Abstract
OBJECTIVE
We measured the relative impact of influenza and respiratory syncytial virus (RSV) infections in young children in terms of emergency department (ED) visits, clinical care requirements, and overall resource use.
METHODS
Patients who were aged ≤7 years and treated in the ED of a tertiary care pediatric hospital for an acute respiratory infection were enrolled during 2 winter seasons between 2003 and 2005. We quantified health care resource use for children with influenza or RSV infections, and extrapolated results to estimate the national resource use associated with influenza and RSV infections.
RESULTS
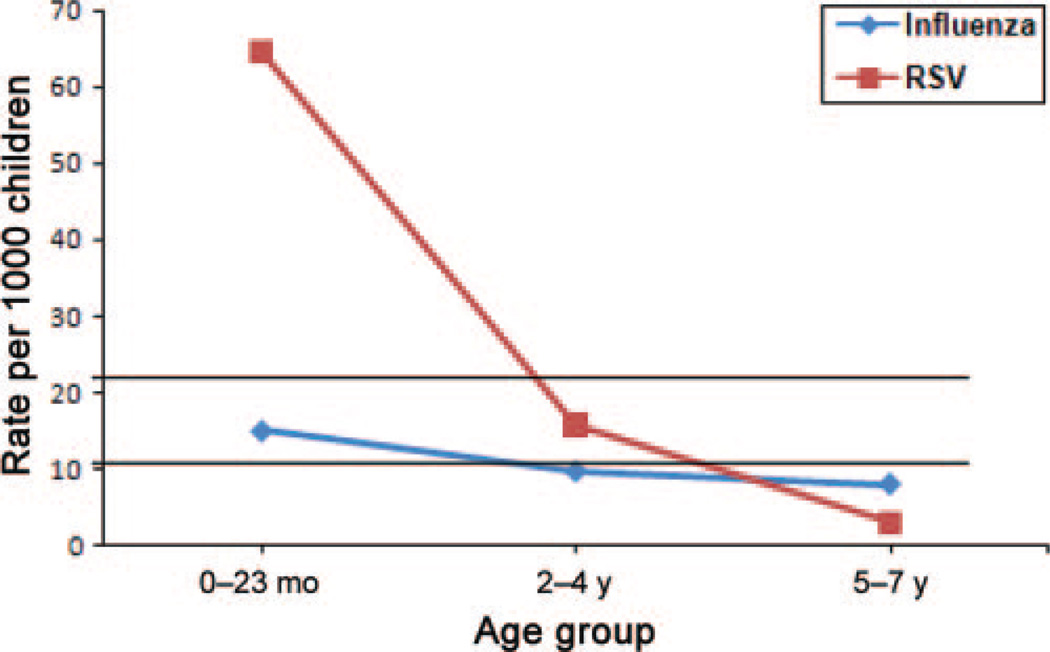
Nationally, an estimated 10.2 ED visits per 1000 children were attributable to influenza and 21.5 visits per 1000 to RSV. Children who were aged 0 to 23 months and infected with RSV had the highest rate of ED visits with 64.4 visits per 1000 children. Significantly more children required hospitalization as a result of an RSV infection compared with influenza, with national hospitalization rates of 8.5 and 1.4 per 1000 children, respectively. The total number of workdays missed yearly by caregivers of children who required ED care was 246 965 days for influenza infections and 716 404 days for RSV infections.
CONCLUSION
For young children, RSV is associated with higher rates of ED visits, hospitalization, and caregiver resource use than is influenza. Our results provide data on the large number of children who receive outpatient care for influenza and RSV illnesses and serve to inform analyses of prevention programs and treatments for both influenza and RSV disease.
Keywords: burden of illness, influenza, respiratory syncytial virus, emergency health services
Each year, influenza and respiratory syncytial virus (RSV) result in substantial morbidity among young children, with >40% of preschool-aged children experiencing an influenza illness and nearly 100% of children infected with RSV by 3 years of age.1–4 Illnesses range from self-limited upper respiratory infections to life-threatening respiratory compromise and result in a high volume of yearly hospitalizations, outpatient visits, and antibiotic use.5–10 These viruses exert considerable economic impact through medical expenses for affected children, missed workdays by parents, and the increased overall burden of disease across age groups, because children are the chief vectors of influenza transmission to the adult population.11–16
Effective strategies to reduce the burden of childhood respiratory illnesses require a better understanding of the relative impact of viral agents and the resources used for treating sick children. The disease burden associated with influenza and RSV has been estimated primarily through extrapolation from hospitalization rates6–8,17–19; however, a substantial portion of the resource use that is attributable to these viruses is in the outpatient setting.10,20–22 Emergency department (ED) visits for influenza may be up to 30 times more common than hospitalizations,21 making the ED a prime setting for measuring the societal burden of these viruses.
We hypothesized that RSV illness among young children results in greater health care and societal burden compared with influenza illness. Through the lens of ED use, we measured the relative impact of influenza and RSV infections in young children in terms of ED visits, clinical care requirements, and overall resource use.
