Abstract
Introduction
Dysphagia is a common side effect following chemoradiation therapy (CRT) in head and neck cancer (HNC) patients. Current dysphagia management includes swallowing therapy and dilation procedures, but these treatments have limitations. While acupuncture has been reported to positively impact swallowing function and quality of life (QOL) in patients with dysphagia, current evidence is inconclusive.
Material and Methods
In an ongoing trial, 42 squamous cell carcinoma HNC patients, who are receiving platinum-based CRT with curative intent, are being recruited from a comprehensive cancer center. They are randomized to 12 sessions of either active acupuncture or to sham acupuncture during and following CRT over a 24-week period. Blinded research staff assesses outcomes at baseline, 20 weeks post-CRT (end of acupuncture), and 12 months after baseline (6-month follow-up). The primary outcome is change in M.D. Anderson Dysphagia Inventory score from baseline to 12 months. Secondary outcomes include QOL measures pertaining to HNC patients. In addition, a subset of study patients are tested for salivary flow rates and cytokines, including plasma transforming growth factor –β1 and interleukin 6 (n=10 per arm), to preliminarily explore the biological mechanisms of acupuncture for dysphagia.
Discussion
This paper addresses unique challenges related to study design in nonpharmacological, sham-controlled acupuncture trials including development of evidence-based credible verum and sham treatment protocols, blinding, and assuring fidelity of treatment. Results of this study will inform the feasibility of conducting a large scale trial and will provide preliminary evidence regarding the value of acupuncture for dysphagia in HNC patients.
Keywords: Acupuncture, chemoradiation therapy, radiation therapy, head and neck cancer, dysphagia, TGF-β1, IL-6, MDADI, randomized sham-controlled trial
1. Introduction
Dysphagia, or difficulty with swallowing, is a common and expected side effect following chemoradiation therapy (CRT) in patients with head and neck cancer (HNC). It is reported to occur in up to 50% of patients after CRT[1–3]. Dysphagia and its related clinical presentation, aspiration, can significantly impact quality of life in cancer patients recovering from CRT. Many factors contribute to dysphagia, including prolonged mucositis, diffuse fibrosis, contracture and loss of flexibility of the pharyngeal constrictor muscles, xerostomia, and pain[4]. A significant proportion of HNC patients are feeding tube dependent for many months after completion of CRT[5]. A number of studies suggest that quality of life related to swallowing function for HNC patients fails to improve 12 months after therapy[6–8]. Consequently, innovative non-pharmacologic therapies offer an attractive option that may increase the rate and magnitude of recovery from dysphagia in HNC patients.
Acupuncture is an ancient Chinese medical technique that is growing in popularity in the United States. Previous research suggests that acupuncture may reduce symptoms and side effects that are associated with primary cancer therapy, such as chemotherapy-induced nausea[9, 10], hot flashes in women with breast cancer[11], and dysfunction and pain after neck dissection[12].
The uses of acupuncture for dysphagia are well documented in ancient Chinese medicine texts[13]. More recently, research using both animal models and human trials has begun to evaluate the efficacy and underlying mechanisms through which acupuncture may positively impact dysphagia.
Three published studies have characterized the responses of HNC patients with dysphagia to acupuncture[14–16]. In addition, our group has reported a case series of 10 HNC patients who had received acupuncture treatment and appeared to have a shorter duration with percutaneous endoscopic gastrostomy (PEG) tube[17]. Besides these HNC-related dysphagia reports, a significant body of literature exists that characterizes the efficacy of acupuncture for stroke-related dysphagia[18, 19]. While the etiology of dysphagia related to HNC and stroke are quite different, from a traditional Chinese medicine (TCM) perspective, many components of stroke-related acupuncture needling techniques are still relevant to radiation-induced dysphagia[18, 20, 21].
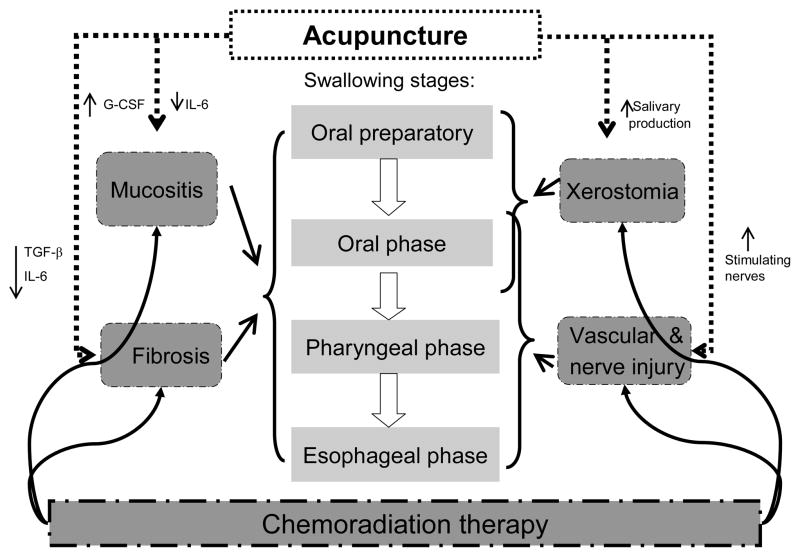
There are several pathologic changes affected by CRT that may impact dysphagia in the post CRT phase, namely vascular and nerve damage, xerostomia and fibrosis. Preliminary evidence suggests that acupuncture promotes the recovery of impaired swallowing function by inhibiting pro-inflammatory cytokines and growth factors[22–25]; stimulating peripheral and central nerve coordination[21, 26, 27]; increasing salivary production[28–30] and promoting tissue repair[31]. The hypothesized biological effects of acupuncture on dysphagia and the supporting evidence are summarized and presented in Table 1 and Figure 1.
Table 1.
Supporting evidence for biological effects of acupuncture on dysphagia.
| Author/Year | Subjects | N | Groups* | Conditions | Interventions | Relevant Measurements | Results |
|---|---|---|---|---|---|---|---|
| Cui 2007[31] | rats | 60 | 6 | cyclophosphamide induced leukopenic rats | EA† vs. rat model | serum GM-CSF‡ | EA significantly increased GM-CSF level at day 11 compared with model group (p<0.01) |
| Chen 2006[22] | humans | 120 | 2 | acute cerebral infarction | MA§ plus medications vs. medications | serum IL-6** | IL-6 level significantly decrease in acupuncture group compared with medication group at day 14 (p<0.05) |
| Zhuang 2006[25] | rats | 36 | 3 | chemical radiculitis | MA vs. no treatment | plasma IL-6 | IL-6 level significantly decreased in the acupuncture group compared with model group at day 30 (p<0.05) |
| Ma 2009[23] | rats | 40 | 4 | carbon tetrachloride induced hepatic fibrosis | EA vs. model | tissue TGF-β1†† | Protein expression of TGF-β1 significantly decreased in EA-treated group vs. model group at week 8 (p<0.01) |
| Xiao 2002[24] | rats | 72 | 4 | acute ischemic myocardial infarction | EA vs. model | tissue TGF-β1 | TGF β1 expression in myocardium less in EA group than model group (+++ vs. +) at week 1 |
| Zhang 2002[26] | humans | 30 | 1 | chronic stroke related dysphagia | MA | evoked potential in brainstem and swallowing related muscles | Amplitude and time duration of circothyroid and tongue muscles decreased after acupuncture (p<0.05) |
| Seki 2003[21] | humans | 41 | 1 | chronic cerebral infarction related dysphagia | MA | latency time in swallowing (LTSR) | Significant improvements in LTSR 30 minutes after MA; continued for up to 7 days |
| Seki 2005[20] | humans | 32 | 2 | poststroke with dysphagia | MA+ usual care vs. usual care | videofluoroscopic swallow study | Mean swallowing time significantly shorter in MA group vs. usual care group at week 4 (p<0.05) |
| Deng 2008[27] | humans | 20 | 1 | healthy volunteers | true MA vs. sham MA | fMRI‡‡ | True MA associated with bilateral activation of the insula and adjacent operculum; induced more saliva production than sham MA |
| Braga 2008[29] | humans | 12 | 1 | radiation induced xerostomia | MA | objective resting and stimulated whole salivary flow rates | Statistically significant improvement for salivary flow rates found at week 6 (P<0.05) |
| Blom 1992[28] | humans | 21 | 2 | xerostomia | MA vs placebo MA | salivary flow rates | MA group showed significant persistent increase of salivary flow rates vs. placebo MA |
| Dawidson 1997[30] | humans | 8 | 1 | healthy volunteers | MA and EA | stimulated and unstimulated salivary flow rates | Significant increase of unstimulated salivary flow both during and after MA |
Randomization assignments were applied in all groups except single arm studies
EA: electroacupuncture
GM-CSF: granulocyte-macrophage colony-stimulating factor
MA: manual acupuncture
IL-6: interleukin 6
TGF-β1: transforming growth factor beta 1
fMRI: functional magnetic resonance imaging
Figure 1.
