Abstract
Background: Inadequate fruit and vegetable consumption is associated with increased chronic disease risk and represents a considerable global health burden. Despite evidence that dietary habits track from early childhood, there are few published trials of interventions attempting to increase preschoolers’ fruit and vegetable consumption.
Objective: The Healthy Habits trial aimed to assess the efficacy of a telephone-based intervention for parents to increase the fruit and vegetable consumption in their 3–5-y-old children.
Design: A cluster randomized controlled trial was conducted involving 394 parents of children aged 3–5 y recruited through local preschools. Parents allocated to the intervention received printed resources plus four 30-min telephone calls targeting aspects of the home food environment associated with children's fruit and vegetable consumption. Parents allocated to the control group received generic printed nutrition information. Children's fruit and vegetable consumption was assessed by using the Fruit and Vegetable Subscale of the Children's Dietary Questionnaire, which was administered via telephone interview at baseline and 2 and 6 mo later.
Results: Analysis of all available data showed that children's fruit and vegetable scores were significantly higher in the intervention group than in the control group at 2 mo (P < 0.001) and at 6 mo (P = 0.021). Sensitivity analysis using baseline observation carried forward showed an intervention effect at 2 mo (P = 0.008) but not at 6 mo (P = 0.069).
Conclusions: Telephone-delivered parent interventions may be an effective way of increasing children's fruit and vegetable consumption in the short term. Further investigation to determine whether the intervention effect is maintained in the longer term is recommended. This trial was registered at http://www.anzctr.org.au as ACTRN12609000820202.
INTRODUCTION
Inadequate fruit and vegetable consumption increases chronic disease risk (1–3) and represents a considerable health burden worldwide (4). Evidence suggests that childhood dietary patterns track into adulthood (5), and high fruit and vegetable consumption in childhood has been associated with a lower risk of adulthood stroke and cancer (6, 7). Because early childhood is important in the development of dietary habits (8), interventions to promote young children's fruit and vegetable intakes may help to establish dietary habits that decrease chronic disease risk in adulthood.
Systematic reviews have identified a dearth of quality intervention studies to increase fruit and vegetable consumption in preschoolers (children aged 3–5 y) (9, 10). Most of the published trials have investigated multicomponent interventions conducted in the preschool setting and have predominantly targeted the policies and practices within the preschool environment (11–14). Interventions targeting the home environment, however, may be particularly effective (9) given that social and physical characteristics of the home environment are among the strongest correlates of children's fruit and vegetable consumption (15, 16). Despite this, to our knowledge, only one published intervention trial has targeted the home food environment of preschoolers. In this randomized controlled trial of 1306 disadvantaged, rural-dwelling participants in the United States, an intervention consisting of 4 home visits, resources, and tailored newsletters had no overall effect on children's fruit and vegetable intakes at 6–11 mo of follow-up (17).
Given evidence of the efficacy of telephone-delivered interventions in improving adult dietary behaviors (18, 19), telephone interventions delivered to parents and targeting the home environment may represent an effective primary prevention strategy to enhance children's fruit and vegetable intake. As such, we recently conducted a pre-post pilot trial and reported a significant postintervention increase in preschoolers’ fruit and vegetable consumption immediately after a 4-contact, telephone-based intervention (20). On the basis of the pilot findings and the broader telephone and health behavior literature (19), we sought to test the longer-term efficacy of the intervention in an appropriately powered randomized controlled trial.
The primary aim of the current study was to assess the efficacy of a telephone-based intervention for parents to increase the fruit and vegetable consumption of their 3–5-y-old children. It was hypothesized that the change in children's fruit and vegetable scores from baseline to 2 mo and from baseline to 6 mo would be greater in the intervention children than in the control children. Given that dietary patterns that include a high intake of fruit and vegetables have been associated with higher food costs (21), as an assessment of a possible adverse effect, an additional aim was to determine whether intervention participation was associated with an increase in reported weekly household food expenditure.
SUBJECTS AND METHODS
Design overview
The Healthy Habits trial used a cluster randomized controlled design and was prospectively registered with the Australian New Zealand Clinical Trials Registry. All trial outcomes and subgroup analyses reported in this article were prespecified. The research was approved by the Human Research Ethics Committees of the University of Newcastle (H-2008-0410) and the Hunter New England Area Health Service (08/10/15/5.09). This article reports the 2- and 6-mo primary trial outcomes collected via telephone interviews with the parents. The methods used to conduct this trial were published elsewhere (22) and are described briefly below.
Participants
Parents were recruited through preschools within 4 Local Government Areas of the Hunter region of New South Wales, Australia, by using strategies found to be effective in increasing participation in child health research (23). All nongovernment preschools were eligible to participate if they did not provide meals to children, did not exclusively cater for children with special needs, or had not been involved in healthy eating studies within the preceding 6 mo. At preschools where the manager consented to participate, a research assistant, blind to preschool allocation, distributed study information and consent forms to parents as they dropped off or picked up their child. The consent form contained questions about the child's usual fruit and vegetable consumption and the child's sex, age, and residential postal code. To assess bias due to selective nonparticipation, all parents were asked to complete these details on the consent form, even if they chose not to consent to participate in the study. Parents were eligible to participate if they had a 3–5-y-old child who resided with them for ≥4 d/wk, were responsible for providing food to their child at least half of the time, had a child with no dietary requirements that would make Australian fruit and vegetable intake recommendations unsuitable, and were literate in English. Recruitment took place from February to August 2010.