METHODS
Study Design and Population
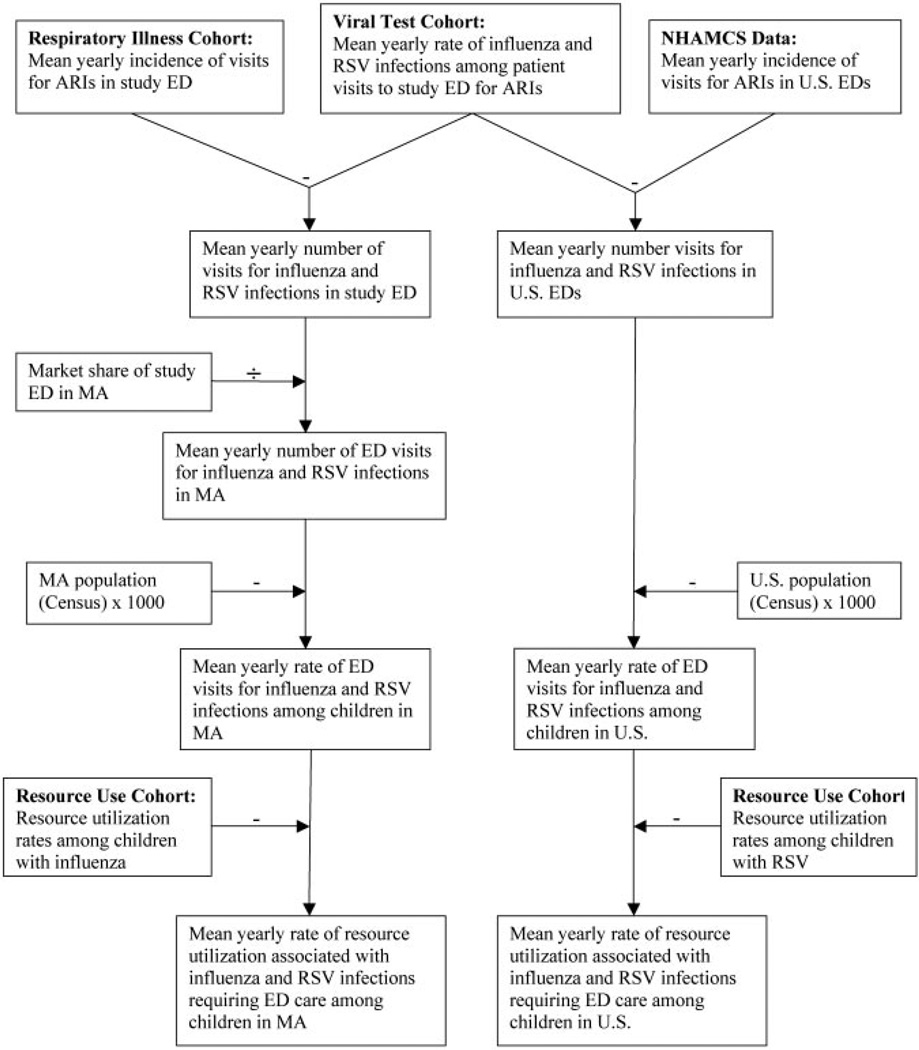
Data from 3 patient cohorts were used to estimate population-based rates of resource use associated with influenza and RSV infections among children who presented to EDs in Massachusetts and the United States (Fig 1). The resource-use cohort was used to quantify resource use for children with influenza and RSV infections. The cohort was collected as a convenience sample of patients who were prospectively enrolled in the ED of a tertiary care pediatric hospital in Massachusetts during 2 influenza and RSV seasons—December 2003 to April 2004 and November 2004 to May 2005—on the basis of local peak activity of these winter respiratory viruses.23,24 Eligible patients were identified by research assistants and included children who were ≤7 years of age and presented to the ED with an acute respiratory infection (ARI), defined as the presence of 2 or more of the following symptoms: fever, cough, sore throat, sneezing, congestion, or rhinorrhea. Patients who had neutropenia were excluded.25,26 Viral testing was performed on all patients in this cohort to identify patients who had ARIs that resulted from influenza and RSV. The Children’s Hospital Boston institutional review board approved the study.
FIGURE 1.
Use of data sources in estimating state- and national-level rates of resource use for influenza and RSV infections that required ED care among children ≤8 years of age. NHAMCS indicates National Hospital and Ambulatory Medical Care Survey; MA, Massachusetts.
Research assistants administered standardized interviews to parents of participants at the time of enrollment and again by telephone 7 to 10 days after the ED visit. Information was collected on the participant’s illness, including previous health care visits, home medication administration, days of missed school, and parental lost workdays resulting from the child’s illness. Specific medications were identified, including over-the-counter agents (eg, antipyretics, cold remedies) and antibiotics. Medical records for the ED visit and, when applicable, the hospitalization were reviewed by a physician. Data were extracted on medication, oxygen, and intravenous fluid administration; radiologic and laboratory testing; and discharge prescriptions, by using a standardized form.
The respiratory illness cohort was a retrospective cohort from the same pediatric hospital used to estimate the mean yearly incidence of ED visits for ARIs. This cohort included all visits by patients who were aged ≤7 years and presented to the ED with an ARI between December and April during a 5-year period from 2001 to 2006. These winter months represent the period with the greatest number of visits for viral ARIs.7,17 Overall, 98% of laboratory-confirmed influenza specimens and 91% of RSV specimens were obtained during this period. ARIs were identified by using patient chief complaints, which are routinely recorded for all patient visits to the ED.27 Data from this cohort were combined with data on the study ED’s market share (ie, the proportion of visits to the study ED among all EDs in the state) to determine population-based rates of ED visits for ARIs.28
The viral test cohort was also retrospective and included all visits by patients who were aged ≤7 years and were evaluated in the ED with laboratory-confirmed influenza or RSV between December and April from 2001 through 2006. The laboratory tests were ordered by clinicians during routine clinical care. This cohort was used to calculate the mean yearly risks for influenza and RSV infections among patients with ARIs. The risks for influenza and RSV infections were based on the average of the yearly risks and weighted by the age distribution of children who presented to the study ED to correct for differences in the age distribution between children who were tested for influenza and RSV and children who presented to the ED. We previously demonstrated that these mean risks for viral infection are representative of the infection rates among children with known ARIs.29 Five years of retrospective viral test results were used to obtain robust mean risks for influenza and RSV infections given the yearly fluctuation in viral activity.
Nasopharyngeal aspirates were obtained from patients in the resourceuse cohort and tested for the presence of influenza virus A and B, RSV, parainfluenza virus types 1 through 3, adenovirus, enterovirus, and human metapneumovirus (during 2004 –2005 season only). All specimens were tested for influenza virus with culture and reverse transcriptase–polymerase chain reaction (RT-PCR) and for RSV by direct immunofluorescent antibody stain (DFA) and RT-PCR.30,31 A specimen was defined as influenza- or RSV-positive when either test was positive.7,21 We tested for parainfluenza and adenovirus by culture only, for enterovirus by using culture and RT-PCR, and for rhinovirus and human metapneumovirus by using RT-PCR only. Children with viral co-infections were not included in the measurements of resource use to obtain accurate estimates of the use attributable to influenza and RSV specifically. Tests on patients in the viral test cohort included DFAs and viral culture for influenza A and B, RSV, parainfluenza virus types 1 through 3, adenovirus, and enterovirus. A specimen that tested positive for influenza A or B or for RSV by either DFA or culture was considered influenza- or RSV-positive, respectively.
