Abstract
Purpose
To sensitize practitioners working with individuals with spinal cord injury to the complex life circumstances that are implicated in the development of pressure ulcers, and to document the ways that interventions can be adapted to target individual needs.
Methods
Content analysis of weekly fidelity/ quality control meetings that were undertaken as part of a lifestyle intervention for pressure ulcer prevention in community-dwelling adults with spinal cord injury.
Results
Four types of lifestyle-relevant challenges to ulcer prevention were identified: risk-elevating life circumstances, communication difficulties, equipment problems, and individual personality issues. Intervention flexibility was achieved by changing the order of treatment modules, altering the intervention content or delivery approach, or going beyond the stipulated content.
Conclusion
Attention to recurrent types of individual needs, along with explicit strategies for tailoring manualized interventions, has potential to enhance pressure ulcer prevention efforts for adults with spinal cord injury.
Target audience
This continuing education article is intended for practitioners interested in learning about a comprehensive, context-sensitive, community-based pressure ulcer prevention program for people with spinal cord injury.
Objectives
After reading this article, the reader should be able to:
Describe some of the contextual factors that increase pressure ulcer risk in people with spinal cord injury living in the community.
Distinguish between tailored and individualized intervention approaches.
Identify the issues that must be taken into account to design context-sensitive, community-based pressure ulcer prevention programs for people with spinal cord injury.
Describe approaches that can be used to individualize manualized interventions.
INTRODUCTION
People with spinal cord injury (SCI) are at high risk for developing pressure ulcers. The incidence of pressure ulcers in community-dwelling adults with SCI is more than 30% per year and up to 80% cumulatively over the course of a lifetime.1-3 Compromised mobility and sensation along with repetitive exposure to pressure, shearing and friction contribute to the development of pressure ulcers.4,5 Along with urinary tract infections, fractures, and depressive disorders, pressure ulcers are one of the most frequent causes of hospitalization in this population and also predict early mortality.5,6
Numerous factors elevate risk for pressure ulcers in SCI. With respect to physical variables, for example, people with quadriplegia, increased age at time of injury, a lengthier time since injury, or complete injury are more likely to develop pressure ulcers after SCI. 7-10 Additionally, it has been reported that the risk of developing pressure ulcers in adults with SCI is greater in the community than in acute care settings, and that multiple lifestyle-related considerations such as obesity, substance abuse, depression, activity choices, an inability to self-advocate for health care, and equipment breakdowns are ulcer risks. 10-13 Along these lines, eight key themes have been indentified that pertain to the link between lifestyle and pressure ulcer development in high-risk adults with SCI: (1) perpetual danger, (2) change or disruption of routine, (3) decay of prevention behaviors, (4) lifestyle risk ratio, (5) individualization, (6) simultaneous presence of awareness and motivation, (7) lifestyle trade-offs between the goals of activity participation and ulcer prevention, and (8) access to needed care, services, and supports.13
Our research group developed the Lifestyle Redesign Pressure Ulcer Prevention Program (LR-PUP) to address the heightened pressure ulcer risk of people with SCI living in the community. Incorporating the above themes, the intervention needed to: (a) address the perpetual danger of pressure ulcer development; (b) focus on change or disruption in routine, as such alterations heighten pressure ulcer risk; (c) respond to the complexly fluctuating risk-relevant liabilities that surface in the lives of people with SCI; and (d) address not only person factors but also access to resources, needed care, services, and support.
These provisions required that the intervention, although manualized, allow for tailoring and/ or individualization in response to the real world exigencies of daily life. In contrast to standardized interventions that are applied across all patients in the same way, both tailored and individualized interventions are customized in accordance with unique patient needs, attributes, values, goals, and life circumstances.14 The term tailored refers to intervention approaches that are guided by pre-established protocols or manuals, but nevertheless are customized to specific patient characteristics such as readiness-to-change. In contrast, individualized interventions, although having a high degree of person specificity, do not necessarily involve the use of a pre-established manual. Both tailored and individualized approaches, however, entail a high-degree of patient centeredness.14,15
Our purpose in this paper is to describe how a manualized intervention can be flexibly adapted in response to unanticipated circumstances that pose threats to skin integrity in the lives of community-dwelling people with SCI. In this regard, we typologized the emergent challenges that were faced by people with SCI who participated in a lifestyle-based pressure ulcer prevention program. We also derived a classification scheme for describing the ways in which the manualized intervention was adjusted to address such challenges.16,17
METHOD
The PUPS-RCT
The data analyzed for this paper were generated as part of an ongoing clinical trial, the Pressure Ulcer Prevention Study (PUPS-RCT), and consisted of observations stemming from weekly therapy team meetings pertaining to the first 11 participants who were randomized to the lifestyle intervention condition. Within the wider experiment, a total of 160 people with SCI who meet the eligibility criteria listed in Table 1 (80 experimental and 80 usual care control participants) will eventually be enrolled in the study. The chief purpose of the PUPS trial is to assess whether the lifestyle intervention, relative to usual care, reduces serious (stage 3 or stage 4) pressure ulcers and associated surgeries in a cost-effective manner.
