Abstract
Objective: Peer-assisted learning is widely used in medical education. However, little is known about an appropriate didactic preparation for peer tutors. We herein describe the development of a focused didactic training for skills lab tutors in Internal Medicine and report on a retrospective survey about the student tutors’ acceptance and the perceived transferability of attended didactic training modules.
Methods: The course consisted of five training modules:
‘How to present and explain effectively’: the student tutors had to give a short presentation with subsequent video analysis and feedback in order to learn methods of effective presentation.
‘How to explain precisely’: Precise explanation techniques were trained by exercises of exact description of geometric figures and group feedback.
‘How to explain on impulse’: Spontaneous teaching presentations were simulated and feedback was given.
‘Peyton’s 4 Step Approach’: Peyton‘s Method for explanation of practical skills was introduced and trained by the participants.
‘How to deal with critical incidents’: Possibilities to deal with critical teaching situations were worked out in group sessions.
Twenty-three student tutors participated in the retrospective survey by filling out an electronic questionnaire, after at least 6 months of teaching experience.
Results: The exercise ‘How to present and explain effectively’ received the student tutors’ highest rating for their improvement of didactic qualification and was seen to be most easily transferable into the skills lab environment. This module was rated as the most effective module by nearly half of the participants. It was followed by ‘Peyton’s 4 Step Approach’ , though it was also seen to be the most delicate method in regard to its transfer into the skills lab owing to time concerns. However, it was considered to be highly effective. The other modules received lesser votes by the tutors as the most helpful exercise in improving their didactic qualification for skills lab teaching.
Conclusion: We herein present a pilot concept for a focused didactic training of peer tutors and present results of a retrospective survey among our skills lab tutors about the distinct training modules. This report might help other faculties to design didactic courses for skills lab student tutors.
Keywords: Peer-assisted learning, Skills lab, didactic training, Peyton's Methode
Abstract
Ziele: Tutorgestütztes Lernen ist ein etablierter Bestandteil der medizinischen Ausbildung vieler Fakultäten. Allerdings herrscht Unklarheit darüber, ob und wie studentische Tutoren für diese Aufgabe didaktisch geschult werden sollen. Ziel dieses Artikels ist die Beschreibung der Entwicklung und Implementierung eines Didaktiktrainings für Tutoren unseres Skills Lab Innere Medizin. Wir berichten darüber hinaus die Ergebnisse einer retrospektiven Umfrage in Bezug auf studentische Akzeptanz und Erfahrungen mit der Umsetzung des Trainings in der Lehrpraxis.
Methoden: Unser Kurs umfasst fünf Module:
„Effektiv präsentieren“ – Kurzvortrag der Tutoren mit anschließendem Video-Feedback.
„Gutes Erklären“ – exakte Beschreibung geometrischer Figuren und anschließendes Gruppen-Feedback.
„Ad-hoc Erklären“ – spontaner Kurzvortrag mit Feedback.
„Peyton Methode“ – Erklärung und praktische Übung zur Methodik.
„Umgang mit schwierigen didaktischen Situationen“ – Erarbeitung möglicher Lösungen in schwierigen didaktischen Situationen in Gruppenarbeit.
Nach > 6 Monaten Lehrerfahrung beantworteten 23 studentische Tutoren retrospektiv einen elektronischen Fragebogen.
Ergebnisse: Das Modul „Effektiv präsentieren“ wurde als die hilfreichste Trainingseinheit für die eigene didaktische Befähigung bewertet. Die Tutoren attestierten diesem Modul außerdem die beste Übertragbarkeit für den Skills Lab Unterricht. Fast die Hälfte der Teilnehmer bewertete dieses Modul deshalb auch als das Effektivste. Es folgte die „Peyton Methode“, wobei die Umsetzung aus Zeitgründen als schwierig angesehen wurde. Dennoch wurde auch dieses Modul als sehr effektiv bewertet. Die übrigen Module wurden von deutlich weniger Tutoren als besonders effektives Training für didaktische Fähigkeiten bewertet.
Schlussfolgerung: Das Pilotprojekt unseres Didaktiktrainings für studentische Tutoren wird zusammen mit einer retrospektiven Evaluation detailliert dargestellt, so dass andere Fakultäten bezüglich einer eigenen Trainingsentwicklung davon profitieren können.
