Abstract
Risk factors of mortality in burn patients such as inhalation injury, patient age, and percent of total body surface area (%TBSA) burned have been identified in previous publications. However, little is known about the variability of mortality outcomes between burn centers and whether the admitting facilities or facility volumes can be recognized as predictors of mortality. De-identified data from 87,665 acute burn observations obtained from the National Burn Repository between 2003 and 2007 were used to estimate a multivariable logistic regression model that could predict patient mortality with reference to the admitting burn facility/facility volume, adjusted for differences in age, inhalation injury, %TBSA burned, and an additional factor, percent full thickness burn (%FTB). As previously reported, all three covariates (%TBSA burned, inhalation injury, and age) were found to be highly statistically significant risk factors of mortality in burn patients (P value < 0.0001). The additional variable, %FTB, was also found to be a statistically significant determinant, although it did not greatly improve the multivariable model. The treatment/admitting facility was found to be an independent mortality predictor, with certain hospitals having increased odds of death and others showing a protective effect (decreased odds ratio). Hospitals with high burn volumes had the highest risk of mortality. Mortality outcomes of patients with similar risk factors (%TBSA burned, inhalation injury, age, and %FTB) are significantly affected by the treating facility and their admission volumes.
The American Burn Association has reported that one million Americans suffer from burn injuries per year, with roughly 140,000 requiring hospitalization for appropriate treatment and serious burns, accounting for approximately 7,000 deaths in 2006.1 Burn deaths occur in a bimodal distribution, either immediately after the injury or weeks later due to multiorgan failure. Young adults, children younger than 15 years of age, and the elderly tend to be at an increased risk for burn injury, as are patients from lower socioeconomic classes and unsafe environments.2 In the past 20 years, prevention efforts leading to decreases in the number and extent of burn injuries, as well as advances in therapy, such as earlier emergency responses, improved resuscitation efforts and treatment of inhalation injuries, and enhanced wound care have decreased the number of burn hospital admissions and deaths by 50 percent.2, 3
Despite advances in burn prevention and care, patient morbidity and mortality remain evident, generating a significant socioeconomic burden. Inhalation injuries, percent total body surface area (%TBSA) burned, and age have been suggested as major risk factors of burn mortality, with the presence of all three risk factors (to a great degree) being associated with a mortality as high as 90 percent.3
Although most surgeons agree that burn treatment consists of minimization of heat loss, resuscitation, appropriate wound care, etc., burn centers will frequently report varying rates of morbidity and mortality.1, 4 Though some of these disparities may be attributable to geographic differences in patient populations and previously acknowledged variability in National Burn Repository (NBR) data accuracy, divergent care practices and real differences in clinical efficacy that influence the survival of individual patients are also likely to be present. The purpose of this paper is to document the magnitude of the survival differences of burn patients admitted to different facilities by adjusting survival rates for variation in %TBSA burned, inhalation injury, age, and percent full thickness burn (%FTB).
Methods
Data Source
Data were extracted from the National Burn Repository database maintained by the American Burn Association (ABA), with burn admission data collected from 73 (52%) of 140 verified and nonverified burn centers in the United States and Canada in 2007. This computerized database contains information on outpatient, inpatient, or rehabilitation visits. With personal identifiers removed, patient age, gender, race, year of injury, mortality status and cause, percent total body surface area burned, degrees of burns, preexisting medical conditions, inhalation injury, and several other variables are stored in the database. Although the ABA originally developed NBR to collect basic information on hospitalized patients for the treatment of burns, participation in the burn registry has since become a required component for burn center verification. Unfortunately, NBR database does not include facility Burn Verification Status, and de-identified center data further eliminates the possibility of identifying Verification Status from additional sources.