Table 1.
Inclusion criteria for PUPS-RCT
| • Male or female aged 18 years or older. |
| • Consumer of health care services at Rancho Los Amigos National Rehabilitation Center (RLANRC) |
| • Spinal cord injury (paraplegia or tetraplegia). |
| • Non-ambulatory |
| • Spinal cord injury due to trauma. |
| • Spinal cord injury due to non traumatic causes are eligible if the following criteria are met: |
| • Well defined spinal cord lesion. |
| • Spinal cord lesion not expected to improve or worsen. |
| • All subjects with non-traumatic SCI may be reviewed by the investigative team or a designated staff member if there is any ambiguity regarding these inclusion criteria. |
| • Able to undergo intervention and testing in English or Spanish. |
| • At least 6 months post-injury. |
| • History of at least one serious (Stage 3 or 4) pressure ulcer in the past 5 years. |
| • No present serious (stage 3 or 4) ulcer. |
| • Cognitively intact. |
| • Personally expressed willingness to undertake recommended lifestyle changes for ulcer prevention. |
| • Can be reached by telephone. |
| • Reside in or within 100 miles of RLANRC with no plans to relocate beyond this area. |
| • Lack of participation in our preliminary research studies. |
| • Agreement to participate and completion of consent form. |
| • Not participating in the neuromuscular stimulation study. |
The Intervention
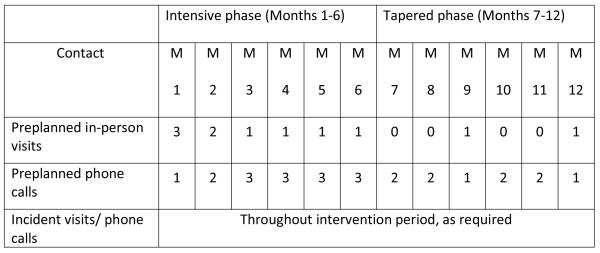
Figure 1 depicts the structure of the intervention, termed the Lifestyle Redesign Pressure Ulcer Prevention Program (LR-PUP). The intervention spans one year and is divided into 2 six-month phases: an intensive phase, with 4 preplanned sessions per month; and a tapered phase, with 2 preplanned sessions per month. Preplanned contacts include both person-to-person visits and phone calls. The majority of visits occur in the participant’s residence, with the remainder occurring at Rancho Los Amigos National Rehabilitation Center (RLANRC, the primary study site) clinics or at other community-based sites. Preplanned contacts are supplemented as needed with participant-initiated “incident” visits and phone calls, which are spontaneously scheduled in response to an emerging pressure ulcer or an event that significantly heightens pressure ulcer risk such as equipment breakage or sudden loss of an attendant. As part of the protocol, participants are provided with up to $400 to be used for the purchase of specialized equipment relevant to ulcer prevention. The 11 participants who are the focus of this report completed an average of 3.9 (range= 1.25 to 6) intervention months within the ongoing clinical trial. Intervention sessions draw upon content included in the LR-PUP manual. Divided into 6 modules, the manual contains the following content domains: (a) Understanding Lifestyle and Pressure Ulcer Risk, (b) Taking Charge (Advocacy), (c) Accessing the Physical Environment, (d) Social Networks and Meaningful Relationships, (e) Happiness and Personal Well-being, and (f) Planning the Future. Each module addresses fixed and variable topics. Fixed topics are reviewed and discussed with all intervention participants. Variable topics, in contrast, are incorporated into sessions at the discretion of the intervener-participant pair, depending on the participant’s particular lifestyle needs.
Figure 1.
Structure of the intervention in the PUPS-RCT
Each of the interveners was an occupational therapist who received training for a minimum of 30 hours in LR-PUP intervention delivery, and also received instruction in motivational interviewing to guide phone contacts. Motivational Interviewing is a clinical method that uses collaboration, evocation, and patient autonomy to promote behavioral change, and is effective for reducing at-risk behaviors when used in conjunction with other approaches.18-20 Finally, within the context of intervention delivery the treating therapists had access to consultation from a registered nurse when specialized medical information or assistance was needed.
