Abstract
The purpose of this study was to investigate the relationships of chronic stress, social undermining, and social support with symptom reduction and remission in depressed patients treated with antidepressant medication (citalopram), and to determine whether these relationships were moderated by ethnicity. A sample of 301 treatment-seeking adult patients with non-psychotic depression, including 169 African-American and 132 Caucasian men and women, were enrolled in an eight week, dose escalation clinical trial. Intent-to-treat analyses indicated that, consistent with expectations, more baseline social support was associated with greater symptom reduction and higher likelihood of remission, especially at higher levels of social undermining. Additionally, increases in social support from baseline to last visit were associated with more symptom reduction and higher likelihood of remission. However, contrary to expectations, higher levels of baseline social undermining were associated with more symptom reduction in Caucasians, but not in African-Americans. Results supported the treatment enhancing effect of available social support at the beginning of treatment and over the course of treatment. Efforts to enhance social support for patients on antidepressants should be considered as part of comprehensive treatment.
Keywords: antidepressant, depression, ethnicity, psychosocial, stress, social support
Introduction
Over the past few decades, research on major depression has consistently shown that psychosocial factors, such as stressful life circumstances and quality of interpersonal relationships, play important roles in the onset and course of major depression (e.g., Backs-Dermott et al., 2010; Hammen, 2003; Kendler et al., 2004; Kendler et al., 2005). A growing body of literature has also shown that these psychosocial factors influence depressive symptoms even in the context of pharmacotherapy (e.g., Bosworth et al., 2008; Pedrelli et al., 2008). Additionally, some earlier studies suggested that ethnicity might play a role in treatment outcomes of those undergoing pharmacotherapy for depression (e.g., Wagner et al., 1998). The current study examines the complex interactions between ethnicity and psychosocial factors in relation to symptom improvement in the context of pharmacotherapy.
The literature to date suggests that life stress, social undermining, and social support are psychosocial factors that may distinguish for whom, and under which psychosocial conditions, antidepressants such as citalopram (CIT) may be most effective. Exposure to various life stressors and chronic interpersonal stress has been consistently linked to the onset and course of major depression (Hammen, 2003; Kendler et al., 1999; Kendler et al., 2004; Kendler et al., 1997; see Kessler, 1997 for a review). However, the evidence linking stress to antidepressant response has been mixed, with some studies suggesting that there is no relationship between stress and depression in the context of antidepressant treatment (Bosworth et al., 2008), some showing that stress is associated with worse treatment outcomes (Mazure et al., 2000; Pedrelli et al., 2008; Tomaszewska et al., 1996), and others suggesting that interpersonal stress is associated, counter-intuitively, with better treatment outcomes (Sherbourne et al., 2004; Vallejo et al., 1991).
There are several factors that could account for these mixed findings, including differences in study samples, study design, measurement of stress, and tailoring of drug dose to patient needs. For example, Bosworth and colleagues (2008) reported that pre-treatment life stress was unrelated to severity of depression after antidepressant treatment. However, this finding was based on a much longer follow-up (i.e., 12 months) than studies that examined the effects of pre-treatment stress in the context of 6 or 8 week structured antidepressant trials. The latter found that recent stressful life events were associated with poorer short-term treatment response (e.g., Mazure et al., 2000; Pedrelli et al., 2008). Additionally, some studies show that stressful life events and perceived stress may be related to poorer treatment response only in specific sub-samples, such as those exhibiting a strong need for control, those with high levels of dysfunctional attitudes, or those without melancholia (Mazure et al., 2000; Pedrelli et al., 2008; Tomaszewska et al., 1996). To our knowledge, no studies have examined the effects of chronic overall stress across life domains on symptom change in those undergoing pharmacotherapy.
Surprisingly, there are also few studies investigating how the effects of stress on depression in the context of pharmacotherapy may differ between those who receive little social support from close family members and friends and those who receive high social support. More available social support at baseline and greater satisfaction with social support at baseline have been shown to be associated with better treatment response and more complete remission of major depression (Bosworth et al., 2008; Coyne and Downey, 1991; Ezquiaga et al., 1999; Sherbourne et al., 2004; Tomaszewska et al., 1996; Vallejo et al., 1991). Additionally, increases in social support over time have been shown to be associated with decreases in depressive symptoms in in-patients, but not within the context of a controlled antidepressant trial (Sayal et al., 2002). Some have suggested that the relationship between adequate social support and desirable treatment outcomes may be mediated through better medication adherence (Voils et al., 2005). In addition, conceptualizations of social support as a stress-buffering resource would suggest that the relationship between social support and treatment outcomes might vary depending on level of stress burden (Cohen and Wills, 1985; Stanton et al., 2007). Unfortunately, however, few studies have investigated whether social support may serve as a moderator of the relationship between chronic life stress burden and outcome after treatment with an antidepressant.
Another aspect of interpersonal interactions that might influence depressive symptom reduction of those undergoing an antidepressant trial is social undermining. Social undermining is a construct that captures behaviors that involve criticism, displays of negative affect, and placing strain on an individuals’ ability to progress on important goals (Vinokur & van Ryn, 1993). Studies have consistently shown that social undermining is associated with greater depressive symptoms (Cranford, 2004; Gant et al., 1993; Okun & Keith, 1998; Vinokur et al., 1996). Studies have also consistently shown that the same individuals who give support may undermine, sometimes supporting and undermining over the course of just one interaction (e.g., Foster et al., 1997). A meta-analysis by Okun and Keith (1998) found that the effects of undermining behaviors by ones’ spouse, children, or other loved ones are buffered by supportive behaviors of that spouse, those children, or those loved ones, respectively. However, no studies have examined how social undermining and social support might affect changes in depressive symptoms in response to an antidepressant.
