Abstract
Objectives
Despite substantial evidence supporting the efficacy of stimulant medication for children with attention-deficit/hyperactivity disorder (ADHD), adherence to stimulant treatment is often suboptimal. Applying social/cognitive theories to understanding and assessing parent attitudes toward initiating medication may provide insight into factors influencing parent decisions to follow ADHD treatment recommendations. This report describes results from formative research that used focus groups to obtain parent input to guide development of a provider-delivered intervention to improve adherence to stimulants.
Methods
Participants were caregivers of children with ADHD who were given a stimulant treatment recommendation. Focus groups were recorded and transcribed verbatim. Data were analyzed by inductive, grounded theory methods as well as a deductive analytic strategy using an adapted version of the Unified Theory of Behavior Change to organize and understand parent accounts.
Results
Five groups were conducted with 27 parents (mean child age=9.35 years; standard deviation [SD]=2.00), mean time since diagnosis=3.33 years (SD=2.47). Most parents (81.5%) had pursued stimulant treatment. Inductive analysis revealed 17 attitudes facilitating adherence and 25 barriers. Facilitators included parent beliefs that medication treatment resulted in multiple functional gains and that treatment was imperative for their children's safety. Barriers included fears of personality changes and medication side effects. Complex patterns of parent adherence to medication regimens were also identified, as well as preferences for psychiatrists who were diagnostically expert, gave psychoeducation using multiple modalities, and used a chronic illness metaphor to explain ADHD. Theory-based analyses revealed conflicting expectancies about treatment risks and benefits, significant family pressures to avoid medication, guilt and concern that their children required medication, and distorted ideas about treatment risks. Parents, however, took pride in successfully pursuing efforts to manage their child behaviorally and to avoid medication when possible.
Conclusions
Focus group data identified social, cognitive, and affective influences on treatment decision making. Results support prior research comparing family/social functioning, physician characteristics, and adherence. Findings suggest that parent attitudes to psychiatric care need to be assessed comprehensively at initial evaluation to aid the development of psychoeducational messages, and a more careful consideration about how parents interpret and respond to adherence-related questioning.
Introduction
Treating the symptoms of attention-deficit/hyperactivity disorder (ADHD) with stimulant medication has been designated a best practice by experts in child psychiatry and pediatrics (Pliszka 2007) and has been documented by research to be generally safe and efficacious (MTA Cooperative Group 1999). Research data on the short-term and extended benefits of sustained stimulant use on core ADHD symptoms are extensive (see Conners 2002; Jensen 2002). The effects of stimulants on functional outcomes are more equivocal, and often moderated by the presence of co-morbid learning disabilities and other psychiatric diagnoses. However, some research suggests that stimulant treatment is associated with higher levels of academic performance (Powers et al. 2008; Marcus and Durkin 2011). Stimulant treatment may also facilitate improved family interactions (Gustafsson et al. 2008), and may protect against later substance use disorders (Katusic et al. 2005). A recent review also suggests that there is some empirical support for the positive benefits of medication treatment on children's quality of life (Coghill 2010).
Despite expert recommendations and supportive empirical evidence, adherence to stimulant treatment recommendations in children with ADHD remains low (Sanchez et al. 2005). One recent review reported nonadherence ranging from 13% to 64% (Adler and Nierenberg 2010). These identified rates appear highly dependent on the source of information and researcher-determined definitions of adequate adherence; yet, adherence is identified as less than optimal even in highly structured clinical trials (Pappadopulos et al. 2009).
Research investigations that examine unitary rates of adherence mask the complex and dynamic nature of following treatment recommendations. Investigating adherence to medication should attend to the different types of decisions that occur over time, and the range of adherence behaviors that result (Charach and Gajaria 2008; Gearing et al. 2011). Such a line of inquiry would begin with the initial step in treatment adherence, which is deciding whether to follow a medical provider's treatment recommendation. A clinician who recommends a treatment plan that includes a stimulant trial does so in the context of evidence suggesting that parents often do not pursue such treatment. A Medicaid database report indicated that approximately half of newly diagnosed youth with ADHD do not initiate stimulant treatment, and half of those who do begin treatment discontinue it within a year (Winterstein et al. 2008). Similarly, adherence to stimulants has been shown to decline over time in clinical trial participants, regardless of dosing or type of supportive services (Jensen et al. 2007).
Understanding why families of children diagnosed with ADHD depart from stimulant treatment recommendations requires further research. Parent attitudes toward ADHD treatment exist in the societal context of significant ambivalence about psychiatric conceptualizations of children's mental health, and about behavioral problems related to the ADHD syndrome in particular (Pescosolido et al. 2008). Key influences on decision making about medication options include the health-related attitudes parents bring into their encounter with the recommending medical provider. Parent attitudes toward stimulant treatment have been documented as fraught with ambivalence, in which expectations about symptomatic and functional improvements typically coexist with concerns about short- and longer-term negative effects (Hansen and Hansen 2006; Brinkman et al. 2009). In addition, while parent satisfaction with stimulant treatment response may be associated with higher rates of adherence (Faraone et al. 2007), negative attitudes about the acceptability of medication as a treatment for ADHD persist in the face of scientific evidence, and even despite positive personal experiences with medication (Johnston et al. 2008). Closing the gap between negative parental attitudes and treatment acceptance is crucial given the known negative outcomes associated with untreated ADHD. There is a need to develop interventions that educate, encourage, and support families in following stimulant treatment recommendations. These interventions would also need to explore and address parental discomfort with medication in ways that facilitate treatment follow-through.
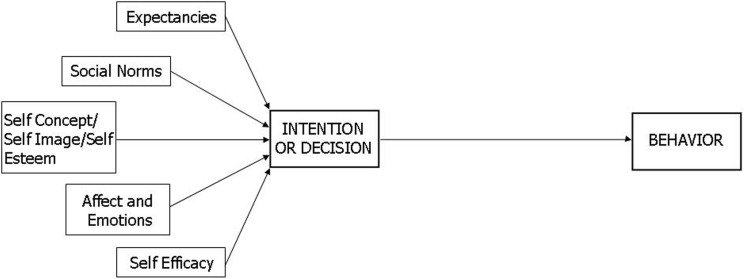
Recent years have seen theory-driven descriptions of the interrelationships between attitudes, skills, and environmental determinants to explain adherence-related behaviors (Charach et al. 2008; Hamrin et al. 2010). The Unified Theory of Behavior Change (UTBC) illustrates a full range of social, cognitive, and environmental influences on adherence (Fishbein et al. 2001), and adaptations of this model have been useful in research on health communication between parents and children (Jaccard et al. 2002; Guilamo-Ramos et al. 2008). This adapted model posits five core variables—expectancies, affect, self-efficacy, self-image, and social norms—that are hypothesized to determine the intention to engage in a health-related behavior, such as the decision to initiate a stimulant trial for a child (see Fig. 1). Expectancies are the positive and negative attitudes about the costs and benefits of initiating medication, with the supposition that attitudes will be favorable when low negative expectancies coexist with high positive expectancies. Affect may delay or facilitate the decision to try medication, and may depend on the strength of the arousal engendered as well as whether the emotions are experienced as positive (hopeful, relieved, etc.) or negative (fearful, sad, etc.). Efficacy beliefs refer to a parent's perceived ability to make a good decision about whether to engage in a medication trial, as well as their confidence level to engage in the process of evaluation, treatment, and parenting a child with ADHD. Parents' self-image may influence a medication decision to the degree to which seeking medical assistance and accepting a medication recommendation are consistent with their image of themselves as a person and parent. Finally, decision making about stimulant medication occurs in the context of social norms or attitudes—more specifically, the parent's experience of the attitudes and beliefs of others—in their immediate environment (partners, families, friends, etc.), as well as the larger community (teachers, other parents, cultural groups, etc.).