Influenza- and RSV-Associated Resource-Use Rates
Resources were grouped into clinical care requirements associated with the enrollment ED visit, resource use that occurred before and after the ED visit, and antibiotic use during the illness. The proportion of children who used each resource for influenza and RSV infections, as measured in the resource-use cohort, was multiplied by the rate of ED visits for influenza and RSV in Massachusetts and the United States.
Age-Specific Influenza- and RSV-Associated Resource-Use Rates
National rates of ED visits specific to age groups (0–23 months, 2–4 years, and 5–7 years) were calculated following the same procedure as for the study population as a whole but using age-specific ARI incidences, proportions of influenza and RSV infections, and census data. The age-specific number of primary care visits and workdays lost by caregivers resulting from an ED-treated ARI were determined by multiplying the mean total number of primary care visits and workdays missed by a caregiver per child by the mean yearly rate of ED visits for influenza and RSV infections per 1000 children in the United States.
Statistical Analysis
We compared demographic and clinical characteristics of patients by using Pearson χ2 and Fisher’s exact tests, as appropriate. Details of the estimation of the yearly incidence of ARIs have been previously described.21 All other rates and variances were estimated by using the δ method and conditional probability rules.32 To estimate the mean total number of primary care visits and workdays missed by a caregiver per child, we used overdispersed Poisson models.
All confidence intervals (CIs) were at the 95% level, and all test statistics were 2-sided with P values considered statistically significant at a .05 α level. Analyses were performed by using SAS 9.1 (Cary, NC) and S-plus 8.0 (Insightful, Seattle, WA).
RESULTS
Study Population
Among the resource-use cohort, 895 patients who presented to the ED with ARIs during the 2 consecutive influenza and RSV seasons were approached and eligible for participation. Of these, 708 (79%) were enrolled in the study. Among the 187 not enrolled, 42 were non–English-speaking and an interpreter was not available, and 145 refused to participate. A total of 67 (9.5%) enrolled patients were infected with influenza, 164 (23.2%) with RSV, and 144 (19%) with other viruses included in the testing protocol. Eight children with influenza infections had evidence of a viral co-infection (3 with RSV, 2 with parainfluenza virus, and 3 with rhinovirus), and 13 children with RSV infections were infected with a second virus (3 with influenza, 2 with parainfluenza virus, and 8 with rhinovirus).
Demographic and Clinical Characteristics
Patients who were infected with influenza and RSV were similar in terms of gender and race/ethnicity distribution, but age distributions differed (Table 1). There were also differences in terms of the living environment, medical history, clinical presentation, and diagnoses given to patients with influenza and RSV infections.
TABLE 1.
Demographic and Clinical Characteristics of Children Who Presented to the ED With Influenza and RSV Infections
| Characteristic | Influenza (N = 59), %a |
RSV (N = 151), %a |
Pb |
|---|---|---|---|
| Age | <.001 | ||
| 0–5 mo | 15 | 37 | |
| 6–23 mo | 12 | 22 | |
| 2–4 y | 46 | 36 | |
| 5–7 y | 27 | 5 | |
| Female gender | 49 | 44 | .530 |
| Race/ethnicity | .290 | ||
| Non-Hispanic white | 32 | 44 | |
| Non-Hispanic black | 20 | 17 | |
| Hispanic | 34 | 31 | |
| Other | 14 | 7 | |
| Living environment | |||
| Smoke exposure | 15 | 26 | .100 |
| Child care attendance | 31 | 31 | .930 |
| ≥2 siblings | 14 | 29 | .020 |
| >2 family members per bedroom | 0 | 7 | .060 |
| Medical history | |||
| Asthmac | 36 | 38 | .770 |
| Other chronic illness | 0 | 8 | .020 |
| Prematurityd | 12 | 19 | .200 |
| Influenza immunized | 27 | 31 | .570 |
| Clinical presentation | |||
| Fevere | 90 | 67 | <.010 |
| Cough | 93 | 99 | .010 |
| Rhinorrhea | 88 | 81 | .200 |
| Sore throat | 24 | 10 | <.010 |
| Hypoxiaf | 14 | 38 | <.010 |
| Wheeze on auscultation | 10 | 42 | <.010 |
| Crackles or rhonchi on auscultation | 15 | 48 | <.010 |
| ED diagnosisg | |||
| Otitis media | 10 | 11 | .820 |
| Pneumonia | 5 | 13 | .090 |
| Bronchiolitis | 14 | 44 | <.010 |
| Asthma | 5 | 16 | .040 |
| Influenza | 5 | 0 | .020 |
| Febrile illness | 25 | 5 | <.010 |
| Viral illness | 25 | 20 | .380 |
Eight patients with influenza co-infections and 13 patients with RSV co-infections were excluded.
P values were estimated by using Pearson’s χ2 except for the variables “>2 family members per bedroom,” “other chronic illness,” and “Influenza,” for which Fisher’s exact test was used.
History of asthma or wheezing.
Defined as <37 weeks’ estimated gestational age.
Defined as measured temperature at home or in ED of >37.9°C.
Defined as oxygen saturation in ED of <97%.
Includes primary and secondary diagnoses.
Local and Population-Based Influenza and RSV ED Visit Rates
The mean yearly number of visits for ARIs to the study ED was 5288 (95% CI: 4770–5806), with 11.2% (95% CI: 0.6–21.8) infected with influenza and 23.6% (95% CI: 13.8 –33.5%) infected with RSV. The ED visit rate for ARIs per 1000 children in Massachusetts was 76.6 (95% CI: 69.2–84.8) and nationally was 91.2 per 1000 children.