Randomization and allocation
After the commencement of parent recruitment, a statistician not associated with the project used a random number function in Microsoft Excel to allocate preschools to the intervention or control group. Randomization was carried out at the level of the preschool to reduce potential contamination from parents at the same preschool sharing intervention information or resources. Randomization of preschools was stratified by socioeconomic status based on the decile of disadvantage classification of the postal code area in which the preschool was located (24). Preschools were randomly assigned in a 1:1 ratio (intervention:control) in randomly sequenced blocks of between 2 and 6 preschools. Parents were informed of group allocation via a letter after baseline data collection.
Experimental group
Intervention
Parents allocated to the intervention group received 4 telephone calls over a period of 4 wk. Intervention participants were also mailed a series of instructional resources, including a guidebook, a meal planner, cookbooks, and a water bottle for all family members. A complete description of the intervention is provided in the trial protocol (22). Telephone-delivered interventions of a similar intensity were previously shown to be effective at increasing adult health behaviors (25, 26). An overview of the intervention content and structure is provided in Table 1.
TABLE 1.
Intervention content, strategies, and structure1
| Key theme | Content | Behavior change technique | Application of behavior change technique |
| Week 1: Availability and accessibility | • Dietary recommendations and serving sizes | ||
| • Children's food diary • Ways to provide fruit and vegetables throughout the day | • Prompt self-monitoring of behavior | • Parents are asked to monitor their children's intake of fruit and vegetables over 3 d | |
| • Setting goals | • Prompt specific goal-setting | • Parents are encouraged to set a program goal | |
| Week 2: Availability and accessibility, supportive family eating routines | • Changing the family routine • Availability and accessibility of foods in the home • Mealtime practices • Meal planning • Review of goals | • Prompt intention formation • Provide general encouragement • Teach to use prompts or cues • Prompt review of behavioral goals | • Parents decide which activities they will attempt in the coming week • Interviewers provide positive feedback about any helpful practices occurring in the home • Parents learn the HELPS acronym, ie, try to eat when Hungry, not attempting anything else at the same time (focus on Eating), at an appropriate Location to eat, from a Plate, and while Sitting • Parents review the goals they set during the previous calls and evaluate their progress |
| Week 3: Parental role-modeling, supportive family eating routines | • The Ps and Cs division of feeding responsibility • Mealtime strategies to encourage vegetable consumption • Role-modeling of fruit and vegetable consumption | • Teach to use prompts or cues • Prompt intention formation • Provide general encouragement • Prompt identification as a role model | • Parents learn the Ps and Cs: parents are encouraged to Plan, Prepare, and Provide. Children are encouraged to Choose (whether, what, and how much to eat) (27) • Parents decide which activities they will attempt in the coming week • Interviewers provide positive feedback about any helpful practices occurring in the home • Parents are provided information about their importance in role-modeling fruit and vegetable consumption; their consumption is compared with national nutrition recommendations, and tailored feedback is provided |
| Week 4: Availability and accessibility, parental role-modeling, supportive family eating routines | • Review of weeks 1 to 3 • Planning for the future and dealing with difficult situations • Review of goals | • Provide general encouragement • Prompt barrier identification • Prompt review of behavioral goals | • Interviewers provide positive feedback about any helpful practices occurring in the home • Parents are encouraged to identify barriers that will prevent them from implementing what they have learned and to generate solutions • Parents review their program goal, evaluate their progress, and identify how they can maintain the change |
From Wyse et al (22). Cs, responsibilities of the “children,” which are to “choose whether or not to eat,” “choose what to eat from a variety of healthy options,” and “choose how much to eat at scheduled meal and snack times” Ps, responsibilities of the “parents”—to “plan,” “prepare,” and “provide.”
The intervention assumes that children's fruit and vegetable consumption stems from the complex interaction between personal, cultural, and environmental factors and draws on socioecologic theory (28). Specifically, the intervention used the conceptual model of family-based intervention proposed by Golan and Weizman (29) in the treatment and prevention of childhood obesity. This model focuses on introducing new familial norms associated with healthy eating. This is achieved through making changes within the home food environment, providing positive parental role-modeling, and increasing knowledge and skills related to parenting and nutrition (29). The intervention used a range of behavior-change techniques as classified in the taxonomy proposed by Abraham and Michie (30) to encourage parents to make such changes (Table 1). These techniques included goal setting, behavioral self-monitoring, intention formation, use of prompts or cues, and review of behavioral goals (30). The calls focused on increasing fruit and vegetable availability and accessibility in the home, increasing parental role-modeling of fruit and vegetable consumption, and enhancing supportive food routines around the home, such as eating dinner as a family without the television on. The calls were scripted and delivered by using computer-assisted telephone interview (CATI)4 (31) software. Participants had to complete each call before progressing to the next, ie, no intervention calls could be skipped. All participants received information relating to each intervention content area (Table 1). Within content areas, however, the information provided was tailored based on assessments made during baseline data collection or earlier intervention calls regarding the participant's home food environment, parenting, or dietary practices. For example, to facilitate role-modeling, parents already regularly consuming fruit and vegetables in front of their children (based on baseline assessment) were congratulated and encouraged to maintain this behavior. Parents not routinely modeling consumption of these foods, however, were given the opportunity to set a goal to work toward achieving this over the next week and were provided with strategies to assist with goal attainment. Parents could be offered between 1 and 4 activities to undertake between calls. Data from the pilot trial suggest that parents actively engaged in these tasks (20).
The scripts and the resources were extensively pretested and piloted (20). Five experienced health interviewers with no formal qualifications in nutrition or psychology and not blind to participant allocation delivered the scripted telephone support. Interventionists received 2 d of training in script delivery and associated nutrition and parenting issues from an accredited practicing dietitian, a psychologist specializing in parenting, and health-promotion practitioners and were then required to complete an additional 10 h of delivery practice. For the duration of the intervention delivery period (April to December 2010), interventionists participated in biweekly group supervision sessions with a psychologist specializing in parenting to ensure that any arising issues were dealt with in an appropriate and standardized manner. Members of the research team monitored each interventionist multiple times throughout the intervention delivery period to assess adherence to the intervention protocol.