FIG. 1.
Determinants of behavioral intentions: Adapted Unified Theory of Behavior Change (Guilamo-Ramos et al. 2008).
The UTBC has been presented as a particularly salient conceptualization of ADHD treatment decision making because of the multiple ways it might guide behaviorally based interventions (Chacko et al. 2010). The initial interactions with the recommending medical provider represent an important opportunity to address parent attitudes, fears, and beliefs about ADHD, about parenting a child with ADHD, and about psychotropic medication. Research in pediatrics has documented a strong association between medical provider characteristics and parent acceptance of treatment recommendations in general (Francis et al. 1969), and for psychosocial problems in particular (Hart et al. 2007). Specific characteristics of pediatricians' practices, including providing adequate time and demonstrating expertise, were shown in one study to be associated with parent acceptance of ADHD recommendations (Concannon and Tang 2005). In the field of child psychiatry, however, a recent report documented relatively low levels of perceived competency among prescribing professionals, and identified inadequate communication as a key barrier to effective assessment and intervention of ADHD (Brown et al. 2011). Although even a brief intervention has been shown to enhance parent provider communication in primary care pediatric settings (Hart et al. 2006), we are unaware of similar interventions targeting the competencies and communication skills of child psychiatrists to address parent ideas and attitudes about their child's ADHD, and about how such an intervention might be structured.
The objective of this report is to describe results from formative research activities to obtain stakeholder input for a physician-delivered intervention targeting adherence to stimulant regimens. Medication adherence was conceptualized broadly for this exploratory study as aligned with the World Health Organization (2003) definition: “the extent to which a person's behaviour—taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health-care provider.” Specifically, we used parent focus group methods to (a) elicit parent experiences receiving an ADHD diagnosis for their child and (b) understand parental decision-making processes for accepting and persisting with stimulant treatment. These activities were guided by expectations that parent accounts would provide insight into the facilitators and barriers to stimulant adherence, and illustrate UTBC constructs to guide intervention design and implementation.
Methods
Setting
The current study was conducted in the ambulatory care child psychiatry clinic of a large Northeastern suburban teaching hospital. As a tertiary care center, this is the largest provider of outpatient child and adolescent mental health services in the region and serves a socioeconomically and culturally diverse catchment area.
Participants
Participants were parents or legal guardians of children aged 5–12 years who had received a diagnosis of ADHD by a child psychiatrist in the outpatient clinic, and a recommendation for stimulant treatment. Participants were recruited through patient records, referral by child psychiatry staff members, and through self-referral after viewing a study flyer. The subsequent formation of groups by the research team reflected a stratified purposeful strategy for parent sampling (Miles and Huberman 1994) to ensure a broad range of parent experiences. Specifically, attempts were made to construct groups combining parents who had pursued medication treatment with parents who had decided to forego medication.
Procedures
This investigation was approved by the medical center's Institutional Review Board. Parents or legal guardians who provided informed consent were asked to complete a family information form that incorporated demographic information, their child's treatment history, and assessments of adherence to prescribed medication (Coletti et al. 2005).
Focus groups were two hours in duration and led by two child psychologists with experience in focus group methodology (authors DJC and EP). Discussion was facilitated by a semistructured interview guide that allowed for open-ended responses but also ensured that participants discussed theory-driven constructs and shared experiences interacting with their children's medical providers about treatment decisions (see Appendix A). Groups were audio-taped and transcribed for subsequent analysis. Transcripts were supplemented by research staff members' written observations of group interactions.
Two strategies were utilized to analyze focus group transcripts (Fereday and Muir-Cochrane 2006). An initial strategy was to utilize a data-driven, inductive approach to transcript analysis to using grounded theory methods to allow themes to emerge independent of theory or prior hypotheses about thematic content (Strauss and Corbin 1998). Transcripts were read multiple times and segmented into meaningful units of analysis. All raters had training in a mental health discipline and clinical experience working with children and families affected by ADHD. Three of four raters were from psychology backgrounds, and one rater was a child psychiatrist. Raters examined transcripts and categorized data segments into meaningful themes. Multiple meetings among raters were held in the iterative process of content analysis, where parent accounts were successively grouped and collapsed. Weekly meetings were held to review thematic groupings. Priority was given to identify categories that would aid intervention development. Categories that remained had been discussed during two different focus groups, or were discussed at one group by three or more parents. After data analysis was complete, five group participants were presented with a list of group themes to assess their perceptions of the match between group proceedings and the organized thematic content. Two statements were modified to more closely reflect parent perceptions of the discussion.
A second analytic strategy was a deductive set of procedures to identify exemplars of preexisting data constructs; in this case, the adapted UTBC. Data coders were instructed to identify examples of aspects of the model in parent accounts. A coding manual was developed that included definitions of the constructs and multiple examples of potential parent responses that would illustrate each aspect of the theory. Four raters independently coded transcripts for examples of (1) parent expectancies regarding the advantages and disadvantages of using medication for their children; (2) evidence that parents' affective responses were influencing treatment decision making; (3) sense of self-efficacy in parenting a child with ADHD and pursuing treatment recommendations; (4) the impact of managing a child with ADHD on self-image; and (5) the influence of social norms and social pressures on parenting and treatment decision making. All transcripts were coded by at least two raters independently, and consensus meetings were held with coding teams to reconcile discrepancies.
Results
Sample
Eligible parents or guardians of 96 children with ADHD were contacted to assess willingness and availability to participate in one of the scheduled focus groups that were held over a three-month period in 2009. The 27 parent participants were 78% women, had a mean age of 45.27 years (standard deviation [SD]=11.16), and were from a socioeconomic spectrum that was largely middle to upper-middle class and reflective of the medical center's diverse catchment area (mean Hollingshead 4-factor score of 45.14, SD=10.56). Almost all (93%) were biological parents; two grandmothers who were legal guardians also participated in the groups. The identified patients (children with ADHD) were 20 boys and 7 girls; the mean age of the children at the time of parent participation was 9.35 years (SD=2.00). Almost one-third of the children (8/27 or 29.6%) had received at least one co-morbid diagnosis, including oppositional defiant disorder (n=4), an anxiety disorder (n=4), a pervasive developmental disorder (n=1), or a mood disorder (n=1). The sample was comprised largely of families who had been living with the ADHD diagnosis for some time (mean time since diagnosis=3.33 years, SD=2.47).
