397. doi: 10.1037//0022-006x.62.2.387. [DOI] [PubMed] [Google Scholar]
- Harrison LD, Martin SS, Enev T, Harrington D. Comparing drug testing and self-report of drug use among youths and young adults in the general population. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2007. (DHHS Publication No. SMA 07-4249, Methodology Series M-7) [Google Scholar]
- Hart SD, Cox DN, Hare RD. The Hare Psychopathy Checklist: Screening Version. 1st ed Multi-Health Systems; Toronto, ON, Canada: 1995. [Google Scholar]
- Hemphill JF, Hart SD, Hare RD. Psychopathy and substance use. Journal of Personality Disorders. 1994;8:169–180. [Google Scholar]
- Hicks BM, Markon KE, Patrick CJ, Krueger RF, Newman JP. Identifying psychopathy subtypes based on personality structure. Psychological Assessment. 2004;16:276–288. doi: 10.1037/1040-3590.16.3.276. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Vaidyanathan U, Patrick CJ. Validating female psychopathy subtypes: Differences in personality, antisocial and violent behavior, substance abuse, trauma, and mental health. Personality Disorders: Theory, Research, & Treatment. 2010;1:38–57. doi: 10.1037/a0018135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser Y, Maglione M, Boyle K. Validity of self-report of drug use among STD patients, ER patients, and arrestees. American Journal of Drug and Alcohol Abuse. 1999;25:81–91. doi: 10.1081/ada-100101847. [DOI] [PubMed] [Google Scholar]
- Hundt NE, Kimbrel NA, Mitchell JT, Nelson-Gray RO. High BAS, but not low BIS, predicts externalizing symptoms in adults. Personality and Individual Differences. 2008;44:565–575. [Google Scholar]
- Insightful Corporation . S-PLUS version 7.0 for Windows. Insightful Corporation; Seattle, Washington: 1988-2005. [Google Scholar]
- Karpman B. Conscience in the psychopath: Another version. American Journal of Orthopsychiatry. 1948;18:455–491. doi: 10.1111/j.1939-0025.1948.tb05109.x. [DOI] [PubMed] [Google Scholar]
- Karpman B. Criminal psychodynamics: A platform. Archives of Criminal Psychodynamics. 1955;1:3–100. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for affective disorders and schizophrenia for school-age children-present version and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychology. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of drug use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ, Mack JF, Schatzberg AF. Heroin use as an attempt to cope: Clinical observations. American Journal of Psychiatry. 1974;131:160–164. doi: 10.1176/ajp.131.2.160. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Skeem J, Cauffman E, Dmitrieva J. Are secondary variants of ‘juvenile psychopathy’ more reactively violent and less psychosocially mature than primary variants? Law and Human Behavior. 2011;35(5):381–391. doi: 10.1007/s10979-010-9243-3. doi: 10.1007/s10979-010-9243-3. [DOI] [PubMed] [Google Scholar]
- Kosson DS, Cyterski TD, Steuerwald BL, Neumann CS, Walker-Matthews S. The reliability and validity of the Psychopathy Checklist: Youth Version (PCL:YV) in nonincarcerated adolescent males. Psychological Assessment. 2002;14(1):97–109. doi: 10.1037//1040-3590.14.1.97. [DOI] [PubMed] [Google Scholar]
- Kosson D, Newman J. An evaluation of Mealey’s hypotheses based on Psychopathy Checklist identified groups. Behavioral and Brain Sciences. 1995;18:562–563. [Google Scholar]
- Krischer MK, Sevecke K. Early traumatization and psychopathy in female and male juvenile offenders. International Journal of Law and Psychiatry. 2008;31:253–262. doi: 10.1016/j.ijlp.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Lang S, af Klinteberg B, Alm PO. Adult psychopathy and violent behavior in males with early neglect and abuse. Acta Psychiatricka Scandinavica. 2002;106:93–100. doi: 10.1034/j.1600-0447.106.s412.20.x. [DOI] [PubMed] [Google Scholar]