Data Collection
Seventy-three hospitals from 30 states plus the District of Columbia contributed to a total of 306,304 records. Analysis was performed on 57 hospitals that contributed more than 500 cases, having a reasonable cross sectional representation of United States hospitals with no single center dominating. Only cases of acute burn injuries with admission type “initial” during the period from 2003 to 2007 were included (n = 154,574). Readmissions, rehabilitation, outpatient cases, records without hospital identifiers, admissions not related to burn injury, records with missing outcome variable (death), age, and inhalation injury were excluded from the analysis. Those with missing %TBSA burned and %FTB were included, however, since exclusion of these subjects would result in elimination of more than 85 per cent of the records. Although imputation techniques were considered for the substitution of missing values, previous studies using NBR database have shown that results are essentially unchanged when imputation versus exclusion of missing data is used.5
Variable Selection
Admission facility was identified for each patient. Patient demographics, in-hospital mortality, and key determinants of burn outcomes (%TBSA burned group, age, and inhalation injury) were included based on prior studies.6 Percent full thickness burn (%FTB group) was also used, because it was considered to be a potentially significant predictor of mortality risk.
Statistical Analysis
Descriptive analyses comparing demographic characteristics of survivors and decedents were performed using the χ2 statistic to compare proportions, and Single Factor Analysis of Variance to compare means. A multivariable logistic regression model7 was then generated to estimate mortality risk as a function of the admitting facility, adjusted for patient level covariates (%TBSA burned group, age, inhalation injury, and %FTB group). The maximum adjusted R2 value and C statistic were calculated to assess the proportion of variability explained by the model and to assess the model’s ability to discriminate between survivors and nonsurvivors, respectively. Odds ratios for the adjusted risk of in-hospital deaths were calculated for each facility, with reference to a facility with mortality rate at the overall facility average. In other words, each facility odds ratio (except for the reference facility) represented the relative difference in the odds of death between patients in any admitting facility as compared with the average overall odds of death (reference facility).
Another analysis was performed examining the effect of facility volume on mortality risk, using the same model format, but substituting the facility identifier variable with a variable measuring facility volume. Facility volumes were calculated by summing the total number of patients during the observation period and dividing by the number of years the facility submitted data to the NBR. Volume deciles were then created to assess the potential nonlinear relationship between facility volumes and mortality risk. Odds ratios for the adjusted risk of in-hospital death were calculated for each level of facility volume, with reference to the highest decile of volume, adjusted for %TBSA burned group, inhalation injury, age, and %FTB group.
A second multivariable logistic regression model was developed excluding all patient records with either %TBSA burned group or %FTB group listed as either 0 per cent or as unknown, to assess whether the effects of model covariates were similar in this subset of the study population. The second model otherwise was identical to the original model used to estimate mortality risk.
All statistical analyses were performed using SAS 9.1.3 (SAS Institute, Cary, NC). The research was reviewed by the University of Virginia Internal Review Board and determined to be exempt human subjects research.
Results
Univariate Analysis
A total of 87,665 records from 57 facilities out of the original 306,304 met the inclusion criteria for data analysis. Table 1 presents the distribution of risk factor values among patients discharged alive, discharged deceased, and for the total study population. Three thousand two hundred and fifty-five (3.7%) patients suffered from inhalation injuries, 9,574 (10.9%) were age 65 or older, 8,425 (9.6%) had less than 10 per cent full thickness burns, and 33,282 (37.9%) were found to have less than 25 %TBSA burned. The majority of burn patients were white, male, between the ages of 15 and 25, mostly injured by a flame (41.0%) followed by a scalding injury (30.0%). Death was reported for 3509 patients, or 4.0 per cent of the evaluated population. The single most common cause of death was multi-organ failure, although cause of death was omitted or unknown in almost one-half of the patients. The majority of the deceased were injured by the mechanism of flame burns (70%) or scalding injuries (6%).
Table 1.