Hypothesized effects of acupuncture for dysphagia in head and neck cancer
Solid curve lines: pathological damage of chemoradiation therapy;
Dash lines: potential effects of acupuncture on pathological factors of dysphagia;
Downward small arrows: inhibitory effects of acupuncture;
Upward small arrows: stimulating effects of acupuncture.
This paper addresses some of unique challenges related to study design and development of protocols in nonpharmacological, sham controlled acupuncture trials. The primary aims of this study are to collect preliminary data on the efficacy of acupuncture on dysphagia-related quality of life in HNC patients receiving chemoradiation therapy, while assessing the feasibility of recruiting and retaining patients into a randomized sham-controlled acupuncture trial. The secondary aim of the study is to preliminarily explore the biological mechanisms of acupuncture on dysphagia.
2. Materials and Methods
2.1 Overview of study design
This study is a pilot randomized, sham-controlled trial of acupuncture for HNC patients with dysphagia after chemoradiation therapy.
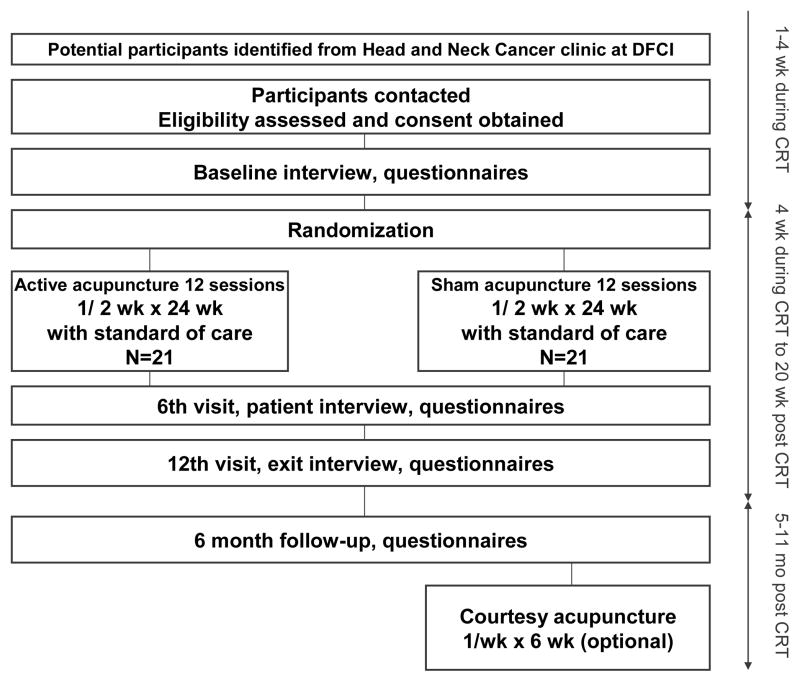
Participants who are diagnosed with squamous cell carcinoma of the head and neck receiving CRT, with or without neck dissection, and who are already undergoing swallowing therapy are randomized to 12 sessions of either active acupuncture (n=21) or sham acupuncture (n=21), over a period of 24 weeks. The primary aims of this study are to collect preliminary data on the efficacy of acupuncture in changing scores of quality of life in post CRT head and neck cancer patients. The primary outcome is change in M.D. Anderson Dysphagia Inventory score from baseline to 12 months, i.e. 6 month follow-up after completion of acupuncture treatment[32]. The feasibility of recruiting and retaining patients into a randomized sham-controlled acupuncture trial will also be assessed. Feasibility is evaluated with respect to our ability to recruit subjects, administer interventions and outcome measurements, elicit subjects’ compliance, and retain subjects in this trial. A secondary aim of the study is to preliminarily explore, in a subset of 20 participants, the biological mechanisms of acupuncture on dysphagia, through evaluation of salivary flow production, and plasma TGF-β1 and IL-6 levels.
Study participants randomized to the sham acupuncture will be offered a series of active acupuncture treatment as a courtesy at the end of the trial. Figure 2 summarizes the overall design and the flow of the patients through the study.
Figure 2.
The study design and the flow of the participants through the trial
2.2 Sponsors
This trial is funded by the National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health. The grant is awarded to Dana-Farber Cancer Institute (DFCI), Boston, Massachusetts, and all clinical work will be performed there. Acupuncture will be administered at the Leonard P. Zakim Center for Integrative Therapies (Zakim Center), DFCI. Institutional Review Boards of Harvard Medical School and the Dana-Farber/Harvard Cancer Center have approved the study and the study is registered at clinical trials.gov (Identifier: NCT00797732).
2.3 Study population and enrollment procedures
2.3.1 Study population
Participants are recruited through the Head and Neck Cancer Program at DFCI, which has a large population of HNC patients in the Boston area. Over 500 new cases of HNC are seen each year. The potential study patients are mainly squamous cell carcinoma HNC patients who are receiving curative intent CRT for stage II, III or IV, without distant metastasis. Eligibility criteria for the study are presented in Table 2.
Table 2.
Eligibility criteria of the acupuncture study for dysphagia in HNC patients
| Inclusion criteria | Exclusion criteria |
|---|---|
| Histologically or cytologically proven squamous cell carcinoma of the head and neck at stage II, III or IV, without evidence of distant metastasis Stage I disease will also be permitted if the patient is receiving CRT Primary tumor sites eligible: nasopharyngeal, oropharynx, hypopharynx or larynx, and tumors of the nasal and paranasal cavities Unknown primary squamous cell carcinoma in the neck Receiving chemoradiation Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 Adequate hematological function: neutrophil count >1.0 x109/L, platelet count >50x109/L Age ≥ 18 years Signed informed consent |
Unstable cardiac disease or myocardial infarction within 6 months prior to study entry Wearing a pacemaker or implantable cardioverter-defibrillator History of significant neurologic disorder that affects swallowing, including stroke, neurodegenerative disease, advanced dementia, or uncontrolled seizure disorder Active clinically significant uncontrolled infection Prior use of acupuncture for dysphagia Patients with uncontrolled major psychiatric disorders, such as major depression or psychosis |
The identification of potential study subjects is primarily done during weekly tumor board meeting. Identified patients who initially meet eligibility criteria, are sent an introductory letter describing the study, inviting participation, and outlining initial eligibility requirements. In the letter, those who are interested in the study will be encouraged to call or send back a permission letter to the clinical research coordinator (CRC) for more information. A face-to-face contact at regular clinical visits is another way to recruit patients; interested patients names are then forwarded to the CRC.
During the initial interview, the CRC reviews the purpose of the study and required commitment for participation, and preliminarily confirms eligibility criteria. If at the end of this interview the participant is deemed preliminarily eligible and expresses interest, the CRC schedules a meeting with one of medical oncologists at the HNC unit. The oncologist confirms all eligibility criteria and asks subjects to sign the informed consent form to participate in the study. Eligible and interested subjects are then registered and randomized to either active or sham acupuncture treatments.
The consent form specifically states that all study patients will be invited to participate in additional “mechanistic tests” (salivary flow rate and cytokine tests) during the acupuncture study. Twenty patients interested in completing the mechanistic tests are randomly selected to perform the salivary flow rate assessment and have blood drawn for plasma TGF-β1 and IL-6 at the baseline visit and at the 20-week post CRT visit, i.e. the end of acupuncture treatment.