Introduction
Peer-assisted learning (PAL) is widely used in medical education [1], [2], and is popular among tutees as well as their peer tutors [3]. PAL has been established throughout a broad range of medical specialties including communication skills as well as a variety of technical medical skills [4], [5], [6], [7]. The efficiency of PAL has been investigated in very different contexts, as e.g. injection skills [8], basic abdominal ultrasound [9], musculosceletal ultrasound [10], communication skills [7] and clinical examination courses [11]. Since there is a positive correlation between effective teaching and the competency of the teacher [12], [13], [14], [15], the student tutors ability to teach is crucial for the success of the tutees. Thus, making tutors ‘fit to teach’ is of pivotal importance for an effective PAL program.
Only some programs reported to train tutors in didactic techniques for teaching them on how to teach [7], [12], [16], [17], [18]. However, most of these reports lack of any details on the corresponding didactic syllabus used in these settings. In addition, most of these programs did not evaluate their didactic training program in regard to its acceptance and its transferability into teaching reality (see ref. [12] for further review).
At our faculty, we introduced a student-tutor based technical skills lab training in 2005 [4].
After establishing student tutor training courses in regard to taught medical skills, we stepwise introduced a specific didactic tutor training, designed by our Competence Center for University Teaching in Medicine [19]. This training comprises five distinct elements, reaching from Peyton’s Method [20] to a tutorial on effective presentation techniques based on individual feedback by video coaching. Our PAL system was found to be effective in a clinical skills lab setting as well as in undergraduate anatomy courses [8], [9], [21], [22].
In this paper, we report the details of our didactic training for skills lab student tutors, which is provided at the beginning of the tutors’ teaching activities. We comment on why certain contents of the didactic training were selected for our purpose. In addition, we provide the results of a retrospective survey among 23 experienced skills lab student tutors, both on their acceptance of the training and on their experience with the subsequent transfer of learned didactic elements into the real teaching situation.
Methods
Participants
We invited 25 experienced (more than 6 months of teaching activity) student tutors who worked in our skills lab for Internal Medicine to participate voluntarily in this survey. A total of 23 tutors responded (11 females, 12 males). All study participants had received a didactic training targeted to their needs as a teacher in undergraduate skills lab training before their teaching activity (see below for further details on this training). The survey participants were from three different tutor cohorts, and therefore were trained on three separate occasions with a time lag of 6 months each. As not all modules were taught to every single student out of the 25 surveyed tutors in this pilot project, the number of participants for each of the modules slightly differs and is given separately in brackets.
General considerations on helpful didactic elements
The 1-day didactic training of student tutors was conducted in parallel groups of no more than 8 participants. The courses were held by two experienced instructors. If appropriate, e.g. for more extensive individual instruction, the groups were either divided in smaller groups, or they joined in a plenary session for theoretical input. The aim of the didactic training was to provide helpful didactic techniques and tips for the upcoming skills lab tutorial. In our opinion, student tutors not only need medical professional knowledge, but also social, communicative, and conflict solving competencies as well as knowledge about group dynamics and some insight into different learning theories. In our training, the tutors worked on the topics interactively (“learning by doing”) and transferred the new information learned to their own tutorial setting. In the following, the main training modules are presented in detail:
Description of the didactic training
Module 1
Title: How to present and explain effectively (N=19)
Objectives:
Demanding active knowledge from the students using activating teaching methods,
Giving and receiving feedback effectively.
Method: A tutorial simulation with 1:1 video analysis [23] – The tutors were asked to simulate a 7 min-tutorial session that they had prepared at home (group size: no more than 8 participants). The module was focused on techniques like explaining, visualizing, questioning, impulse setting as well as important presentation aspects like e.g. eye contact and body language. Using the simulations as case model, we focused on one or two of the techniques and discussed alternatives. Giving and receiving feedback effectively was practiced extensively during these sessions. Peers provided systematic feedback with a structured observation sheet. The student tutors’ self reflections, their peers’ feedback as well as 1:1 trainer’s feedback during watching their own video ensured a comprehensive view on their acting as a teacher.
Module 2
Title: How to explain precisely (N=21)
Objective: Getting aware of how difficult it is to describe a problem in such a way that the audience may understand correctly, and learning supportive as well as interfering aspects.
Method: In groups of four students, a one way-communication was constructed: One participant was asked to turn his/her back on the others and to describe a complex geometrical figure without any eye or reciprocal verbal contact. Two other participants were listening and tried to reconstruct the figure by means of given wooden pieces, by using sign language only. The fourth person observed and recorded positive and negative observations for further plenary discussion: What worked best? What impeded the understanding?