The majority of parents had at one time pursued recommendations for stimulant treatment (n=22, 81.5%), although each group included parents who had chosen to forego a medication recommendation or who had discontinued medication. Just over two thirds (70.3%) of the children on medication were taking stimulants, and a significant proportion were currently taking two or more medications (n=8 or 36.4%). Parent reports of their children's adherence to treatment on the written questionnaire indicated that on average, children had missed only 1.32 doses in the previous 4 weeks, and 51% reported all medication taken as prescribed during the assessment period.
Data collection was ended after it became apparent that there was a high degree of homogeneity in the thematic content of the discussion across the first five groups. The following is a description of focus group results, including particularly illustrative parent accounts.
Inductive analysis
Three themes from group transcripts had particular relevance for intervention development. They were labeled (a) defining “adherence,” (b) attitudes that promote or interfere with adherence, and (c) parent perceptions of medical providers.
Defining “adherence.”
During each group, parents' self-reported pattern of adherence to their children's medication treatments was discussed. It was interesting to note that as the topic turned to adherence, initial parent statements indicated that they had no difficulties with consistent and timely medication administration. As each discussion would continue, however, many examples were shared in which medication was not given as prescribed. While parents maintained self-identification as “adherent” parents, further discussion elicited significant variability in the degree to which they (a) consistently ensured that medication was given as prescribed, (b) understood appropriate timing of doses, and (c) grasped the impact of missing doses of stimulant or adjunctive nonstimulant medications (e.g., the parent of a child on stimulant/alpha agonist combination therapy who would abruptly stop both medications on weekends).
“The doctor recommended a specific time, but our daily activities are altered every day…like tonight he'll take it at 7:30. [On another night] I wouldn't give it to him until I know he's ready for bed.”
“We broke open the capsule…[and] by the end of the day when he came home from school he was melting down. So we thought the medication didn't work, but then…the pharmacist said you can't open it—the XR is gone. By that time we'd already taken him off of it.”
For example, while one father initially stated that “medicine is not negotiable so he is never not on it,” he later clarified that “if we truly have nothing to do that day and nothing is going on, we'll give him a lower dose.” A grandparent who initially self-identified as always ensuring that medication was administered on schedule later clarified that occasional departures from the regimen occurred but were unmentioned because they were unintended: “[he] would get distracted and accidentally not take the pill. It would never be intentional….”
Attitudes that promote or interfere with adherence
Of the 42 distinct attitudes to medication identified by two or more raters during the inductive analysis, 17 (40.5%) were categorized as facilitating adherence and 25 (59.5%) presented as potential barriers to pursuing stimulant treatment. The most prominent facilitator of adherence, described across each of the five groups, was a perception that medication for ADHD should be initiated because it was effective, and that stabilization of ADHD symptoms would lead to functional improvements beyond mere symptom relief. Functional areas mentioned included sleep, mood, academic performance, and social functioning. Parents were able to express their joy at the multiple positive outcomes that they felt had led from initiating stimulant treatment:
“You feel like [treatment] has become your friend, because you see your child happy and successful.”
“My son has gone from ‘special ed’ to ‘general ed.’ He has no problems, he's popular, he's got everything going on.”
Parent accounts suggested that, for some, medication was necessary for their children's basic well-being and safety:
“My child would not listen…. [he] would dart into traffic, try to scale fences and get himself stuck…. it became a matter of protecting him.”
“… without the medication he's just beyond control…you need a spatula to pull him off the ceiling…he cannot focus.”
In addition to concerns about children's immediate safety, parents also discussed using medication to prevent more serious issues later in life:
“If I don't attend to this issue with the impulse [control] it becomes a larger problem in the future, because I'm bailing my son out of jail or burying him because…someone said ‘stop’ and his impulse said ‘go.’ ”
Parent perceptions that medication helped keep their children safe coexisted with concerns about medication safety and potential adverse effects. Fears about negative side effects (specifically, tics and reduced appetite) emerged as barriers to treatment:
“There were all these different studies with problems that were occurring later on in life with the medication…I didn't want to put my son through all that.”
A related attitude expressed at each group was that medication effects on children would have unwanted effects on an otherwise highly appreciated personality.
“My fear is that he would kind of ‘zombie out.’ ”
“I didn't want to take the sparkle away from her.”
“We like him the way he is. I love his personality…when he takes the [medication] all of a sudden he becomes very serious and he's focused but I don't like it as much.”
However, concerns about specific side effects for some parents were outweighed by the behavioral control (and safety in daily functioning) of a child whose behavior was improved on medication:
“It's not even a matter of…is my kid going to grow a third breast or is one arm going to be longer than the other…my main concern is, is this kid going to be safe?”
Another emergent attitude shared by parents with implications for treatment initiation was a consensus that medication might be deferred while parents tried treatments such as behavior modification, social skills training, or nutrition therapy before acquiescing to a stimulant trial. One mother described her efforts to construct a holistic ADHD management plan in the year after her daughter's ADHD diagnosis. This plan included school-based interventions, home-based behavior management, and herbal therapies. She felt that this process helped her agree eventually to medication: “I couldn't say yes to medication until I had all the pieces in place…looking at him from the natural, the educational…and in terms of the developmental.”
Another parent suggested that moving through a process of trial and error should be encouraged before accepting a medication recommendation: “Let them try the holistic route like I did for 6 months…you have to get past that.”
Perceptions of medical providers
During each group, parents discussed their experiences interacting with medical providers at the time of the ADHD diagnosis, when the medication recommendation was made, and over the course of their children's treatment. Both positive and negative interactions were shared toward the development of a composite set of qualities that would describe an optimal parent–professional interaction. Among the positive experiences that were shared involved medical professionals who made them feel part of shared decision making and collaborative care:
“It's like we just meshed…he'll listen. He'll ask me, ‘do you think it'll be better this way?’…it's like we're a team, it's not just him.”
Medical providers conveyed a collaborative stance by paying close attention to parents' stories and by taking a careful history of the child. Positive interactions with medical providers reinforced hope and persistence, conveying the notion that “… we will find a solution for this, it might take a while but together we're going to help your child.”
Although collaborative care was ideal, consensus was that medical providers needed to acknowledge that parents were the ultimate decision makers about medication treatment:
“We are the experts on our children. We are the number one [people] responsible for advocating for them and making decisions about their treatment.”