2.3.2 Randomization and blinding procedures
Treatment assignments (active or sham acupuncture) are generated by the study statistician using a permuted block design with randomly varying block size. During the study, only treating acupuncturists and a designated unblinded study staff know the true treatment assignments of the patients. The study patients and the rest of the team members, including patients’ treating oncologists, speech-language pathologists and study CRCs are blinded to the treatment assignments throughout all follow-up visits. All information that might indicate treatment assignment, including Clinical Research Forms (CRF) with data on acupuncture needling protocols, will not be accessible by the CRC.
At a patient’s first acupuncture visit, the treating acupuncturist will not be aware of the randomized treatment assignment until the completion of the initial interview and explanation of the acupuncture procedure. They will obtain results of randomization by calling the central trial quality office immediately prior to beginning the first needling procedure.
2.4 Overview of acupuncture interventions
The acupuncture protocol outlined below is based on a comprehensive and systematic review of the published evidence, in combination with the clinical experience of our Zakim Center oncology acupuncture group. The reviewed literature includes: 1) an English- and Chinese-language peer-reviewed clinical and basic studies of acupuncture used for dysphagia; and 2) English- and Chinese-language acupuncture text books that describe treatment strategies for dysphagia[33, 34]. Our Zakim Center clinical team includes 5 practitioners with an average of 15 years of training, all of whom have specific expertise in oncology and who have participated in prior NIH studies evaluating acupuncture for cancer patients.
Our systematic review identified 7 papers with information on protocols and 6 primary text books. Data from this review were summarized and synthesized, presented to and extensively discussed by study team, with the resulting protocol arrived at by consensus [15, 16, 19, 33–43].
As indicated by the results of the review, according to TCM, key imbalances of HNC-related dysphagia include local “heat toxin” from radiation, weakness in muscles, and “stagnation of Qi and blood” (inflammation). Consequently, our treatment strategy includes acupuncture points and needle stimulation strategies that “sedate fire”, “clear heat”, “invigorate blood” and “reduce stagnation”. These classical concepts coincide with the purported anti-inflammatory and neuromuscular stimulation effects of acupuncture discussed in the previous section[21–23, 25, 26, 44] (Figure 1) . A summary of acupuncture points, locations and related nerve innervations for the study of dysphagia is presented in Table 3.
Table 3.
Acupuncture points, locations and related nerve innervations for the study of dysphagia
| Name | Chinese Pinyin Name | Location | Innervations |
|---|---|---|---|
| GV24 | Shenting | 0.5 cun§§ directly above midpoint of anterior hairline. | The branch of the frontal nerve. |
| GV20 | Baihui | On the midline of the head; 7 cun directly above posterior hairline; approximately on midpoint of line connecting apexes of two auricles. | The branch of the great occipital nerve. |
| SI16 | Tianchuang | In the lateral aspect of the neck, in the posterior border of m. sternocleidomastoideus, posterosuperior to Futu. | The cutaneous cervical nerve, the emerging portion of the great auricular nerve. |
| GB20 | Fengchi | In the depression between the upper portion of m. sternocleidomastoideus and m. trapezius, on the same level with Fengfu. | The branch of the lesser occipital nerve. |
| CV24 | Chengjiang | In the depression in the centre of the mentolabial groove. | The branch of the facial nerve. |
| CV23 | Lianquan | Above the Adam’s apple, in the depression of the upper border of the hyoid bone. | The branch of the cutaneous cervical nerve, the hypoglossal nerve, and the branch of the glossopharyngeal nerve. |
| ST7 | Xiaguan | At the lower border of the zygomatic arch, in the depression anterior to the condyloid process of the mandible. This point is located with the mouth closed. | The zygomatic branch of the facial nerve and the branches of the auriculotemporal nerve. |
| ST6 | Jiache | One finger-breadth anterior and superior to the lower angle of the mandible where m. masseter attaches at the prominence of the muscle when the teeth are clenched. | The great auricular nerve, facial nerve and masseteric nerve. |
| ST5 | Daying | Anterior to the angle of mandible, on the anterior border of the attached portion of m. masseter, in the groove-like depression appearing when the cheek is bulged. | The facial and buccal nerves. |
| LI2 | Erjian | On the radial side of the index finger, distal to the metacarpal-phalangeal joint, at the junction of the red and white skin. The point is located with the finger slightly flexed. | The dorsal digital nerve of the radial nerve, and the palmar digital proprial nerve of the median nerve. |
| LI11 | Quchi | When the elbow is flexed, the point is in the depression at the lateral end of the transverse cubital crease, midway between Chize and the lateral epicondyle of the humerus. | The posterior antebrachial cutaneous nerve; deeper, on the medial side, the radial nerve. |
| ST36 | Zusanli | 3 cun below Dubi, one finger-breadth from the anterior crest of the tibia, in m. tibialis anterior. | Superficially, the lateral aural cutaneous nerve and the cutaneous branch of the saphenous nerve; deeper, the deep peroneal nerve. |
| Sp9 | Yinlingquan | On the lower border of the medial condyle of the tibia, in the depression on the medial border of the tibia. | Superficially, in the medial crural cutaneous nerve; deeper, the tibial nerve. |
| Sp6 | Sanyinjiao | 3 cun directly above the tip of the medial malleolus, on the posterior border of the medial aspect of the tibia. | Superficially, the medial crural cutaneous nerve; deeper, in the posterior aspect, the tibial nerve. |
| K3 | Taixi | In the depression between the medial malleolus and tendo calcaneus, at the level with the tip of the medial malleolus. | The medial crural cutaneous nerve, on the course of the tibial nerve. |
| Extra | Yintang | Midway between the medial ends of the two eyebrows. | N/A |
cun, a measuring unit in acupuncture, approximately 1 inch
There is currently no consensus regarding the ideal sham acupuncture intervention[45–48]. We have chosen to use a minimally invasive, shallow insertion control for a number of reasons. First, compared to our active TCM protocol, we believe our sham intervention is relatively inert. As discussed below in more detail, we employ very small and thin needles, and insert them shallowly, away from acupuncture points and meridians, and with minimal stimulation. Preliminary results from our previous study with cancer patients[49] suggest a significant difference between this sham approach and more vigorous active needling. Second, we have previously demonstrated that this method results in patients remaining blinded with respect to treatment allocation[49]. Therefore, the particular sham intervention we are using allows us to test the effect of active, clinically relevant treatments from non-specific effects of needle insertion and patient-practitioner interaction.
To assure consistent and high quality treatment and high fidelity to protocols, all treatments take place in the Zakim Center at DFCI and are administered by experienced, licensed and credentialed staff acupuncturists. All acupuncturists graduated from TCM medical schools in China with the same acupuncture training, and have a minimum of 10 years experience in practice. They have also participated in prior NIH-funded acupuncture trials for cancer patients. Protocol-specific trainings for treating acupuncturists are conducted prior to the study and throughout the study period. The study principal investigator periodically audits the study records to ensure the fidelity of acupuncture performance.
2.4.1 Active acupuncture procedure
The active protocol uses a unique, three-phase step-up protocol to gradually increase treatment area and treatment intensity. Based on our experiences in prior trials and in the Zakim Clinic, this protocol reduces the initial anxiety of patients to the treatment and maximizes the treatment intensity. The three phases of treatment are presented in Table 4.
Table 4.
Acupuncture treatment strategy and treatment phases for HNC patients with dysphagia
| Phases of Treatment | Treatment Intention | Treatment Visits | Points, Stimulation and Number of Needles |
|---|---|---|---|
| 1 | Reduce anxiety regarding needling; familiarize patient with procedure; initiate body response | 1st and 2nd | ST36, SP9, K3, LI11, GV20, GV24, Yintang; mild; 13 needles*** |
| 2 | Increase intensity; expand to facial area; continue body response | 3rd–7th | Add LI2, ST7, ST5, CV24; Add electroacupuncture moderate; 22 needles |
| 3 | Increase intensity; expand to the back and front of neck; maximize body response | 8th–12th | Add SI16, GB20, CV23, continue electroacupuncture; 27 needles |
‘Acupuncture point selection will remain at phase one until the 4th week post CRT, regardless of the number of acupuncture sessions received.