Current evidence also suggests the need to investigate whether these relationships might be moderated by ethnicity. There is compelling epidemiological evidence that African-Americans may be more likely than Caucasians to have a more persistent, disabling course of major depression after onset (Breslau et al., 2005; Williams et al., 2007), as well as suggestive evidence of ethnic differences in the metabolism of SSRIs (Lin et al., 1993). However, recent dose-escalation clinical trials and quality improvement interventions have shown that, when demographic and baseline variables are controlled and quality of care is equivalent across participants, there are no ethnic differences in response to antidepressant treatment and rate of symptom improvement (e.g., Lesser et al., 2010; Lesser et al., 2007). However, it is possible that, even in the case of equivalent treatment outcomes, there may be ethnocultural differences in the relative contributions that psychosocial factors play in treatment outcome. Prospective studies with untreated samples have found greater impact of chronic stress burden and social support on the depressive symptoms of African-Americans compared to Caucasians (e.g., Gurung et al., 2004). Thus, although specific cultural factors and processes were not measured in the current trial, the trial provides an opportunity to explore how psychosocial factors might contribute to treatment outcome in African-Americans and Caucasians.
To our knowledge, no study has specifically investigated the associations of multiple psychosocial factors and changes in these factors over time with symptom improvement during a trial of anti-depressant treatment, including with CIT, and whether there are ethnic differences in these associations. The current study investigated whether chronic stress burden, social undermining, and social support are associated with symptom change during a dose-escalating trial of an anti-depressant, and whether these factors are differentially associated with symptom change among African-American and Caucasian patients.
Hypotheses
We hypothesized, consistent with suggestive evidence, that: (1) psychosocial factors would be associated with symptom reduction and remission status, with greater chronic stress burden and social undermining associated with less symptom reduction and lower likelihood of remission and greater social support associated with greater symptom reduction and higher likelihood of remission; (2) social support would modify the detrimental effects of chronic stress and social undermining on symptom change, with lower social support exacerbating these effects and higher social support attenuating these effects; and (3) the strength of these relationships might vary as a function of ethnicity, such that the impact of stresses and social support would be greater in African-Americans compared to Caucasians. Finally, recognizing that psychosocial factors are not static, we also hypothesized (4) that changes in psychosocial factors would be associated with symptom reduction, with increases in social support and decreases in social undermining over the course of the trial associated with greater symptom reduction. The fact that chronic stress was only measured at baseline precludes us from formally testing the association between change in chronic stress burden and symptom reduction.
Methods
Participants
All data were collected as part of a multisite, collaborative, 8-week dose escalation open label trial of CIT. All participants were self-identified as African-American or Caucasian and reported that both parents and at least 3 of 4 grandparents were from the same ethnic group, were 18 years and older, met DSM-IV-R criteria for non-psychotic depression, and had a depression severity rating (Hamilton Rating Scale for Depression [HRSD]; Hamilton, 1960) of 17 or greater. Prospective participants were excluded if they had an unstable medical or neurological condition that would interfere with treatment or had a history of bipolar disorder, psychosis or substance abuse disorders, seizure disorder, allergy to CIT, or failure to respond to an adequate CIT drug trial (i.e. 40mg/day for at least 6 weeks). Prospective female participants were excluded if they were pregnant or planning to get pregnant in the next 3 months. See Lesser et al. (2010) for a more detailed description of recruitment methods.
The study sample consisted of 301 intent-to-treat participants, including 169 African-American and 132 Caucasian men and women, with mean age of 42.24 years (SD = 10.58) and mean education of 14.20 years (SD = 2.28). The average number of trial visits attended was approximately 7 visits. A total of 235 participants completed weekly assessments for the entire study duration (i.e., 22% attrition rate).
Procedures
Written informed consent was obtained from all participants, and all were assessed weekly for 8 weeks and compensated up to $320, with the amount of compensation prorated by number of sessions attended. A comprehensive battery of clinical and psychosocial measures was administered by trained staff in face-to-face private interviews at baseline and at various times over the course of treatment. Following the baseline assessment, participants were on placebo medication for one week and then were placed on active medication for 8 weeks. For a more detailed description of study procedures, see Lesser et al. (2010).
Measures
Ethnicity was measured by self-report. Education was measured as self-reported years of formal schooling completed.
Hamilton Rating Scale for Depression (HRSD)
Severity of depression, which was the primary outcome, was assessed each week using the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). This is a widely used interview measure completed by clinically trained interviewers who received standardized training and rated participants on a 24-item version of the measure. Item rating scales are based on either a 3- or 5-point Likert scale, with a rating of 0 indicating that the symptom is absent or within normal limits and the highest rating indicating that the symptom is present and severe. Coefficient alpha and inter-rater reliability were within appropriate range in earlier studies. Only responses to the core 17 items that were common across study sites were summed to create HRSD composite scores (coefficient alpha = .82). Pre-post HRSD change scores were calculated by subtracting participants’ sum baseline scores from their sum scores at their last visits. Remission scores were calculated by giving participants with HRSD scores equal to or less than 7 at their last visit a score of 1, and those who did not meet this criterion a score of 0, i.e., not remitted.
Chronic Stress Burden
The cumulative burden of life stresses experienced during the last month was assessed at baseline with the Chronic Burden Scale (CBS) (Gurung et al., 2004). This 21-item scale assesses the degree of difficulty caused by life stressors over the past month in several life domains (e.g., interpersonal, financial, health, and community stressors). In addition to traditional sources of life stress, the CBS includes several items that evaluate social status stressors such as experiences of discrimination and immigration problems. Items are answered on a 4-point scale from “not a problem for me in the last month” to “a major problem for me in the last month”. Responses were summed to form a reliable composite score (coefficient alpha = .76).
