Abstract
Background: Following recent modifications of the Medical Licensure Act (ÄApprO) in the year 2009, palliative care was introduced as a compulsory 13th cross-disciplinary subject (Q13) in the undergraduate curriculum. Its implementation must have taken place before the beginning of the final year (´practical year´) in August 2013 and has to be substantiated for the medical exams taking place in October 2014.
Very diverse structures pertaining to palliative care teaching were described in previous surveys at various medical faculties in Germany. As a result, the current and future plans and concepts related to content and exams of a mandatory Q13 course at the respective faculty sites should be ascertained.
Methods: Since 2006, the German Medical Students' Association (bvmd) has been carrying out a bi-annual survey at all medical faculties in Germany regarding the current situation of teaching in the field of palliative care.
After designing and piloting an online survey in May 2010, a one-month online survey took place. The data was assessed using a descriptive approach.
Results: 31 of 36 medical faculties took part in the survey. At the time of questioning, 15 faculties already taught courses according to the requirements of the new ÄApprO; at three sites the Q13 is yet to be introduced commencing in 2012. A teaching curriculum for Q13 already existed at 15 faculty sites, partly based on the curricular requirements of the German Association for Palliative Medicine (DGP). Six sites described an implementation process as yet without an independent curriculum. Most of the faculties aim for 21-40 course hours, which will for the most part be provided as lectures, seminars or less often in more assisted and intense formats.
The majority of the participating faculties intend an examination containing multiple choice questions. At 8 universities there is an independent Chair for palliative medicine (5 more are planned); this was linked with a higher degree of mandatory teaching in alignment with the requirements of the ÄApprO. A broad spectrum of educationally-involved occupational groups, specialist disciplines and external co-operating partners, were mentioned.
Conclusion: The infrastructural prerequisites of the present curricular concepts and the degree of implementation of the Q13 according to the requirements of the new ÄApprO diverge significantly among the various medical faculties. The efforts made to produce a qualitatively high standard of teaching with regard to the multifaceted questions concerning the support for severely and terminally ill patients is as much reflected in the survey, as the special implications of an independent Chair for palliative medicine for the implementation of the requirements by law. The participation of various occupational groups in this survey as well as the broad spectrum of those involved highlights the interdisciplinary and multi-professional dimension of teaching in palliative care.
Keywords: Palliative care, cross-disciplinary subject, implementation process, curriculum, examinational didactics
Abstract
Fragestellung: Mit der Änderung der ärztlichen Approbationsordnung (ÄApprO) im Jahre 2009 wurde die Palliativmedizin als 13. Querschnittsfach (Q13) verpflichtend in das studentische Curriculum eingeführt. Die Umsetzung dieser Änderung muss bis zum Beginn des Praktischen Jahres im August 2013 oder bei der Meldung zum Zweiten Abschnitt der Ärztlichen Prüfung für den Prüfungstermin im Oktober 2014 erfolgen.
In vorangegangenen Umfragen wurden an den medizinischen Fakultäten in Deutschland sehr heterogene palliativmedizinische Lehrstrukturen beschrieben. Daher sollten nun die curricularen und prüfungsbezogenen Planungen der jeweiligen Fakultäten zur Implementierung eines verpflichtenden Q13 Palliativmedizin erfragt werden.
Methodik: Die Bundesvertretung der Medizinstudierenden Deutschlands (bvmd) führt seit 2006 zweijährliche Umfragen an allen medizinischen Fakultäten in Deutschland zum gegenwärtigen Stand der palliativmedizinischen Lehre durch.
Nach Konzeption eines Online-Fragebogens und Pilotierung erfolgte im Mai 2010 eine einmonatige Online-Umfrage. Die Daten wurden deskriptiv ausgewertet.