A total of 8.6 (95% CI: 3.3–22.4) per 1000 children in Massachusetts required an ED visit for an influenza infection and 18.1 (95% CI: 11.7–28.0) per 1000 required a visit for an RSV infection. At the national level, there were an estimated 10.2 visits (95% CI: 4.0–26.4) per 1000 children related to influenza and 21.5 visits (95% CI: 14.2–32.7) per 1000 to RSV.
Influenza- and RSV-Associated Resource-Use Rates
There were differences in the clinical care requirements for children who were infected with influenza and RSV (Table 2). Compared with children who were infected with influenza, children with RSV were significantly more likely to have medications administered (74% [95% CI: 68%–81%] vs 49% [95% CI: 38%–64%], respectively; P < .001 for Pearson χ2) with the difference primarily attributable to greater rates of over-the-counter medication administration at home. Children with RSV were also more likely to have a radiologic study (69% [95% CI: 62%–77%] vs 44% [95% CI: 33%–59%], respectively; P < .001 for Pearson χ2) in the ED and were more likely to be admitted to the hospital (40% [95% CI: 33%–48%] vs 14% [95% CI: 7%–26%], respectively; P = .02 for Pearson χ2; Table 2). National estimates for the rate of hospitalization for RSV infection were significantly higher than for influenza.
TABLE 2.
Clinical Care Requirements by Children ≤7 Years of Age With Influenza and RSV Infections
| Treatment Administered or Intervention Performed |
Influenza (N = 59) | RSV (N = 151) | ||||
|---|---|---|---|---|---|---|
| Proportion (95% CI) Among Prospective Patients |
Yearly Rate (95% CI) in Massachusetts Population/1000 Children |
Yearly Rate (95% CI) in US Population/ 1000 Children |
Proportion (95% CI) Among Prospective Patients |
Yearly Rate (95% CI) in Massachusetts Population/1000 Children |
Yearly Rate (95% CI) in US Population/ 1000 Children |
|
| Medication | 49 (38–64) | 4.2 (1.5–11.6) | 5.0 (1.9–13.5) | 74 (68–81) | 13.4 (8.6–21.0) | 16.0 (10.4–24.5) |
| Supplemental oxygen | 2 (0–12) | 0.1 (0.0–1.8) | 0.2 (0.0–1.8) | 14 (9–21) | 2.5 (1.3–4.7) | 3.0 (1.7–5.4) |
| Intravenous fluids | 31 (21–45) | 2.6 (0.9–7.6) | 3.1 (1.1–8.8) | 28 (22–37) | 5.2 (3.1–8.7) | 6.1 (3.7–10.0) |
| Radiologic study | 44 (33–59) | 3.8 (1.4–10.5) | 4.5 (1.7–12.2) | 69 (62–77) | 12.5 (7.9–19.6) | 14.8 (9.6–22.8) |
| Laboratory blood test | 32 (22–47) | 2.8 (1.0–8.0) | 3.3 (1.2–9.2) | 32 (26–41) | 5.9 (3.5–9.8) | 7.0 (4.3–11.3) |
| Urinalysis | 20 (12–34) | 1.7 (0.6–5.4) | 2.1 (0.7–6.3) | 13 (9–20) | 2.4 (1.3–4.5) | 2.8 (1.6–5.1) |
| Lumbar puncture | 10 (5–22) | 0.9 (0.2–3.3) | 1.0 (0.3–3.7) | 3 (1–8) | 0.6 (0.2–1.7) | 0.7 (0.3–1.9) |
| Hospital admission | 14 (7–26) | 1.2 (0.4–4.0) | 1.4 (0.4–4.5) | 40 (33–48) | 7.2 (4.4–11.7) | 8.5 (5.4–13.6) |
| Medication prescription | 19 (11–32) | 1.6 (0.5–5.1) | 1.9 (0.6–5.8) | 20 (14–27) | 3.6 (2.0–6.3) | 4.3 (2.5–7.3) |
Measures of overall resource use were high both for children with influenza and RSV infections (Table 3). Approximately 90% of children required some type of additional health care encounter. Almost two thirds of caregivers missed at least 1 day of work as a result of the child’s illness. The estimated total number of workdays missed per year on a national basis by caregivers of children with influenza and RSV infections was 246 965 days and 716 404 days, respectively. Antibiotics were frequently administered to children with influenza and RSV infections, with 45% of children with influenza and 53% of children with RSV receiving antibiotics at some point during the course of their illness (Table 4).
TABLE 3.
Resource Use by Children ≤7 Years of Age Treated in an ED for Influenza and RSV Infections
| Type of Resource | Influenza (N = 58)a | RSV (N = 150)a | ||||
|---|---|---|---|---|---|---|
| Proportion (95% CI) Among Prospective Patients |
Yearly Rate (95% CI) in Massachusetts Population/1000 Children |
Yearly Rate (95% CI) in US Population/ 1000 Children |
Proportion (95% CI) Among Prospective Patients |
Yearly Rate (95% CI) in Massachusetts Population/1000 Children |
Yearly Rate (95% CI) in US Population/ 1000 Children |
|
| Any additional health care encounterb | 90 (82–98) | 7.7 (2.9–20.2) | 9.2 (3.5–23.8) | 93 (89–97) | 16.9 (10.9–26.2) | 20.1 (13.2–30.6) |
| Visit to primary care clinic | 71 (60–83) | 6.1 (2.3–16.2) | 7.2 (2.7–19.0) | 78 (72–85) | 14.1 (9.0–22.1) | 16.8 (10.9–25.7) |
| Additional visit to ED | 21 (13–34) | 1.8 (0.6–5.5) | 2.1 (0.7–6.4) | 32 (25–40) | 5.8 (3.5–9.6) | 6.9 (4.3–11.1) |
| Medication administered at home | 98 (95–102) | 8.4 (3.2–22.1) | 10.0 (3.9–25.9) | 93 (89–97) | 16.9 (10.9–26.2) | 20.1 (13.2–30.6) |
| Child care, preschool, or school day missed | 48 (37–63) | 4.1 (1.5–11.4) | 4.9 (1.8–13.3) | 37 (30–45) | 6.6 (4.0–10.9) | 7.9 (4.9–12.6) |
| Workday missed by caregiver | 64 (53–77) | 5.5 (2.0–14.7) | 6.5 (2.5–17.2) | 66 (59–74) | 11.9 (7.6–18.8) | 14.2 (9.2–21.9) |
One patient with influenza and 1 with RSV were lost to follow-up.