Data Collection and Analysis
The data used for this paper originated from recordings of weekly Fidelity/ Quality Control (FQC) meetings, which were held as a component of the PUPS-RCT research design. The purpose of these meetings was to provide supervisory support to the intervening therapists, solve problems collectively in response to participant crises, and ensure fidelity of intervention delivery.21 Meetings lasted 75 minutes on average and were attended by the interveners along with an oversight/supervisory team including two senior level occupational therapists, the intervention’s nurse practitioner, the grant project manager, a research assistant, and a project assistant.
Data were analyzed in two steps. First, the discussions that transpired during weekly FQC meetings were audio taped or digitally recorded in audio format. Eighteen such meetings were held within the observation window for this paper. Eight of the 18 meeting recordings were transcribed for analytic purposes.
In the second step, content analysis was applied to extract (a) a set of intervention-relevant challenges that were the focus of meeting discussions, (b) the courses of action that were undertaken to meet such challenges, and (c) the ways in which flexibility was applied in using the manual. The content analysis was performed by the first author who took detailed notes while reviewing the 8 transcripts and listening to the remaining set of 10 recordings. For each meeting, treatment-related problems or issues were noted, along with the solutions that were discussed. These issues and solutions were coded and common themes were identified using an inductive approach. Following their derivation, the themes were reviewed for consistency and essential accuracy by two of this paper’s additional authors, who also attended the FQC meetings. Further, the primary coder checked some of the themes and obtained feedback from selected interveners.
RESULTS
Data analysis resulted in typologies pertaining to: (a) lifestyle relevant challenges to prevention and (b) avenues for achieving intervention flexibility. The obtained themes for these typologies are presented below.
Lifestyle –Relevant Challenges to Prevention
Theme 1: Risk-elevating life circumstances
Risk-elevating life circumstances refer to occurrences that heighten the likelihood of pressure ulcer development. These conditions required the team to deliberate on plausible solutions for reducing ulcer risk. For example, one of the interveners was unsure about how to handle problems arising from certain participants who had immigrated to this country. Commonly, the participants in this study who were immigrants were also from lower socioeconomic strata, needed to work long hours, had unsettling living situations with substandard basic facilities, and had limited access to health care services. In treating members of this group, the intervener had to consider their minimal resources as well as lack of familiarity with mainstream culture. For example, in one case, a participant had rigged an outdoor shower for himself in his backyard, which increased pressure ulcer risk due to the lack of an appropriate shower bench. The fact that he was a recent immigrant and poor made it difficult for him to obtain the equipment he needed. That he lived in a backyard shack, was reluctant to impose on others for help, and could not speak English brought about a cascade of circumstances that magnified his pressure ulcer risk.
Participants who were fortunate enough to have medical insurance were sometimes at risk due to its upcoming expiration. They were found to hoard supplies such as diapers, urine bags, or catheters in anticipation of the day when costs for such items would no longer be covered. These participants perceived periods of limited coverage as “waves of opportunity” not to be squandered. In turn, the intervener customized certain intervention sessions to assist these participants in capitalizing on such opportunities. In the words of one intervener:
“ I am learning a lot of them are kinda like squirrels…..they collect a lot of medical supplies and they try to get as much as they can because they don’t know what’s going to happen in the future…so I said, ‘ Come on let’s take advantage of this. You have MediCal [coverage] for one year. So let’s think of the pros and cons of everything, your life situation… which one is the best one to take.’ ”
Life circumstances that elevated risk also included unanticipated egregious events. In one such instance, a participant’s caregiver became inebriated and left him sitting in his wheelchair for nine hours. Throughout this time, no one was available to assist the participant in changing position or obtaining food and water, which greatly elevated pressure ulcer risk. To counteract the likelihood of another deleterious episode of this kind, the therapist assisted the participant in connecting with reputable community-based support organizations.
Even settings that we think of as relatively stable and safe could be saturated with unobtrusive threats to pressure ulcer prevention. For example, in nursing home environments the interveners found that the absence of personal belongings such as a television, an mp3 player, or reading materials sometimes reduced motivation to stay in bed when rest was needed to heal a developing ulcer.
Further, the life circumstances of the participants presented a wide range of challenges to their ability to perform “standardized” prevention behaviors such as pressure reliefs or to participate in intervention sessions. Some of the participants spent a significant amount of time on the streets, working ten to twelve hours a day or juggling busy lifestyles combining work and school activities. Interveners needed to be creative and accommodating, yet persistent, in scheduling intervention sessions in the face of unique, ongoing, and shifting life circumstances.