Control
Parents allocated to the control group were mailed the Australian Guide to Healthy Eating—a 22-page booklet outlining the dietary guidelines and ways to meet them (32). They received no further contact until the 2-mo follow-up data collection call.
Data collection and blinding
All data collection occurred via CATI by using trained telephone interviewers. Participants could be contacted on landlines or mobile numbers and were called ∼1 wk after recruitment to complete the baseline survey and then ∼2 and 6 mo later for follow-up data collection. At each time point, data collectors attempted to contact participants for a 2-mo period, and, if the call could not be completed, contact was attempted again at the subsequent follow-up point. The baseline survey was conducted from April to October 2010. Parents were instructed to complete the baseline and follow-up surveys with respect to their preschool-aged child. If they had more than one child aged 3–5 y, they were instructed to select the child who would have the next birthday. Data collectors received 4 h of training in script delivery and during the data-collection periods were regularly monitored by members of the study team to ensure standardized survey delivery across data collectors. Data collectors were blind to group allocation. To assess whether blinding was maintained, after collection of follow-up trial outcomes, the CATI system prompted the data collector to nominate the group to which they thought the participant had been allocated. The proportion of times data collectors correctly identified group allocation at each time point was calculated.
Measures
Participant characteristics
Information regarding parent and child characteristics was collected from the consent form and the baseline CATI. The consent form included questions about child sex, age, and postal code and 2 items that assessed the child's usual daily intake of fruit and vegetable servings. These items were included to allow for comparison between those who did and did not consent to study participation. During the CATI, participants were asked their age, their sex, their annual household income, their highest level of education, whether they identified as Aboriginal and/or Torres Strait Islander, the number of children in their household, and the number of servings of fruit and vegetables they consumed daily. Participants also reported their child's date of birth and sex and whether their child identified as Aboriginal and/or Torres Strait Islander.
Childrenrsquos fruit and vegetable intake
Children's fruit and vegetable intake was the primary trial outcome and was assessed at baseline and at the 2- and 6-mo follow-ups by using the Fruit and Vegetable Subscale (F&V) of the Children's Dietary Questionnaire. The subscale has been established as reliable (test-retest intraclass correlation coefficient = 0.75) in samples of 39 children aged 4–5 y and 92 children aged 5–16 y and was established as valid as compared with a 7-d checklist (Spearman correlation coefficient = 0.58) in samples of 126 children aged 5–6 y and 132 children aged 5–10 y (33). A preliminary assessment using data from a sample of 126 children aged 5–10 y indicated that the subscale demonstrated the ability to detect change in the hypothesized direction (Wilcoxon's signed rank test, P < 0.001) (33).
The scale requires parents to report the frequency and variety of fruit and vegetables consumed by their child over the previous 24 h and previous 7 d. Scores on this scale can range from 0 to 28, with a score of ≥14 indicating that the child is meeting Australian Dietary Guidelines (33). An increase in the score could arise from a range of changes to children's fruit and vegetable consumption patterns, eg, a 1-point increase could result from eating an additional type of fruit or vegetable or eating fruit or vegetable at an additional occasion in the previous 24 h.
Food expenditure
Participants were asked at baseline and at each follow-up to estimate their average weekly household expenditure on food: “On average, how much do you spend on food for your household each week? This includes foods you buy from the supermarket as well as any foods you buy and eat outside the home, for example, takeaway, restaurant meals, lunches.” The psychometric properties of this item are unknown.
Process measures
Intervention fidelity. The number of intervention calls completed by participants was automatically recorded by the CATI system. During the monitoring of intervention calls, members of the research team used a checklist to record whether the interventionist discussed the key topics of each call (eg, serving size recommendations) and the extent to which they delivered the script as per the protocol (always, mostly, sometimes, rarely, or never).
Data collection. The CATI system automatically recorded the date, time, and outcome of each data collection call attempt. The proportion of times data collectors correctly identified the participants’ group allocation at each time point was calculated.
Sample size calculation
The sample size allowed a detectable difference between the intervention and control F&V scores of 1.27 (equivalent to a change of 0.25 of an SD), with 80% power at the 0.05 significance level. Assuming an intraclass correlation coefficient of 0.03 [unpublished data from Good for Kids. Good for Life, Australia's largest childhood obesity prevention program (34)], it was calculated that recruiting 400 parents from 30 preschools would achieve the desired sample of 300 participants (150 per group) at the final follow-up data collection at 18 mo.
Analysis
All statistical tests were performed by using SAS version 9.2 statistical software (SAS Institute). Descriptive statistics were used to describe the study sample and process measures. Data were analyzed by using an intention-to-treat approach, whereby all participants were analyzed based on the group to which they were allocated. For the analyses of F&V scores at follow-up, a linear regression model within a generalized estimating equation (GEE) framework was used to account for clustering by preschool. The GEE accounts for clustering by weighting each cluster inversely to its variance matrix, which is a function of the within-cluster dependence (35). Children's F&V score at baseline was included as a covariate. Significance testing was performed with an α level of 0.05. Determination of intervention efficacy was based on an analysis using all available data and specified a priori (22). This main analysis compared intervention and control F&V scores at 2 mo and at 6 mo and assumed that any missing data at follow-up were missing at random and included all participants with complete baseline and 2-mo data and baseline and 6-mo data, respectively. Little's test was performed to determine whether the missing data were missing completely at random (36). A sensitivity analysis, specified a priori, was undertaken to ensure that the findings of the main analysis were robust against the missing data assumptions of the GEE. This involved imputing missing data at the 2- or 6-mo follow-up by using baseline observation carried forward. A per-protocol analysis was also undertaken in which only intervention participants who had received all 4 telephone calls were included. When randomized trials are conducted, both sensitivity and per-protocol analyses are recommended to aid interpretation of the trial outcome (37). A subgroup analysis was also conducted. The sample was divided into 2 subgroups: those whose children were and those whose children were not meeting national dietary guidelines for fruit and vegetable consumption at baseline (ie, a baseline F&V score ≥14 or <14), and a GEE model was fitted that included a subgroup by experimental group interaction. Changes in reported food expenditure at 2 and 6 mo were also assessed by using a GEE model adjusted for baseline values and by using participants with no missing data at 2 and 6 mo, respectively, on this measure.