Along the lines of reviewing treatment options, parents felt strongly that psychiatrists needed to be “open to other therapies and treatments” besides medication. Once the decision to try medication was made, they respected psychiatrists who were “conservative.” This adjective was clarified as a professional who took a methodical and sequential approach to a child's treatment on-boarding:
“She [the psychiatrist] said we're not going to take all these medications at once, we're going to take it step by step …”
Parents discussed their experiences receiving psychoeducation about ADHD and about medication. All parents appreciated attempts by their medical provider to explain ADHD and medications; however, there were differences in parent preferences about the quantity of information they wished to receive and the preferred modality. Some parents expressed the preference for comprehensive, detailed information, often in writing and through pamphlets and/or Internet resources. Others preferred concise, orally presented summaries based on the provider's own experiences, and “just what they needed to know.” Describing the need to strike a balance between comprehensive and comprehensible information, one parent explained that “you don't want [the physician] to be too technical, but you don't want to have them insulting your intelligence either.” Parents felt that explanations of ADHD using a chronic medical illness metaphor were particularly effective in illustrating the role of medication in illness management:
“My doctor said to me, ‘If your child had diabetes would you not give him insulin?’ And that's what did it for me. My child is sick and he needs medication.”
Consensus across all groups was that while diagnostic and treatment expertise was appreciated, empathy and compassion were the qualities valued mostly highly in psychiatrists. The most common descriptions of positive medical provider interactions included specific mentions of active listening skills, good eye contact, and comfort being around (highly active) children. Although technical expertise was important, even more appreciated were attempts to meet caregiver informational needs in a caring and authentic manner. This was strikingly depicted by one grandmother of an 8-year-old boy, who had asked how stimulants might work for her grandchild. The child's psychiatrist “took out hands-on equipment and showed me how the brain works.” This grandparent expressed feeling as impressed with the time and effort taken to answer her question as she was with the methods: “She showed me all this stuff and I was like, “What?” I didn't know what she was talking about, but at least it let me know she was concerned.”
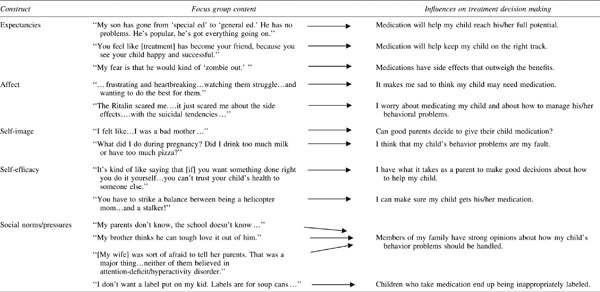
Deductive analysis
In addition to the parent perceptions of medication, medication regimens, and medical providers described previously, analysis of group transcripts yielded parent accounts that illustrated each variable hypothesized to influence behavioral intentions according to the adapted version of the UTBC. The five constructs, sample parent accounts, and attitudinal representations developed through the coding process that might influence treatment decision making are depicted in Table 1.
Table 1.
Parent Accounts Illustrating [Adapted] Unified Theory of Behavior Change Constructs: Underlying Attitudes Influencing Treatment Decision Making
 |
Expectancies
Ongoing examination of the costs and benefits of medication treatment was a theme that resurfaced throughout each group. Many of the positive and negative attitudes to medication grouped together in the inductive analysis could also be conceptualized as positive and negative expectancies about treatment effectiveness and potential risks. Moreover, maintaining a positive mindset for treatment success required transcending the hurdles of time and delays in response, as treatment success was not always immediate:
“The first medicine he was on was not helpful at all…but I found a second medication that worked…being a parent of a child with ADHD [requires] patience.”
Parents felt that positive expectations about treatment outcome needed to be tempered by realism, and the understanding that trial and error were often part of the process of successful long-term treatment. This aspect of the conceptual model was clearly a salient concept in influencing treatment decisions, as parents reported continually examining hopes and expectations for their child's well-being against the backdrop of the perceived shadow of negative treatment effects. These contrasting attitudes did not appear to mitigate over time, and were present in parents of newly diagnosed children as well as older children who had been diagnosed years previously.
Affect
Parents readily shared deep emotional reactions to living with a child with ADHD and managing their children's behavior. A mother of an 8-year-old girl recalled her experiences over the past two years since receiving her daughter's ADHD diagnosis as “frustrating and heartbreaking…watching them struggle…and wanting to do the best for them.” In addition, affect-laden responses took the form of expressions of self-blame for the causes of their child's condition, or feelings of guilt that illness-related symptoms were caused by lack of time or effort implementing consistent discipline or behavioral interventions. Emotional arousal caused by concerns for their children contrasted with fears about medication. This arousal seemed to distort factual information; for example, in one parent who had extrapolated media reports about suicidal risk from antidepressant medication to risks from stimulants, and feared that ongoing stimulant treatment might place her child at risk for self-injury.
Self-image
Themes emerged from the discussion that highlighted parents' personal engagement in decision making and how they felt about themselves in the role of parenting a child with ADHD. Parental self-image related to medication decisions was influenced heavily by social groups; one parent described subsequent self-doubts about medicating her child after an incident with peers:
“One day at work we were having lunch, and…I mentioned it [medication]. Oh my goodness! I felt like I was being lynched and I was a bad mother…How could you put your child on medication?…. [I felt] I should have tried other avenues.”
An additional aspect of decision making involved accepting the idea that medication management of ADHD was consistent with being a good parent rather than a parent who was taking the “easy way out”:
“You know…you have to be a strong person…parents who know…educated parents who do the research put their child on medicine.”
Self-efficacy beliefs
Parent accounts illustrated ideas that went beyond self-image per se to include self-evaluative beliefs about managing ADHD. The beliefs involved the ability to feel good about initiating medication, as well as about parenting their child with ADHD. Although parents clearly described the strain of managing an ADHD child, high levels of self-efficacy were evident in parents' accounts of impassioned efforts to manage their child's behavior, and in descriptions of assertive searches for more effective collaboration with schools and community agencies:
“For a long time I was sneaking into the classroom on Fridays at the end of the day…I would come in and read to the kids…that's what helped him. You do what you can.”
“It's kind of like saying that [if] you want something done right you do it yourself…you can't trust your child's health to someone else.”
Parents also took pride in humorously describing elaborate morning routines for their child that included medication administration: “You have to strike a balance between being a helicopter mom and a…stalker!” In these accounts parents were clearly describing experiences that reflected the intense effort required to manage a child with ADHD but also feelings of success and efficacy in mastering multiple challenging situations, including daily medication administration.
Social norms/pressures
Finally, the social/interactive nature of the focus groups facilitated discussion of the effects of peer, family, and societal influences on the management of children's behavior problems.
“I was wary to put [him] on anything. Everyone I [knew had a] kid [who] was on something…they're forcing you to do something with your child that you feel is really not right.”