Patients lie supine on a massage table with their arms and legs exposed. The skin on the acupuncture points is prepared with 70% ethyl alcohol. Acupuncture needles (Vinco, Helio Medical Supplies, 36 or 32 gauge, 0.20–0.25 x 25–40 mm) are inserted into acupuncture points bilaterally. The depth of insertion at each point is between 5–10 mm, except for points on the head and neck, which are between 2–5 mm. After insertion, acupuncture needles are manually manipulated in order to obtain the De Qi sensation. The De Qi sensation is defined as the acupuncturist feeling a tugging or grasping sensation from the needle manipulation and the patient feeling mild soreness, fullness, heaviness or local distension at local needling sites. The De Qi sensation is required on at least 2 points bilaterally on the lower extremity and at least 1 point bilaterally on the upper extremity. During the treatment protocol, and after De Qi is obtained, electroacupuncture is administered to a subset of acupuncture points. One pair of microalligator clips from the AWQ-104L electroacupuncture machine (Lhasa OMS, Inc.) is connected with the needles at GV20 and Yintang, with the negative pole on the GV20 and the positive pole on the Yintang. The stimulation frequency is set at 4 Hz and the pulse width at 350 μs, with a continuous wave pattern that is well-tolerated by the patient. The patient is asked to report sensations and should feel comfortable with the intensity of the electrostimulation. A TDP CQ-27 infrared heat lamp (Lhasa OMS, Inc) is turned on and is placed about 30 cm above the legs of the patient for warmth. The needles remain in place for 30 minutes. The patient is left alone in the treatment room with dimmed lights. A call bell is available to the study patient during the treatment period. After 30 minutes of treatment, needles are manually manipulated again before removal. De Qi sensation is not required at this time. A complete list of points that are used in active treatments is listed in Table 3. A total of 13, 22 and 27 needles are used during each acupuncture session at each of three phases respectively. Acupuncture point selection will remain at phase one until the 4th week post CRT, regardless of the number of acupuncture sessions received. This ensures that no needles are placed around the chin and neck area during CRT. Electrostimulation starts at the 3rd visit.
2.4.2. Sham acupuncture protocol
The sham intervention is designed to be maximally inert and minimally invasive while simulating most aspects of the active protocol. To minimize stimulation, very thin acupuncture needles (Seirin brand J type, size #02; 0.12 mm x 30 mm) are used. Seirin brand needles are manufactured with a special silicon coating on the tip and body of the needle to ensure smooth insertion. According to a needle test report published by Material Research & Testing Institute, Bauhaus University, Weimar, the Seirin needle requires approximately 30% of the force to insert the needle into a skin-like dermafoil as compared with other acupuncture needles. The #02 needle is the thinnest acupuncture needle available on the market. Needle insertion is limited to 0.2 mm to 0.5 mm in depth, and no needle manipulation is performed after the needle insertion; eliciting De Qi is prohibited. Sham needles are inserted at 14 locations paralleling the same body regions needled in the active group. Point locations include: 2 on each arm; 2 on the top of the head; 1 on the neck; and 3 on each leg.
All the sham points are administered bilaterally except No 6. and No. 7. All sham acupuncture locations are off the pathways of meridians and acupuncture points according to TCM theory. The number of needles used mirrors the phases of treatment in the active arm. Table 5 presents the locations of the sham acupuncture points.
Table 5.
Sham acupuncture point locations
| Sham points | Anatomical Locations |
|---|---|
| No 1. | 3 cun above the tip of the medial malleolus, 2 cun posterior to the posterior border of the medical aspect of tibia. |
| No 2. | 2 cun above the superior lateral border of the patella and 2 cun posterior to the line of connecting with the Anterior Superior Iliac Spine (ASIS) |
| No. 3 | 1 cun above the superior medial border of the patella and 1 cun posterior. |
| No. 4 | 3 cun above crease of wrist on the posteriorlateral aspect of the forearm, midway between TW 6 (Zhiguo) and LI 6 (Pianli). |
| No. 5 | On the lateral side of the upper arm, 1 cun above LI11(Quchi), midway between LI12(Zhouliao) and the pathway of Lung meridian. |
| No 6. | 3 cun directly above the midpoint of the anterior hairline and 1 cun lateral to the midline on the right side. |
| No 7. | 3 cun directly above the midpoint of the anterior hairline and 1 cun lateral to the midline on the left side. |
| No 8. | 1 cun directly below the depression posterior and inferior to the mastoid process, GB12 (Wangu) |
An electroacupuncture stimulation device identical to the one used in the active treatment arm is used. The internal electrical wires are disconnected so that no electric current will pass through. The green light on the device that indicates an “on” status is activated during each treatment. The wires are connected to the needles at sham points No. 6 and No. 7. The sham procedures related to the use of the heat lamp include the placement of the lamp at a greater distance from the body to minimize the therapeutic effect. These methods have been used in other studies[49–51].
2.4.3 Effective masking of treatment allocation and blinding
A number of measures will be taken to assure effective patient masking and blinding of treatment allocation. To draw attention away from the treatments, an eye pillow will be used in both the active and sham arms during each visit. To minimize differences between sham and active group, all treating acupuncturists are trained to follow a scripted standard operating procedure. Discussing treatment procedures with study subjects is prohibited.
To monitor one key aspect of quality of the needling technique, the treating acupuncturist verbally asks the patient the following questions right after the completion of the needling procedure at each session: “Would you please tell me the level of overall sensation you just experienced during the needling process, where zero (0) is you did not feel the needling sensation at all and ten (10) is the strongest you could imagine? Please account for all sensations you experienced, e.g. tingling or numbness, not just pain.” The patient’s answer is documented on the CRF.
2.5 Outcome measures
All outcome measures are assessed by a CRC, blinded to treatment assignment. The primary clinical outcomes are changes in MDADI score from baseline to 12 months from baseline (i.e. 6 months follow-up after acupuncture). We have chosen this time frame because other studies suggest that swallowing function after CRT reaches a steady state that is representative of long-term outcome at approximately 12 months after therapy. Additional outcome measures include changes from baseline in MDADI at 20 weeks post CRT, i.e. end of acupuncture treatment, and other QOL questionnaires with changes from baseline in scores at 20 weeks post CRT; changes from baseline in weight at 20 weeks post CRT; and time-to-removal of feeding tube from baseline to the event. Table 6 summarizes all outcomes measurements.
Table 6.
Summary of outcome measures and testing schedule
| Assessment | Description | Baseline | @2nd Tx | @ 4 wk post CRT | @ 8 wks post CRT | @ 12 wk post CRT | @20 wk post CRT | @ 12 mos from baseline |
|---|---|---|---|---|---|---|---|---|
| History/physical | Cancer history and treatment | x | ||||||
| Weight | Weight changes | x | x | x | x | x | x | |
| Feeding Tubes | Presence and absence of feeding tube and time-to-removal | x | x | x | x | x | x | |
| QOL: MDADI | Dysphagia specific QOL | x | x | x | x | x | x | |
| QOL: FACT-H&N | General cancer plus HNC QOL | x | x | x | x | x | x | |
| QOL: XQ | Xerostomia specific QOL | x | x | x | x | x | x | |
| Dietary Consistency | Monitor dietary continuum | x | x | x | x | x | x | |
| TCS | Monitor treatment expectation and credibility | x | x | |||||
| Blinding | Assess treatment blinding effect | x | x | |||||
| VFSS study* | Assess the oral pharyngeal and esophageal stages of deglutition | x | ||||||
| Salivary flow rate* | Assess salivary flow production | x | x | |||||
| TGF-β1*/IL-6* | Assess TGF-β1/IL-6 levels | x | x |
MDADI: The M.D. Anderson Dysphagia Inventory
FACT-H&N: The Functional Assessment of Cancer Therapy-Head and Neck
XQ: Xerostomia Questionnaire
TCS: Treatment Credibility Scale
VFSS: Videofluorographic swallowing study
only patients who participate the mechanistic tests need to take these tests.