Ergebnisse: 31 von 36 medizinischen Fakultäten nahmen an der Befragung teil. An 15 Fakultäten existierten zum Befragungszeitpunkt bereits verpflichtende Lehrveranstaltungen entsprechend der Vorgabe der neuen ÄApprO; an drei Standorten soll das Q13 Palliativmedizin erst ab dem Sommersemester 2012 verpflichtend eingeführt werden. An 15 Fakultäten bestand bereits ein Lehrcurriculum für Q13, teils angelehnt an die curricularen Vorgaben der Deutschen Gesellschaft für Palliativmedizin. Sechs Standorte beschrieben einen begonnenen Implementierungsprozess noch ohne Curriculum. An den meisten Fakultäten werden 21-40 Lehrveranstaltungsstunden angestrebt, die überwiegend in Form von Vorlesungen oder Seminaren, seltener auch in betreuungsintensiveren Formaten angeboten werden sollen. Die Mehrzahl der teilnehmenden Fakultäten strebt eine Prüfung in Form von Multiple Choice Fragen an. An 8 Universitäten bestand ein eigenständiger Lehrstuhl für Palliativmedizin (5 weitere in Planung); dies war mit einem höheren Maß an Pflichtlehre analog der Vorgabe der ÄApprO verbunden. Ein breites Spektrum an lehrbeteiligten Berufsgruppen, Fachdisziplinen und externen Kooperationspartnern wurde angegeben.
Schlussfolgerung: Die infrastrukturellen Voraussetzungen, die bisherigen curricularen Planungen und der Grad der Implementierung des Q13 analog der Vorgabe der neuen ÄApprO divergieren zwischen den einzelnen medizinischen Fakultäten erheblich. Die Bemühungen um eine qualitativ hochwertige Lehre in Hinblick auf die vielschichtigen Fragestellungen bei der Betreuung schwerst- und sterbenskranker Patienten spiegeln sich in der Umfrage ebenso wider wie der besondere Stellenwert eines eigenständigen Lehrstuhls für Palliativmedizin für die Umsetzung der gesetzlichen Vorgaben. Die Mitwirkung der verschiedenen Berufsverbände an dieser Umfrage sowie das große Spektrum der Lehrbeteiligten unterstreicht die interdisziplinäre und multiprofessionelle Dimension palliativmedizinischer Lehre.
Introduction
In the course of revising the Medical Licensure Act (ÄApprO; 07/2009), palliative care as the care of severely and terminally ill patients was incorporated as a 13th cross-disciplinary (Q13) subject in the mandatory undergraduate curriculum. Providing proof of teaching in the subject of palliative care will be obligatory starting from the beginning of the final year (´practical year´) in August 2013, i.e. at the latest by the time of registering for the second part of the medical examination in October 2014. At present, the German faculties are facing the challenge of implementing appropriate teaching structures by that point in time, given that only 6 universities offered a mandatory course in palliative care in 2008 [1].
The formal conditions with respect to the the implementation as well as the curricular context were described in detail elsewhere [2], [3], [4], [5], [6], [7].
In context of the bi-annual surveys of the German Medical Students' Association (Bundesvertretung der Medizinstudierenden in Deutschland e.V., bvmd), conducted for the first time in 2006 and last amended in the year 2008 [1], very diverse teaching concepts in palliative care - ranging from a complete, mandatory curriculum with graded exams to no teaching at all in an explicit palliative care context - became evident.
As a result it becomes apparent that the medical faculties will begin or continue the implementation process for the new teaching subject under very different starting conditions. Accordingly, the formal implementation of Q13 as a compulsory subject within the required implementation deadline will be a substantial challenge for individual faculties in view of structural and particularly content-related questions which may arise.
The aim was not only to bring transparency to the present implementation process, but also to support those faculties with less didactical experiences with respect to teaching and examining palliative care contents. Therefore, the bvmd survey of 2010 - approximately half a year after the revision of the Medical Licensure Act - thoroughly questioned the current situation of palliative care teaching as well as the conceptual planning and future development of the respective faculties.
These concepts and developments should be the focus of this contribution.