- Lee Z, Salekin RT, Iselin AR. Psychopathic traits in youth: Is there evidence for primary and secondary subtypes? Journal of Abnormal Child Psychology. 2010;38:381–393. doi: 10.1007/s10802-009-9372-7. [DOI] [PubMed] [Google Scholar]
- Lilienfeld S. Conceptual problems in the assessment of psychopathy. Clinical Psychology Review. 1994;14:17–38. [Google Scholar]
- Lilienfeld S. Methodological advances and developments in the assessment of psychopathy. Behaviour Research and Therapy. 1998;36:99–125. doi: 10.1016/s0005-7967(97)10021-3. [DOI] [PubMed] [Google Scholar]
- Lykken DT. The antisocial personalities. Erlbaum; Mahwah, NJ: 1995. [Google Scholar]
- Lynam DR. The early identification of chronic offenders: Who is the fledgling psychopath? Psychological Bulletin. 1996;120:209–234. doi: 10.1037/0033-2909.120.2.209. [DOI] [PubMed] [Google Scholar]
- Mailloux DL, Forth AE, Kroner DG. Psychopathy and substance use in adolescent male offenders. Psychological Reports. 1997;81:529–530. [PubMed] [Google Scholar]
- Marcus DK, Lilienfeld SO, Edens JF, Poythress NG. Is antisocial personality disorder continuous or categorical? A taxometric analysis. Psychological Medicine. 2006;36:1571–1581. doi: 10.1017/S0033291706008245. [DOI] [PubMed] [Google Scholar]
- Marshall LA, Cooke DJ. The role of childhood experiences in the aetiology of Psychopathy. Issues in Criminological and Legal Psychology. 1995;24:107–108. [Google Scholar]
- Mealey L. The sociobiology of sociopathy: An integrated evolutionary model. Behavioral and Brain Sciences. 1995;19:523–540. [Google Scholar]
- Muris P, Merckelbach H, Ollendick TH, King NJ, Bogie N. Three traditional and three new childhood anxiety questionnaires: their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40:753–772. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- Murrie DC, Cornell DG. The Millon Adolescent Clinical Inventory (MACI) and psychopathy. Journal of Personality Assessment. 2000;75:110–125. doi: 10.1207/S15327752JPA7501_8. [DOI] [PubMed] [Google Scholar]
- Murrie DC, Marcus DK, Douglas K, Lee Z, Salekin RT, Vincent GM. Youth with psychopathy features are not a discrete class: a taxometric analysis. Journal of Child Psychology and Psychiatry. 2007;48(7):714–723. doi: 10.1111/j.1469-7610.2007.01734.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5th Ed Muthén & Muthén; Los Angeles, CA: 2007. [Google Scholar]
- Needle R, McCubbin H, Lorence J, Hochhauser M. Reliability and validity of adolescent self-reported drug use in a family-based study: A methodological report. Substance Use & Misuse. 1983;18:901–912. doi: 10.3109/10826088309033058. [DOI] [PubMed] [Google Scholar]
- Novaco RW. The Novaco Anger Scale and Provocation Inventory. Western Psychological Services; Los Angeles: 2003. [Google Scholar]
- Oetting ER, Beauvais F. Adolescent drug use: Findings of national and local surveys. Journal of Consulting and Clinical Psychology. 1990;58:385–394. doi: 10.1037//0022-006x.58.4.385. [DOI] [PubMed] [Google Scholar]
- O’Neill ML, Lidz V, Heilbrun K. Adolescents with psychopathic characteristics in a substance abusing cohort: Treatment process and outcomes. Law and Human Behavior. 2003;27:299–313. doi: 10.1023/a:1023435924569. [DOI] [PubMed] [Google Scholar]
- Porter S. Without conscience or without active conscience? The etiology of psychopathy Revisited. Aggression and Violent Behavior. 1996;1:179–189. [Google Scholar]
- Poythress NG, Dembo R, Wareham J, Greenbaum P. Construct validity of the Youth Psychopathic traits Inventory (YPI) and the Antisocial Process Screening Device (APSD) with justice involved adolescents. Criminal Justice and Behavior. 2006;33:26–55. [Google Scholar]