Theme 2: Communication difficulties
A second theme, communication difficulties, referred to barriers that impeded the ability of the participants to make their needs known to health care professionals. Such problems required adjustments in intervention delivery. For example, interveners often reported at FQC meetings that they were experiencing frustration contacting participants to schedule appointments. Specifically, participants often could not be reached because they were at work or in class for extended hours, their phone numbers changed, or they failed to return phone calls. One of the participants living in a nursing home did not have easy access to a telephone. Solutions to address these barriers came in the form of bolstering interveners’ persistence in attempting to reach the participants, extending hours of selected treatment sessions to make up for previously missed content, using a tracking system to reach participants at RLANRC when they arrived for appointments at various clinics, and providing the nursing home resident with a cellular phone that could be used for contact with the intervener.
A second type of communication problem stemmed from language barriers. Some of the Spanish-only speaking participants had difficulties communicating their problems to healthcare professionals who were insufficiently fluent in Spanish. Moreover, interpreters were not always present at the facilities where they sought treatment. To some extent these problems were anticipated and were addressed in the PUPS-RCT design by requiring that certain interveners speak fluent Spanish. However, for appointments during which the Spanish speaking intervener was unavailable to provide assistance, a decision was made at an FQC meeting to hire a translator who could be on call solely for in-person healthcare visits.
Communication styles of selective participants that were cause for concern were also discussed at FQC meetings so that intervention sessions could be tailored accordingly. Some of the participants were overbearing or verbally aggressive in demanding that their needs be met. Others were not assertive enough. How to modify these extremes in communication style is covered in the “Taking charge” module of the LR-PUP manual, but its content had to be individualized to address the unique struggles each participant faced. For example, a participant who was in desperate need of a seating clinic appointment was insufficiently assertive and as a result was unable to adequately convey the urgency of his need to the clinic receptionist. Consequently, in customizing an intervention session, the intervener provided coaching on exactly what to say and who to call so that the participant could overcome this barrier. The intervener described the session as follows:
“We (intervener and participant) contacted so many people to get him in….and we got him in….into the seating clinic…we planned it all, how to talk to them, how to set up appointments.”
Theme 3: Equipment problems
Equipment problems were continually brought up as serious concerns during the FQC meetings. Mattresses, wheelchair cushions, cell phones, mirrors, digital cameras to photograph interrupted skin, shower cushions, toilet seat cushions, vibrating watches, and wheelchair ramp rails were among the plethora of items that were discussed. Although one of the LR-PUP modules that is recommended to be covered in the third month of the intervention focuses on the acquisition of equipment, for one participant it was critical to begin the intervention by helping him procure a mattress to reduce immediate pressure ulcer risk. Because the standard procedure for such a purchase is time-consuming, in an FQC meeting the supervisory team deliberated on low-cost and speedier alternatives. Options included trying to obtain a mattress through donation, directly contacting mattress vendors, and examining the possibility of a rental. In fact, the team’s experience with the first few participants indicated that it was imperative to examine equipment at the outset of the intervention. It also was evident that participants needed to become savvy and highly skilled in researching regarding equipment options, talking to vendors, obtaining equipment, and overseeing the setup for personal use. Notably, the intervention extended well beyond equipment provision. Participants were helped to develop routines for equipment maintenance, anticipate future breakdowns, and generate backup plans to ensure immediate access to replacement parts or new equipment following breakdown.
Theme 4: Individual personality issues
Another recurring concern discussed at FQC meetings was how individual personality issues impacted pressure ulcer prevention practices, healthcare received, or patterns of participation in the intervention. As an illustration, one participant developed a serious pressure ulcer before enrolling in the PUPS-RCT because he resisted what he referred to as “overreacting” to a developing wound. Once the participant was enrolled in the intervention, the intervener speculated that his complacency was consequential to not having directly viewed the wound, which caused him to underestimate the gravity of the situation. A proposed solution was to photograph the lesion using a digital camera so that the participant could obtain high definition visual feedback. It was hypothesized that the sight of the wound would motivate the participant to seek care in a timelier manner in the future.
Another participant felt self-conscious about performing pressure reliefs in public and lacked any sense of urgency in his wound care practices. In general, complacency and procrastination hampered performance of pressure ulcer prevention practices and delayed decisions to seek medical attention. To combat these proclivities, in some instances the interveners shared stories with participants about how certain individuals in our previous qualitative study failed to take immediate action, incurred serious pressure ulcers, needed to undergo flap surgeries, and ultimately experienced devastating functional losses.
In another vein, an impulsive individual who was frustrated by the waiting time required to arrange an appointment at the facility he always used made the decision to seek care at an outside hospital at which he had no previous experience. While hospitalized at the new facility, he developed an advanced pressure ulcer. The intervener used relaxation techniques to help the participant experience calmness and then, in this state, be more reflective by weighing the pros and cons of impending decisions.
Avenues for Achieving Intervention Flexibility
The components of the typology of lifestyle challenges to prevention suggest an overarching need to maintain flexibility in the delivery of the LR-PUP manualized intervention content. Below, we describe three overarching strategies through which intervention flexibility was accomplished.