RESULTS
Participant characteristics
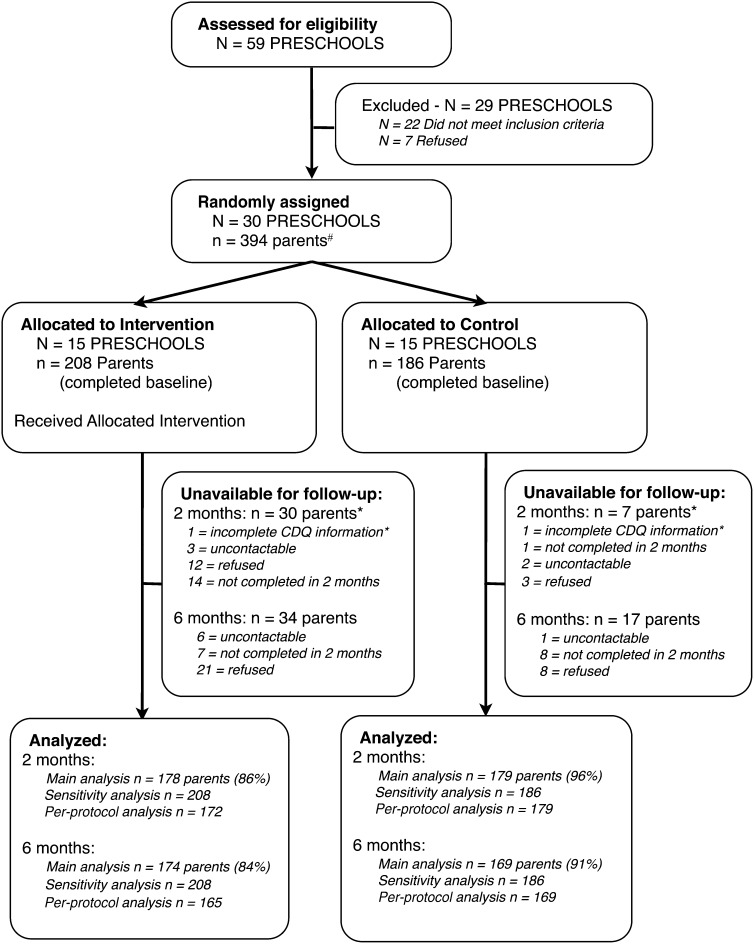
Children from ∼2200 families attended the 30 eligible and consenting preschools. In total, 418 parents returned a signed consent form indicating a willingness to participate, 394 of whom completed the baseline telephone survey and were included in the study; 178 parents did not consent to participate but returned a form with completed demographic details. The preschool and participant flow throughout the trial is shown in Figure 1.
FIGURE 1.
Consolidated Standards of Reporting Trials diagram showing cluster (preschool) and participant (parent) flow throughout the trial. #Although 418 parents consented, 24 parents were not randomly assigned because they were subsequently uncontactable (n = 5), did not meet inclusion criteria (n = 9), or refused to complete the baseline survey when contacted (n = 10). *Two parents were excluded from the 2-mo analysis because they had been away from their child for the previous 24 h and/or previous 7 d and were unable to answer questions about their child's fruit and vegetable consumption. CDQ, Children's Dietary Questionnaire.
The characteristics of participants allocated to the intervention and control groups were similar (Table 2). No significant differences in child age, sex, or daily intake of fruit or vegetables were found between study participants and the children of 202 parents who either did not consent or initially consented but did not complete the baseline survey. When compared with a random sample of parents of 3–5-y-olds from the broader study region, participants in the current study had higher levels of education (47% compared with 36% with tertiary education) and higher household incomes (41% compared with 20% ≥US$100,000) (38). The proportion of children consuming at least one daily fruit serving in the current sample was similar to a random sample of 2–4-y-old children in a broader region (96% compared with 96%), but more children in the study sample were consuming ≥2 servings of vegetables each day (65% compared with 48%) (39).
TABLE 2.
Characteristics of the 394 participants who completed baseline by group1
| Parent and child demographic characteristics | Control(n = 186) | Intervention(n = 208) |
| Parents | ||
| Age (y) | 35.7 ± 5.02 | 35.2 ± 5.6 |
| Female sex (%) | 96.8 | 95.2 |
| Household income ≥$100,000 (%) | 40.2 | 42.4 |
| University education (%) | 49.5 | 45.2 |
| Aboriginal and/or Torres Strait Islander (%) | 3.2 | 1.0 |
| No. of children aged <16 y in household | 2.3 ± 0.7 | 2.3 ± 0.8 |
| No. of daily servings of fruit | 1.8 ± 1.0 | 1.8 ± 1.1 |
| No. of daily servings of vegetables | 3.1 ± 1.3 | 3.3 ± 1.3 |
| Children | ||
| Age (y) | 4.3 ± 0.6 | 4.3 ± 0.6 |
| Female sex (%) | 45.7 | 51.0 |
| Aboriginal and/or Torres Strait Islander (%) | 4.8 | 1.0 |
| No. of daily servings of fruit3 | 2.2 ± 1.0 | 2.3 ± 1.0 |
| No. of daily servings of vegetables3 | 2.0 ± 1.2 | 2.1 ± 1.1 |
Between-group differences at baseline were tested by using chi-square tests for categorical data and t tests for continuous data; there were no significant differences between the intervention and control groups (P < 0.05).