Module 3
Title: How to explain on impulse (N=12; provided only for tutor cohort 3)
Objective: Answering questions by explaining in a structured, understandable and precise way.
Method: Spontaneous teaching presentations as might occur during the skills lab tutorial were simulated. The tutor had to explain on demand a FAQ, an abstract term, a defined clinical problem, a physiological or topographical background to each tutorial module. For the ad hoc-exercise, topics consented by the group were written on a piece of paper. In turn, any participant drew a task and started to “explain immediately and, if appropriate, visualize” in 2-3 minutes. Peer feedback was focused on structure, comprehensibility and visualization tools.
Module 4
Title: How to convey practical skills effectively with Peyton’s 4 Step Approach [20] (N=23)
Objective: Teaching complex practical skills.
Method: The tutors were asked to prepare any practical skill that they would like to teach their peers, as e.g. making a sailor’s knot, knitting, dancing, using chemical pipettes correctly, or suturing. In groups of 3, the tutors practiced by following the four steps of Peyton’s Method, with one person in each group observing. Finally, the positive and negative experiences were analyzed and the transfer into tutorial practice was discussed.
Module 5
Title: How to deal with critical incidents (N=20)
Objective: Ensuring a conductive atmosphere in the tutorial group and handling difficult teaching situations.
Method: Tutors need to perceive group processes in order to influence them as positive as possible. For reviewing group dynamics [24], a trainer input to group development was integrated. In a brainstorming, the tutors collected situations that they perceived as difficult in earlier teaching or speaker situations. Critical incidents and the role occupied by certain participants (e.g. the “opposer”, the “troublemaker”, the “insensible”, etc.) were analyzed systematically. Supportive and interfering roles were worked out, and alternatives of reactions were discussed.
Evaluation
Retrospective evaluation was performed when tutors had at least six months experience as a teacher following the didactic course. We used an online questionnaire consisting of a 6-point Likert scale (1=totally agree, 6=totally disagree) for each provided module, a global rating of the didactic training and a text box for free comments. In this global rating, tutors were asked, which of the 5 distinct modules had mostly improved their didactic qualification. Furthermore, data on previous education in other medical specialties (nurse, paramedic) or previous teaching activities/experiences were obtained in order to avoid any systematic bias.
Results
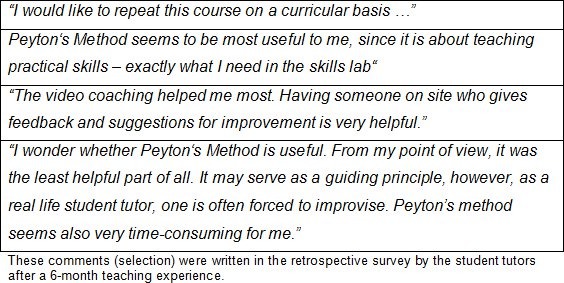
Of the 23 student tutors participating in this survey, a total of 17 disposed over previous teaching experience as e.g. as a student tutor in gross anatomy, pediatrics or emergency medicine. Having previous experience as a teacher was not associated with preference for one of the modules of the didactic training. In general, the tutors’ perception of the didactic course was very positive, as reflected by the oral as well as written feedback (some examples are given in table 1 (Tab. 1)).
Table 1. Free comments about the didactic training.
The module “How to present effectively” was rated to improve the tutors’ general didactic qualification most (1.79±0.71), while there were only little differences between the other four modules provided (2.35-2.68). The module “How to present effectively” was also seen to be most easily transferable into the skills lab environment (1.68±0.75). Furthermore, the practice “How to present effectively” was reported to be the most useful part (1.21±0.42) for skills lab teaching, followed by “How to deal with critical incidents” (1.35±0.81, further details are provided in table 2 (Tab. 2)).
Table 2. Retrospective rating of the different training modules.