Theme 1: Changing order
Changing order refers to departures from the preplanned sequence of modular presentation that were made in response to participant needs. For example, the LR-PUP manual specifies that on one of the preplanned visits the intervener should accompany the participant to a medical appointment. These appointments needed to be set well in advance and offered virtually no flexibility. For this reason, the sequence of modules often had to be altered to align with the participants’ medical appointments. Rearrangements of this kind, as already described, were also common in the case of urgent equipment needs. Also, participants with higher injury levels presented with more complex equipment needs than those with lower level injuries. Their problems had to be addressed expeditiously because of potential life-threatening consequences. In short, although modules were developed with an “ideal” order of delivery in mind, in real world applications the sequence was frequently rearranged in response to risk-related concerns.
Theme 2: Changing the content or approach
Changing the content or approach refers to the process through which interveners altered session content or mode of delivery in accordance with participant attitudes or needs. Preplanned content encompassed a wide range of topics within each module. Because certain topics were of relevance to only select participants, professional judgment needed to be exercised to distill exactly what content should be covered in each session. Also on occasion, as some of the modular topics addressed sensitive issues, interveners needed to be especially tactful in how such content was presented. For example, although the topic of intimacy and how it could contribute to pressure ulcer development was planned for a given session, one younger participant was uncomfortable talking about the subject matter and asked to change the focus of the session. The intervener, therefore, modified his usual approach. He began the session by initiating a discussion on the subject of the participant’s favorite movies and then steered the conversation to the topics that more directly related to the preplanned theme.
Theme 3: Going beyond the content
Going beyond the content refers to the numerous instances when sessions were individualized at the highest end of the patient-centeredness continuum. In such cases, although the manualized content paved the way for goal setting, the resulting intervention sessions were extremely situation-specific and collaborative. Such sessions were spawned by the intensity of the initial intervention phase, in which the interveners become closely connected to the social and physical worlds of the participants. Such immersion rendered them acutely aware of emerging or ongoing risk-relevant concerns and the extent to which manual content was limited in addressing them. As an illustration, one of the participants wished to take swimming lessons but was hesitant to do so because of long term bowel movement issues and an open abdominal wound. At one of the FQC meetings, the team devised a solution that required the acquisition of foolproof swimwear in conjunction with systematic regulation of food and liquid intake. This adaptive system made it possible for the participant to confidently take part in the lessons without worries pertaining to incontinence.
On occasion, unexpected events prompted the specification of intervention goals that went beyond the manualized content. Usually these occurrences, deemed crisis events, significantly heightened pressure ulcer risk. As an example, one participant needed to unexpectedly change residence, but the movers failed to arrive as scheduled. This situation elevated ulcer risk exponentially because it could have led to temporary homelessness, with the result that the participant would have sat in his wheelchair for extended time periods while living on the streets. To counteract this threat, the intervention goal shifted to monitoring and facilitating the participant’s efforts to move and to simultaneously assist him to better manage moment-to-moment concerns related to pressure ulcer risk in his destabilized life situation.
Such crisis events demanded creative solutions along with a certain amount of improvisation. However, they were managed in conjunction with the content of the modules insofar as possible. We discovered that in general the modular content and its preplanned sequence could only be closely followed for participants who were relatively crisis free. One intervener expressed this idea in these words:
“…actually the modules are followed more with the ones that have less crises. With the others I just go to the needs because that’s what we have to do [in order to reduce pressure ulcer risk].”
To maximize effectiveness, the intervention required ongoing tailoring and sometimes amplification of modular content in response to risk-elevating circumstances. For example, the module Understanding the Relationship Between Lifestyle and Pressure Ulcer Risk was expanded into a multifaceted plan to avoid homelessness, the module Happiness and Personal Well being was broadened to include the construction of a total adaptive system to enable swimming without the threat of incontinence, and the module Accessing the Physical Environment went beyond ordering an appropriate sleeping surface to ensuring that it was procured, delivered, and slept on without delay.
DISCUSSION
In this paper we have described how lifestyle-related challenges were taken into account to customize a manualized pressure ulcer prevention program for community-dwelling adults with SCI. Key strengths of the study include the use of a rich, intervention-relevant data set; the focus on a medically relevant problem that requires highly involved solutions; and the development of typologies that can be used to help guide individualized practice approaches or the development of treatment manuals.