Includes call to primary care clinic, visit to primary care clinic, additional visit to ED, or hospitalization not associated with enrollment encounter.
TABLE 4.
Antibiotic Use by Children Who Were ≤7 Years of Age and Treated in an ED for Influenza and RSV Infections
| Type of Antibiotic Use | Influenza (n = 58)a | RSV (n = 150)a | ||||
|---|---|---|---|---|---|---|
| Proportion (95% CI) Among Prospective Patients |
Yearly Rate (95% CI) in Massachusetts Population/1000 Children |
Yearly Rate (95% CI) in US Population/ 1000 Children |
Proportion (95% CI) Among Prospective Patients |
Yearly Rate (95% CI) in Massachusetts Population/1000 Children |
Yearly Rate (95% CI) in US Population/ 1000 Children |
|
| Any antibiotic use | 45 (34–60) | 3.8 (1.4–10.7) | 4.6 (1.7–12.4) | 53 (46–62) | 9.6 (6.0–15.3) | 11.4 (7.3–17.8) |
| Antibiotic administered before ED visit | 19 (11–32) | 1.6 (0.5–5.1) | 1.9 (0.6–5.8) | 19 (14–27) | 3.5 (2.0–6.2) | 4.1 (2.4–7.1) |
| Antibiotic administered in ED | 24 (15–37) | 2.0 (0.7–6.2) | 2.4 (0.8–7.1) | 23 (17–31) | 4.2 (2.4–7.2) | 5.0 (3.0–8.3) |
| Antibiotic administered in hospitalb | 38 (15–92) | 0.4 (0.1–2.3) | 0.5 (0.1–2.5) | 45 (34–60) | 3.2 (1.8–5.8) | 3.8 (2.4–6.1) |
| Antibiotic prescribed upon discharge from ED or hospital | 12 (6–24) | 1.0 (0.3–3.6) | 1.2 (0.4–4.1) | 14 (9–21) | 2.5 (1.3–4.7) | 3.0 (1.7–5.4) |
One patient with influenza and 1 with RSV were lost to follow-up.
n = 8 for influenza and 59 for RSV.
Age-Specific Influenza- and RSV-Associated Resource-Use Rates
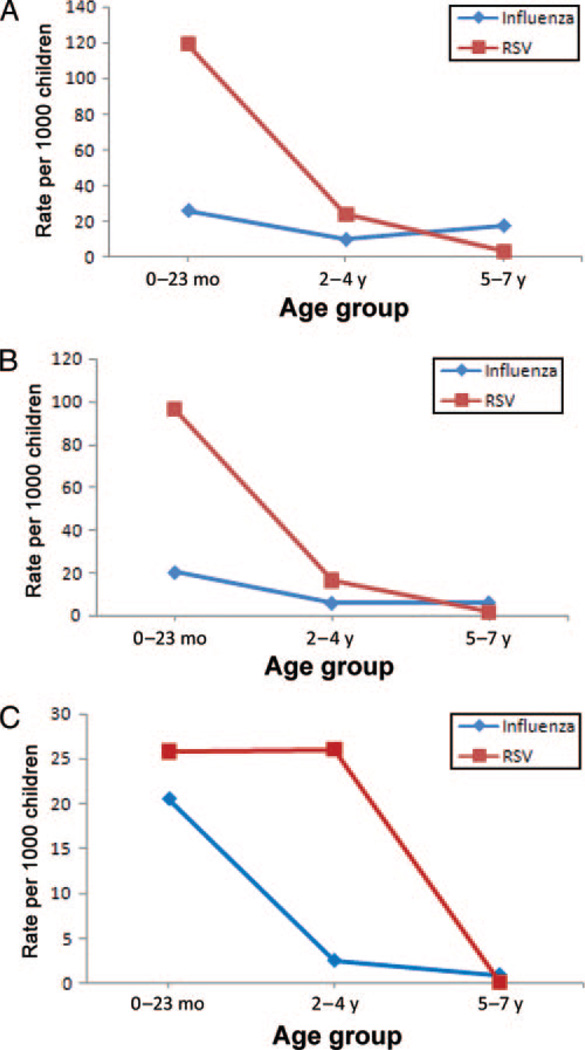
ED visit rates were highest among children who were aged 0 to 4 years, with higher rates attributable to RSV infections compared with influenza. Children who were younger than 2 years and infected with RSV had 64.4 (95% CI: 45.4–91.3) ED visits per 1000 children who were younger than 2 years compared with 15.0 (95% CI: 4.4–50.6) visits per 1000 children among those who were infected with influenza (Fig 2). National rates of workdays missed by a caregiver, visits to primary care physicians, and prescription of an antibiotic to children were highest among children who were aged 0 to 4 years and had an RSV-associated infection and were similar in magnitude among children who were aged 5 to 7 years and had either an RSV or influenza illness (Fig 3).
FIGURE 2.
Age-specific and mean national rates of ED visits for children with influenza and RSV infections. The mean rate of ED visits for influenza was 10.2 per 1000 children; the mean rate of ED visits for RSV was 21.5 per 1000 children.
FIGURE 3.
National yearly rates of resource use for children with influenza and RSV infections. A, Workdays missed by caregiver. B, Visits to primary care clinics. C, Children prescribed an antibiotic.