Social Support
Social support was measured at baseline and Week 8 using a short version of the Vinokur and Vinokur-Kaplan (1990) social support scale, which was adapted from a measure developed by Abbey et al. (1985). Participants were asked to list the four most important people to them and to rate each on a 5-point scale (1 = not at all to 5 = a great deal) on the following aspects of social support: giving useful information or advice, listening, showing care, help with specific problems, and providing needed resources. Responses were summed to form a reliable composite score (coefficient alpha = .90). Social support change scores were calculated by subtracting participants’ sum scores at baseline from their sum scores at Week 8.
Social Undermining
The extent to which a participant was undermined in interactions in his or her four most important relationships was measured at baseline and Week 8 with a 3-item version of a social undermining scale that Vinokur and Vinokur-Kaplan (1990) partially adapted from Abbey et al. (1985). Specifically, participants rated the extent to which the four most important people in their lives criticized them, made their life difficult, and acted in an angry and unpleasant manner towards them on a scale of 1 = not at all to 5 = a great deal. Responses were summed to form a reliable composite score (coefficient alpha = .76). Social undermining change scores were calculated by subtracting participants’ sum scores at baseline from their sum scores at Week 8.
Data Analysis
Univariate analyses of variance (ANOVAs) were run to test for differences between completers vs. dropouts on baseline demographic, clinical, and psychosocial characteristics. ANOVAs and chi-square analyses were run to test for main and interaction effects of ethnicity on demographic, clinical, and psychosocial variables. Finally, hierarchical multiple linear regressions were run: (1) to estimate the relative contributions of ethnicity, chronic stress burden, social undermining, and social support in accounting for variance on pre-post changes on HRSD and to examine interactions; and (2) to estimate the relative contributions of change in social undermining and change in social support in accounting for variance on pre-post changes on HRSD and to examine interactions (for these analyses, the sample size drops to 184 due to attrition and missing data on Week 8 psychosocial measures). Parallel logistic regressions were also run to estimate the respective contributions of the above factors and interactions in accounting for remission status. In order to reduce the potential for multicollinearity, all continuous psychosocial variables were centered before being entered into the regressions and before calculating interaction terms.
For linear and logistic regressions using baseline psychosocial variables, variables were entered in invariant order as follows: Step 1 - ethnicity, education, and dose of CIT at study exit; Step 2 - baseline chronic stress; Step 3 - baseline social undermining; Step 4 - baseline social support; Step 5 - ethnicity by chronic stress interaction term; Step 6 - ethnicity by social undermining interaction term; Step 7 - ethnicity by social support interaction term; Step 8 -chronic stress by social support interaction term; and Step 9 - social undermining by social support interaction term.
For linear and logistic regressions using psychosocial change variables, variables were entered in invariant order as follows: Step 1 - ethnicity, education, and dose of CIT at study exit; Step 2 – social undermining change; Step 3 – social support change; Step 4 – ethnicity by social undermining change interaction term; Step 5 - ethnicity by social support change interaction term; Step 6 - social undermining change by social support change interaction term. Chronic stress was not measured at last visit, so it was not included in this set of analyses.
Results
Differences between Completers and Non-Completers
There were no significant differences on education, baseline HRSD severity, baseline chronic stress burden, or baseline social support between completers and dropouts. Additionally, there was no significant difference between African-Americans and Caucasians in attrition rate. However, dropouts were significantly younger than completers (F(1, 297) = 4.49, p=.035) and a strong trend on social undermining was observed, with dropouts reporting higher levels of social undermining than completers (F(1, 279) = 3.69, p=.056).
Ethnic Differences in Demographic, Clinical, and Psychosocial Variables
As reported previously (See Lesser et al., 2010), African-Americans reported less education and were less likely to be employed than Caucasians, F(1, 290) = 10.58, p=.001 and χ2(1, N = 242) = 4.41, p = .036, respectively. African-Americans also were less likely than Caucasians to report consuming alcohol, χ2(1, N = 222) = 6.35, p = .012. Of these demographics, only education was associated with treatment outcome, so education was included as a covariate in all regressions. Controlling for education, African-Americans had higher baseline HRSD scores (M=19.9, SE=.40) than Caucasians (M=18.4, SE=.45), F(1,298)=5.46, p=.020, but there were no ethnic differences on HRSD score at the last visit or on pre-post HRSD change.
Results for ethnic differences in baseline psychosocial factors are displayed in Table 1. African-Americans had higher baseline chronic stress burden and more social support than Caucasians, F(1,293)=10.91, p=.001 and F(1,279)=11.11, p=.001, respectively. However, there were no ethnic differences in amount of social support change or social undermining change from baseline to Week 8. It is important to note that there was considerable variability in changes in these psychosocial variables over time in both ethnic groups. The majority of the sample (60.2%) reported receiving higher social support by the end of the trial compared to baseline and a slight majority (56%) reported experiencing lower social undermining. It is unclear, however, whether these positive changes results from changes in the behaviors of the people in their lives or in their interpretations of their behaviors.
Table 1.