Mean ± SD (all such values).
Information taken from a consent form.
In total, 86% and 84% of participants allocated to the intervention and 96% and 91% of participants allocated to the control group provided 2- and 6-mo follow-up data, respectively. No significant differences in demographic characteristics or in baseline fruit and vegetable intakes were found between the intervention group participants who completed and those who did not complete the 2- or 6-mo follow-up surveys. Among the control group, participants who did not complete the 6-mo follow-up consumed more vegetable servings per day (mean ± SD: 3.8 ± 1.0 compared with 3.0 ± 1.3; P = 0.013) at baseline and were less likely to have a tertiary education qualification (24% compared with 52%; P = 0.025) than were control participants who provided 6-mo data.
Childrenrsquos fruit and vegetable intakes
The analysis showed that the mean F&V scores were significantly higher in the intervention than in the control group at both the 2-mo and 6-mo follow-ups (Table 3). Little's test (χ2 = 15.233, 2 df, P < 0.001) (36) was significant, which suggests that group allocation and the children's F&V score at baseline predicted missing data at follow-up. In the sensitivity analysis, the intervention effect remained significant when children's F&V scores at baseline were carried forward for missing data at the 2-mo follow-up. Although the effect was nearly significant when such values were carried forward at the 6-mo follow-up, the effect was not significant (Table 3). The per-protocol analysis showed that intervention participants who completed all 4 intervention calls had significantly higher F&V scores than did control participants at 2 and 6 mo (Table 3). The subgroup analysis comparing children who did and did not meet the dietary guidelines at baseline found that the subgroup-by-experimental group interaction term was not significant.
TABLE 3.
Fruit and Vegetable Subscale scores in the intervention and control groups at baseline, 2 mo, and 6 mo1
| Time point | Mean ± SEM |
Regression coefficient (95% CI)2 | P value | |
| Control | Intervention | |||
| Main analysis | ||||
| Baseline (n = 394) | 14.5 ± 0.4 | 15.0 ± 0.3 | — | |
| 2 mo (n = 357) | 15.4 ± 0.3 | 17.0 ± 0.3 | 1.28 (0.54, 2.03) | <0.001 |
| 6 mo (n = 343) | 15.9 ± 0.3 | 17.0 ± 0.3 | 0.80 (0.12, 1.49) | 0.021 |
| Sensitivity analysis | ||||
| Baseline (n = 394) | 14.5 ± 0.4 | 15.0 ± 0.3 | — | |
| 2 mo (n = 394) | 15.3 ± 0.3 | 16.6 ± 0.3 | 0.98 (0.26, 1.70) | 0.008 |
| 6 mo (n = 394) | 15.8 ± 0.2 | 16.7 ± 0.2 | 0.59 (−0.05, 1.22) | 0.069 |
| Per-protocol analysis | ||||
| Baseline (n = 367) | 14.5 ± 0.4 | 15.2 ± 0.4 | — | |
| 2 mo (n = 351) | 15.4 ± 0.3 | 17.1 ± 0.3 | 1.34 (0.59, 2.10) | <0.001 |
| 6 mo (n = 334) | 15.9 ± 0.3 | 17.1 ± 0.3 | 0.87 (0.17, 1.56) | 0.014 |
Data were analyzed by using a generalized estimating equation framework, adjusted for children's scores at baseline and clustering within preschools (P < 0.05).
Adjusted for baseline scores.
Food expenditure
At the 2-mo follow-up, the estimated weekly food expenditure in intervention households was significantly lower than that in control households, adjusted for the baseline values, and no significant difference was observed at 6 mo (Table 4).
TABLE 4.
Estimated weekly food expenditure in the intervention and control groups at baseline, 2 mo, and 6 mo1
| Mean ± SEM |
||||
| Estimated weekly food expenditure | Control | Intervention | Regression coefficient (95% CI)2 | P value |
| US$ | US$ | US$ | ||
| Baseline (n = 392) | 234 ± 3 | 241 ± 7 | — | — |
| 2 mo (n = 358) | 252 ± 5 | 235 ± 5 | −20 (−32, −8) | <0.001 |
| 6 mo (n = 342) | 246 ± 5 | 245 ± 7 | −5 (−17, 7) | 0.426 |
Data were analyzed by using a generalized estimating equation framework, adjusted for weekly food expenditure at baseline and clustering within preschools (P < 0.05).
Adjusted for baseline expenditure.
Process measures
Intervention fidelity
Of the 208 participants allocated to the intervention, 87% completed all 4 intervention calls. No significant differences in parent or child demographic characteristics or baseline fruit and vegetable consumption were found between those who completed all intervention calls (n = 181) and those who did not (n = 27). Among those who did not, 16 participants did not complete the first call, 6 participants completed only the first call, 4 completed the first 2 calls, and 1 participant completed 3 calls. The mean duration of all intervention calls was 29 min (34, 30, 26, and 28 min for calls 1–4, respectively). In total, 44 intervention calls were monitored, representing 6% of all completed calls and an average of 9 calls per interventionist. Across all monitored calls, interventionists covered 97% of key content areas, and in >80% of calls they “rarely” deviated from the script. In instances in which calls deviated from the script, interventionists were provided with feedback immediately after the call, and the issue was raised during biweekly supervision.