DISCUSSION
Our findings indicate that RSV causes a substantially greater burden in young children and their families than influenza. ARIs caused by RSV result in more than twice as many ED visits and 6 times as many hospitalizations compared with ARIs related to influenza. RSV infections are also twice as likely to result in additional primary care clinic visits and in antibiotic treatment. The parents of children with RSV miss almost 3 times more workdays than parents of children with influenza, and those with children younger than 2 years are nearly 5 times more likely to miss work when their child has RSV. Because the economic burden of childhood illnesses is largely driven by lost caregiver wages,33–35 prevention and control approaches that address RSV as well as influenza among young children are likely to be most cost-effective.
Detailed guidelines that summarize recommendations for the containment of influenza infection are published every year by the Influenza Division of the Centers for Disease Control and Prevention.36,37 These include well-developed influenza vaccination policies, guidelines for the use of antiviral medications, and control measures for specific settings such as child care facilities and nursing homes. Similar strategies are not available for the containment of RSV. Despite many years of vaccine research, prevention measures for RSV remain limited to immunoprophylaxis of children at high risk.38,39 A better understanding of the contribution of RSV to the yearly burden of winter respiratory infections will serve to inform the development of prevention initiatives and to identify at-risk populations and cost-effective policies.
Although we provide new data on resource use in the clinical and outpatient settings, the rates of viral infection are consistent with previous studies, lending external validation to our methods. Similar to our laboratory-confirmed positivity rates of 11.2% for influenza and 23.6% for RSV infections among children who were aged ≤7 years and had ARIs, published estimates of viral prevalence among children range from 6% to 16% for influenza21,40–43 and 20% to 48% for RSV40–42 during seasons and among patient populations that are different from the ones studied here. Poehling et al21 reported ED visit rates for influenza of 6 and 27 per 1000 children aged 0 to 4 years during 2 influenza seasons, comparable to the rate in this study of 10.2 per 1000 children. In a recent study by Hall et al,25 ED visit rates for RSV illnesses were found to range from 22 to 32 for children aged 0 to 4 years, similar to the rate of 21.5 per 1000 children reported in this study. Hospitalization rates reported in the literature are also similar to ours, ranging from 0.6 to 1.8 per 1000 children5,7,8,17,18,20,42,43 for influenza infections and 3.0 to 5.8 per 1000 children for RSV illnesses6–8,18,25,42,44 among children in similar age groups.
Additional support for the accuracy of our findings is the similarity in the rates that we report for the state and national populations. We calculated estimates for the Massachusetts population by using public health data, which include counts of all visits to Massachusetts EDs.28 To obtain national estimates, we used a survey conducted by the National Center for Health Statistics, which collects information on national samples of visits to US EDs and allows computation of national estimates on the basis of proportional weights assigned to surveyed visits.45 These 2 approaches yielded very similar results with slightly higher estimates for the national rates but none appreciably different from the state-level figures.
The methods used in this study—using cohort data in combination with public health and national survey data—may serve as a model for estimating the disease burden of other infectious and noninfectious illnesses. A similar approach has been used in studies published by the New Vaccine Surveillance Network, which conducts population-based surveillance of ARIs among children who are younger than 5 years.21,25 In those studies, surveillance is conducted in 3 counties in the United States, and population estimates of virus-specific infections are obtained by using local market share rates, US Census figures, and National Hospital and Ambulatory Medical Care Survey data.
Our study has several limitations. In the resource-use cohort, our enrollment rate was high, but it is possible that a nonparticipation bias affected our resource-use rates. It is also possible that there were inaccuracies in the information provided by parents, which we were not able to verify; however, it is unlikely that there was a systematic bias toward either RSV or influenza infection. Our results are based on a patient population from a single institution, possibly limiting the generalizability of our findings. We assumed that results of virologic testing from our sample were applicable to all patients who were treated in the ED with ARIs. This assumption is supported by comparable rates found in our prospective cohort and from published reports.21,40–43 To extrapolate to the state-level population, we assumed that the other state EDs had similar rates of visits for ARIs as well as influenza and RSV infections. For national estimates, we assumed that the rate of influenza and RSV infections was the same among ARI visits as in our study population. The use of National Hospital and Ambulatory Medical Care Survey data and this method, however, is consistent with the approach used in a previous study that examined national rates of ED visits for influenza.21 Finally, we may have underestimated the total burden of influenza and RSV by excluding visits with viral co-infections, although there were similar rates of co-infections among patients with influenza and RSV. None of these limitations should impede our main objective to make relative comparisons between influenza- and RSV-associated health care use. In fact, the total burden of RSV may have been underestimated in this study, because the RSV season may begin as early as November and we chose to include only December through April in our definition of the winter season; however, a recent article reported the medical onset of yearly RSV outbreaks as December 1.25
CONCLUSIONS
RSV has a substantially greater impact on young children than influenza, and because young children drive transmission of viral infections to older age groups,11,12 they likely contribute to a large burden across the age spectrum. Infection control measures should take into account the relative impact of these viruses and provide strategies for RSV as well as influenza prevention. Our results highlight the impact of these viruses on the health care system and on caregivers and provide data necessary for cost/benefit analyses of prevention programs and treatments for influenza and RSV infection.
WHAT’S KNOWN ON THIS SUBJECT
Winter respiratory viruses lead to substantial morbidity in young children. A better understanding of the relative impact of these viruses is required to inform the development of treatment and control measures.
WHAT THIS STUDY ADDS
Among young children, RSV results in a greater burden of illness than does influenza, with higher rates of ED visits and hospitalizations and greater caregiver resource utilization.
ACKNOWLEDGMENTS
This work was supported by R01LM007970 from the National Library of Medicine, 5 T32 HD40128 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, 5225 3 338CHI from the Massachusetts Department of Public Health, MO1 RR-02172 from the General Clinical Research Center at Children’s Hospital Boston, and 290-00-0020 from the Agency for Healthcare Research and Quality.