2.5.1 M.D. Anderson Dysphagia Inventory (MDADI)
Our primary outcome is dysphagia-related QOL as measured by the MDADI. The MDADI is a validated, self-administered questionnaire specifically for dysphagia in HNC patients[32]. It is considered the best measure of QOL for this specific population, with a high reliability and sensitivity (Cronbach α =0.85–0.93), and has been used in a number of prior studies[32, 52–56]. This questionnaire is designed to characterize how patients view their swallowing ability as a result of treatment and how the swallowing dysfunction affects their quality of life. The MDADI can be used to track the longitudinal course of individual patient’s outcomes.
The MDADI has four sub-scales: global, emotional, physical, and functional, which were developed to characterize effects of dysphagia on different aspects of QOL. Five responses to items on the MDADI are printed for each item: strongly agree, agree, no opinion, disagree, and strongly disagree, and are scored on a scale of 1–5. Total scores range from 20 to 100, with 20 being low-functioning and 100 being high functioning.
2.5.2 Xerostomia Questionnaire (XQ)
The XQ is a validated 8-item questionnaire that specifically measures radiation-induced xerostomia in HNC patients. It has been used in a number of studies evaluating treatment effects in HNC patients[57–59]. It has been shown to have high reliability and sensitivity (test-retest correlation coefficient γ =0.82, p<0.01). Patients rate each symptom on an 11-point ordinal Likert scale from 0 to 10, with higher scores indicating greater dryness or discomfort due to dryness. The questions are equally divided into 4 items related to dryness while eating or chewing and 4 items related to dryness while not eating or chewing. Each item score is added, and the sum is transformed linearly to produce the final summary score ranging between 0 and 100, with higher scores representing greater level of xerostomia.
2.5.3 The Functional Assessment of Cancer Therapy-Head and Neck Scale (FACT-H&N)
The FACT-G (General) is a multidimensional quality of life instrument specifically designed for use with cancer patients[60]. The FACT-G consists of a 28-item core that can be supplemented by site and /or treatment specific subscales, including a HNC specific subscale (FACT-H&N)[60, 61]. The FACT-H&N has been shown to be reliable in HNC patients (coefficient α=0.70 for 9-item HNS). The FACT-H&N is a self-reported instrument consisting of 28 general plus 11 head and neck specific items, each rated on a 0 to 4 Likert-type scale. Items are combined to describe patient functioning in six areas: physical well-being, social and family well-being, relationship with doctor, emotional well-being, functional well-being and head and neck related symptoms including dysphagia. Higher scores represent better quality of life.
2.5.4 Expectation and Treatment Credibility Scale
Patients’ beliefs or expectations regarding the efficacy of acupuncture for treating dysphagia are assessed using a self-administered Treatment Credibility Scale (TCS) (scale 0–4, 4=greatest expectancy) developed by Borkovec and Nau, and modified for acupuncture studies[62, 63]. The instrument is administered at the baseline, second visit, and end of the study to assess the effectiveness of blinding.
2.5.5 Mechanistic Measurements
2.5.5.1 Salivary flow rate evaluation
Tests are done with unstimulated as well as stimulated methods following standard protocols[64]. During unstimulated saliva collections, patients are seated with eyes open and head tilted slightly forward and given instructions to minimize orofacial movements and to avoid sucking or swallowing, to prevent the influence on salivary flow[64]. Collections are performed between 9:00 am and noon to minimize diurnal variation. Patients are asked to refrain from eating, drinking, and performing oral hygiene for a minimum of 90 min before saliva collection. Just before collection, patients are instructed to swallow and then spit accumulating saliva into a preweighed 50-mL polycarbonate vial continuously for 5 min without swallowing. Stimulated collections consist of an initial swallowing, then the swabbing of 2% citric acid with cotton-tipped applicators to the lateral tongue bilaterally 5 times over a 2-min period, emptying the mouth, then collecting saliva into a polycarbonate tube, as above. Unstimulated and stimulated whole-mouth salivary flow rates are measured at the baseline visit and after the completion of 12th acupuncture treatment.
2.5.5.2 Plasma TGF-β1 and IL-6
Plasma TGF-β1 is a cytokine that reflects tissue fibrosis process. IL-6 is a major pro-inflammatory cytokine that is especially important in the initiation, development and prognosis of head and neck cancer[65, 66].
Study samples of plasma TGF-β1 and IL-6 are sent to R&D Systems, Inc. for testing results. Briefly, for each sample, 5 mL of venous blood are collected into polypropylene tube on ice using EDTA as an anticoagulant. The plasma is centrifuged for 15 minutes within 30 minutes of collection and stored at <−70 °C[67]. Plasma TGF-β1 and IL-6 level are determined by ELISA using monoclonal anti-human TGF-β1 and IL-6 antibodies according to manufacturer’s instructions (R&D Systems, Inc. USA). Samples are collected at the baseline visit and at the completion of the 12th acupuncture treatment. All study samples for a given individual will deidentified and analyzed in batch; each batch includes a quality control (QC) sample.
2.5.6. Other secondary outcomes
Other secondary outcomes including changes of weight, PEG tube duration, and dietary consistency. These data will be extracted from patients’ medical records by the study CRC. In addition, data from a video fluorographic swallowing study will be exploratory measured in patients who are required to undergo the study as part of clinical practice.
2.5.6 Adverse Events
The safety of the acupuncture intervention is evaluated by documenting any symptoms possibly related to acupuncture at each acupuncture visit, which includes bleeding, bruising at needling sites, pain level, and fatigue. The treating acupuncturist records these items and documents them in a toxicity form. All adverse events will be reported to the DFCI IRB and the protocol sponsor.
Care will be available for any sequelae that may occur. Each patient will have usual access to their primary physician and oncologist. All intervention sessions will be held in DFCI where an emergency code cart and hospital code team are immediately available at all times.
To minimize risks, this trial requires all acupuncturists to have high standards of education and experience, and to observe the state requirement of using one-time-use disposable sterile needles.
2.6 Statistical Analysis Size and Power
2.6.1 Statistical analysis
The primary outcome is change in M.D. Anderson Dysphagia Inventory score from baseline to 12 months (6 month post acupuncture treatment) between the active acupuncture and sham acupuncture arms. This study will provide preliminary estimates of the differences between sham and active acupuncture as well as estimates of the standard deviations of change (from baseline) for each of the outcome measures. This information will inform the design and sample size for a definitive study. A secondary aim of the analyses is to compare both groups with respect to changes between baseline and 20 weeks post CRT for MDADI scores and all other QOL questionnaires; and to compare groups with respect to time-to-removal of feeding tube.
To assess the feasibility of conducting a trial of acupuncture for HNC patients, we use screening logs to determine the proportion of screened patients who are eligible and the proportion of eligible patients who enroll in the study. We track factors that make subjects ineligible, and for unwilling eligible subjects, reasons for not participating. We measure compliance through attendance at treatments. Participants who attend at least 80% of the target number of treatments are considered protocol compliant. Overall, we will consider further study feasible if at least 75% of intervention participants are compliant and at least 80% of participants in each group complete all study evaluations (i.e., baseline, 2nd treatment, 4 weeks, 8 weeks, 12-weeks, 20 weeks post CRT, and at 6 months post acupuncture, i.e., 12 months from baseline), and we are able to recruit patients at the anticipated rate.
We will conduct all primary analyses according to the intention-to-treat paradigm using the Wilcoxon rank-sum test. As a non-parametric test, the Wilcoxon test is conservative, less sensitive to outliers in smaller samples, and does not require the assumption of normality. Exploratory secondary analyses include fitting ordinary least squares regression models to evaluate the association between the primary outcomes and a variety of possible predictors (e.g., severity of dysphagia, age, tumor site, radiation dose, etc). We will also test blinding, expectancy and perceived intensity of acupuncture needling and other effect modifiers. The goals are to identify factors that need to be included in the design of a definitive study (i.e., stratification factors) and to identify interesting associations for further investigation (i.e., hypothesis generation). Individual missing items in multi-item scales will be handled as recommended by the scale developers. For missing data due to loss to follow-up or other reasons for non-response, we will employ multiple imputation methods to adjust for the missing data. We will use an imputation model that accounts for the longitudinal structure of the missing data.