Methods
Since 2006 the bvmd conducts a bi-annual survey of all medical faculties in Germany with respect to the current state of teaching in palliative care. Based on an online questionnaire used by the bvmd in the year 2008 in order to evaluate the current state of palliative care teaching, an expanded version of this questionnaire was developed that aims to compile conceptual and structural as well as curricular and examination-related plans and future developments at the respective faculties.
Apart from the bvmd as project manager, different professional associations cooperated in this survey (German Association for Palliative Medicine DGP, German Association for Haematology and Oncology DGHO, German Cancer Society DKG, and German Association for the Study of Pain DGSS). The questionnaire was piloted at the universities of Munich LMU (n=4), Göttingen (n=10) and Jena (n=8), and was uploaded online for one month (HTML- document) with an inviting cover letter to all faculties, starting on 01.05.2010.
In the case of non-response, the respective Deanery was contacted by telephone.
The data was assessed using a PHP script exported in SPSS.
The survey comprised general information regarding the faculty and teaching structures, extended questions regarding the implementation of the Q13 requirements, the scope of the course, the curricular content, the didactics and examinations, the inclusion of students in planning, the presence or planned establishment of a Chair or professorship, the qualification of the person in charge of palliative care teaching, the participating medical disciplines and external co-operating partners.
Selected results of this publication were presented at the congress of the European Association for Palliative Care (EAPC) in 2011 [8], and at the congress of the DGP in 2010 [9].
Results
Response rate
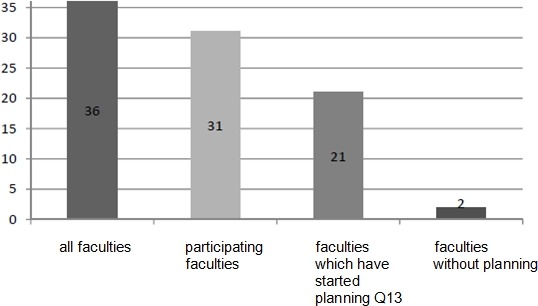
The response rate was 86% (31 of 36 faculties).
Status of implementation
Prior steps in the implementation of the palliative care as a mandatory subject were described at 21 sites. In the current survey 2010, two of the 31 participating faculties reported to have no teaching activities so far with respect to palliative care (see figure 1 (Fig. 1)).
Figure 1. Participating faculties and status of implementation.
Timing
The majority of faculties aim to introduce the Q13 as a compulsory subject as of the summer semester 2011; at three faculties this is due to take place as of the summer semester 2012, a year before the latest possible date.
Curriculum
15 faculties reported to rely on a teaching curriculum; at seven sites, the curricular content is being based on the DGP and the EAPC recommendations. Eight faculties reported to already have compiled an independent curriculum. Despite having commenced the implementation process, six faculty sites do not have a comprehensive curriculum yet. 10 of the 31 responding faculties did not provide information regarding the presence of a curriculum for palliative care teaching.
7 faculties reported to have drawn upon a catalogue of learning objectives.
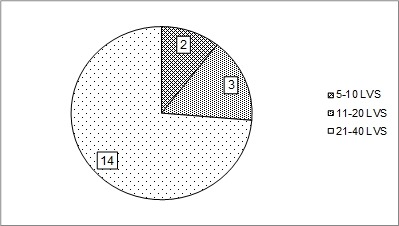
14 faculties aim to provide 21-40 course hours (Lehrveranstaltungsstunden, LVS); 3 faculties aim for 11-20 LVS, and at 2 faculties merely 5-10 LVS are intended (see figure 2 (Fig. 2)). 12 faculties provided no information. In contrast, the DGP recommends – in line with the European Standards – up to 40 LVS. “A range of 20 course units under the direct leadership of a palliative care department i.e. of a corresponding Chair should however not be undercut” [6].
Figure 2. Distribution of the faculties based on their LVS aim for Q13 (n = 19).