The influence of social norms ranged from hiding the use of stimulants for fear of disapproval, to alternative views of behavior management held by spouses and other family members. Parental concern about social stigma was also expressed, as well as resistance to initiating medication treatment because social norms suggested that stimulant medication was overused and would lead to inappropriate labeling. Social interactions and self-image appeared particularly intertwined in terms of ADHD-related treatment decisions, and perceptions of stigma were heavily influenced by prior personal experiences. As a single father raising a child with ADHD and co-morbid Asperger's disorder stated:
“I went to school years ago myself…when I had to get medication I was labeled. I said, I don't want a label put on my kid. Labels are for soup cans, you know.”
Discussion
Qualitative methods were used for this phase of our intervention development to provide the descriptive depth that group interactions offer when held around a relevant topic. The consistency of thematic content across groups and the use of multiple coders provided confirmatory evidence of the credibility of the data (Lincoln and Guba 1985). In addition, we utilized both inductive analytic methods as well as a theory-driven examination of transcripts. This strategy provided for a broad and multidimensional “lens” to extrapolate meaning from parent accounts. For example, parents' complex and at times inconsistent views of their own medication adherence was an unexpected finding that might have gone undetected through theory-based analysis alone.
Parent accounts obtained from the focus groups suggest that multiple social, cognitive, and affective dimensions influence decisions to accept treatment recommendations. Parents described deeply ambivalent feelings about medication. Those who did pursue treatment maintained their sights on their child's larger functional picture and future well-being. Many of the attitudes expressed during the groups confirm earlier research findings assessing parent perceptions of ADHD. For example, Charach and colleagues (2006) described parental fears of side effects, inadequate family support for the decision to medicate, and parental guilt fueled by social pressures that were similar to parent accounts in this current investigation. Moreover, our parent narratives suggesting an elaborate preliminary process prior to trying medication are consistent with other research. Ghanizadeh (2007) detected a gap of ∼1.5 years between initial parent suspicions that their child had ADHD and pursuing a referral for services. DosReis and colleagues (2009) found that an average of 4 years elapsed between parental identification of an initial presenting problem and the decision to try medication. The reasons for this long deliberative process are likely to include the belief that nonpharmacological approaches such as behavior management are “more acceptable” and should be attempted prior to a “less acceptable” treatment such as stimulant medication (Johnston et al. 2005).
Parent fears about the effects of stigma from receiving an ADHD diagnosis and from using medication are findings consistent with prior research (dosReis et al. 2010). However, there was also consensus that receiving an ADHD diagnosis and conceptualizing it as an illness had heuristic value for understanding their child's problems. This contrasts with dosReis and colleagues (2009) who found that a large subgroup of parents took a problem-oriented as opposed to an illness-oriented approach to their child's ADHD and medication. In fact, our sample agreed that an illness representation of ADHD helped them to accept a medication trial. This conceptualization made psychopharmacological approaches more understandable, and comparable to managing other pediatric illnesses (for which medication is not only essential but also socially more neutral, such as insulin for diabetes). The sample for the current investigation was drawn from a child psychiatry clinic, and may have been more likely to include parents comfortable integrating a medical understanding of their child's condition, as compared with the more heterogeneous sample in the dosReis et al. (2009, 2010) reports that utilized an individual interview protocol and included parents from primary care and specialty pediatric settings.
The desirable characteristics parents described in their physicians are consistent with research that finds a greater likelihood of treatment initiation in the presence of positive attitudes toward a medical provider. In addition, parent ideas of partnership were characterized by equality with physicians, who were seen as providing expertise so that a parent could make a treatment decision. Although parents underscored the importance of ADHD expertise, their definitions of expertise were as likely to incorporate a provider's compassionate and caring demeanor as they were to include his/her experience and factual knowledge about treatment options. This is comparable to parent attitudes reported by Fiks and colleagues (2011) in a study of parents' and pediatricians' ideas about shared decision making, and is also consistent with Gearing and colleague's (2011) framework of provider–patient interactions as having distinct needs and characteristics at different phases of the treatment process. Parent accounts also provide empirical support for an “enhanced autonomy” approach outlined in Quill and Brody (1996). This model conceptualizes an optimal patient-provider encounter as acknowledging patients as managers and decision makers for their healthcare, while also noting that good patient decisions are made with physician input, guidance, and recommendations.
Interpretation of study findings is limited by a disproportion of participants who had pursued recommendations for stimulant treatment. Therefore these data may overrepresent the views of parents who choose medication for their child. These parents also had access to a range of specialty mental health services from which to make choices and form opinions. Their attitudes and decision-making processes may differ from parents who lack access to psychiatric support and other behavioral health services (Zima et al. 2010). Nonetheless, these limitations did not hinder our ability to identify barriers to stimulant treatment, as all parents were able to discuss fears and concerns about medication even when they had eventually agreed to pursue treatment. Furthermore, among those who had chosen medication treatment, several parents had delayed treatment initiation and also reported during the group that they did not consistently give medication as prescribed.
The five constructs of the adapted UTBC model organized a significant proportion of the topics that parents reported as influencing their decision to medicate. Thus, the investigation adds an important theory-driven dimension to the literature on parent attitudes to medication initiation, and our results should serve as a springboard for additional inquiry to refine the specific contributions of these variables in influencing parent decision making. For example, the focus group data did not clearly indicate the directionality or magnitude of these influences on whether to try stimulant medication, or when. In addition, analysis of focus group discussions indicated that constructs such as parent emotional reactions and expectations about treatment may both facilitate and hinder treatment initiation. Further research is needed on the specific ways that the UTBC construct(s) assessed at initial evaluation might predict treatment initiation. Other theories that emphasize the transactional nature of adherence behavior (see Gearing et al. 2011) may be incorporated into future research to give temporal dimension to the five UTBC constructs as they might change over time. An additional limitation is the lack of information about the attitudes, beliefs, and expectations of the medical providers themselves. Incorporating a theory-driven approach in any intervention to improve adherence would also involve dealing with physicians' own perceived competencies, standards of care in their immediate environment and in their professional field, and their conceptions of barriers to implementing any adjunctive intervention to aid children and families (Perkins et al. 2007).
Clinical Significance
The objective of this research was to identify ways to encourage stimulant treatment initiation and support adherence to recommendations over time. Study findings suggest several specific areas for clinicians to consider when engaging a family of a child with ADHD in medication treatment:
1. The ambivalence about medication outlined in the literature and supported by this investigation suggests that broad and multidimensional assessment of parent attitudes to medication should be conducted, ideally during an initial evaluation and before a medication recommendation is made.
2. Clinicians should attempt to understand the degree to which parents think their child will be subjected to stigma and labeling if they were to take medication. In addition, parent sadness or anxiety about receiving an ADHD diagnosis for their child may influence motivation to treat and may affect clarity in decision making. Perhaps most importantly, understanding specific parent ideas about the “pros and cons” of medication treatment appear critical to detecting what types of information and encouragement parents will need before consenting to a medication trial. More targeted communication might then accelerate the extended delay that appears to be a common part of the decision-making process.