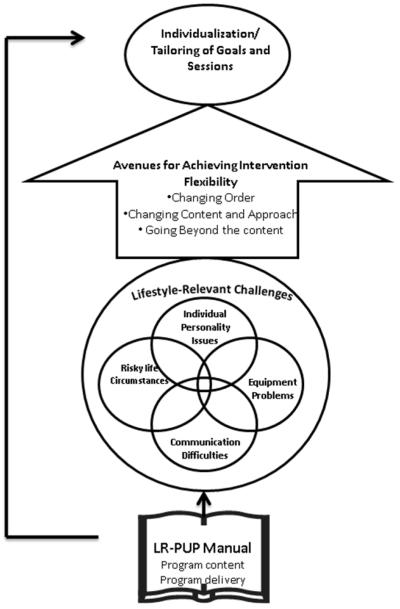
Figure 2 summarizes the various components that contributed to the customization process. As can be seen in the figure, the LR-PUP manual served as the foundation for program content and delivery. However, goal setting and session content needed to be flexibly approached to enable tailoring and individualizing in accordance with emerging challenges. Typically, these challenges involved risk-elevating life circumstances, communication difficulties, equipment problems, or individual personality issues. The need for flexibility led to departures from the preplanned order of module presentation, changes in the intervention content and delivery approach, and a need to go beyond the manualized content.
Figure 2.
Relationship between risk elevating life circumstances and avenues for achieving intervention flexibility
Although structured, the intervention permitted both tailoring and individualizing of sessions and goals in response to the exigencies of in-context daily life pressure ulcer risk. In general, manualization enables interventions to be replicable with a degree of uniformity in structure and content. However, if too calcified, manualization can stifle overall effectiveness.16, 17 LR-PUP possesses the advantages of manualization. However the drawbacks of a more rigid intervention are offset in LR-PUP by its individualization and tailoring capabilities (Blanche EI, Fogelberg D, Carlson M, Clark F, unpublished data, 2009).
The contextualized problems and solutions addressed in the obtained typologies underscore an overarching need for flexibility in community-based rehabilitation intervention delivery. Consistent with this need, studies have reported that patients tend to value health care that is customized to their particular attributes and needs.14, 22-24 In contrast, highly prescriptive, standardized protocols may be more appropriate for in-patient, short term care.25
The thematic categories of pressure ulcer risk were not mutually exclusive. For example, it was evident that challenging life circumstances at the macro level (such as MediCal policy) in combination with personality attributes (such as aggressiveness) combined in complex ways to affect what equipment and services participants were able to obtain. Such interdependency was not surprising, as one of our previous studies indicated that a complex interplay of fluid life circumstances impact pressure ulcer risk.11,13Therefore, it was crucial to identify not one but a set of key interacting risk factors in identifying intervention goals.
An unanticipated finding was that compromised autonomy, either due to higher levels of injury or lower socioeconomic circumstances, tended to produce a greater need for intervention flexibility. This was evidenced by the fact that participants with the fewest resources or the most compromised health conditions most often required “going beyond” the content of the manualized intervention. In contrast, adherence to the preplanned order for content delivery was more likely when the participant had a stable living situation that was associated with fewer “crisis” situations and better established pressure ulcer prevention routines.
Arguably, our examples of “going beyond” the manualized content may cause one to question the extent to which appropriate intervener-participant boundaries were maintained. We believe that the complexity of the interacting factors that lead to serious pressure ulcers in people with SCI justifies the need for an intense and robust intervention approach. However, on occasion the legitimacy of a given course of action was unclear. For this reason the team instituted a consensus building process for evaluating ambiguous situations. When non-standardized solutions were introduced, team members collectively evaluated whether they were suitable for counteracting particular risk relevant liabilities.
Clinical Implications
The findings of this study have at least two key clinical implications. First, they suggest that goal setting and interventions for pressure ulcer prevention for people with SCI living in the community, even when manualized, can be tailored, individualized, and flexibly delivered. However, from a practical vantage point it may be necessary to provide relatively rich intervention services that include components such as extensive therapist training, in-depth oversight meetings, and multiple in-home visits. Second, in light of the ubiquitous threats to skin integrity encountered by the participants in their daily lives, our findings reinforce the view that community-based pressure ulcer prevention efforts are strongly needed. Although, prolonged individualized interventions may be expensive, such efforts are potentially justifiable given the complexity of the link between lifestyle and ulcer risk, as well as the extreme costs of surgery and hospitalization for advanced ulcers. Accordingly, a key aim of the PUPS-RCT is to address the cost-effectiveness of the LR-PUP program.
It is also important to note that the identification of specific issues that require an individualized approach goes beyond the mere recognition that “interveners need to be flexible.” The fourfold typology of key concerns can be used to direct therapists’ attention to specific issues that, if insufficiently addressed, can undermine the success of an intervention. For example, a communication problem could disrupt an otherwise ideal plan of prevention. By articulating specific problem areas, the study results provide important clues that can enable therapists to attend to such critical concerns.