Didactics
17 faculties responded regarding this issue (multiple answers permitted). Intended teaching methods include:
lectures (at 16 of 17 sites)
seminars (16 of 17)
case discussions (14 of 17)
bedside teaching (13 of 17)
teaching with simulated patients (8 of 17)
e-learning (6 of 17)
Examinations
17 faculties responded regarding this issue (multiple answers permitted). Intended teaching methods include:
multiple-choice questions (11)
oral examinations (8)
OSCE (4)
homework (3)
Students
At 18 of 31 faculty sites students are being involved in the implementation process.
Main responsibility
At the time of recording, an independent Chair for palliative medicine existed at the eight universities Aachen, Bonn, Erlangen, Göttingen, Cologne, Munich LMU (with the associated endowed professorships paediatric palliative care, social work in palliative care, and spiritual care), Mainz, and Witten / Herdecke (with the Chair for paediatric palliative care and paediatric pain therapy).
In addition, six further faculties (Freiburg, Homburg, Jena, Lübeck, Rostock and Tübingen) reported that they are taking concrete steps in the planning of a Chair for palliative medicine.
Statements were made by 19 faculties regarding the qualification of the respective person in charge (multiple answers possible):
specialization in the field of palliative care, at 10 sites
specialization in the field of palliative care with more than two years of clinical experience in palliative care, at 15 sites
teaching experiences in palliative care, at 9 sites
structured postgraduate qualification, at 11 sites.
At two sites, no special qualification requirements were demanded.
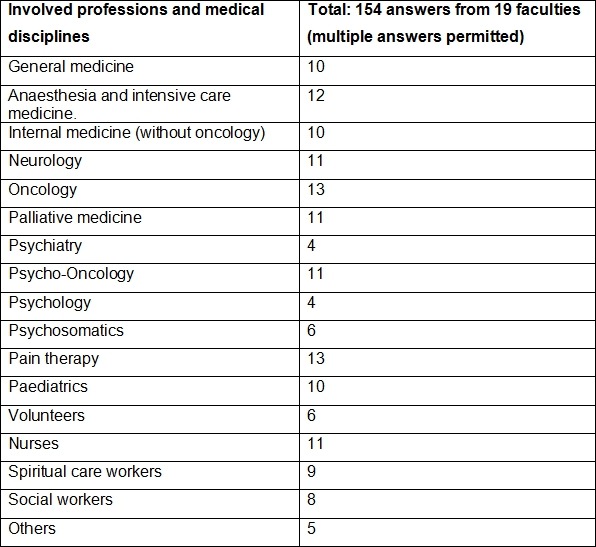
Participating professions and medical disciplines
19 faculties responded regarding this issue (multiple answers permitted, see table 1 (Tab. 1)):
Table 1. Involved professions.
External co-operating partners
17 faculties responded, concerning questions pertaining to external co-operating partners (multiple answers permitted). Co-operations are made particularly with specialized outpatient palliative care teams (SAPV; n=13), outpatient hospice services (n=11), inpatient hospices (n=10), general practitioners (n=9) or other hospitals (n=8), but also with medical specialists (n=5), other faculties (n=4) or other institutions (n=2).
Implementation of teaching dependent upon the existence of a Chair
Six of the eight faculties that by now have an established Chair in palliative medicine stated they have already implemented compulsory courses in palliative care. On the other hand, only nine of the remaining 23 participating faculties without a Chair provide compulsory courses. Thus, the degree of commitment is significantly higher at sites with an independent Chair.
Discussion
By expanding the bi-annual survey of the bvmd, that describes the current state of palliative care teaching in Germany, and by ascertaining the plans of the German medical faculties with respect to Q13 implementation, the various ideas and curricular concepts at the medical faculties should be made more transparent.
The 2010 survey confirmed the different “starting positions” of the various faculty sites – ranging from faculties with a complete organisational and curricular infrastructure to those faculties without any form of specific palliative care teaching.
On the other hand, the variety of implementation requirements also mirrors the different teaching intensities that are intended: quantitatively, in terms of course hours (LVS), as well as qualitatively, in terms of the teaching formats.
As such, the faculties have specified that lectures and seminars will be the main format of teaching; however, bedside-teaching, simulated patient training and other, more elaborate teaching formats will also be offered.