Frequency and Percentage Distribution of Study Population Characteristics, by Discharge Status and Overall
| Discharged Alive
|
Discharged Deceased
|
Total
|
||||
|---|---|---|---|---|---|---|
| Number | Percent | Number | Percent | Number | Percent | |
| Total | 84,156 | 100.00 | 3,509 | 100.00 | 87,665 | 100.00 |
| Race (chi-squared P value < 0.0001) | ||||||
| African American | 14,984 | 17.81 | 536 | 15.28 | 15,520 | 17.70 |
| Asian | 1,456 | 1.73 | 49 | 1.40 | 1505 | 1.72 |
| White | 45,000 | 53.47 | 2,022 | 57.62 | 47,022 | 53.64 |
| Hispanic | 9,511 | 11.30 | 226 | 6.44 | 9737 | 11.11 |
| Native American | 517 | 0.61 | 17 | 0.48 | 534 | 0.61 |
| Other | 1,952 | 2.32 | 77 | 2.19 | 2,029 | 2.31 |
| Unknown | 10,736 | 12.76 | 582 | 16.59 | 11,318 | 12.91 |
| Gender (chi-squared P value < 0.0001) | ||||||
| Male | 57,730 | 68.60 | 2,356 | 67.14 | 60,086 | 68.54 |
| Female | 26,426 | 31.40 | 1,153 | 32.86 | 27,579 | 31.46 |
| Age group (chi-squared P value < 0.0001) | ||||||
| 5 years or less | 7,152 | 8.50 | 82 | 2.34 | 7,234 | 8.25 |
| 5 to 15 years | 10,448 | 12.42 | 89 | 2.54 | 10,537 | 12.02 |
| 15 to 25 years | 15,415 | 18.32 | 491 | 13.99 | 15,906 | 18.14 |
| 25 to 35 years | 12,867 | 15.29 | 377 | 10.74 | 13,244 | 15.11 |
| 35 to 45 years | 12,953 | 15.39 | 398 | 11.34 | 13,351 | 15.23 |
| 45 to 55 years | 10,773 | 12.80 | 455 | 12.97 | 11,228 | 12.81 |
| 55 to 65 years | 6,192 | 7.36 | 399 | 11.37 | 6,591 | 7.52 |
| 65 to 75 years | 3,585 | 4.26 | 370 | 10.54 | 3,955 | 4.51 |
| >75 years | 4,771 | 5.67 | 848 | 24.17 | 5,619 | 6.41 |
| Inhalation injury (chi-squared P value < 0.0001) | ||||||
| Yes | 2,615 | 3.11 | 640 | 18.24 | 3,255 | 3.71 |
| No | 81,541 | 96.89 | 2,869 | 81.76 | 84,410 | 96.29 |
| Total burn size percentage group (chi-squared P value < 0.0001) | ||||||
| 0% or unknown | 49,089 | 58.33 | 2,331 | 66.43 | 51,420 | 58.66 |
| >0–5% | 19,129 | 22.73 | 73 | 2.08 | 19,202 | 21.90 |
| >5–25% | 13,743 | 16.33 | 337 | 9.60 | 14,080 | 16.06 |
| >25–50% | 1,705 | 2.03 | 305 | 8.69 | 2,010 | 2.29 |
| > 50% | 490 | 0.58 | 463 | 13.19 | 953 | 1.09 |
| Full thickness burn size percentage group (chi-squared P value < 0.0001) | ||||||
| 0% or unknown | 73,737 | 87.62 | 2,572 | 73.30 | 76,309 | 87.05 |
| >0% to 5% | 6,523 | 7.75 | 105 | 2.99 | 6,628 | 7.56 |
| >5–10% | 1,719 | 2.04 | 78 | 2.22 | 1,797 | 2.05 |
| >10–20% | 1,133 | 1.35 | 140 | 3.99 | 1,273 | 1.45 |
| >20–50% | 821 | 0.98 | 288 | 8.21 | 1,109 | 1.27 |
| >50% | 223 | 0.26 | 326 | 9.29 | 549 | 0.63 |
Multivariate Analysis
Multivariable logistic regression analysis was used to estimate the risk of death as a function of the admitting facility, adjusted for age, presence of inhalation injury, %TBSA burned group, and %FTB group. The model demonstrated good statistical performance, obtaining a C statistic of 0.82, showing adequate discrimination between survivors and decedents. It also obtained a maximum adjusted R2 value of 0.25, indicating that one-fourth of the observed variability in the risk of death was explained by the model. Each covariate in the model, including the admitting facility, was found to be a highly statistically significant predictor of mortality (P < 0.0001), as shown in Table 2. The largest contribution to the model’s predictive performance was provided by patient age group (Wald χ2 = 1586.3), followed by the admitting facility (Wald χ2 = 501.9). The variable %FTB group, although statistically significant, contributed the least to the model’s performance. All originally specified covariates were retained in the final model.