2.6.2 Sample Size and Statistical Power
Sample size calculations are based on the primary outcome, MDADI. According to Chen, the lead developer of the MDADI[32], a difference of 20 points is considered clinically significant (AY Chen, personal communication). Only one study provides data on the standard deviation of change in MDADI[53], but in a different subpopulation of HNC, and at 12 months follow-up rather than 6 months. The observed standard deviation in their study was 17.1 points. Allowing for a 20% loss to follow-up and a 10% loss in efficiency for the nonparametric test (relative to a t-test), we estimate that a sample size of 21 per treatment group will provide 90% power to detect a 20 point difference between active and sham acupuncture.
3. Discussion
The design of this study takes into account a number of unique aspects of nonpharmacological trials, particularly issues for sham controlled acupuncture trials[47]. This includes developing an evidence-based standardized active treatment protocol, selecting an appropriate sham control, and maintaining the effectiveness of blinding.
Developing a standardized active treatment protocol of acupuncture is an imperative step for clinical trials[68]. STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) provides an excellent guidelines[69]. Although acupuncture has been practiced for several thousand years, standardized or validated treatment protocols for most biomedical conditions do not exist. In this study, we used a systematic and evidence-based approach, combined with a consensus building process, to develop both active and sham protocols. Our approach not only identify acupuncture points most relevant for treating HNC patients undergoing CRT, but also identified other key protocol components such as depth of needling, intensity of needling stimulation, frequency of treatments, and strategies to gradually escalate the treatment intensity. The resulting protocol thus represents a strong test of the potential effects of acupuncture for this population.
There is substantial debate regarding the optimal sham control for an acupuncture trial. Sham intervention ideally should mimic the procedure of acupuncture without eliciting therapeutic effects[48]. However, it has been suggested that sham acupuncture needling also evokes physiological responses that are similar to real acupuncture needling, and this may explain why effect sizes in many sham controlled studies are small[45, 46, 70, 71]. For this reason, some have argued that using non-invasive acupuncture needles as sham control is a better approach than the minimally invasive needling approach we are employing[71, 72]. Because of the smaller needle diameter, softer needle body, and very shallow insertion we are employing in this study, we believe the stimulation will be quite minimal, and perhaps even less strong than non-insertive controls that often apply significant surface pressure. The intent of our method is to minimize stimulating effects of needling and to avoid the activation of sensory receptors. Nevertheless, the subtle effect of needling procedure on the system cannot be completely discounted. Therefore, this study represents a rigorous test of specific effects of acupuncture needling.
Sham-controlled acupuncture trials closely resemble many aspects of sham surgical trials[73]. While sensory acuity of study participants is usually suppressed by anesthesia in sham surgical trials, participants in sham controlled acupuncture trials are fully aware of the entire needling process. Therefore, maintaining an effective blinding in acupuncture procedure poses a great challenge. This is particularly important since our IRBs request explicit statements in the consent form to inform study participants regarding the use of sham acupuncture. Therefore, all study participants clearly understand that there is a chance to be randomized into a “sham control”. Because of possible bias that may develop due to incomplete blinding, we will assess the effectiveness of blinding by using the credibility scale in our secondary analysis[50], and these blinding outcomes will be used as potential confounders in secondary analyses.
Overall, our protocol design follows three principles: 1. collecting the best evidence available to determine a valid and maximally effective acupuncture protocol for a specific clinical condition; 2. minimizing the variability of acupuncture performance by using standardization operation procedures, repeat protocol training, and constant monitoring; and, 3. maximizing the potentially therapeutic differences between protocol parameters in the active acupuncture and the sham acupuncture.
The preliminary evidence generated from this study will be used to evaluate the value of acupuncture as an intervention for radiation induced dysphagia in head and neck cancer patients. If the results are positive, the data collected from this study will be used to design and inform a larger definitive study to fully evaluate the clinically meaningful effects of acupuncture for this group of patients and an exploratory study to further evaluate the mechanisms underlying acupuncture’s effect on HNC-related dysphagia.
Acknowledgments
This study is supported by grant 1K01 AT004415 from the National Center for Complementary and Alternative Medicine (NCCAM).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Peter M. Wayne, Email: peter_wayne@hms.harvard.edu.
Roger B. Davis, Email: rdavis@bidmc.harvard.edu.
Julie E. Buring, Email: jburing@rics.bwh.harvard.edu.
Hailun Li, Email: hailunli@jimmy.harvard.edu.
Laura A. Goguen, Email: lgoguen@partners.org.
David S. Rosenthal, Email: drose@uhs.harvard.edu.
Roy B. Tishler, Email: rtishler@lroc.harvard.edu.
Marshall R. Posner, Email: marshall.posner@mssm.edu.
Robert I. Haddad, Email: Robert_Haddad@dfci.harvard.edu.
References
- 1.Nguyen NP, Moltz CC, Frank C, Vos P, Smith HJ, Karlsson U, et al. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann Oncol. 2004;15:383–8. doi: 10.1093/annonc/mdh101. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen NP, Moltz CC, Frank C, Vos P, Smith HJ, Nguyen PD, et al. Impact of swallowing therapy on aspiration rate following treatment for locally advanced head and neck cancer. Oral Oncol. 2006 doi: 10.1016/j.oraloncology.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen NP, Sallah S, Karlsson U, Antoine JE. Combined chemotherapy and radiation therapy for head and neck malignancies: quality of life issues. Cancer. 2002;94:1131–41. doi: 10.1002/cncr.10257. [DOI] [PubMed] [Google Scholar]
- 4.Connor NP, Cohen SB, Kammer RE, Sullivan PA, Brewer KA, Hong TS, et al. Impact of conventional radiotherapy on health-related quality of life and critical functions of the head and neck. Int J Radiat Oncol Biol Phys. 2006;65:1051–62. doi: 10.1016/j.ijrobp.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 5.Duncan GG, Epstein JB, Tu D, El Sayed S, Bezjak A, Ottaway J, et al. Quality of life, mucositis, and xerostomia from radiotherapy for head and neck cancers: a report from the NCIC CTG HN2 randomized trial of an antimicrobial lozenge to prevent mucositis. Head Neck. 2005;27:421–8. doi: 10.1002/hed.20162. [DOI] [PubMed] [Google Scholar]
- 6.Lazarus CL, Logemann JA, Pauloski BR, Rademaker AW, Larson CR, Mittal BB, et al. Swallowing and tongue function following treatment for oral and oropharyngeal cancer. J Speech Lang Hear Res. 2000;43:1011–23. doi: 10.1044/jslhr.4304.1011. [DOI] [PubMed] [Google Scholar]