- Poythress NG, Edens JF, Skeem JL, Lilienfeld SO, Douglas KS, Frick PJ, et al. Identifying subtypes among offenders with antisocial personality disorder: A cluster-analytic study. Journal of Abnormal Psychology. 2010 doi: 10.1037/a0018611. [DOI] [PubMed] [Google Scholar]
- Poythress N, Skeem J. Disaggregating psychopathy: Where and how to look for variants. In: Patrick’s C, editor. Handbook of Psychopathy. Guilford; New York: 2005. pp. 172–192. [Google Scholar]
- Poythress NG, Skeem JL, Lilienfeld SO. Associations among early abuse, dissociation, and psychopathy in an offender sample. Journal of Abnormal Psychology. 2006;115:288–297. doi: 10.1037/0021-843X.115.2.288. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reynolds CR. Long-term stability of scores on the Revised-Children ’s Manifest Anxiety Scale. Perceptual and Motor Skills. 1981;53:702. doi: 10.2466/pms.1981.53.3.702. [DOI] [PubMed] [Google Scholar]
- Reynolds CR. Convergent and divergent validity of the Revised Children’s Manifest Anxiety Scale. Educational and Psychological Measurement. 1982;42:1205–1212. [Google Scholar]
- Reynolds CR, Richmond BO. The Revised Children’s Manifest Anxiety Scale manual. Western Psychological Services; Los Angeles: 1985. [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology. 1997;25:15–20. doi: 10.1023/a:1025751206600. [DOI] [PubMed] [Google Scholar]
- Rutherford MJ, Alterman JS, Cacciola AI. Psychopathy and substance abuse: A bad mix. In: Gacono CB, editor. The Clinical and Forensic Assessment of Psychopathy: A Practitioner’s Guide. Laurence Erlbaum Associates; Mahwah. New Jersey: 2000. pp. 351–368. [Google Scholar]
- Salekin RT, Leistico AR, Trobst KK, Schrum CL, Lochman JE. Adolescent psychopathy and the interpersonal circumplex: Expanding evidence of a nomological net. Journal of Abnormal Child Psychology. 2005;33:445–460. doi: 10.1007/s10802-005-5726-y. [DOI] [PubMed] [Google Scholar]
- Salekin RT, Neumann CS, Leistico AR, DiCicco TM, Duros R. Construct validity of psychopathy in a young offender sample: Taking a closer look at psychopathy’s potential importance over disruptive behavior disorders. Journal of Abnormal Psychology. 2004;113:416–427. doi: 10.1037/0021-843X.113.3.416. [DOI] [PubMed] [Google Scholar]
- Schmitt WA, Newman JP. Are all psychopathic individuals low-anxious? Journal of Abnormal Psychology. 1999;108:353–358. doi: 10.1037//0021-843x.108.2.353. [DOI] [PubMed] [Google Scholar]
- Schubert C, Mulvey E, Steinberg L, Cauffman E, Losoya S, Hecker T, et al. Operational lessons from the pathways to desistance project. Journal of Youth Violence and Juvenile Justice. 2004;2:237–255. doi: 10.1177/1541204004265875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeem JL, Cauffman E. Views of the downward extension: Comparing the Youth Version of the Psychopathy Checklist with the Youth Psychopathic Traits Inventory. Behavioral Sciences and the Law. 2003;21:737–770. doi: 10.1002/bsl.563. [DOI] [PubMed] [Google Scholar]
- Skeem JL, Cooke DJ. Is criminal behavior a central component of psychopathy? Conceptual directions for resolving the debate. Psychological Assessment. 2010a;22:433–445. doi: 10.1037/a0008512. [DOI] [PubMed] [Google Scholar]
- Skeem JL, Cooke DJ. One measure does not a construct make: Directions toward reinvigorating psychopathy research—Reply to Hare and Neumann (2010) Psychological Assessment. 2010b;22:455–459. doi: 10.1037/a0014862. [DOI] [PubMed] [Google Scholar]
- Skeem JL, Johansson P, Andershed H, Kerr M, Eno Louden J. Two subtypes of psychopathic violent offenders that parallel primary and secondary variants. Journal of Abnormal Psychology. 2007;116:395–409. doi: 10.1037/0021-843X.116.2.395. [DOI] [PubMed] [Google Scholar]
- Skeem JL, Poythress N, Edens JF, Lilienfeld SO, Cale EM. Psychopathic personality or personalities? Exploring potential variants of psychopathy and their implications for risk assessment. Aggression and Violent Behavior. 2003;8:513–546. [Google Scholar]