Table 2.
Summary of Mortality Predictors Sorted by their Contribution to the Model’s Predictive Performance (Wald χ2 test statistic)
| All Patients (n = 87,665)
|
Excluding Patients with Total Burn Size or Full Thickness Burn Size = 0% or unknown (n = 11,356)
|
|||||
|---|---|---|---|---|---|---|
| Analysis of effects | Degrees of freedom | Wald χ2 test statistic | P value | Degrees of freedom | Wald χ2 test statistic | P value |
| Age group | 8 | 1,586.3 | <0.0001 | 8 | 593.8 | <0.0001 |
| Admitting facility | 56 | 501.9 | <0.0001 | 56 | 148.4 | <0.0001 |
| Inhalation injury | 1 | 309.8 | <0.0001 | 1 | 110.7 | <0.0001 |
| Total burn size | 4 | 362.1 | <0.0001 | 3 | 100.3 | <0.0001 |
| Full thickness burn size | 5 | 263.2 | <0.0001 | 4 | 157.3 | <0.0001 |
| Model performance | ||||||
| C statistic | 0.82 | 0.95 | ||||
| Maximum adjusted R2 | 0.25 | 0.59 | ||||
The multivariable logistic regression analysis was repeated excluding all patient records with either %TBSA burned group or %FTB group listed as either 0 per cent or as unknown. These results demonstrate that all of the covariates in the model were also statistically significant at the P < 0.0001 level in this subset of patients. Age group provided the largest contribution to the performance of the model (Wald χ2 = 593.8), followed by %FTB group (Wald χ2 = 157.3). The covariate for admitting facility was the third most important variable in this subset analysis (Wald χ2 = 148.4). The model developed for the subset had better statistical performance than the original model, obtaining a C statistic of 0.95 and maximum adjusted R2 of 0.59. This difference in performance reflects the increased frequency of death among patients in the subset of patients with known %TBSA burned group or %FTB group values.
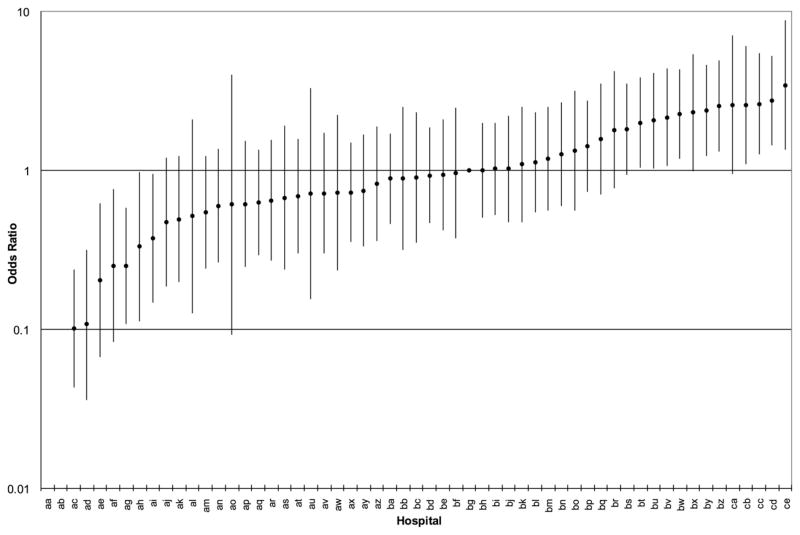
Figure 1 displays facility odds ratios, arranged in an ascending order and adjusted for age, %TBSA burned group, inhalation injury, and %FTB group, each referent to a selected facility (“gb”), with observed mortality approximately equal to the average mortality for the study population. A total of 11 centers were found to have adjusted mortality odds ratios significantly higher than the average odds of death. The facility with the highest risk had an adjusted odds ratio that was 3.5 times higher than the odds in the reference facility. There were seven centers with adjusted mortality odds ratios significantly below 1, or significantly lower than the odds in the reference facility.
Fig. 1.