We thank Jenny Wei, MD, Kelly Slack, MD, Jennifer Woo, MD, Hector Rivera, MD, and Sara Ivey, MPH, for assistance in data collection and processing; James West, PhD, for compilation of the registry data from the Massachusetts Division of Healthcare Finance and Policy; David Wypij, PhD, for suggestions on data analysis; Don Goldman, MD, for guidance and expertise in infectious diseases; and Karen Olson, PhD, for developing and managing the data sets.
ABBREVIATIONS
- RSV
respiratory syncytial virus
- ED
emergency department
- ARI
acute respiratory infection
- RT-PCR
reverse transcriptase–polymerase chain reaction
- DFA
direct immunofluorescent antibody stain
- CI
confidence interval
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Monto AS, Sullivan KM. Acute respiratory illness in the community: frequency of illness and the agents involved. Epidemiol Infect. 1993;110(1):145–160. doi: 10.1017/s0950268800050779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simoes EA. Respiratory syncytial virus infection. Lancet. 1999;354(9181):847–852. doi: 10.1016/S0140-6736(99)80040-3. [DOI] [PubMed] [Google Scholar]
- 3.Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980–1996. JAMA. 1999;282(15):1440–1446. doi: 10.1001/jama.282.15.1440. [DOI] [PubMed] [Google Scholar]
- 4.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 5.Neuzil KM, Mellen BG, Wright PF, Mitchel EF, Jr, Griffin MR. The effect of influenza on hospitalizations, outpatient visits, and courses of antibiotics in children. N Engl J Med. 2000;342(4):225–231. doi: 10.1056/NEJM200001273420401. [DOI] [PubMed] [Google Scholar]
- 6.Schanzer DL, Langley JM, Tam TW. Hospitalization attributable to influenza and other viral respiratory illnesses in Canadian children. Pediatr Infect Dis J. 2006;25(9):795–800. doi: 10.1097/01.inf.0000232632.86800.8c. [DOI] [PubMed] [Google Scholar]
- 7.Iwane MK, Edwards KM, Szilagyi PG, et al. Population-based surveillance for hospitalizations associated with respiratory syncytial virus, influenza virus, and parainfluenza viruses among young children. Pediatrics. 2004;113(6):1758–1764. doi: 10.1542/peds.113.6.1758. [DOI] [PubMed] [Google Scholar]
- 8.Nicholson KG, McNally T, Silverman M, Simons P, Stockton JD, Zambon MC. Rates of hospitalisation for influenza, respiratory syncytial virus and human metapneumovirus among infants and young children. Vaccine. 2006;24(1):102–108. doi: 10.1016/j.vaccine.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Gaur AH, Hare ME, Shorr RI. Provider and practice characteristics associated with antibiotic use in children with presumed viral respiratory tract infections. Pediatrics. 2005;115(3):635–641. doi: 10.1542/peds.2004-0670. [DOI] [PubMed] [Google Scholar]
- 10.Menec VH, Black C, MacWilliam L, Aoki FY. The impact of influenza-associated respiratory illnesses on hospitalizations, physician visits, emergency room visits, and mortality. Can J Public Health. 2003;94(1):59–63. doi: 10.1007/BF03405054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monto AS, Davenport FM, Napier JA, Francis T., Jr Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J Infect Dis. 1970;122(1):16–25. doi: 10.1093/infdis/122.1-2.16. [DOI] [PubMed] [Google Scholar]
- 12.Longini IM, Jr, Koopman JS, Monto AS, Fox JP. Estimating household and community transmission parameters for influenza. Am J Epidemiol. 1982;115(5):736–751. doi: 10.1093/oxfordjournals.aje.a113356. [DOI] [PubMed] [Google Scholar]
- 13.Munoz FM. The impact of influenza in children. Semin Pediatr Infect Dis. 2002;13(2):72–78. doi: 10.1053/spid.2002.122992. [DOI] [PubMed] [Google Scholar]
- 14.Fox JP, Cooney MK, Hall CE, Foy HM. Influenzavirus infections in Seattle families, 1975–1979: II. Pattern of infection in invaded households and relation of age and prior antibody to occurrence of infection and related illness. Am J Epidemiol. 1982;116(2):228–242. doi: 10.1093/oxfordjournals.aje.a113408. [DOI] [PubMed] [Google Scholar]
- 15.Glezen WP, Couch RB. Interpandemic influenza in the Houston area, 1974–76. N Engl J Med. 1978;298(11):587–592. doi: 10.1056/NEJM197803162981103. [DOI] [PubMed] [Google Scholar]
- 16.Brownstein JS, Kleinman KP, Mandl KD. Identifying pediatric age groups for influenza vaccination using a real-time regional surveillance system. Am J Epidemiol. 2005;162(7):686–693. doi: 10.1093/aje/kwi257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Izurieta HS, Thompson WW, Kramarz P, et al. Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med. 2000;342(4):232–239. doi: 10.1056/NEJM200001273420402. [DOI] [PubMed] [Google Scholar]
- 18.Weigl JA, Puppe W, Schmitt HJ. The incidence of influenza-associated hospitalizations in children in Germany. Epidemiol Infect. 2002;129(3):525–533. doi: 10.1017/s0950268802007707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mangtani P, Hajat S, Kovats S, Wilkinson P, Armstrong B. The association of respiratory syncytial virus infection and influenza with emergency admissions for respiratory disease in London: an analysis of routine surveillance data. Clin Infect Dis. 2006;42(5):640–646. doi: 10.1086/499810. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien MA, Uyeki TM, Shay DK, et al. Incidence of outpatient visits and hospitalizations related to influenza in infants and young children. Pediatrics. 2004;113(3 pt 1):585–593. doi: 10.1542/peds.113.3.585. [DOI] [PubMed] [Google Scholar]
- 21.Poehling KA, Edwards KM, Weinberg GA, et al. The underrecognized burden of influenza in young children. N Engl J Med. 2006;355(1):31–40. doi: 10.1056/NEJMoa054869. [DOI] [PubMed] [Google Scholar]
- 22.Bourgeois FT, Valim C, Wei JC, McAdam AJ, Mandl KD. Influenza and other respiratory virus–related emergency department visits among young children. Pediatrics. 2006;118(1) doi: 10.1542/peds.2005-2248. Available at: www.pediatrics.org/cgi/content/full/118/1/e1. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. The National Respiratory and Enteric Virus Surveillance System (NREVSS) [Accessed October 20, 2009]; Available at: www.cdc.gov/surveillance/nrevss/rsv/default.html.