3. Results identified divergent parent opinions about the optimal quantity and modality of psychoeducational messages. This suggests that providing information to families about ADHD should involve flexibility and attempt to match parent preferences to the approach taken (e.g., more information vs. summative outlines, written vs. informal strategies, etc.).
4. In addition, parent accounts suggested that a wide range of alternative treatments are tried prior to initiating medication. Strategies varied from well-studied and efficacious behavioral treatments and group therapies, to nutritional and alternative treatments with less empirical support that were implemented without professional guidance. Professionals might help parents work through the process of developing an integrative management plan by presenting information about the varying levels of evidence for the effectiveness of these treatments. This information might set the stage for a more careful consideration of which strategies to use before trying medication, and establish a working relationship with the parent that would allow an “open-door” for including a medication trial at a later date.
5. Parents' prior interactions with medical providers, and their expectations for subsequent medical encounters, should be considered when delivering messages about ADHD treatment. Parent accounts suggest that their conceptions of professional expertise are multidimensional. An “expert” provider not only has extensive training, information, and experience, but also takes adequate time to understand the child and family, exhibits empathy, and is actively engaged as a helping professional. Along these lines, providers exhibiting these qualities will convey a strong sense of conviction about their recommendations and will demonstrate respect for parents' right to choose. A medical provider who can integrate these composite qualities is most likely to establish a positive groundwork for treatment initiation.
6. Parents need clear guidance from medical providers about how the medication is to be administered—for example, including whether it is to be swallowed whole or if drug holidays are advisable.
7. Ongoing and creative assessment of adherence is vital throughout the course of ADHD treatment. Parents often respond affirmatively to questions about whether they are administering medication as prescribed. In fact, they maybe departing from recommendations in critical ways that are outside their awareness or despite their best of intentions to administer optimal treatment. Accurate assessment is likely to require multiple questions framed differently and nonjudgmentally, and that inquire into concrete behavioral patterns. Optimal adherence should not be inferred from a particular behavioral presentation of the child during an appointment, or from parent reports of treatment response alone (Velligan et al. 2010).
Summary
Data from this qualitative investigation suggest that a parent's decision to initiate medication treatment for their child with ADHD requires significant attention to their attitudes to psychiatric treatment and the impact of social and emotional influences. Additional research is needed to identify how these attitudes influence treatment decision making, and how to modify attitudes that may impede successful treatment onboarding. These qualitative data suggest that clear information and an unequivocal recommendation to try medication, balanced with patience and acceptance of a parent's decision as a process, are likely to facilitate successful initiation. Future research should test theory-driven strategies for enhancing the decision-making process by targeting parent attitudes and enhancing the communication skills of the providers making the recommendations.
Disclosures
Daniel J. Coletti, Ph.D., has no institutional or corporate/commercial relationships that might pose a conflict of interest. Elizabeth Pappadopulos, Ph.D., is employed by Pfizer, Inc. Nikki Katsiotas, B.A., has no institutional or corporate/commercial relationships that might pose a conflict of interest. Alison Berest, M.A., has no institutional or corporate/commercial relationships that might pose a conflict of interest. Peter S. Jensen, M.D., has participated on advisory boards for Shire, Inc., and received speaking fees from Janssen-Ortho. Vivian Kafantaris, M.D., has received investigator-initiated research support in the form of donation of medication from Bristol-Myers Squibb. The pharmaceutical companies had no access to these data and were not involved in data analysis or in the preparation of this manuscript.
Appendix A: Parent Focus Group Question Guide
• The following are questions developed prior to Focus Group implementation that structured discussion and ensured that adherence patterns and UTBC constructs were reviewed.
• The groups were semistructured. The order of the topics, and the use of follow-up questions and probes, varied across each group.
Participant Introductions and Unstructured Discussion
Facilitators welcome group, review goals, and ground rules for interaction. Participants are asked to share brief biographical information about themselves and about their child, and the treatment their child currently receives.
Follow-up questions:
• Please give us 1 or 2 words or adjectives that sum up your experiences of having a child diagnosed with attention-deficit/hyperactivity disorder (ADHD). Probes: Group leaders should be prepared to reflect and probe the adjectives that are shared—“would other people have used that word?”
Adherence
We would like to get a good picture of what the plan is for managing your child's ADHD, and for coordinating the medication if that is a part of the plan.
Follow-up questions:
• Is there a plan?
• Who does what?
• What happens when you realize the plan isn't being followed? Probes: Shared responsibilities among caregivers, level of parental involvement and monitoring, behavior management techniques used to facilitate adherence, etc.
• Think about the kinds of things or issues that HELP or MAKE IT EASIER when it comes to following management plans or regimens, and the issues that GET IN THE WAY or MAKE IT HARD to follow management regimens. What are the things that come to mind? Probe: Tell me how it works in your homes? What specifically makes it hard? How did you think of that (idea that facilitates adherence)?
Theory-Based Constructs
For the NEXT part, we would like to go over some specific ideas to see how each of the following plays a role in your child's treatment. For each idea, we would like to get your immediate reaction (do not censor yourself). BUT: Consider things like the following:
• How are these ideas influencing your thoughts and feelings about medication?
• How do these things play a role in giving your child his/her medication?
• Do they make it easier or harder for you to manage your child's medication?
Expectancies
Some people think that making sure your child follows his/her medication plan is influenced by what you expect to happen if you do or do not follow through with the plan …
• Does thinking about what the medication will do for your child make it easier or harder for you to get them to take it as prescribed? Probe: Do you make it happen because of the things that will come afterward?
• What do you see as the advantages of your child always taking their medication as prescribed? Are there disadvantages? (Probe: Positive outcomes of, benefits of, good/bad things that would happen, etc.)
Social norms
Now we would like to discuss how taking medication and following a plan is influenced by what people hear about medication in general (in the media, in your circle of friends, etc.).
• Do people talk about medications for behavior? What is being said about taking medications?
Probe: For positive/negative attitudes about medication in different social contexts.
• Who supports/approves of your child taking medication as prescribed? Who disapproves? Who would you like support from? Do you get that support?
• Who or what else comes to mind when you think about your child taking medication for ADHD?
Self-efficacy
We would like to talk a little about how you all feel as parents and your ability to do all the things you need to do when you have a child with ADHD.
• I'm wondering if there are people in the group who feel relatively good about how they get their child to take his/her medicine?
• On the other hand are there people who just feel they don't know how to do it? Probe: Are there people who feel they can do it sometimes and not others? What helps you or makes it easier for your child to take the medication as prescribed?
Self-image
Some people believe that having a child who is on medication for their behavior says something about who they are as a parent….
• Does having a child who has been prescribed medicine for his/her behavior problems have any effect on how you feel as a parent? How did it affect your decision to try medication to help your child? How does it make your child feel?
• If your child takes medication for ADHD, does this say something about you as a parent? What does it say?
Affect
Having a child who takes medicine for his/her behavior creates feelings or emotions in the parent.
• Do these feelings either help with following the plan or do they get in the way?