Odds ratios for each hospital in the study population, compared to the reference hospital (‘bg’), whose unadjusted odds approximately equaled the overall odds of death for the study population (average odds of death). The odds ratios are presented in the order of magnitude, with vertical bars representing minimum and maximum values of the calculated 95% confidence intervals. Odds ratios and 95% confidence interval values are plotted on the logarithmic scale.
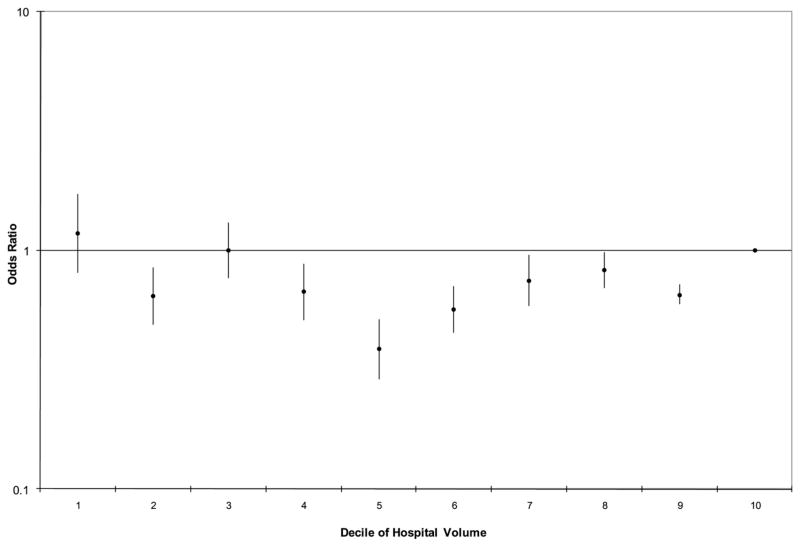
Figure 2 is a graphic representation of adjusted facility odds ratios for deciles of facility volume. Each decile included between five and six hospitals. Each odds ratio is referent to the peak volume decile (decile 10). The results demonstrate that compared with patients in the highest volume decile, patients receiving care in hospitals included in nearly all other deciles (except deciles 1 and 3) were at significantly decreased risk for death. Table 3 lists the distribution of the number of hospitals with higher or lower mortality by volume decile.
Fig. 2.
Plot of the odds ratios for each decile of hospital volume in the study population, with each compared to the mortality risk for patient in the 10th decile of volume, calculated using adjustments for other covariates included in the multivariable logistic regression model. The odds ratios are presented in decile order, with vertical bars representing minimum and maximum values of the 95% confidence intervals calculated for each odds ratio. Odds ratios and 95% confidence interval values are plotted on the logarithmic scale.
Table 3.
Number of Hospitals with Significantly Higher or Lower Mortality (Odds of Death) by Decile of Patient Volume
| Hospital Decile of Patient Volume
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total | |
| Odds ratio lower than expected | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 7 |
| Odds ratio higher than expected | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 2 | 2 | 3 | 10 |
| Total hospitals | 5 | 6 | 6 | 5 | 6 | 6 | 5 | 6 | 6 | 6 | 57 |
Discussion
Improving medical therapy has become an important health care issue for policymakers, physicians, managers, and most importantly patients. As such, a multitude of quality improvement programs have evolved with the intent of reducing morbidity, mortality, and cost. These efforts, and the increasingly prevalent requirements for surgeons to participate in some form of outcomes assessment, means that quality improvement has become an essential part of nearly every surgeon’s professional life.8
The most well known and effective investigations in surgical quality improvement based upon risk-adjusted outcomes assessment to date were performed within the Veterans’ Administration health system as a part of the national quality initiative to assess and improve system deficiencies with regard to surgical patient management. The National Surgical Quality Improvement Program distributed “report cards” to individual centers and witnessed a 28 per cent decrease in unadjusted 30-day mortality and a 43 per cent decrease in unadjusted 30-day morbidity rates since implementation in 1991 (3.2% to 2.3% for mortality and 17.4% to 9.9% for morbidity).9 The National Surgical Quality Improvement Program paradigms and methodology have since been incorporated within similar programs for trauma centers (The Trauma Quality Improvement Program) in the hopes of improving the outcomes of trauma patients. And now, with the publication of these results, a Burn-Center Quality Improvement Program could be envisioned as a natural extension of the nationwide effort to set higher hospital standards and provide better patient care for those with thermal injury.