Ethnic Differences on Baseline Psychosocial Measures
| Baseline Measure |
African-American M(SD) n |
Caucasian M(SD) n |
F | p |
|---|---|---|---|---|
| Chronic Stress | ||||
| Intent-to-Treat E | 39.08(9.58) 166 |
35.63(7.89) 128 |
10.91 | .001 |
| Completers E | 39.67(9.96) 126 |
35.21(7.89) 105 |
13.86 | .000 |
| Remitters | 38.76(8.69) 82 |
36.15(8.17) 67 |
3.50 | .063 |
| Social Undermining | ||||
| Intent-to-Treat | 21.59(8.52) 159 |
20.65(7.98) 121 |
.90 | .344 |
| Completers | 21.03(8.68) 121 |
20.30(7.53) 101 |
.45 | .505 |
| Remitters | 21.15(7.93) 79 |
21.91(7.89) 65 |
.33 | .569 |
| Social Support | ||||
| Intent-to-Treat E | 69.31(19.37) 158 |
61.52(19.40) 122 |
11.11 | .001 |
| Completers E | 68.17(20.34) 121 |
61.90(19.41) 101 |
5.46 | .020 |
| Remitters E | 70.65(19.27) 79 |
62.56(19.11) 66 |
6.38 | .013 |
Note. E superscript indicates that there is a main effect of ethnicity on a measure.
Given that there were no significant gender differences in treatment outcomes and no gender by ethnicity interactions associated with Pre-Post HRSD change, gender was not included in the final treatment outcome analyses.
Regressions Predicting Symptom Improvement (Pre-Post HRSD Change)
Impact of Baseline Factors
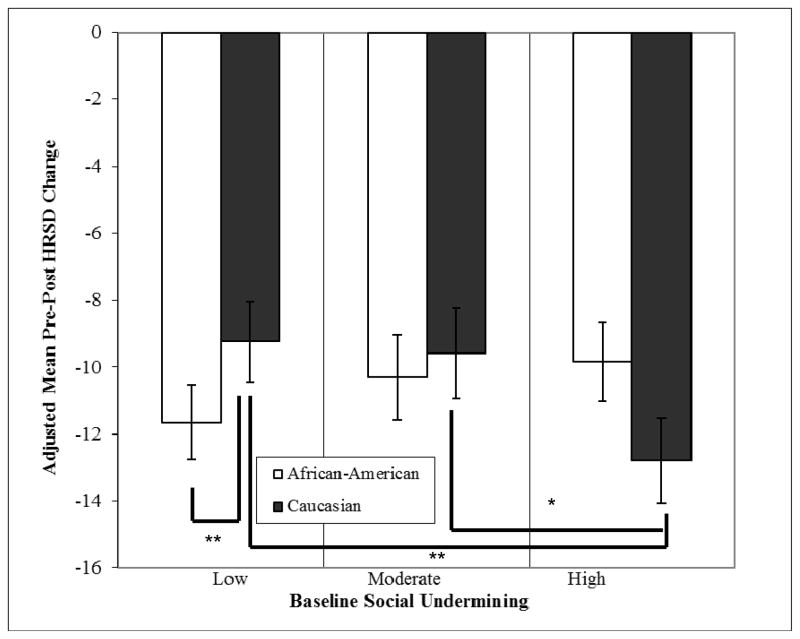
The hierarchical multiple regression model significantly accounted for amount of HRSD symptom reduction from baseline to final week in the trial, F(11, 289) = 2.55, p=.004, R2 = .09. As shown in Table 2, independent of ethnicity, education, and final CIT dose, the interaction of ethnicity and social undermining was significantly associated with symptom improvement, Fchange = 8.36, p=.004, final b = −.21. Post-Hoc analyses indicated that symptom reduction increased significantly among the Caucasians as social undermining increased (Fchange = 6.09, p=.015, final b = −.31), but among African-Americans this relationship was non-significant. Viewed another way, African-Americans experienced greater symptom reduction than Caucasians (Fchange = 6.80, p=.01, Cohen’s d=.28) under conditions of low social undermining (i.e. those with scores in the lowest tertile), but evidenced slightly, but non-significantly lower symptom improvement than Caucasians under conditions of greater exposure to social undermining (i.e. those with scores in the second and third tertiles of social undermining).
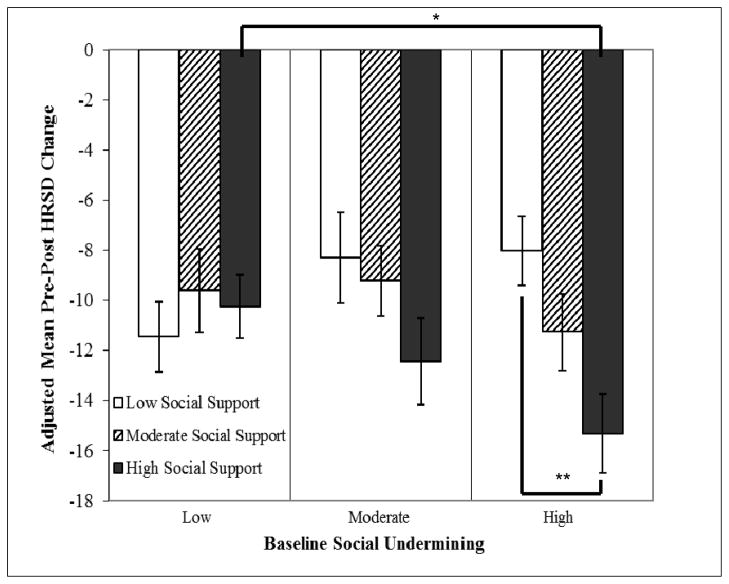
Results also indicated that social support moderated the effect of social undermining on symptom improvement, Fchange = 7.02, p=.009, final b = −.18, such that under conditions of higher social undermining, social support was associated with greater symptom reduction. For example, among participants experiencing high social undermining, social support was significantly associated with symptom reduction, Fchange = 7.00, p=.009, with a greater difference in symptom reduction between those with both high social support and high social undermining vs. those with low social support and high social undermining (Cohen’s d=.86). In contrast, among those experiencing low social undermining, social support had no significant benefit. These interactions are displayed in Figures 1 and 2 respectively.