The lifestyle-based intervention challenges varied in their degree of generality versus specificity. For relatively widespread issues, such as the need to deal with equipment issues early in the intervention or the presence of language barriers to the receipt of effective healthcare for Hispanic participants, the qualitative methodology was useful in identifying new content areas that need to be incorporated into future versions of the PUPS manual. In contrast, more idiosyncratic concerns such as the need to obtain specialized swimwear are too detailed to be manualized and will continue to require creative problem solving that stretches beyond published guidelines. As in the current intervention approach, such problem solving could be undertaken through multiple routes including FQC meetings, therapist-client collaboration within motivational interviewing sessions, and independent research performed by the therapist. The typology of avenues for achieving intervention flexibility has implications for the development of manualized interventions. In particular, our results suggest that treatment manuals should, to the degree possible, explicate the conditions under which interveners should change the order of concepts, change the content itself or the delivery approach, go beyond the content. Although such solutions seem straightforward, to our knowledge they have not been explicitly typologized in previous publications on the manualization process.26,27 Strategies for tailoring an intervention in each of the above ways, as well as for identifying the limits of such changes, should be routinely included in treatment manuals as well as training sessions.
Limitations
This study had four primary limitations. First, our analysis was based on a circumscribed set of recordings of meeting discussions. A more comprehensive study of the particular ways in which the intervention was delivered, using a more robust data set, might potentially yield more extensive findings. Such additional data sources could include therapist notes, patient interviews, or videotapes of intervention sessions. Second, the PUPS-RCT sample was preselected on the basis of having high pressure ulcer risk. Many of the treated individuals were economically or socially disadvantaged. Therefore, the need for individualization that was noted in this study may not be as prominent when treating other groups with SCI, which on average are likely to have more economic stability or reduced lifestyle-related pressure ulcer risk. Third, the use of a single coder precluded the ability to directly assess the reliability of the typological categories across multiple raters. Finally, bias in our analysis may have occurred because we were only able to analyze the recordings of 18 meetings, all of which occurred in the first year of the PUPS-RCT. Because the FQC meetings that were included in this study occurred in the first few months of PUPS-RCT, the interveners and team members had relatively limited experience in implementing and overseeing LR-PUP intervention delivery. It is anticipated that over two hundred such meetings will take place over the course of the wider PUPS-RCT. In the future, the content of all such meetings will be analyzed to identify potential shifts in focus or approach, and to determine whether the typology needs fine tuning or major revision due to long-term changes that occur in intervention delivery.
Acknowledgement
We would like to acknowledge the valuable input of the interveners and oversight team members.
Disclosure of funding: This paper is part of an ongoing randomized controlled trial supported by award number R01HD056267 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ashwini Vaishampayan, Division of Occupational Science and Occupational Therapy at the University of Southern California, Los Angeles, California.
Florence Clark, Division of Occupational Science and Occupational Therapy at the University of Southern California, Los Angeles, California.
Mike Carlson, Division of Occupational Science and Occupational Therapy at the University of Southern California, Los Angeles, California.
Erna Imperatore Blanche, Division of Occupational Science and Occupational Therapy at the University of Southern California, Los Angeles, California.
REFERENCES
- 1.Krause JS. Skin sores after spinal cord injury: relationship to life adjustment. Spinal Cord. 1998;36:51–56. doi: 10.1038/sj.sc.3100528. [DOI] [PubMed] [Google Scholar]
- 2.Walter JS, Sacks J, Othman R, Rankin AZ, Nemchausky B, Chintam R, Wheeler JS. A database of self-reported secondary medical problems among VA spinal cord injury patients: its role in clinical care and management. J Rehabil Res Dev. 2002;39:53–61. [PubMed] [Google Scholar]
- 3.Garber SL, Rintala DH. Pressure ulcers in veterans with spinal cord injury: a retrospective study. J Rehabil Res Dev. 2003;40:433–41. doi: 10.1682/jrrd.2003.09.0433. [DOI] [PubMed] [Google Scholar]