We performed a retrospective analysis of the NBR database to assess the effects of admitting facilities on burn outcomes. Data showed that mortality was dependent on the treating facility in addition to the already known risk factors—%TBSA burned group, the presence of inhalation injury, and age. An additional factor—%FTB group—was also shown to be a significant predictor of burn outcomes. Although the majority of burn centers report mortality rates that are concordant with the national average, there are facilities whose mortality rates are significantly above or below the mean. The reasons behind these different outcomes are not clear, and could vary between such disparate factors as inaccurate reporting, suboptimal resuscitation protocols, and many others. A study of high- and low-performing centers for the comparison of burn treatment protocols could reveal common themes that may be associated with better outcomes. Furthermore, a comparison between hospital protocols of centers with superior outcomes could yield valuable insights into the determinants of survival after thermal injury. Well performing hospitals may become great educational assets for the burn community.
Admitting volumes could offer an additional explanation of facility mortality rates. From our analysis, it is apparent that treatment of patients with thermal injuries at medium- or low-volume centers does not necessarily result in worse risk-adjusted survival. In fact, higher admitting volumes suggest worse outcomes, perhaps due to the fact that some hospital systems may be overwhelmed with excess patient admissions. At the same time, high volume is not a direct predictor of poor outcomes, since some hospitals have adjusted odds ratios at or below the national average. There may be, in fact, a “sweet-spot” for center volumes, whereby centers receive sufficient number of patients to allow for maintenance of proficiency and streamlining of care, but not so many that critical hospital resources are overwhelmed. Identification of facilities with scarce resources due to an overwhelming volume of patients would help to allocate resources more appropriately in the future.
There are several limitations that need to be addressed with regard to the results of this study. Although data from large registries encompasses information from multiple patient care centers, it may be less accurate then if gathered from a single center or by alternate methods. First, NBR data is extracted by chart review, recording International Classification of Diseases, Ninth Revision codes rather than more precise methods.9 Although this may be the easiest, most efficient, and most consistent form of data gathering, it is not as accurate as patient interviews, surveys, etc. Secondly, data collection may not be identical between burn centers, leading to data misrepresentation. And thirdly, missing or invalid data is extremely problematic in outcomes evaluation. Collection of higher quality information through designation of properly trained personnel would prevent records with missing or incorrect data from being submitted to ABA/NBR. Only after substantial improvements in ABA/NBR data quality could hospitals count on semiannual reports from ABA to identify facilities that require additional resources, create an online registry that would allow generation of yearly outcome reports, and ultimately improve patient care.
One of the limitations of the analysis is the potential influence of missing data on the adjusted odds of death, resulting in inaccurate facility rankings. Many patient records in the Burn-Center Quality Improvement Program data set were excluded because of missing information for the patient characteristics. Systemic differences among hospitals in their reporting of patient age, inhalation injury, %TBSA burned group and %FTB group by patient outcome could potentially bias the comparison of associated odds of death.
Although incomplete, the data available from the National Burn Repository allows the most comprehensive perspective available on burn care mortality outcomes for United States hospitals. In this analysis we have included unknown values of percent total body surface area group variable and unknown values in the percent full thickness group variable as a category of response. The advantage of this approach is that we are able to retain cases in the study population with known values for the other covariates but with unknown values for these variables. The main disadvantage of this approach is that we are not able to accurately measure the effect of percent total body surface area or percent full thickness on mortality risk. Both variables are recognized as key predictors of mortality risk, so excluding these variables from the model would yield suboptimal estimates of mortality risk. Excluding cases with unknown values for these variables was also not the best choice, because this exclusion would substantially bias the results. We were also unable to impute unknown values, given the large number of cases with unknown values.