Figure 1.
Adjusted mean pre-post HRSD change as a function of ethnicity and levels of social undermining (groups determined by tertile split).
** = p < .01
* = p < .05
Figure 2.
Adjusted mean pre-post HRSD change as a function of levels of social undermining and social support (groups determined by tertile split).
** = p < .01
* = p < .05
None of the other direct effects or interactions was significantly associated with reduction in depressive symptoms.
Impact of Changes in Psychosocial Factors
The hierarchical multiple regression model testing the effect of changes in psychosocial factors over time significantly accounted for pre-post change in HRSD symptom reduction from baseline to final week in the trial, F(8, 174) = 3.20, p=.002, R2 = .13. Independent of ethnicity, education, and final CIT dose, change in social undermining was significantly associated with symptom improvement, Fchange = 4.05, p=.046. However, when all of the changes in the psychosocial variables are included in the analysis, only change in social support was an independent predictor of symptom improvement, final b = −.23.
Regressions Predicting Remission
Impact of Baseline Factors
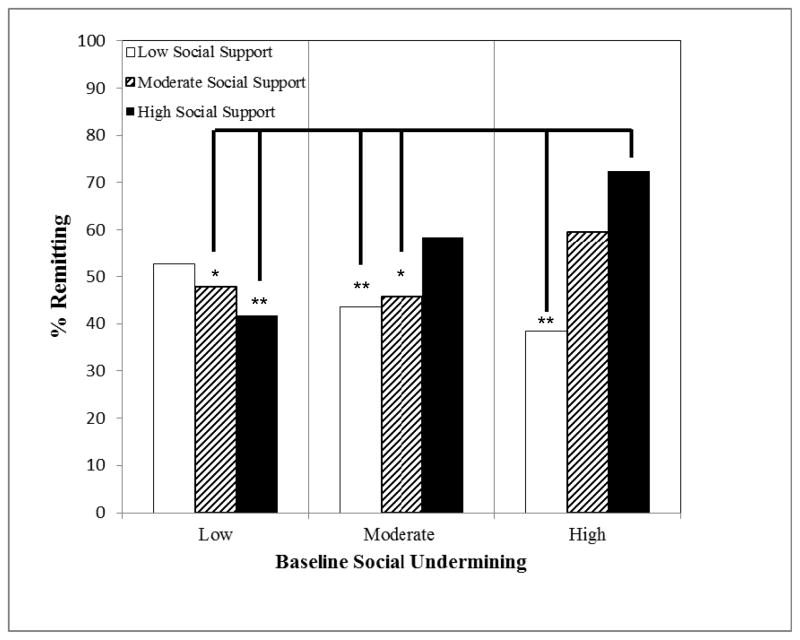
Binary logistic regressions revealed that, independent of ethnicity, education, and final CIT dose, social support moderated the association of social undermining with likelihood of remission (B = .002, Exp(B) = 1.002, p = .047), such that, as social undermining increases, the positive effect of social support on likelihood of remission increases. This interaction is displayed in Figure 3.
Figure 3.
Percent remitting as a function of social undermining and social support (groups determined by tertile split).
** = p < .01
* = p < .05
Note: Each p level indicates the statistical difference in percent remitting compared to the high social undermining, high social support group.
Impact of Changes in Psychosocial Factors
Binary logistic regressions testing for effects of changes in social support and social undermining over time on likelihood of remission revealed that, after accounting for ethnicity, education, and final CIT dose, change in social support was significantly associated with likely of remission (B = .04, Exp(B) = 1.04, p = .023), but change in social undermining was not, (B = −.02, Exp(B) = .98, p = .654). Chi square analyses were conducted to explore further the influence of social support change score on remission, with those who evidenced increases in social support given a score of 1 and those with no change or decreases in social support given a 0. Results of this analysis indicated that increase in social support was significantly associated with greater likelihood of remitting, χ2(1, N = 186) = 6.11, p = .016, such that the majority of those who remitted (i.e., 68%) reported receiving greater social support at the end of the trial than at study entry.
Discussion
The current study provides partial support for our hypotheses and initial evidence that interactions among sets of psychosocial factors and changes in these factors over time in treatment may affect symptom reduction while treated with CIT. Specifically, results showed that, independent of ethnicity, education, final CIT dosage, and the direct effects of other psychosocial variables, increases in social support during the trial and exposure to both high social undermining and high social support at entry into treatment were associated with greater symptom improvement over the course of treatment with CIT. Results also showed that social undermining at treatment entry had a counterintuitive effect on symptom reduction among the Caucasians participants but not among the African-Americans. This finding is noteworthy given that there were no significant overall ethnic differences in treatment response regardless of whether response was measured as magnitude of pre-post change, remission rates, number of completers, number of visits made, final dose of medication or in side effect profiles (see Lesser et al., 2010).
It is very interesting that the combination of high social undermining and high social support was the most conducive to symptom reduction and remission. One possibility is that those patients who evidenced the greatest improvement were those who experienced both greater criticism for their symptoms and functional limitations due to their depression along with strong support for seeking treatment. These experiences may have been conducive to behavioral activation, which is a common element of psychotherapeutic treatment for depression. It is also interesting that social support had little beneficial effect on those who had experienced low levels of social undermining, which supports the notion that social support serves best as a buffer between undesirable circumstances and psychological well-being. In contrast, increases in social support were directly associated with symptom reduction and remission, but decreases in social undermining had no effects on symptom improvement.