• Tell us about the feelings you experience when you think about your child, and his/her treatment.
• What kind of feelings do you have about giving your child medication for ADHD?
Parent Provider Communication
We are interested in the kinds of roles your doctors (the psychiatrists who prescribe the medicine) play in helping you manage your child's care.
Follow-up:
• Parents learn a lot of new information when their child is diagnosed with ADHD and is prescribed medication. What did your child's doctor say to you when your child was diagnosed with ADHD?
• What did he/she tell you about ADHD medications and their side effects?
• What were/are follow-up visits like?
• What kind of information do you wish your doctor informed you about?
• How does your child's doctor communicate important information (talking, handouts, etc.) about ADHD? (methods)
• What was your psychiatrist's communication style when discussing these issues? What words would you use to describe HOW they gave you the information?
• In your opinion what kind of communication style works best with YOU when you're in a doctor–parent relationship?
• Do doctors ever give you advice about how to get your child to take their medications? How do they try to be helpful? If they give advice, do you follow it? Why or why not? Does it work?
• Some doctors may be better (in some way) than others in treating children with ADHD. What makes a doctor better at managing ADHD?
Acknowledgments
The authors would like to thank Hara Stephanou and Michele Gonen for their contributions to this manuscript.
References
- Adler LD. Nierenberg AA. Review of medication adherence in children and adults with ADHD. Postgrad Med. 2010;122:184–191. doi: 10.3810/pgm.2010.01.2112. [DOI] [PubMed] [Google Scholar]
- Brinkman WB. Sherman SN. Zmitrovich AR. Visscher MO. Crosby LE. Phelan KJ. Donovan EF. Parental angst making and revisiting decisions about treatment of attention-deficit/hyperactivity disorder. Pediatrics. 2009. http://pediatrics.aappublications.org/content/124/2/580.long. [May 18;2011 ]. pp. 580–589.http://pediatrics.aappublications.org/content/124/2/580.long [DOI] [PubMed]
- Brown JJ. Hertzer JL. Findling RL. Assessment of core competencies in childhood attention-deficit/hyperactivity disorder practice. J Child Adolesc Psychopharmacol. 2011;21:33–41. doi: 10.1089/cap.2010.0029. [DOI] [PubMed] [Google Scholar]
- Chacko A. Newcorn JH. Feirsen N. Uderman JZ. Improving medication adherence in chronic pediatric health conditions: A focus on ADHD in youth. Curr Pharm Des. 2010;16:2416–2423. doi: 10.2174/138161210791959908. [DOI] [PubMed] [Google Scholar]
- Charach A. Gajaria A. Improving psychostimulant adherence in children with ADHD. Expert Rev Neurother. 2008;8:1563–1571. doi: 10.1586/14737175.8.10.1563. [DOI] [PubMed] [Google Scholar]
- Charach A. Skyba A. Cook L. Antle BJ. Using stimulant medication for children with ADHD: What do parents say? A brief report. J Can Acad Child Adolesc Psychiatry. 2006;15:75–83. [PMC free article] [PubMed] [Google Scholar]
- Charach A. Volpe T. Boydell KM. Gearing RE. A theoretical approach to medication adherence for children and youth with psychiatric disorders. Harv Rev Psychiatry. 2008;16:126–135. doi: 10.1080/10673220802069715. [DOI] [PubMed] [Google Scholar]
- Coghill D. The impact of medications on quality of life in attention-deficit hyperactivity disorder: A systematic review. CNS Drugs. 2010;24:843–866. doi: 10.2165/11537450-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Coletti D. Leigh E. Gallelli K. Kafantaris V. Patterns of adherence to treatment in adolescents with bipolar disorder. J Child Adolesc Psychopharmacol. 2005;15:913–917. doi: 10.1089/cap.2005.15.913. [DOI] [PubMed] [Google Scholar]
- Concannon PE. Tang YP. Management of attention deficit hyperactivity disorder: A parental perspective. J Paedriatr Child Health. 2005;41:625–630. doi: 10.1111/j.1440-1754.2005.00771.x. [DOI] [PubMed] [Google Scholar]
- Conners CK. Forty years of methylphenidate treatment in attention-deficit/hyperactivity disorder. J Atten Disord. 2002;6((Suppl. 1)):S17–S30. doi: 10.1177/070674370200601s04. [DOI] [PubMed] [Google Scholar]
- dosReis S. Barksdale CL. Sherman A. Maloney K. Charach A. Stigmatizing experiences of parents of children with a new diagnosis of ADHD. Psychiatr Serv. 2010;61:811–816. doi: 10.1176/ps.2010.61.8.811. [DOI] [PubMed] [Google Scholar]
- dosReis S. Mychailyszyn MP. Evans-Lacko SE. Beltran A. Riley AW. Myers MA. The meaning of attention-deficit/hyperactivity disorder medication and parents' initiation and continuity of treatment for their child. J Child Adolesc Psychopharmacol. 2009;19:377–383. doi: 10.1089/cap.2008.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV. Biederman J. Zimmerman BJ. An analysis of patient adherence to treatment during a 1-year, open-label study of OROS methylphenidate in children with ADHD. J Atten Disord. 2007;11:157–166. doi: 10.1177/1087054706295663. [DOI] [PubMed] [Google Scholar]
- Fereday J. Muir-Cochrane E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5:80–92. [Google Scholar]
- Fiks AG. Hughes CC. Gafen A. Guevara JP. Barg FK. Contrasting parents' and pediatricians' perspectives on shared decision-making in ADHD. Pediatrics. 2011;127:e188–e196. doi: 10.1542/peds.2010-1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M. Triandis H. Kan F. Becker M. Middlestadt S. Eichler A. Factors influencing behavior, behavior change. In: Baum A., editor; Tevenson T., editor; Singer J., editor. Handbook of Health Psychology. Mahwah, NJ: Erlbaum; 2001. pp. 3–16. [Google Scholar]
- Francis V. Korsch BM. Morris MJ. Gaps in doctor-patient communication: Patients' response to medical advice. N Engl J Med. 1969;280:535–540. doi: 10.1056/NEJM196903062801004. [DOI] [PubMed] [Google Scholar]
- Gearing RE. Townsend L. MacKenzie M. Charach A. Reconceptualizing medication adherence: Six phases of dynamic adherence. Harv Rev Psychiatry. 2011;19:177–189. doi: 10.3109/10673229.2011.602560. [DOI] [PubMed] [Google Scholar]
- Ghanizadeh A. Educating and counseling of parents of children with attention-deficit hyperactivity disorder. Patient Educ Couns. 2007;68:23–28. doi: 10.1016/j.pec.2007.03.021. [DOI] [PubMed] [Google Scholar]
- Guilamo-Ramos V. Jaccard J. Dittus P. Collins S. Parent-adolescent communication about sexual intercourse: An analysis of maternal reluctance to communicate. Health Psychol. 2008;27:760–769. doi: 10.1037/a0013833. [DOI] [PubMed] [Google Scholar]