Similarly, most of the faculties that responded planned to use multiple choice questions as the preferred format of examination; however, some faculties intended to use more elaborate, partly oral or practical, examinations. With respect to the selected teaching and examination formats, the question arises whether a subject that does not only aim to convey specialised knowledge but also intends to convey a therapeutic attitude of empathy towards severely and terminally ill patients, should rely predominantly on lectures i.e. respective multiple choice questions [10], [11], [12]. In view of the organisational and structural demands resulting from the new legal requirements, it might to be expected that many faculties may employ more general teaching and examination formats as a temporary solution.
However, more individualistic, differentiated and authentic - but more extensive and mentoring teaching and examination formats would be desirable.
By aspiring more complex teaching and examination formats, the necessity for labelling a clear, coordinating responsibility, ideally in the form of an independent Chair for the subject of palliative medicine, becomes evident. Particularly in light of the results of our survey regarding the degree of responsibility, it can be surmised that the presence of a Chair is likely to be the main force for the implementation of the legal requirements of undergraduate palliative care teaching.
It is encouraging, though, that a high percentage (58%) of faculties reported to involve students in the implementation process. This should not only be deemed as a good starting position for constructive teamwork between teachers and students, but may also be interpreted as a sign of considerable interest of students regarding palliative care issues.
The variety of co-operating occupational groups and specialist disciplines that were found in our survey mirrors the multifaceted and multi-professional aspect of palliative care. It also serves however to emphasise the great complexity in the coordination of student teaching in Q13.
This study presents a range of limitations. Only 31 of 36 faculties took part in the survey, despite being repeatedly contacted by telephone, and despite extensive support of the project by those medical associations that share responsibility for palliative care.
A majority of the questions that regard the future planning of the faculties was answered by merely 17-19 of the participating faculties. Methodological problems such as the absence of mandatory fields, as well as content-related aspects such as the absence of well-defined curricular contents or examinations, could contribute in the sense of a negative response. As a result, fully representative statements cannot be made based on the present study, for instance with respect to curricular contents, details of teaching methods or examinations. At most, tendencies can be formulated.
Moreover, in this publication the term “Chair” was used in a common, non-juridical understanding of a university-based leading position, implying distinct tasks in teaching and education, research and patient care. It does not take into account the subtle nuances of the respective professorships, even though the degree of independence of a professorship might have an influence on the positioning of palliative care at a university setting.
Moreover, this survey could not make any statements regarding the quality of teaching in palliative care but could only describe organisational and structural aspects and objectives related to curriculum and teaching and examination didactics.
Nevertheless, this study can contribute impulses and ideas to the implementation of palliative care teaching, given the requirements for implementing the cross-disciplinary subject Q13, and might therefore contribute to a transparent, uniform and future-oriented implementation process in Germany.