- 7.Pauloski BR, Logemann JA. Impact of tongue base and posterior pharyngeal wall biomechanics on pharyngeal clearance in irradiated postsurgical oral and oropharyngeal cancer patients. Head Neck. 2000;22:120–31. doi: 10.1002/(sici)1097-0347(200003)22:2<120::aid-hed3>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 8.Pauloski BR, Logemann JA, Rademaker AW, McConnel FM, Stein D, Beery Q, et al. Speech and swallowing function after oral and oropharyngeal resections: one-year follow-up. Head Neck. 1994;16:313–22. doi: 10.1002/hed.2880160404. [DOI] [PubMed] [Google Scholar]
- 9.Ezzo JM, Richardson MA, Vickers A, Allen C, Dibble SL, Issell BF, et al. Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev. 2006:CD002285. doi: 10.1002/14651858.CD002285.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Shen J, Wenger N, Glaspy J, Hays RD, Albert PS, Choi C, et al. Electroacupuncture for control of myeloablative chemotherapy-induced emesis: A randomized controlled trial. JAMA. 2000;284:2755–61. doi: 10.1001/jama.284.21.2755. [DOI] [PubMed] [Google Scholar]
- 11.Walker EM, Rodriguez AI, Kohn B, Ball RM, Pegg J, Pocock JR, et al. Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: a randomized controlled trial. J Clin Oncol. 2010;28:634–40. doi: 10.1200/JCO.2009.23.5150. [DOI] [PubMed] [Google Scholar]
- 12.Pfister DG, Cassileth BR, Deng GE, Yeung KS, Lee JS, Garrity D, et al. Acupuncture for pain and dysfunction after neck dissection: results of a randomized controlled trial. J Clin Oncol. 2010;28:2565–70. doi: 10.1200/JCO.2009.26.9860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gou AC. In: The Translation and Edited Yellow Emperor’s Classic of Internal Medicine. 1. Jing Ling Shu., editor. Tianjing: Tianjing Science and Technology Publishing House; 1989. [Google Scholar]
- 14.Shen H, Shen CX. Acupuncture treatment on “Tian Tu” (CV22) for dysphagia in advanced esophageal cancer; a 120 cases report. Zhejiang Journal of Traditional Chinese Medicine. 1996;31:561. [Google Scholar]
- 15.Zheng P, Ruan J. Effect of acupuncture combined with psychotherapy on quality of life in patients with nasopharyngeal cancer in post radiation therapy. Chinese Journal of Information on Traditional Chinese Medicine. 2002;9:63–4. [Google Scholar]
- 16.Zhou H, Zhang P. Effect of swallowing training combined with acupuncture on dysphagia in nasopharyngeal carcinoma after radiotherapy (in Chinese) Chinese Journal of Rehabilitation in Theory and Practice. 2006;12:58–9. [Google Scholar]
- 17.Lu W, Posner MR, Wayne P, Rosenthal DS, Haddad RI. Acupuncture for dysphagia after chemoradiation therapy in head and neck cancer: a case series report. Integr Cancer Ther. 2010;9:284–90. doi: 10.1177/1534735410378856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nowicki NC, Averill A. Acupuncture for dysphagia following stroke. Medical Acupuncture. 2003;14:17–9. [Google Scholar]
- 19.Wang LP, Xie Y. Systematic evaluation on acupuncture and moxibustion for treatment of dysphagia after stroke. Zhongguo Zhen Jiu. 2006;26:141–6. [PubMed] [Google Scholar]
- 20.Seki T, Iwasaki K, Arai H, Sasaki H, Hayashi H, Yamada S, et al. Acupuncture for dysphagia in poststroke patients: a videofluoroscopic study. J Am Geriatr Soc. 2005;53:1083–4. doi: 10.1111/j.1532-5415.2005.53338_11.x. [DOI] [PubMed] [Google Scholar]
- 21.Seki T, Kurusu M, Tanji H, Arai H, Sasaki H. Acupuncture and swallowing reflex in poststroke patients. J Am Geriatr Soc. 2003;51:726–7. doi: 10.1034/j.1600-0579.2003.00227.x. [DOI] [PubMed] [Google Scholar]
- 22.Chen J, Xiang B, Yuan H, Xu B. The effects of acupuncture treatment on acute cerebral infarction and the relation with interleukin-6. Journal of Taishan Medical College ( in Chinese) 2006;27:562–3. [Google Scholar]
- 23.Ma X-p, Min Y-j, Wu H-g, Shi Z, Zhao TP, Qi L-z, et al. Effects of electroacupuncture on expression of TGF-β1 and its receptor in rats with hepatic fibrosis. Chinese Archives of Traditional Chinese Medicine ( in Chinese) 2009;27:1616–18. [Google Scholar]
- 24.Xiao Y, Du Y, Li T, Liu X, Shi X. Effects of acupuncture at “Neiguan” (PC 6) on inschemic myocardial bFGF and TGF-β1 expression in rats. Zhen Ci Yan Jiu ( in Chinese) 2002;27:130–35. [Google Scholar]
- 25.Zhuang Z, Wang D, Tang F, Wu L, Li X. Effects of acupuncture on neurofunction, hemorheology and inflammatory factors in radiculitis rats. Journal of Guangzhou University of Traditional Chinese Medicine (in Chinese) 2006;23:513–17. [Google Scholar]
- 26.Zhang W, Liu ZS, Sun SC, Huang M, Liu YS. Study on mechanisms of acupuncture treatment for moderate-severe dysphagia at chronic stage of appoplexy. Zhonguo Zhen Jiu. 2002;22:405–7. [Google Scholar]
- 27.Deng G, Hou BL, Holodny AI, Cassileth BR. Functional magnetic resonance imaging (fMRI) changes and saliva production associated with acupuncture at LI-2 acupuncture point: a randomized controlled study. BMC Complement Altern Med. 2008;8:37. doi: 10.1186/1472-6882-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blom M, Dawidson I, Angmar-Mansson B. The effect of acupuncture on salivary flow rates in patients with xerostomia. Oral Surg Oral Med Oral Pathol. 1992;73:293–8. doi: 10.1016/0030-4220(92)90124-9. [DOI] [PubMed] [Google Scholar]
- 29.Braga FP, Sugaya NN, Hirota SK, Weinfeld I, Magalhaes MH, Migliari DA. The effect of acupuncture on salivary flow rates in patients with radiation-induced xerostomia. Minerva Stomatol. 2008;57:343–8. [PubMed] [Google Scholar]
- 30.Dawidson I, Blom M, Lundeberg T, Angmar-Mansson B. The influence of acupuncture on salivary flow rates in healthy subjects. J Oral Rehabil. 1997;24:204–8. [PubMed] [Google Scholar]
- 31.Cui J, Yan J. Effect of moxibustion or acupuncture at Geshu acupoint on the granulocyte-macrophage colony stimulating factor of cyclophosphamide induced leukopenic rats. Journal of Clinical Rehabilatative Tissue Engineering Research ( in Chinese) 2007;11:5473–76. [Google Scholar]
- 32.Chen AY, Frankowski R, Bishop-Leone J, Hebert T, Leyk S, Lewin J, et al. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. 2001;127:870–6. [PubMed] [Google Scholar]
- 33.Cheng XN. Chinese Acupuncture and Moxibustion. Beijing: Foreign Languages Press; 1999. p. 590. Revised Edition ed. [Google Scholar]
- 34.Qiu P-R, Chen H-P. Newly Edited Chinese Acupuncture and Moxibustion (in Chinese) 1. Shanghai: Shanghai Science and Technology Publishing House; 1992. p. 1034. [Google Scholar]
- 35.Ellis A, Wiseman N, Boss K. Fundamentals of Chinese Acupuncture. Brookline, Massachusetts: Paradigm Publications; 1988. [Google Scholar]
- 36.Ma Y-T, Ma M, Cho ZH. Biomedical Acupuncture for Pain Management. St. Louis, Missouri: Elsevier (USA); 2005. [Google Scholar]
- 37.The East Asican Medical Studies Society. Fundamentals of Chinese Medicine. Brookline, Massachusetts: Paradigm Publications; 1985. p. 606. [Google Scholar]
- 38.Yang J, Zhang J, Chen Z, He S. Acupuncture and Moxibustion, The Higher Education Reference Books for Traditional Chinese Medical Colleges. 1. Beijing, China: People’s Health Press; 1995. p. 895. [Google Scholar]
- 39.Liu ZS, Liu BY, Zhang W, Sun SC, Wang DW, Liu J, et al. Clinical study on acupuncture treatment for moderate and severe deglutition disorders at the chronic stage of apoplexy. Zhongguo Zhen Jiu. 2002;22:291–4. [Google Scholar]
- 40.Han J. Clinical observation on acupuncture treating bulbar paralysis after actue cerebrovascular accodent. Henan Journal of Practical Nervous Diseases. 2004;7:81–2. [Google Scholar]
- 41.Lou W, Huang H, Tan J, Lai Y, Huang J, He Y, et al. Clinical observation of acupuncture combined with swallowing therapy on dysphagia after stroke. Chinese Acupuncture & Moxibustion. 2004;24:528–30. [Google Scholar]
- 42.Ji Q, Xu Q, Zhou Y, Gu H, Zhang Y. Acupuncture treating peseudobular palsy-retaled dysphagia after stroke, a report of 35 cases. Shanghai Journal of Acupuncture and Moxibustion. 2004;23:11–2. [Google Scholar]
- 43.Chen X-h, Lai X-s, Chen Z-z. Clinical observation of acupuncture on pseudobulbar palsy after stroke. Chinese Acupuncture & Moxibustion. 2005;25:161–3. [PubMed] [Google Scholar]