Data collection
On average, 74 d (2.4 mo) elapsed between baseline and the scheduled 2-mo data collection call, and an average of 198 d (6.5 mo) elapsed between baseline and the scheduled 6-mo call; no differences were observed between groups in the time elapsed from baseline to either follow-up point. At the conclusion of the 2-mo and 6-mo follow-ups, data collectors correctly identified the participants’ group allocation in 59% (P < 0.001) and 56% (P = 0.027) of cases, respectively, which represents slightly more cases than would be expected by chance. In accordance with the study protocol, 43 data collection calls (4%) were monitored across the 3 time points, and, in every instance, interviewers delivered the questions as per the protocol “all” or “most of the time.”
DISCUSSION
This is the first randomized controlled trial of a telephone-based primary prevention intervention to increase fruit and vegetable consumption in preschool-aged children. An analysis using all available data showed that children whose parents were randomly allocated to receive 4 weekly scripted support calls had higher fruit and vegetable scores at 2 and 6 mo after baseline than did children whose parents were randomly allocated to receive printed nutrition material. The sensitivity analysis, which adopted a conservative imputation approach (baseline observation carried forward), found a significant intervention effect at 2 mo, which was nearly significant at 6 mo. The effect of the intervention did not vary between children who were and those who were not meeting fruit and vegetable dietary guidelines at baseline. Furthermore, increases in child fruit and vegetable scores did not coincide with increases in household expenditure on food, which suggested that the intervention did not pose any additional financial burden on families.
The findings are promising given the limited effectiveness of interventions attempting to increase young children's fruit and vegetable consumption. The only randomized controlled trial of an intervention that explicitly targeted the home food environment to encourage fruit and vegetable consumption of preschool children failed to increase fruit and vegetable consumption overall but increased intake among a subsample of normal-weight children (17). The intervention, which also consisted of 4 intervention contacts, was delivered via home visits to a sample of predominantly disadvantaged families (20–25% university educated, 50–60% with an annual household income <$35,000) (17). The contrasting findings may reflect the difficulties experienced by socioeconomically disadvantaged parents, relative to the current sample, of increasing children's fruit and vegetable intake. Whereas the effect of this telephone-based intervention on children from disadvantaged families is not known, more intensive telephone-based support, which is considerate of the distinct challenges of disadvantaged families [including cost, work schedules, lack of time, and lack of skills and confidence (40–42)], may maximize the potential effectiveness and acceptability of a telephone-based approach to such parents. Nonetheless, the results are consistent with the pilot study (20) and with systematic reviews finding strong evidence of the efficacy of adult dietary interventions delivered by telephone (19, 43).
Given the positive trial findings, the research has many important public health implications. First, the intervention was relatively brief, scripted, and delivered by nonspecialist staff. Such attributes suggest that the intervention could easily be integrated into existing telephone support services (44) and may be relatively inexpensive compared with services using specialist health professionals for the provision of child nutrition support. Second, the intervention had high retention rates (87%) and was previously found to be acceptable to parents (20), indicating broad appeal of this form of support. Finally, the intervention was delivered by using a modality that affords almost population-wide access in the developed world (45). As such, the intervention has the potential to overcome barriers to parent use of traditional support services, such as conflicting or inflexible schedules, time constraints, and transport difficulties (41, 46), particularly those faced by rural and socioeconomically disadvantaged households (41), and should be tested with a less-advantaged sample. Collectively, such research suggests that the telephone-based intervention may represent an appealing policy option for governments or other health agencies to improve public health nutrition and reduce future chronic disease.
The strengths of this study included the experimental design, the standardization of intervention delivery (via scripted dialogue appearing on computer screens), and consideration of unintended cost effects of the intervention. There were, however, many study limitations that warrant consideration. The sample included participants who, on average, were more educated and had a higher household income than did a random sample of parents within the study region, and, as such, further investigation examining intervention effectiveness in more disadvantaged populations is recommended. Furthermore, the generalizability of the findings may be limited by the high proportion of children consuming the recommended number of daily vegetable servings at baseline, compared with the broader study area. The subgroup analysis, however, suggested that no significant difference in intervention efficacy was observed between children who consumed high or low amounts of fruit and vegetables at baseline. As is common in trials of behavioral interventions (47), parent participants in this trial were unblinded, and the primary outcome measure was subjectively assessed by parent report, which increased the risk of a biased assessment of intervention effect (48). Furthermore, the primary outcome was assessed by using a food-frequency questionnaire. Whereas this tool represented the only measure of fruit and vegetable consumption available to the research team that had been validated on a sample of Australian preschool children (33, 49), a more comprehensive method of dietary assessment—such as food records or 24-h dietary recalls—may have yielded more accurate assessments of intake (50) and allowed for a more meaningful comparison with other studies. Finally, by the end of each survey, outcome assessors were 6–9% more likely than chance to correctly identify the group to which participants were allocated, which potentially increased the risk of detection bias (48).
Many opportunities for further research exist. Although the analysis using all available data showed a significant intervention effect at both 2 and 6 mo of follow-up, the sensitivity analysis fell short of significance at 6 mo. Research is therefore required to confirm these findings. Whereas the presence of a short-term intervention effect is encouraging, further investigation to determine whether the effect is maintained in the longer term is also warranted. Research into the optimal schedule of telephone contacts could increase the efficiency of the intervention by determining the maximum effect that can be obtained for a given level of resources. Investigating the characteristics of the home food environment that mediated the relation between the intervention and dietary behavior (eg, parent knowledge, self-efficacy, and fruit and vegetable availability) would also allow a greater understanding of the causal pathways and further intervention refinement and may result in greater efficiencies in intervention delivery (51). Notwithstanding the study limitations, and the value of further research in this area, the study represents an important contribution to the scientific literature regarding public health interventions addressing childhood fruit and vegetable consumption.