It is also important to note that contrary to expectation, burden of chronic stress had no effect on treatment outcome. This finding fits with theories of depression that underscore the strong role of interpersonal relationships in activating cognitive vulnerabilities to the onset and maintenance of major depression. It is also possible that chronic stressors may not have had a strong impact on depression during the trial due to participants’ adjustment to the presence of these ever-present stressors and these stressors not being salient on a daily basis throughout this short-term trial.
It is also interesting that, at low levels of social undermining, African-Americans fared better than Caucasians in terms of symptom reduction, but at high levels of social undermining, they were somewhat less able to achieve the same symptom reduction and the Caucasians fared better. In fact, Caucasians with high amounts of social undermining achieved greater symptom reduction than Caucasians with low amounts of social undermining. Was there some unmeasured characteristic of this sub-sample of participants that allowed them to thrive under conditions of social undermining and maybe use social undermining productively? Other empirical findings suggest that this may be a potential explanation. For example, Mazure and colleagues (2000) found that stressful interpersonal events within the 6 months before the initiation of antidepressant treatment was related to better outcome after 6-weeks of treatment, particularly among individuals high on sociotrophy. Other possible explanations for this counter-intuitive finding were explored, but none were substantiated by the data. For example, the possibility that group differences in decreases in social undermining by the end of the trial (i.e., 2 months after baseline) could explain this finding was not substantiated because Caucasians and African-Americans did not differ on patterns of change in social undermining by the end of the trial. Additionally, although Caucasians with more baseline social undermining experienced significantly greater decrease in social undermining by the end of the trial than Caucasians with low baseline social undermining, they continued to experience relatively more social undermining at the end of the trial.
One possible explanation for our counterintuitive finding that we could not explore empirically is the possibility that the social undermining measure did not capture the most salient social undermining relationships in participants’ lives because the same four important people were rated for support and undermining. It is possible that others in participants’ lives engaged in much more undermining towards them and that participants did not happen to list these people as one of their four important people. Examples of potentially significant sources of undermining are supervisors and coworkers (e.g., Gant et al., 1993), in-laws, friends or neighbors. Despite the fact that participants rated the same individuals on supportive behaviors and undermining behaviors, social support and social undermining variables were not correlated, i.e., r = .05 at baseline and r = .09 at Week 8. This lack of correlation indicates that, in our sample, support and undermining are different processes that occur contemporaneously within the same relationships. Similarly, Vinokur and colleagues have used confirmatory factor analyses to demonstrate that, although support and undermining are usually inversely correlated in their studies, they are not simply different manifestations of the same construct (e.g., Vinokur et al., 1996; Vinokur & van Ryn, 1993). Furthermore, most studies that examine support and undermining have participants rate the same individual on support and undermining. For example, much of the work in this area is on support and undermining from a spouse or significant other (e.g., Cranford, 2004; Vinokur & van Ryn, 1993; Vinokur & Vinokur-Kaplan, 1990).
The findings from our study suggest that future clinical trials should give more attention to assessing and tracking changes in psychosocial factors. Our findings also demonstrate that, using standardized protocols and adequate individualized medical attention, individuals with different levels of chronic stress burdens can achieve equivalent levels of symptom reduction and remission. Findings from the current study also suggest that, for individuals experiencing high levels of social undermining upon initiating antidepressant treatment, social support interventions might be useful adjuncts. Additionally, particularly for African-Americans, engaging an individual’s close social network in the treatment process and problem solving may be especially helpful. Finally, the fact that social undermining influenced whether participants completed the trial supports the notion that psychosocial factors are likely to affect treatment compliance and treatment response to pharmacotherapy.
Several limitations should be noted in interpreting these findings. First, due to the relatively modest sample size and consequent power limitations, null findings in this paper should be interpreted with caution. Second, it is also important not to assume that these findings will generalize to other treatment samples because the medications were provided free of charge to study participants. Outside of a clinical trial, financially disadvantaged patients are likely to experience poorer treatment response due to the inability to consistently access and pay for medications.
Third, because the focus of this trial was the examination of ethnic differences in treatment response rather than the efficacy of CIT, which has already been well documented, the study did not include a placebo-control group. Therefore, the effects of CIT, psychosocial variables, and unexamined variables cannot be easily disentangled. Along these lines, in the case of the association between social support change and symptom change and remission, causality cannot be determined. In other words, it may be possible that those who were experiencing more symptom improvement in the first several weeks of the trial (i.e., less depressed than at baseline) were better able to enlist social support by the end of the trial or were able to perceive the social support they were already receiving at baseline more positively due to less entrapment in a negative cognitive style at that point. Finally, the current study only examined participants during their first 8 weeks of exposure to CIT. Future studies should include a longer follow-up period to test for the long-term effects of psychosocial variables on the maintenance of symptom improvements, as well as whether ethnic differences become more or less apparent after a longer follow-up period. Future treatment outcome studies should also test for the association between change in chronic stress burden over the course of treatment and improvement over time.
More studies are needed to replicate the current findings and directly explore explanations for these results. Future studies conducted by this research group will explore the associations of other psychosocial variables, such as childhood adversity, spirituality, and religiosity, as well as biological variables (i.e., differences between the groups in the distribution of gene polymorphisms in the promoter region of the serotonin transporter and CYP2C19 genes), with symptom reduction in this trial. One promising suggestion of this study is that, although psychosocial variables may make some difference in the amount of symptom improvement and likelihood of remission, more participants responded to antidepressant treatment despite adverse psychosocial circumstances than did not respond.
Table 2.