- 4.Krouskop TA, Noble PC, Garber SL, Spencer WA. The effectiveness of preventive management in reducing the occurrence of pressure sores. J Rehabil Res Dev. 1983;20:74–83. [PubMed] [Google Scholar]
- 5.Correa GI, Fuentes M, Gonzalez X, Cumsille F, Pineros JL, Finkelstein J. Predictive factors for pressure ulcers in the ambulatory stage of spinal cord injury patients. Spinal Cord. 2006;44:734–739. doi: 10.1038/sj.sc.3101914. [DOI] [PubMed] [Google Scholar]
- 6.Dorsett P, Geraghty T. Health-related outcomes of people with spinal cord injury- a 10 year longitudinal study. Spinal Cord. 2008;46:386–391. doi: 10.1038/sj.sc.3102159. [DOI] [PubMed] [Google Scholar]
- 7.Krause JS, Carter RE, Pickelsimer EE, Wilson D. A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2008;89:1482–1491. doi: 10.1016/j.apmr.2007.11.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, DeVivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86:1208–13. doi: 10.1016/j.apmr.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 9.Garber SL, Rintala DH, Hart KA, Fuhrer MJ. Pressure ulcer risk in spinal cord injury: predictors of ulcer status over 3 Years. Arch Phys Med Rehabil. 2000;81:465–471. doi: 10.1053/mr.2000.3889. [DOI] [PubMed] [Google Scholar]
- 10.Gélis A, Dupeyron A, Legros P, Benaïm C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with spinal cord injury Part 2: the chronic stage. Spinal Cord. 2009;47:651–661. doi: 10.1038/sc.2009.32. [DOI] [PubMed] [Google Scholar]
- 11.Clark FA, Jackson JM, Scott M, Carlson ME, Atkins MS, Uhles-Tanaka D, Rubayi S. Data-based models of how pressure ulcers develop in daily living context of adults with spinal cord injury. Arch Phys Med Rehabil. 2006;87:1516–1525. doi: 10.1016/j.apmr.2006.08.329. [DOI] [PubMed] [Google Scholar]
- 12.Dunn CA, Carlson M, Jackson JM, Clark FA. Response factors surrounding progression of pressure ulcers in community-residing adults with spinal cord injury. Am J Occup Ther. 2009;63:301–309. doi: 10.5014/ajot.63.3.301. [DOI] [PubMed] [Google Scholar]
- 13.Jackson J, Carlson M, Rubayi S, Scott MD, Atkins MS, Blanche EI, Saunders-Newton C, Mielke S, Wolfe MK, Clark FA. Qualitative study of principles pertaining to lifestyle and pressure ulcer risk in adults with spinal cord injury. Disab and Rehabil. 2009 doi: 10.3109/09638280903183829. early online 1-12. [DOI] [PubMed] [Google Scholar]
- 14.Richards KC, Enderlin CA, Beck C, McSweeney JC, Jones TC, Roberson PK. Tailored biobehavioral interventions: a literature review and synthesis. Res Theor Nurs Pract. 2007;21:271–285. doi: 10.1891/088971807782428029. [DOI] [PubMed] [Google Scholar]
- 15.Lauver DR, Ward SE, Heidrich SM, Keller ML, Brennan PF, Kirchhoff KT, Wells TS. Patient-centered interventions. Res Nurs Health. 2002;25:246–255. doi: 10.1002/nur.10044. [DOI] [PubMed] [Google Scholar]
- 16.Beutler LE. Manulizing flexibility: the training of eclectic therapists. J Clin Psychol. 1999;55:399–404. doi: 10.1002/(sici)1097-4679(199904)55:4<399::aid-jclp4>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 17.Westen D. Manualizing manual development. Clin Psychol Sci Prac. 2002;9:416–418. [Google Scholar]
- 18.Miller WR, Rollnick S. Motivational Interviewing – Preparing People for Change. 2nd ed The Guilford press; New York: 2002. [Google Scholar]
- 19.Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. J Clin Psychol. 2009;65:1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- 20.Velasquez MM, Von Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: A randomized clinical trial. J Consul Clin Psychol. 2009;77:657–667. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sholomskas DE, Syracuse-Siewert G, Rounsaville BJ, Ball SA, Nuro KF, Carroll KM. We don’t train in vain: A dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. J Consul Clin Psychol. 2005;73:106–115. doi: 10.1037/0022-006X.73.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radwin LE, Alster K. Individualized nursing care: an empirically generated definition. Int Nurs Rev. 2002;49:54–63. doi: 10.1046/j.1466-7657.2002.00101.x. [DOI] [PubMed] [Google Scholar]
- 23.Ryan P, Lauver DR. The efficacy of tailored interventions. J Nurs Schol. 2002;34:331–337. doi: 10.1111/j.1547-5069.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- 24.Whittemore R. Consequences of not “knowing the patient”. Clin Nurs Spec. 2000;14:75–81. doi: 10.1097/00002800-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Radwin LE. Knowing the patient: A process models for individualized interventions. Nurs Res. 1995;44:364–370. [PubMed] [Google Scholar]
- 26.Carroll KM, Nuro KF. One size cannot fit all: A stage model for psychotherapy manual development. Clin Psychol: Sci Prac. 2002;9:396–406. [Google Scholar]
- 27.Herman-Smith R, Pearson B, Cordiano TS, Aguirre-McLaughlin A. Addressing individual client needs in manualized treatment: Case comparisons. Clin Case Stud. 2008;7:377–396. [Google Scholar]