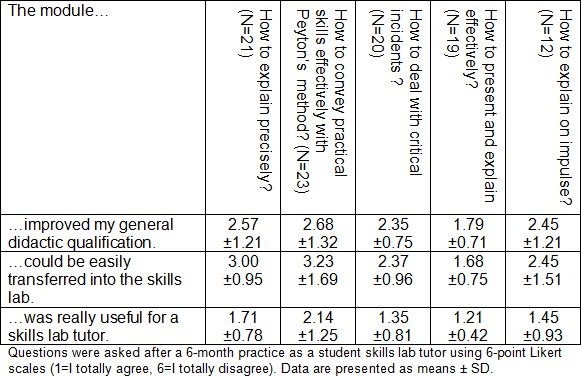
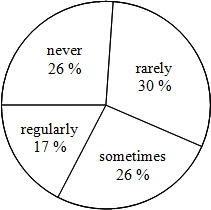
On the other hand, “Peyton’s 4 Step Approach” was rated to be the teaching method most delicate to transfer into the skills lab learning environment (3.23±1.69, table 2 (Tab. 2)). In their personal comments, most tutors which encountered difficulties in transferring Peyton’s Method reported that they did not doubt in general about the usefulness of this teaching method, but rather got a time problem in regard to the curriculum to be taught. However, when asked how often tutors used this specific method, roughly one quarter marked every of the four possible answers (see figure 1 (Fig. 1)).
Figure 1. Frequencies of the skills lab student tutors’ use of Peyton’s Method (N=23).
In the general rating about which single module was considered to be best suitable for improving the tutors’ didactic qualification, nearly half (9 out of 20) chose “How to present effectively”, five chose “How to convey practical skills effectively with Peyton’s Method”, followed by “How to explain precisely” (3 out of 20), and “How to deal with incidents” (2 of 20). One participant chose the part “How to explain on impulse”.
Discussion
In the present pilot study, the didactic course comprising five distinct modules for student tutors of technical skills lab training was very well accepted. The module “How to present effectively” was seen as most easily transferable to the skills lab environment as well as to mostly improve the student tutors’ didactic qualification. Our Competence Center of University Teaching [19] now regularly offers this didactic training twice a year for all student tutors involved in teaching practical skills at our faculty [4], [9], [22]. Although a complete day of training represents a remarkable amount of time, we appraise this expenditure as warranted in light of the number of student tutors that benefit from these courses based on the centrally organized tutor program of our faculty. It should be mentioned that in addition to this central didactic training all tutors are taught by experienced physicians in regard to their competence for the clinical skills themselves.
Interestingly, one module is discussed most controversial among our student tutors in regard to its transferability: “Peyton’s Four-Step Approach” [20]. Even if believed to improve the didactic qualification most by five of the tutors participating in our survey, only less then half the student tutors used it regularly or at least sometimes during their teaching activity in the skills lab (see figure 1 (Fig. 1)). This fraction of tutors was very positive about the method, while the others criticized especially the amount of time that is needed to teach by Peyton’s Method to a group of 4 students (general tutor:student-ratio = 1:4), especially in regard to the skills lab curriculum that has to be taught at our faculty. Hence, the use of Peyton’s Method depends strongly on the individual tutor and maybe on his or her individual teaching style. It is of note that a very recent study [25] revealed “Peyton’s Four-Step Approach” to be superior to standard instruction for teaching medical skills (gastric-tube insertion) with the same amount of teaching time. This finding let us assume that the criticized need of extra teaching time may rather reflect the students’ personal perception and not an objectifiable drawback. We therefore consider Peyton’s Method as a very effective teaching method for practical skills and as a feasible approach for PAL teaching. For this reason, this module remains included in our didactic training.
As we identified the module “How to present effectively” to improve didactic qualification most, to be most easily transferable, and to be most useful for teachers in the skill lab, we suggest including such a module in every didactic course for skills lab tutors. The usefulness of video feedback was implied by another study on peer-teaching [26] and may be partially due to the uncommon – at least for medical students – opportunity to gain an external view on the own teaching style.
We would like to point out that this report only is a descriptive study due to the limited number of participants, the retrospective design and the fact that only the students’ self-perception has been the subject of the conducted survey. However, a recent study from our faculty has shown that a combined technical and didactic training improves the acceptance of student tutors among their tutees [22]. In this study, the same didactic training modules have been used as described in this report in detail. We therefore decided to describe this training in more detail, and are convinced that our results in regard to its acceptance and efficiency are transferable to other PAL systems of other faculties.
Further randomized and prospective studies are needed to optimize the targeted training of peer tutors. These studies should also include an objective evaluation of the tutors’ didactic improvement and the students’ performance after the training.
Authors' contributions
MH analyzed the data of the survey and drafted the main parts of the manuscript. MLK designed the didactic training which now is provided to all student tutors at our faculty. She described this course in detail in the method section, and also contributed to the survey form. NC is responsible for the tutor programme in ultrasound diagnostic, TS is responsible for the corresponding PAL programme in anatomy, and RR is responsible for the student mentor programme at the ICU of our faculty. NC, TS and RR all corrected the manuscript. CN is responsible for the skills lab programme at the University of Heidelberg and contributed to both the survey design and the manuscript. PW initiated the PAL programme for skills lab tutors at our faculty and is responsible for the medical skills lab training part. He conducted the survey and contributed to both study design and drafting the manuscript.