Hierarchical Regression Analysis of Pre-Post HRSD Change
| Step | Variable | Final β | SE(B) | Final Beta | R2change | F change |
|---|---|---|---|---|---|---|
| 1 | Demographics | .017 | 1.679 | |||
| Ethnicity | .441 | .918 | .029 | |||
| Education | −.080 | .201 | −.024 | |||
| Final Dosage | .070 | .033 | .119* | |||
| 2 | Baseline Chronic Stress | −.022 | .062 | −.026 | .003 | .996 |
| 3 | Baseline Social Undermining | .060 | .074 | .063 | .000 | .076 |
| 4 | Baseline Social Support | −.036 | .033 | −.091 | .008 | 2.392 |
| 5 | EthnicityXChronicStress | −.053 | .107 | −.037 | .004 | 1.275 |
| 6 | EthnicityXSocial Undermining | −.307 | .113 | −.205** | .027 | 8.359** |
| 7 | EthnicityXSocSup | −.047 | .048 | −.078 | .005 | 1.574 |
| 8 | ChronicStressXSocSup | .003 | .003 | .079 | .002 | .605 |
| 9 | Social UnderminingXSocSup | −.007 | .003 | −.181** | .022 | 7.019** |
p < .01
p < .05
Acknowledgments
The authors would like to acknowledge with appreciation the significant contributions of the research staff and clinical research coordinators at each of the three study sites, as well as all of the patients who participated in the trial.
The study is registered on ClinicalTrials.gov (ID# NCT00047671) and was supported by NIMH Grant Nos. R01MH62675, R01MH62676, R01MH62677, and M01RR00425.
References
- Abbey A, Abramis DJ, Caplan RD. Effects of different sources of social support and social conflict on emotional well-being. Basic and Applied Social Psychology. 1985;6:111–129. [Google Scholar]
- Backs-Dermott BJ, Dobson KS, Jones SL. An evaluation of an integrated model of relapse in depression. Journal of Affective Disorders. 2010;124:60–67. doi: 10.1016/j.jad.2009.11.015. [DOI] [PubMed] [Google Scholar]
- Bjornsson TD, Wagner JA, Donahue SR, Harper D, Karim A, Khouri MS, Murphy WR, Roman K, Schneck D, Sonnichsen DS, Stalker DJ, Wise SD, Dombey S, Loew C. A review and assessment of potential sources of ethnic differences in drug responsiveness. Journal of Clinical Pharmacology. 2003;43:943–967. doi: 10.1177/0091270003256065. [DOI] [PubMed] [Google Scholar]
- Bosworth HB, Voils CI, Potter GG, Steffens DC. The effects of antidepressant medication adherences as well as psychosocial and clinical factors on depression outcome among older adults. International Journal of Geriatric Psychiatry. 2008;23:129–134. doi: 10.1002/gps.1852. [DOI] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang N, Ford DE. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Downey G. Social factors and psychopathology: stress, social support, and coping processes. Annual Review of Psychology. 1991;42:401–425. doi: 10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- Cranford JA. Stress-buffering or stress-exacerbation? Social support and social undermining as moderators of the relationship between perceived stress and depressive symptoms among married people. Personal Relationships. 2004;11:23–40. doi: 10.1111/j.1475-6811.2004.00069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle JM. What race and ethnicity measure in pharmacologic research. Journal of Clinical Pharmacology. 2006;46:401–404. doi: 10.1177/0091270005282633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezquiaga E, Garcia A, Pallarés T, Bravo MF. Psychosocial predictors of outcome in major depression: a prospective 12-month study. Journal of Affective Disorders. 1999;52:209–216. doi: 10.1016/s0165-0327(98)00057-3. [DOI] [PubMed] [Google Scholar]
- Foster DA, Caplan RD, Howe GW. Representativeness of observed couple interaction: couples can tell, and it does make a difference. Psychological Assessment. 1997;9:285–294. [Google Scholar]
- Gant LM, Nagdo BA, Brabson HV, Jayaratne S, Chess WA, Singh A. Effects of social support and undermining on African American workers’ perceptions of coworker and supervisor relationships and psychological well-being. Social Work. 1993;38:158–164. [PubMed] [Google Scholar]
- Goodman SH, Brand SR. Depression and early adverse experiences. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 2. New York, NY: Guilford Press; 2008. pp. 249–274. [Google Scholar]
- Gurung RAR, Taylor SE, Kemeny M, Myers H. “HIV is not my biggest problem”: The impact of HIV and chronic burden on depression in women at risk for AIDS. Journal of Social and Clinical Psychology. 2004;23:490–511. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Social stress and women’s risk for recurrent depression. Archives of Women’s Mental Health. 2003;6:9–13. doi: 10.1007/s00737-002-0160-4. [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68:782–787. [PubMed] [Google Scholar]
- Hwang W, Myers HF, Abe-Kim J, Ting JY. A conceptual paradigm for understanding culture’s impact on mental health: the cultural influences on mental health (CIMH) model. Clinical Psychology Review. 2008;28:211–227. doi: 10.1016/j.cpr.2007.05.001. [DOI] [PubMed] [Google Scholar]
- Keller MB. Citalopram therapy for depression: a review of 10 years of European experience and data from U.S. clinical trials. Journal of Clinical Psychiatry. 2000;61:896–908. [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events, and risk for major depression in women. Psychological Medicine. 2004;34:1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J, Prescott CA. Sex differences in the relationship between social support and risk for major depression: a longitudinal study of opposite-sex twin pairs. American Journal of Psychiatry. 2005;162:250–256. doi: 10.1176/appi.ajp.162.2.250. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Walters EE, Kessler RC. The prediction of length of Major Depressive episodes: Results from an epidemiological sample of female twins. Psychological Medicine. 1997;27:107–117. doi: 10.1017/s0033291796003893. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Lesser IM, Castro DB, Gaynes BN, Gonzalez J, Rush AJ, Alpert JE, Trivedi M, Luther JF, Wisniewski SR. Ethnicity/race and outcome in the treatment of depression: results from STAR*D. Medical Care. 2007;45:1043–1051. doi: 10.1097/MLR.0b013e3181271462. [DOI] [PubMed] [Google Scholar]