To address the potential differences among patients with complete data, we developed an otherwise identical multivariable logistic regression model excluding all patients with %TBSA burned group or %FTB group listed as either 0 per cent or as unknown. These results demonstrate that all of the covariates in the model were also statistically significant at the P < 0.0001 level in this subset of the population, and that admitting facility remained one of the most important contributors to the performance of the model.
However, even though the developed model was found to be a good predictor of mortality, higher quality data could potentially change facility rankings allowing for more accurate predictions of facility performances in the future. We do acknowledge that the apparent higher mortality odds ratios observed at higher-volume centers could be attributable to more complete death records—if lower volume centers systematically miss recording mortality data, they would seem to enjoy an improved survival in their population. However, facilities should be encouraged to report accurate data, because that would allow for better resource allocation and ultimately, better patient care via improvements in their protocols.
In addition, there may be other important factors affecting mortality of burn patients that were not included in our model. Age, %TBSA burned, and inhalation injury have been the most consistent factors previously published and were additionally shown to be statistically significant in our analysis. We have added a fourth factor, %FTB, although this variable did not change the performance of the model greatly. It is unclear whether the effect of %FTB on the model would increase if data were more complete. Outcomes may be further affected by patient comorbidities, delays in admission to burn centers and/or availability of trained, dedicated multidisciplinary burn teams, intoxicants, and other diagnoses. However, our final model was shown to be a very good performer with a good capacity to discriminate between survivors and nonsurvivors. This reduces the likelihood that unadjusted covariates would meaningfully change the results.
What is completely clear, however, is that the quality of data regarding burns is inadequate, and that better reporting and funding will be required to maintain a registry that is capable of supporting high quality, observational burn research. This finding may, in fact, be the most important aspect of our study. Without such quality data, significant national improvements in burn care and outcomes are unlikely.
Conclusion
Our model, using data from a unique and large data set, was able to identify admitting facility as one of the critical factors predicting mortality in burn patients. However, rather than exposing and penalizing under-performing hospitals, these data should be used to encourage the identification of methods through which superiorly performing hospitals produce improved burn outcomes. If applied broadly, the application of these techniques could increase the quality of burn care, reduce patient mortality, and more appropriately allocate healthcare resources.
Acknowledgments
P.I. Robert G. Sawyer was granted a teaching grant from the National Institutes of Health: NIH 5T32AI078875-02.
Footnotes
Presented at the 2009 Annual Meeting of the American Association for the Surgery of Trauma, October 1–3, 2009, Pittsburgh, PA.
References
- 1.American Burn Association. [Accessed September 1, 2011];Burn incidence fact sheet. Available at: www.ameriburn.org.
- 2.McGwin G, Jr, Cross JM, Ford JW, et al. Long-term trends in mortality according to age among adult burn patients. J Burn Care Rehabil. 2003;24:21–5. doi: 10.1097/00004630-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Brusselaers N, Hoste EAJ, Monstrey S, et al. Outcome and changes over time in survival following severe burns from 1985 to 2004. Intensive Care Med. 2005;12:1648–53. doi: 10.1007/s00134-005-2819-6. [DOI] [PubMed] [Google Scholar]
- 4.Townsend CM, Beauchamp RD, Evers BM, Mattox MD. Sabiston Textbook of Surgery. 18. Elsevier; 2009. [Google Scholar]
- 5.McGwin GJ, George RL, Cross JM, Rue LW. Improving the ability to predict mortality among burn patients. Burns. 2008;34:320–7. doi: 10.1016/j.burns.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Macedo JLS, Santos JB. Predictive factors of mortality in burn patients. Rev Inst Med Trop Sao Paulo. 2007;49:365–70. doi: 10.1590/s0036-46652007000600006. [DOI] [PubMed] [Google Scholar]
- 7.Khuri S. The NSQIP: a new frontier in surgery. Surgery. 2005;138:837–43. doi: 10.1016/j.surg.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Grol R. Improving the quality of medical care: building bridges among professional pride, payer profit and patient satisfaction. JAMA. 2001;286:2578–85. doi: 10.1001/jama.286.20.2578. [DOI] [PubMed] [Google Scholar]
- 9.Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228:491–507. doi: 10.1097/00000658-199810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]