Acknowledgements
We thank all student tutors for their great engagement and their frank feedback in our PAL program, especially Michaela Mack (MD), Melanie Adam-Callau (MD) and Nicolai Netzhammer (MD) who contributed a lot to the success of this project at its beginning.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Topping KJ. The effectiveness of peer tutoring in further and higher education: A typology and review of the literature. High Educ. 1996;32(3):321–345. doi: 10.1007/BF00138870. Available from: http://dx.doi.org/10.1007/BF00138870. [DOI] [Google Scholar]
- 2.Secomb J. A systematic review of peer teaching and learning in clinical education. J Clin Nurs. 2008;17(6):703–716. doi: 10.1111/j.1365-2702.2007.01954.x. Available from: http://dx.doi.org/10.1111/j.1365-2702.2007.01954.x. [DOI] [PubMed] [Google Scholar]
- 3.Sobral DT. Cross-year peer tutoring experience in a medical school: conditions and outcomes for student tutors. Med Educ. 2002;36(11):1064–1070. doi: 10.1046/j.1365-2923.2002.01308.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.2002.01308.x. [DOI] [PubMed] [Google Scholar]
- 4.Weyrich P, Schrauth M, Kraus B, Habermehl D, Netzhammer N, Zipfel S, Jünger J, Riessen R, Nikendei C. Undergraduate technical skills training guided by student tutors--analysis of tutors' attitudes, tutees' acceptance and learning progress in an innovative teaching model. BMC Med Educ. 2008;8:18. doi: 10.1186/1472-6920-8-18. Available from: http://dx.doi.org/10.1186/1472-6920-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lynagh M, Burton R, Sanson-Fisher R. A systematic review of medical skills laboratory training: where to from here? Med Educ. 2007;41(9):879–887. doi: 10.1111/j.1365-2923.2007.02821.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2007.02821.x. [DOI] [PubMed] [Google Scholar]
- 6.Issenberg SB, McGaghie WC, Petrusa ER, Lee GD, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. Available from: http://dx.doi.org/10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 7.Nestel D, Kidd J. Peer assisted learning in patient-centred interviewing: the impact on student tutors. Med Teach. 2005;27(5):439–444. doi: 10.1080/01421590500086813. Available from: http://dx.doi.org/10.1080/01421590500086813. [DOI] [PubMed] [Google Scholar]
- 8.Weyrich P, Celebi N, Schrauth M, Moltner A, Lammerding-Koppel M, Nikendei C. Peer-assisted versus faculty staff-led skills laboratory training: a randomised controlled trial. Med Educ. 2009;43(2):113–120. doi: 10.1111/j.1365-2923.2008.03252.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2008.03252.x. [DOI] [PubMed] [Google Scholar]
- 9.Celebi N, Zwirner K, Lischner U, Bauder M, Ditthard K, Schurger S, Riessen R, Engel C, Balletshofer B, Weyrich P. Student Tutors Are Able to Teach Basic Sonographic Anatomy Effectively - a Prospective Randomized Controlled Trial. Ultraschall Med. 2010 doi: 10.1055/s-0029-1245837. [DOI] [PubMed] [Google Scholar]
- 10.Knobe M, Munker R, Sellei RM, Holschen M, Mooij SC, Schmidt-Rohlfing B, Niethard FU, Pape HC. Peer teaching: a randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ. 2010;44(2):148–155. doi: 10.1111/j.1365-2923.2009.03557.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2009.03557.x. [DOI] [PubMed] [Google Scholar]
- 11.Haist SA, Wilson JF, Fosson SE, Brigham NL. Are fourth-year medical students effective teachers of the physical examination to first-year medical students? J Gen Intern Med. 1997;12(3):177–181. doi: 10.1007/s11606-006-5026-4. Available from: http://dx.doi.org/10.1007/s11606-006-5026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pasquinelli LM, Greenberg LW. A review of medical school programs that train medical students as teachers (MED-SATS) Teach Learn Med. 2008;20(1):73–81. doi: 10.1080/10401330701798337. Available from: http://dx.doi.org/10.1080/10401330701798337. [DOI] [PubMed] [Google Scholar]