- Lesser IM, Myers HF, Lin K, Mira CB, Joseph NT, Olmos NT, Schettino J, Poland RE. Ethnic differences in antidepressant response: a prospective multi-site clinical trial. Depression and Anxiety. 2010;27:56–62. doi: 10.1002/da.20619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin K, Poland RE, Silver B. Overview: the interface between psychobiology and ethnicity. In: Lin K, Poland RE, Nakasaki G, editors. Psychopharmacology and Psychobiology of Ethnicity. Washington, D.C: American Psychiatric Press, Inc; 1993. pp. 11–36. [Google Scholar]
- Mazure CM, Bruce ML, Maciejewski PK, Jacobs SC. Adverse life events and cognitive-personality characteristics in the prediction of major depression and antidepressant response. American Journal of Psychiatry. 2000;157:896–903. doi: 10.1176/appi.ajp.157.6.896. [DOI] [PubMed] [Google Scholar]
- Myers HF, Lesser I, Rodriguez N, Mira CB, Hwan W, Camp C, Anderson D, Erickson L, Wohl M. Ethnic differences in clinical presentation of depression in adult women. Cultural Diversity and Ethnic Minority Psychology. 2002;8:138–156. doi: 10.1037/1099-9809.8.2.138. [DOI] [PubMed] [Google Scholar]
- Okun MA, Keith VM. Effects of positive and negative social exchanges with various sources on depressive symptoms in younger and older adults. Journal of Gerontology: Psychological Sciences. 1998;53B:4–20. doi: 10.1093/geronb/53b.1.p4. [DOI] [PubMed] [Google Scholar]
- Paxton KC, Myers HF, Hall NM, Javanbakht M. Ethnicity, serostatus, and psychosocial differences in sexual risk behavior among HIV-seropositive and HIV-seronegative women. AIDS and Behavior. 2004;8:405–415. doi: 10.1007/s10461-004-7325-2. [DOI] [PubMed] [Google Scholar]
- Pedrelli P, Feldman GC, Vorono S, Fava M, Petersen T. Dysfunctional attitudes and perceived stress predict depressive symptoms severity following antidepressant treatment in patients with chronic depression. Psychiatry Research. 2008;161:302–308. doi: 10.1016/j.psychres.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: the Social Support Questionnaire. Journal of Personality and Social Psychology. 1983;44:127–139. [Google Scholar]
- Sayal K, Checkley S, Rees M, Jacobs C, Harris T, Papadopoulosa A, Poon L. Effects of social support during weekend leave on cortisol and depression ratings: a pilot study. Journal of Affective Disorders. 2002;71:153–157. doi: 10.1016/s0165-0327(01)00414-1. [DOI] [PubMed] [Google Scholar]
- Sherbourne C, Schoenbaum M, Wells KB, Croghan TW. Characteristics, treatment patterns, and outcomes of persistent depression despite treatment in primary care. General Hospital Psychiatry. 2004;26:106–114. doi: 10.1016/j.genhosppsych.2003.08.009. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Revenson TA, Tennen H. Health psychology: psychological adjustment to chronic disease. Annual Review of Psychology. 2007;58:565–592. doi: 10.1146/annurev.psych.58.110405.085615. [DOI] [PubMed] [Google Scholar]
- Tomaszewska W, Peselow ED, Barouche F, Fieve RR. Antecedent life events, social supports and response to antidepressants in depressed patients. Acta Psychiatrica Scandinavica. 1996;94:352–357. doi: 10.1111/j.1600-0447.1996.tb09872.x. [DOI] [PubMed] [Google Scholar]
- Vallejo J, Gasto C, Catalan R, Bulbena A, Menchon JM. Predictors of antidepressant treatment outcome in melancholia: psychosocial, clinical and biological indicators. Journal of Affective Disorders. 1991;21:151–162. doi: 10.1016/0165-0327(91)90036-r. [DOI] [PubMed] [Google Scholar]
- Vinokur AD, Price RH, Caplan RD. Hard times and hurtful partners: how financial strain affects depression and relationship satisfaction of unemployed persons and their spouses. Journal of Personality and Social Psychology. 1996;71:166–179. doi: 10.1037//0022-3514.71.1.166. [DOI] [PubMed] [Google Scholar]
- Vinokur AD, van Ryn M. Social support and undermining in close relationships: their independent effects on the mental health of unemployed persons. Journal of Personality and Social Psychology. 1993;65:350–359. doi: 10.1037//0022-3514.65.2.350. [DOI] [PubMed] [Google Scholar]
- Vinokur AD, Vinokur-Kaplan D. “In sickness and in health”: patterns of social support and undermining in older married couples. Journal of Aging and Health. 1990;2:215–241. [Google Scholar]
- Voils C, Steffens DC, Flint EP, Bosworth HB. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. American Journal of Geriatric Psychiatry. 2005;13:157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- Wagner GJ, Maguen S, Rabkin JG. Ethnic differences in response to fluoxetine in a controlled trial with depressed HIV-positive patients. Psychiatric Services. 1998;49:239–240. doi: 10.1176/ps.49.2.239. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS. Prevalence and distribution of Major Depressive Disorder in African-Americans, Caribbean Blacks, and Non-Hispanic Whites: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]