Note
B. Ilse and J. Hildebrandt contributed equally to the publication.
A project of the federal representation of medical students in Germany (bvmd) and the German Association for Palliative Medicine (DGP), in co-operation with the German Association for Haematology and Oncology (DGHO), the German Cancer Society (DKG) and the German Association for the Study of Pain (DGSS)
Acknowledgement
With genuine thanks to Mrs. Kristina Kluziok for her programming work and to Mrs. Reena Rick for translating the manuscript.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Laske A, Dietz I, Ilse B, Nauck F, Elsner F. Palliativmedizinische Lehre in Deutschland – Bestandsaufnahme an den medizinischen Fakultäten 2009. Z Palliativmed. 2010;11:18–25. doi: 10.1055/s-0029-1223482. Available from: http://dx.doi.org/10.1055/s-0029-1223482. [DOI] [Google Scholar]
- 2.Alt-Epping B, Jung W, Simmenroth-Nayda A, Russo SG, Vormfelde SV, Nauck F. Implementierung des Querschnittsfachs Palliativmedizin (Q13) vor dem Hintergrund der neuen gesetzlichen Rahmenbedingungen am Beispiel der Universitätsmedizin Göttingen. GMS Z Med Ausbild. 2010;27(5):Doc67. doi: 10.3205/zma000704. Available from: http://dx.doi.org/10.3205/zma000704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Becker G, Momm F, Gigl A, Wagner B, Baumgartner J. Competency and educational needs in palliative care. Wien Klin Wochenschr. 2007;119(3-4):112–116. doi: 10.1007/s00508-006-0724-9. Available from: http://dx.doi.org/10.1007/s00508-006-0724-9. [DOI] [PubMed] [Google Scholar]
- 4.Borasio GD, Dietz I, Elsner F, Hildebrandt J, Ilse B, Schiessl C. Münchner Erklärung. Z Palliativmed. 2010;2:45–48. [Google Scholar]
- 5.Deutsche Gesellschaft für Palliativmedizin. Stellungnahme zur Einrichtung von Lehrstühlen für Palliativmedizin an den medizinischen Fakultäten vom 10. Berlin: Deutsche Gesellschaft für Palliativmedizin; 2009. Available from: http://www.dgpalliativmedizin.de/images/stories/pdf/sn/SN%20090210%20DGP%20Lehrstuehle.pdf. [Google Scholar]
- 6.Elsner F, Fittkau-Toennesmann B, Schiessl C. Curriculum: Grundlagen der Palliativmedizin. Gegenstandskatalog und Lernziele für Studierende der Medizin. 2. überarbeitete Fassung 2009. Berllin: Deutsche Gesellschaft für Palliativmedizin; 2009. Available from: http://palliativmedizin.klinikum.uni-muenchen.de/docs/workshop/AG_AFW_CurriculumStudierendeElsnerStand_090810.pdf. [Google Scholar]
- 7.Wasner M, Roser T, Fittkau-Tönnesmann B, Borasio GD. Palliativmedizin im Studium: Spiritualität und psychosoziale Begleitung als wichtige Lehrinhalte. Dtsch Ärztebl. 2008;105:A674–A676. [Google Scholar]
- 8.Hildebrandt J, Ilse B, Borasio GD, Dietz I, Elsner F, Kopf A, Laske A, Nauck F, Posselt J, Wedding U, Alt-Epping B. Palliative Care in Undergraduate Teaching in Germany: Development since 2006 and Current Status Report. Congress of the European Association for Palliative Care; 2011; Lisabon. p. Abstract P642. Available from: http://bvmd.de/fileadmin/PALLIATIV/EAPC18052011_Version_final.pdf. [Google Scholar]
- 9.Ilse B, Hildebrandt J, Borasio GD, Dietz I, Elsner F, Kopf A, Laske A, Nauck F, Posselt J, Wedding U, Alt-Epping B. Palliativmedizinische Lehre in Deutschland - Bestandsaufnahme an den medizinischen Fakultäten 2010. Kongress der Deutschen Gesellschaft für Palliativmedizin. Z Palliativmed. 2010;11:P123. [Google Scholar]
- 10.Gibbins J, McCoubrie R, Forbes K. Why are newly qualified doctors unprepared to care for patients at the end of life? Med Educ. 2011;45(4):389–399. doi: 10.1111/j.1365-2923.2010.03873.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2010.03873.x. [DOI] [PubMed] [Google Scholar]
- 11.Gibbins J, McCoubrie R, Maher J, Wee B, Forbes K. Recognizing that it is part and parcel of what they do: teaching palliative care to medical students in the UK. Palliat Med. 2010;24(3):299–305. doi: 10.1177/0269216309356029. Available from: http://dx.doi.org/10.1177/0269216309356029. [DOI] [PubMed] [Google Scholar]
- 12.Lloyd-Williams M, MacLeod RD. A systematic review of teaching and learning in palliative care within the medical undergraduate curriculum. Med Teach. 2004;26(8):683–690. doi: 10.1080/01421590400019575. Available from: http://dx.doi.org/10.1080/01421590400019575. [DOI] [PubMed] [Google Scholar]