Acknowledgments
We thank Patrick McElduff for his statistical advice and Jenna Hollis for the crucial role she played in the trial's administration. We acknowledge the indispensable contribution of the Hunter New England Population Health CATI interviewers in delivering the intervention and collecting the data and sincerely thank the preschool supervisors and the parents for their generous participation.
The authors’ responsibilities were as follows—LW: conceived of the project idea; LW, RW, EC, JW, KJC, LB, JB, TRH, and AF: designed the research; KJC and LB: provided expert advice on the design and implementation of the intervention; RW, AF, LW, and LB: conducted the research; RW and LW: analyzed the data and performed the statistical analysis; and RW: led the development of the manuscript and had primary responsibility for the final content. All authors contributed to the drafts and read and approved the final manuscript. None of the authors reported a conflict of interest.
Footnotes
Abbreviations used: CATI, computer-assisted telephone interview; F&V, Fruit and Vegetable Subscale; GEE, generalized estimating equation.
REFERENCES
- 1.World Cancer Research Fund/American Institute for Cancer Research Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, DC: AICR, 2007 [Google Scholar]
- 2.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr 2006;136:2588–93 [DOI] [PubMed] [Google Scholar]
- 3.He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet 2006;367:320–6 [DOI] [PubMed] [Google Scholar]
- 4.Lock K, Pomerleau J, Causer L, Altmann DR, McKee M. The global burden of disease attributable to low consumption of fruit and vegetables: implications for the global strategy on diet. Bull World Health Organ 2005;83:100–8 [PMC free article] [PubMed] [Google Scholar]
- 5.Mikkilä V, Rasanen L, Raitakari OT, Pietinen P, Viikari J. Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: the Cardiovascular Risk in Young Finns Study. Eur J Clin Nutr 2004;58:1038–45 [DOI] [PubMed] [Google Scholar]
- 6.Ness AR, Maynard M, Frankel S, Smith GD, Frobisher C, Leary SD, Emmett PM, Gunnell D. Diet in childhood and adult cardiovascular and all cause mortality: the Boyd Orr cohort. Heart 2005;91:894–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maynard M, Gunnell D, Emmett P, Frankel S, Davey Smith G. Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. J Epidemiol Community Health 2003;57:218–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birch LL. Development of food preferences. Annu Rev Nutr 1999;19:41–62 [DOI] [PubMed] [Google Scholar]
- 9.Hector D, Shrewsbury V. Building solutions for preventing childhood obesity. Module 2: Interventions to increase consumption of fruit and vegetables. Sydney, Australia: NSW Centre for Overweight and Obesity, 2008 [Google Scholar]
- 10.Campbell KJ, Hesketh KD. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes Rev 2007;8:327–38 [DOI] [PubMed] [Google Scholar]
- 11.Bayer O, von Kries R, Strauss A, Mitschek C, Toschke AM, Hose A, Koletzko BV. Short- and mid-term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster-randomized trial. Clin Nutr 2009;28:122–8 [DOI] [PubMed] [Google Scholar]
- 12.Witt KE, Dunn C. Increasing fruit and vegetable consumption among preschoolers: evaluation of Color Me Healthy. J Nutr Educ Behav 2012;44:107–13 [DOI] [PubMed] [Google Scholar]
- 13.Vereecken C, Huybrechts I, van Houte H, Martens V, Wittebroodt I, Maes L. Results from a dietary intervention study in preschools “Beastly Healthy at School.” Int J Public Health 2009;54:142–9 [DOI] [PubMed] [Google Scholar]
- 14.Hardy LL, King L, Kelly B, Farrell L, Howlett S. Munch and Move: evaluation of a preschool healthy eating and movement skill program. Int J Behav Nutr Phys Act 2010;7:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr 2009;12:267–83 [DOI] [PubMed] [Google Scholar]
- 16.Rasmussen M, Krolner R, Klepp KI, Lytle L, Brug J, Bere E, Due P. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part I: Quantitative studies. Int J Behav Nutr Phys Act 2006;3:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haire-Joshu D, Elliott MB, Caito NM, Hessler K, Nanney MS, Hale N, Boehmer TK, Kreuter M, Brownson RC. High 5 for Kids: the impact of a home visiting program on fruit and vegetable intake of parents and their preschool children. Prev Med 2008;47:77–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanwormer JJ, Boucher JL, Pronk NP. Telephone-based counseling improves dietary fat, fruit, and vegetable consumption: a best-evidence synthesis. J Am Diet Assoc 2006;106:1434–44 [DOI] [PubMed] [Google Scholar]
- 19.Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med 2007;32:419–34 [DOI] [PubMed] [Google Scholar]
- 20.Wyse R, Wolfenden L, Campbell E, Campbell K, Brennan L, Fletcher A, Bowman J, Heard T, Wiggers J. A pilot study of a telephone-based parental intervention to increase fruit and vegetable consumption in 3-5-year-old children. Public Health Nutr (Epub ahead of print 23 June 2011) [DOI] [PubMed] [Google Scholar]
- 21.Drewnowski A, Darmon N, Briend A. Replacing fats and sweets with vegetables and fruits—a question of cost. Am J Public Health 2004;94:1555–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wyse RJ, Wolfenden L, Campbell E, Brennan L, Campbell KJ, Fletcher A, Bowman J, Heard TR, Wiggers J. A cluster randomised trial of a telephone-based intervention for parents to increase fruit and vegetable consumption in their 3- to 5-year-old children: study protocol. BMC Public Health 2010;10:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolfenden L, Kypri K, Freund M, Hodder R. Obtaining active parental consent for school-based research: a guide for researchers. Aust N Z J Public Health 2009;33:270–5 [DOI] [PubMed] [Google Scholar]