- Smith C, Thornberry TP. The relationship between childhood maltreatment and adolescent involvement in delinquency. Criminology. 1995;33:451–481. [Google Scholar]
- Smith SS, Newman JP. Alcohol and drug abuse/dependence in psychopathic and nonpsychopathic criminal offenders. Journal of Abnormal Psychology. 1990;99:430–439. doi: 10.1037//0021-843x.99.4.430. [DOI] [PubMed] [Google Scholar]
- Stice E, Barrera M, Chassin L. Relation of parental support and control to adolescents’ externalizing symptomatology and substance use: A longitudinal examination of curvilinear effects. Journal of Abnormal Child Psychology. 1993;21:609–629. doi: 10.1007/BF00916446. [DOI] [PubMed] [Google Scholar]
- Swogger MT, Kosson DS. Identifying subtypes of criminal psychopaths: A replication and extension. Criminal Justice and Behavior. 2007;34(8):953–970. doi: 10.1177/0093854807300758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatar JR, Cauffman E, Kimonis ER, Skeem JL. Victimization history and post-traumatic stress: An analysis of psychopathy variants in male juvenile offenders. Journal of Child and Adolescent Trauma. (in press) [Google Scholar]
- Taylor J, Lang AR. Psychopathy and substance use disorders. In: Patrick CJ, editor. Handbook of psychopathy. Guilford Press; New York: 2006. pp. 495–511. [Google Scholar]
- Teplin L, Abram K, McClelland G, Dulcan M, Mericle A. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59:1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasey MW, Kotov R, Frick PJ, Loney BR. The latent structure of psychopathy in youth: A taxometric investigation. Journal of Abnormal Child Psychology. 2005;33(4):411–429. doi: 10.1007/s10802-005-5723-1. [DOI] [PubMed] [Google Scholar]
- Vassileva J, Kosson DS, Abramowitz C, Conrod P. Psychopathy versus psychopathies in classifying criminal offenders. Legal and Criminological Psychology. 2005;10:27–43. [Google Scholar]
- Vaughn MG, Edens JF, Howard MO, Smith ST. An investigation of primary and secondary psychopathy in a statewide sample of incarcerated youth. Youth Violence and Juvenile Justice. 2009;7:172–188. [Google Scholar]
- Walsh Z, Allen LC, Kosson DS. Beyond social deviance: Substance-specific relationships with PCL-R facets. Journal of Personality Disorders. 2007;21:273–288. doi: 10.1521/pedi.2007.21.3.273. [DOI] [PubMed] [Google Scholar]
- Wareham J, Dembo R, Poythress NG, Childs K, Schmeidler J. A latent class factor approach to identifying subtypes of juvenile diversion youths based on psychopathic features. Behavioral Sciences and the Law. 2009;27:71–95. doi: 10.1002/bsl.844. [DOI] [PubMed] [Google Scholar]
- Wickens T. Multiway Contingency Tables Analysis for the Social Sciences. Erlbaum; Hillsdale, NJ: 1989. [Google Scholar]
- Weeks R, Widom C. Self-reports of early childhood victimization among incarcerated adult male felons. Journal of Interpersonal Violence. 1998;13:346–361. [Google Scholar]
- Weiler BL, Widom CS. Psychopathy and violent behavior in abused and neglected young adults. Criminal Behavior and Mental Health. 1996;6:253–271. [Google Scholar]
- Wills TA, Sandy JM, Yaeger AM, Cleary SD, Shinar O. Coping dimensions, life stress, and adolescent substance use: A latent growth analysis. Journal of Abnormal Psychology. 2001;110:309–323. doi: 10.1037//0021-843x.110.2.309. [DOI] [PubMed] [Google Scholar]
- Whiteman SD, Loken E. Comparing analytic techniques to classify dyadic relationships: An example using siblings. Journal of Marriage and Family. 2006;68:1370–1382. [Google Scholar]
- Winters KC, Stinchfield RD, Henly GA, Schwartz RH. Validity of adolescent self-reports of alcohol and other drug involvement. The International Journal of the Addictions. 1991;25:1379–1395. doi: 10.3109/10826089009068469. [DOI] [PubMed] [Google Scholar]