- 24.Centers for Disease Control and Prevention. Flu activity & surveillance. [Accessed October 20, 2009]; Available at: www.cdc.gov/flu/weekly/fluactivity.htm.
- 25.Hall CB, Weinberg GA, Iwane MK, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360(6):588–598. doi: 10.1056/NEJMoa0804877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miller EK, Griffin MR, Edwards KM, et al. Influenza burden for children with asthma. Pediatrics. 2008;121(1):1–8. doi: 10.1542/peds.2007-1053. [DOI] [PubMed] [Google Scholar]
- 27.Beitel AJ, Olson KL, Reis BY, Mandl KD. Use of emergency department chief complaint and diagnostic codes for identifying respiratory illness in a pediatric population. Pediatr Emerg Care. 2004;20(6):355–360. doi: 10.1097/01.pec.0000133608.96957.b9. [DOI] [PubMed] [Google Scholar]
- 28.Massachusetts Division of Healthcare Finance and Policy. Emergency department data. [Accessed October 20, 2009]; Available at: www.mass.gov/?pageID=eohhs2terminal&L=5&L0=Home&L1=Researcher&L2=Physical+Health+and+Treatment&L3=Health+Care+Delivery+System&L4=DHCFP+Data+Resources&sid=Eeohhs2&b=terminalcontent&f=dhcfp_researcher_clinical_database&csid=Eeohhs2.
- 29.Bourgeois FT, Olson KL, Brownstein JS, Mc-Adam AJ, Mandl KD. Validation of syndromic surveillance for respiratory infections. Ann Emerg Med. 2006;47(3):265.e1. doi: 10.1016/j.annemergmed.2005.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright KE, Wilson GA, Novosad D, Dimock C, Tan D, Weber JM. Typing and subtyping of influenza viruses in clinical samples by PCR. J Clin Microbiol. 1995;33(5):1180–1184. doi: 10.1128/jcm.33.5.1180-1184.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mazzulli T, Peret TC, McGeer A, et al. Molecular characterization of a nosocomial outbreak of human respiratory syncytial virus on an adult leukemia/lymphoma ward. J Infect Dis. 1999;180(5):1686–1689. doi: 10.1086/315085. [DOI] [PubMed] [Google Scholar]
- 32.Fleiss J, Levin B, Park M. Statistical Methods for Rates and Proportions. 3rd ed. New York, NY: Wiley; 2003. [Google Scholar]
- 33.Meltzer MI, Neuzil KM, Griffin MR, Fukuda K. An economic analysis of annual influenza vaccination of children. Vaccine. 2005;23(8):1004–1014. doi: 10.1016/j.vaccine.2004.07.040. [DOI] [PubMed] [Google Scholar]
- 34.Hardy AM, Lairson DR, Morrow AL. Costs associated with gastrointestinal-tract illness among children attending day-care centers in Houston, Texas. Pediatrics. 1994;94(6 pt 2):1091–1093. [PubMed] [Google Scholar]
- 35.Luce BR, Nichol KL, Belshe RB, et al. Cost-effectiveness of live attenuated influenza vaccine versus inactivated influenza vaccine among children aged 24–59 months in the United States. Vaccine. 2008;26(23):2841–2848. doi: 10.1016/j.vaccine.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. Seasonal influenza (flu) [Accessed October 20, 2009]; Available at: www.cdc.gov/flu.
- 37.Fiore AE, Shay DK, Haber P, et al. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. MMWR Recomm Rep. 2007;56(RR-6):1–54. [PubMed] [Google Scholar]
- 38.Power UF. Respiratory syncytial virus (RSV) vaccines: two steps back for one leap forward. J Clin Virol. 2008;41(1):38–44. doi: 10.1016/j.jcv.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 39.Stevens WW, Falsey AR, Braciale TJ. RSV 2007: recent advances in respiratory syncytial virus research. Viral Immunol. 2008;21(2):133–140. doi: 10.1089/vim.2008.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolf DG, Greenberg D, Kalkstein D, et al. Comparison of human metapneumovirus, respiratory syncytial virus and influenza A virus lower respiratory tract infections in hospitalized young children. Pediatr Infect Dis J. 2006;25(4):320–324. doi: 10.1097/01.inf.0000207395.80657.cf. [DOI] [PubMed] [Google Scholar]
- 41.Jennings LC, Anderson TP, Werno AM, Beynon KA, Murdoch DR. Viral etiology of acute respiratory tract infections in children presenting to hospital: role of polymerase chain reaction and demonstration of multiple infections. Pediatr Infect Dis J. 2004;23(11):1003–1007. doi: 10.1097/01.inf.0000143648.04673.6c. [DOI] [PubMed] [Google Scholar]
- 42.Henrickson KJ, Hoover S, Kehl KS, Hua W. National disease burden of respiratory viruses detected in children by polymerase chain reaction. Pediatr Infect Dis J. 2004;23(1 suppl):S11–S18. doi: 10.1097/01.inf.0000108188.37237.48. [DOI] [PubMed] [Google Scholar]
- 43.Ampofo K, Gesteland PH, Bender J, et al. Epidemiology, complications, and cost of hospitalization in children with laboratory-confirmed influenza infection. Pediatrics. 2006;118(6):2409–2417. doi: 10.1542/peds.2006-1475. [DOI] [PubMed] [Google Scholar]
- 44.Fleming DM, Pannell RS, Elliot AJ, Cross KW. Respiratory illness associated with influenza and respiratory syncytial virus infection. Arch Dis Child. 2005;90(7):741–746. doi: 10.1136/adc.2004.063461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Center for Health Statistics. Ambulatory health care data. [Accessed October 20, 2009]; Available at: www.cdc.gov/nchs/ahcd.htm.