- Gustafsson P. Hansson K. Eidevall L. Thernlund G. Svedin CG. Treatment of ADHD with amphetamine: Short-term effects on family interaction. J Atten Disord. 2008;12:83–91. doi: 10.1177/1087054707308482. [DOI] [PubMed] [Google Scholar]
- Hamrin V. McCarthy EM. Tyson V. Pediatric psychotropic medication initiation and adherence: A literature review based on social exchange theory. J Child Adolesc Psychiatr Nurs. 2010;23:151–172. doi: 10.1111/j.1744-6171.2010.00237.x. [DOI] [PubMed] [Google Scholar]
- Hansen DL. Hansen EH. Caught in a balancing act: Parents' dilemmas regarding their ADHD child's treatment with stimulant medication. Qual Health Res. 2006;16:1267–1285. doi: 10.1177/1049732306292543. [DOI] [PubMed] [Google Scholar]
- Hart CN. Drotar D. Gori A. Lewin L. Enhancing parent-provider communication in ambulatory pediatric practice. Patient Educ Couns. 2006;63:38–46. doi: 10.1016/j.pec.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Hart CN. Kelleher KJ. Drotar D. Scholle SH. Parent-provider communication and parental satisfaction with care of children with psychosocial problems. Patient Educ Couns. 2007;68:179–185. doi: 10.1016/j.pec.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J. Dodge T. Dittus P. Parent-adolescent communication about sex and birth control: A conceptual framework. New Dir Child Adolesc Dev. 2002;97:9–41. doi: 10.1002/cd.48. [DOI] [PubMed] [Google Scholar]
- Jensen P. Longer term effects of stimulant treatments for attention-deficit/hyperactivity disorder. J Atten Disord. 2002;6(Suppl. 1):S45–S56. doi: 10.1177/070674370200601s06. [DOI] [PubMed] [Google Scholar]
- Jensen PS. Arnold LE. Swanson JM. Vitiello B. Abikoff HB. Greenhill LL. Hechtman L. Hinshaw SP. Pelham WE. Wells KC. Conners CK. Elliott GR. Epstein JN. Hoza B. March JS. Molina BS. Newcorn JH. Severe JB. Wigal T. Gibbons RD. Hur K. 3-year follow-up of the NIMH MTA study. J Am Acad Child Adolesc Psychiatry. 2007;46:989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- Johnston C. Hommersen P. Seipp C. Acceptability of behavioral and pharmacological treatments for attention-deficit/hyperactivity disorder: Relations to child and parent characteristics. Behav Ther. 2008;39:22–32. doi: 10.1016/j.beth.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Katusic SK. Barbaresi WJ. Colligan RC. Weaver AL. Leibson CL. Jacobsen SJ. Psychostimulant treatment and risk for substance abuse among young adults with a history of attention-deficit/hyperactivity disorder: A population-based, birth cohort study. J Child Adolesc Psychopharm. 2005;15:764–776. doi: 10.1089/cap.2005.15.764. [DOI] [PubMed] [Google Scholar]
- Lincoln YS. Guba EF. Naturalistic Inquiry. Beverly Hills, CA: Sage Publications; 1985. [Google Scholar]
- Marcus SC. Durkin M. Stimulant adherence and academic performance in urban youth with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2011;50:480–489. doi: 10.1016/j.jaac.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Miles MB. Huberman AM. 2nd. Thousand Oaks, CA: Sage Publications; 1994. Qualitative Data Analysis: An Expanded Sourcebook. [Google Scholar]
- MTA Cooperative Group: A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder: Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Pappadopulos E. Jensen PS. Chait AR. Arnold E. Swanson JM. Greenhill LL. Hechtman L. Chuang S. Wells KC. Pelham W. Cooper T. Elliott G. Newcorn JH. Medication adherence in the MTA: Saliva methylphenidate samples versus parent report and mediating effect of concomitant behavioral treatment. J Am Acad Child Adolesc Psychiatry. 2009;48:501–510. doi: 10.1097/CHI.0b013e31819c23ed. [DOI] [PubMed] [Google Scholar]
- Perkins MB. Jensen PS. Jaccard J. Gollwitzer P. Oettingen G. Pappadopulos E. Hoagwood KE. Applying theory-driven approaches to understanding and modifying clinicians' behavior: What do we know? Psychiatr Serv. 2007;58:342–348. doi: 10.1176/ps.2007.58.3.342. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA. Jensen PS. Martin JK. Perry BL. Olafsdottir S. Fettes D. Public knowledge and assessment of child mental health problems: Findings from the National Stigma Study-Children. J Am Acad Child Adolesc Psychiatry. 2008;47:339–349. doi: 10.1097/CHI.0b013e318160e3a0. [DOI] [PubMed] [Google Scholar]
- Pliszka S. AACAP Work Group on Quality Issues. Practice parameters for the assessment and treatment of children and adolescents with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- Powers RL. Marks DJ. Miller CJ. Newcorn JH. Halperin JM. Stimulant treatment in children with attention-deficit/hyperactivity disorder moderates adolescent academic outcome. J Child Adolesc Psychopharmacol. 2008;18:449–459. doi: 10.1089/cap.2008.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quill TE. Brody H. Physician recommendations and patient autonomy: Finding a balance between physician power and patient choice. Ann Intern Med. 1996;125:763–769. doi: 10.7326/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- Sanchez RJ. Crismon ML. Barner JC. Bettinger T. Wilson JP. Assessment of adherence measures with different stimulants among children and adolescents. Pharmacotherapy. 2005;25:909–917. doi: 10.1592/phco.2005.25.7.909. [DOI] [PubMed] [Google Scholar]
- Basics of Qualitative Research: Techniques, Procedures for Developing Grounded Theory. In: Strauss A, editor; Corbin J, editor. 2nd. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Velligan DI. Weiden PJ. Sajatovic M. Scott J. Carpenter D. Ross R. Docherty JP. Assessment of adherence problems in patients with serious and persistent mental illness: Recommendations from the Expert Consensus Guidelines. J Psychiatr Pract. 2010;16:34–45. doi: 10.1097/01.pra.0000367776.96012.ca. [DOI] [PubMed] [Google Scholar]
- Winterstein AG. Gerhard T. Shuster J. Zito J. Johnson M. Liu H. Saidi A. Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in Medicaid database. Ann Pharmacother. 2008;42:24–31. doi: 10.1345/aph.1K143. [DOI] [PubMed] [Google Scholar]
- World Health Organization: Adherence to Long-Term Therapies. Geneva: WHO; 2003. Evidence of Action. [Google Scholar]
- Zima BT. Bussing R. Tang L. Zhang L. Ettner S. Belin TR. Wells KB. Quality of care for childhood attention-deficit/hyperactivity disorder in a managed care medicaid program. J Am Acad Child Adolesc Psychiatry. 2010;49:1225–1237. doi: 10.1016/j.jaac.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]