- 44.Xiao YL, Du YH, Li T, Liu XX, Shi XM. Efect of acupuncture at “Neiguan” (PC6) on Ischemic myocardial bFGF and TGF-β1 expression in rats. Zhen Ci Yan Jiu. 2002;27:130–5. [Google Scholar]
- 45.Lund I, Naslund J, Lundeberg T. Minimal acupuncture is not a valid placebo control in randomised controlled trials of acupuncture: a physiologist’s perspective. Chin Med. 2009;4:1. doi: 10.1186/1749-8546-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lundeberg T, Lund I, Sing A, Naslund J. Is Placebo Acupuncture What It is Intended to Be? Evid Based Complement Alternat Med. 2009 doi: 10.1093/ecam/nep049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.MacPherson H, White A, Cummings M, Jobst KA, Rose K, Niemtzow RC. Standards for Reporting Interventions in Controlled Trials of Acupuncture: the STRICTA recommendations. J Altern Complement Med. 2002;8:85–9. doi: 10.1089/107555302753507212. [DOI] [PubMed] [Google Scholar]
- 48.White AR, Filshie J, Cummings TM. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complement Ther Med. 2001;9:237–45. doi: 10.1054/ctim.2001.0489. [DOI] [PubMed] [Google Scholar]
- 49.Lu W, Matulonis UA, Doherty-Gilman A, Lee H, Dean-Clower E, Rosulek A, et al. Acupuncture for chemotherapy-induced neutropenia in patients with gynecologic malignancies: a pilot randomized, sham-controlled clinical trial. J Altern Complement Med. 2009;15:745–53. doi: 10.1089/acm.2008.0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kalish LA, Buczynski B, Connell P, Gemmel A, Goertz C, Macklin EA, et al. Stop Hypertension with the Acupuncture Research Program (SHARP): clinical trial design and screening results. Control Clin Trials. 2004;25:76–103. doi: 10.1016/j.cct.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 51.Schnyer RN, Iuliano D, Kay J, Shields M, Wayne P. Development of protocols for randomized sham-controlled trials of complex treatment interventions: Japanese acupuncture for endometriosis-related pelvic pain. J Altern Complement Med. 2008;14:515–22. doi: 10.1089/acm.2007.0826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gillespie MB, Brodsky MB, Day TA, Lee FS, Martin-Harris B. Swallowing-related quality of life after head and neck cancer treatment. Laryngoscope. 2004;114:1362–7. doi: 10.1097/00005537-200408000-00008. [DOI] [PubMed] [Google Scholar]
- 53.Gillespie MB, Brodsky MB, Day TA, Sharma AK, Lee FS, Martin-Harris B. Laryngeal penetration and aspiration during swallowing after the treatment of advanced oropharyngeal cancer. Arch Otolaryngol Head Neck Surg. 2005;131:615–9. doi: 10.1001/archotol.131.7.615. [DOI] [PubMed] [Google Scholar]
- 54.Kulbersh BD, Rosenthal EL, McGrew BM, Duncan RD, McColloch NL, Carroll WR, et al. Pretreatment, preoperative swallowing exercises may improve dysphagia quality of life. Laryngoscope. 2006;116:883–6. doi: 10.1097/01.mlg.0000217278.96901.fc. [DOI] [PubMed] [Google Scholar]
- 55.Gillespie MB, Day TA, Sharma AK, Brodsky MB, Martin-Harris B. Role of mitomycin in upper digestive tract stricture. Head Neck. 2007;29:12–7. doi: 10.1002/hed.20476. [DOI] [PubMed] [Google Scholar]
- 56.Kazi R, Prasad V, Venkitaraman R, Nutting CM, Clarke P, Rhys-Evans P, et al. Questionnaire analysis of the swallowing-related outcomes following total laryngectomy. Clin Otolaryngol. 2006;31:525–30. doi: 10.1111/j.1365-2273.2006.01335.x. [DOI] [PubMed] [Google Scholar]
- 57.Lin A, Kim HM, Terrell JE, Dawson LA, Ship JA, Eisbruch A. Quality of life after parotid-sparing IMRT for head-and-neck cancer: a prospective longitudinal study. Int J Radiat Oncol Biol Phys. 2003;57:61–70. doi: 10.1016/s0360-3016(03)00361-4. [DOI] [PubMed] [Google Scholar]
- 58.Meirovitz A, Murdoch-Kinch CA, Schipper M, Pan C, Eisbruch A. Grading xerostomia by physicians or by patients after intensity-modulated radiotherapy of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2006;66:445–53. doi: 10.1016/j.ijrobp.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 59.Pacholke HD, Amdur RJ, Morris CG, Li JG, Dempsey JF, Hinerman RW, et al. Late xerostomia after intensity-modulated radiation therapy versus conventional radiotherapy. Am J Clin Oncol. 2005;28:351–8. doi: 10.1097/01.coc.0000158826.88179.75. [DOI] [PubMed] [Google Scholar]
- 60.List MA, Ritter-Sterr C, Lansky SB. A performance status scale for head and neck cancer patients. Cancer. 1990;66:564–9. doi: 10.1002/1097-0142(19900801)66:3<564::aid-cncr2820660326>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 61.List MA, D’Antonio LL, Cella DF, Siston A, Mumby P, Haraf D, et al. The Performance Status Scale for Head and Neck Cancer Patients and the Functional Assessment of Cancer Therapy-Head and Neck Scale. A study of utility and validity. Cancer. 1996;77:2294–301. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2294::AID-CNCR17>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 62.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3:257–60. [Google Scholar]
- 63.Wayne PM, Krebs DE, Macklin EA, Schnyer R, Kaptchuk TJ, Parker SW, et al. Acupuncture for upper-extremity rehabilitation in chronic stroke: a randomized sham-controlled study. Arch Phys Med Rehabil. 2005;86:2248–55. doi: 10.1016/j.apmr.2005.07.287. [DOI] [PubMed] [Google Scholar]
- 64.Parliament MB, Scrimger RA, Anderson SG, Kurien EC, Thompson HK, Field GC, et al. Preservation of oral health-related quality of life and salivary flow rates after inverse-planned intensity-modulated radiotherapy (IMRT) for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2004;58:663–73. doi: 10.1016/S0360-3016(03)01571-2. [DOI] [PubMed] [Google Scholar]
- 65.Haddad R, Sonis S, Posner M, Wirth L, Costello R, Braschayko P, et al. Randomized phase 2 study of concomitant chemoradiotherapy using weekly carboplatin/paclitaxel with or without daily subcutaneous amifostine in patients with locally advanced head and neck cancer. Cancer. 2009;115:4514–23. doi: 10.1002/cncr.24525. [DOI] [PubMed] [Google Scholar]
- 66.Van Tubergen E, Vander Broek R, Lee J, Wolf G, Carey T, Bradford C, et al. Tristetraprolin regulates interleukin-6, which is correlated with tumor progression in patients with head and neck squamous cell carcinoma. Cancer. 2011;117:2677–89. doi: 10.1002/cncr.25859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen HW, Chang YC, Lai YL, Chen YJ, Huang MJ, Leu YS, et al. Change of plasma transforming growth factor-beta1 levels in nasopharyngeal carcinoma patients treated with concurrent chemo-radiotherapy. Jpn J Clin Oncol. 2005;35:427–32. doi: 10.1093/jjco/hyi126. [DOI] [PubMed] [Google Scholar]
- 68.Langevin HM, Wayne PM, Macpherson H, Schnyer R, Milley RM, Napadow V, et al. Paradoxes in acupuncture research: strategies for moving forward. Evid Based Complement Alternat Med. 2011;2011:180805. doi: 10.1155/2011/180805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7:e1000261. doi: 10.1371/journal.pmed.1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lundeberg T, Lund I. Are reviews based on sham acupuncture procedures in fibromyalgia syndrome (FMS) valid? Acupunct Med. 2007;25:100–6. doi: 10.1136/aim.25.3.100. [DOI] [PubMed] [Google Scholar]
- 71.Shuai P, Zhou XH, Lao L, Li X. Issues of design and statistical analysis in controlled clinical acupuncture trials: An analysis of English-language reports from Western journals. Stat Med. 2011 doi: 10.1002/sim.4034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moffet HH. Sham acupuncture may be as efficacious as true acupuncture: a systematic review of clinical trials. J Altern Complement Med. 2009;15:213–6. doi: 10.1089/acm.2008.0356. [DOI] [PubMed] [Google Scholar]
- 73.Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–8. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]