- 24.Australian Bureau of Statistics Census of population and housing: Socio-Economic Indexes for Areas (SEIFA) (2033.0.55.001). Canberra, Australia: ABS, 2006 [Google Scholar]
- 25.Green BB, McAfee T, Hindmarsh M, Madsen L, Caplow M, Buist D. Effectiveness of telephone support in increasing physical activity levels in primary care patients. Am J Prev Med 2002;22:177–83 [DOI] [PubMed] [Google Scholar]
- 26.Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 2003;326:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satter E. Feeding dynamics: helping children to eat well. J Pediatr Health Care 1995;9:178–84 [DOI] [PubMed] [Google Scholar]
- 28.Robinson T. Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. J Community Health 2008;33:395–406 [DOI] [PubMed] [Google Scholar]
- 29.Golan M, Weizman A. Familial approach to the treatment of childhood obesity: conceptual mode. J Nutr Educ 2001;33:102–7 [DOI] [PubMed] [Google Scholar]
- 30.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379–87 [DOI] [PubMed] [Google Scholar]
- 31.Choi BC. Computer assisted telephone interviewing (CATI) for health surveys in public health surveillance: methodological issues and challenges ahead. Chronic Dis Can 2004;25:21–7 [PubMed] [Google Scholar]
- 32.Kellet E, Smith A, Schmerlaib Y. The Australian guide to healthy eating: background information for consumers. Canberra, Australia: The Australian Government Department of Health and Ageing, 1998 [Google Scholar]
- 33.Magarey A, Golley R, Spurrier N, Goodwin E, Ong F. Reliability and validity of the Children's Dietary Questionnaire; a new tool to measure children's dietary patterns. Int J Pediatr Obes 2009;4:257–65 [DOI] [PubMed] [Google Scholar]
- 34. Good for kids. Good for life. 2010. Available from: http://www.goodforkids.nsw.gov.au (cited 9 November 2011)
- 35.Liang KY, Zeger SL. Regression analysis for correlated data. Annu Rev Public Health 1993;14:43–68 [DOI] [PubMed] [Google Scholar]
- 36.Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc 1988;83:1198–12 [Google Scholar]
- 37.Porta N, Bonet C, Cobo E. Discordance between reported intention-to-treat and per protocol analyses. J Clin Epidemiol 2007;60:663–9 [DOI] [PubMed] [Google Scholar]
- 38.Wolfenden L, Hardy LL, Milat A, Bell C, Sutherland R, Wiggers J. Prevalence and socio-demographic associations of overweight and obesity among children attending childcare services in rural and regional New South Wales Australia. Nutr Diet 2011;68:15–20 [Google Scholar]
- 39.Centre for Epidemiology and Research New South Wales Population Health Survey 2007-2008 (HOIST). New South Wales, Australia: NSW Department of Health, 2008 [Google Scholar]
- 40.Omar MA, Coleman G, Hoerr S. Healthy eating for rural low-income toddlers: caregivers’ perceptions. J Community Health Nurs 2001;18:93–106 [DOI] [PubMed] [Google Scholar]
- 41.Katz I, La Placa V, Hunter S. Barriers to inclusion and successful engagement of parents in mainstream services. York, United Kingdom: Joseph Rowntree Foundation, 2007 [Google Scholar]
- 42.Winkler E, Turrell G. Confidence to cook vegetables and the buying habits of Australian households. J Am Diet Assoc 2009;109:1759–68 [DOI] [PubMed] [Google Scholar]
- 43.Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med 2012;42:81–8 [DOI] [PubMed] [Google Scholar]
- 44.O'Hara BJ, Bauman AE, King EL, Phongsavan P. Process evaluation of the advertising campaign for the NSW Get Healthy Information and Coaching Servce. Health Promot J Austr 2011;22:68–71 [DOI] [PubMed] [Google Scholar]
- 45. International Telecommunications Union. Global ICT developments. 2008. Available from: http://www.itu.int/ITU-D/ict/statistics/ict/index.html (cited 9 November 2011)
- 46.Lamb-Parker F, Piotrkowski CS, Baker AJL, Kessler-Sklar S, Clark B, Peay L. Understanding barriers to parent involvement in Head Start: a research-community partnership. Early Child Res Q 2001;16:35–51 [Google Scholar]
- 47.Boutron I, Tubach F, Giraudeau B, Ravaud P. Blinding was judged more difficult to achieve and maintain in nonpharmacologic than pharmacologic trials. J Clin Epidemiol 2004;57:543–50 [DOI] [PubMed] [Google Scholar]
- 48.The Cochrane Collaboration Cochrane handbook for systematic reviews of interventions (version 5.1.0, March 2011). Available from: http://www.cochrane.org/training/cochrane-handbook (cited 2 October 2011) [Google Scholar]
- 49. Australasian Child and Adolescent Obesity Research Network (ACAORN). ACAORN repository of tools to measure dietary intake in children and adolescents—September 2009. Available from: www.acaorn.org.au/streams/nutrition/Pub_Repository_diet_assess_tools_Sept2009.pdf (cited 1 February 2012)
- 50.McPherson RS, Hoelscher DM, Alexander M, Scanlon KS, Serdula MK. Dietary assessment methods among school-aged children: validity and reliability. Prev Med 2000;31:S11–33 [Google Scholar]
- 51.Cerin E, Mackinnon DP. A commentary on current practice in mediating variable analyses in behavioural nutrition and physical activity. Public Health Nutr 2009;12:1182–8 [DOI] [PMC free article] [PubMed] [Google Scholar]