- 13.Dolmans DH, Wolfhagen IH. Complex interactions between tutor performance, tutorial group productivity and the effectiveness of PBL units as perceived by students. Adv Health Sci Educ Theory Pract. 2005;10(3):253–261. doi: 10.1007/s10459-005-0665-5. Available from: http://dx.doi.org/10.1007/s10459-005-0665-5. [DOI] [PubMed] [Google Scholar]
- 14.Morrison EH, Hafler JP. Yesterday a learner, today a teacher too: residents as teachers in 2000. Pediatrics. 2000;105(1 Pt 3):238–241. [PubMed] [Google Scholar]
- 15.Griffith CH, III, Wilson JF, Haist SA, Ramsbottom-Lucier M. Do students who work with better housestaff in their medicine clerkships learn more? Acad Med. 1998;73(10 Suppl):S57–S59. doi: 10.1097/00001888-199810000-00045. Available from: http://dx.doi.org/10.1097/00001888-199810000-00045. [DOI] [PubMed] [Google Scholar]
- 16.Paiva RE, Kienzler LM, Anderson MB. Preparation for the teaching role in residencies: an elective for medical students. J Med Educ. 1982;57(10 Pt 1):792–794. doi: 10.1097/00001888-198210000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Pasquale SJ, Pugnaire MP. Preparing medical students to teach. Acad Med. 2002;77(11):1175–1176. doi: 10.1097/00001888-200211000-00046. Available from: http://dx.doi.org/10.1097/00001888-200211000-00046. [DOI] [PubMed] [Google Scholar]
- 18.Greenberg LW, Jewett LS. Preparing medical students to teach: an educational program using three approaches. Med Teach. 1987;9(4):409–414. doi: 10.3109/01421598709008335. Available from: http://dx.doi.org/10.3109/01421598709008335. [DOI] [PubMed] [Google Scholar]
- 19.Lammerding-Koppel M. The Competence Centre for University Teaching in Medicine Baden Württemberg 2001-2005. GMS Z Med Ausbild. 2006;23(1):Doc15. Available from: http://www.egms.de/static/de/journals/zma/2006-23/zma000234.shtml. [Google Scholar]
- 20.Peyton J. The learning cycle. In: Peyton J, editor. Teaching and learning in medical practice. Rickmansworth, UK: Manticore Europe Limited; 1998. pp. 13–19. [Google Scholar]
- 21.Shiozawa T, Hirt B, Celebi N, Werner A, Weyrich P, Lammerding-Koeppel M. Does a combined technical and didactical training program improve the acceptance of student tutors in the dissection course? A prospective controlled randomized study. Ann Anat. 2010;192(6):361–365. doi: 10.1016/j.aanat.2010.09.006. Available from: http://dx.doi.org/10.1016/j.aanat.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Shiozawa T, Hirt B, Celebi N, Baur F, Weyrich P, Lammerding-Koppel M. Development and implementation of a technical and didactical training program for student tutors in the dissection course. Ann Anat. 2010;192(6):355–360. doi: 10.1016/j.aanat.2010.09.003. Available from: http://dx.doi.org/10.1016/j.aanat.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Perlberg A, Peri JN, Weinreb M, Nitzan E, Shimron J. Microteaching and videotape recordings: a new approach to improving teaching. J Med Educ. 1972;47(1):43–50. [PubMed] [Google Scholar]
- 24.Papinczak T, Tunny T, Young L. Conducting the symphony: a qualitative study of facilitation in problem-based learning tutorials. Med Educ. 2009;43(4):377–383. doi: 10.1111/j.1365-2923.2009.03293.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2009.03293.x. [DOI] [PubMed] [Google Scholar]
- 25.Krautter M, Weyrich P, Schultz HJ, Buss SJ, Maatouk I, Jünger J, Nikendei C. Effects of Peyton's Four-Step Approach on objective performance measures in technical-skills training - a controlled trial. Teach Learn Med. 2011;23(3):244–250. doi: 10.1080/10401334.2011.586917. Available from: http://dx.doi.org/10.1080/10401334.2011.586917. [DOI] [PubMed] [Google Scholar]
- 26.Field M, Burke J, Lloyd D, McAllister D. Peer-assisted learning in clinical examination. Lancet. 2004;363(9407):490–491. doi: 10.1016/S0140-6736(04)15501-3. Available from: http://dx.doi.org/10.1016/S0140-6736(04)15501-3. [DOI] [PubMed] [Google Scholar]


