Abstract
It is crucial to characterize self-regulation in children. We compared the temperamental profiles of children with the Child Behavior Checklist (CBCL) Dysregulation Profile (CBCL-DP) to profiles associated with other CBCL-derived syndromes. 382 children (204 boys; aged 5–18) from a large family study were examined. Temperamental profiles were based on the Juvenile Temperament and Character Inventory (JTCI). . Children with the CBCL-DP had a temperamental profile characterized by high Novelty Seeking (NS), high Harm Avoidance (HA), low Reward Dependence (RD) and low Persistence (P). Linear mixed models and regression-based models demonstrated that the CBCL-DP was associated with a “disengaged” temperamental profile. This profile is similar to the profile seen in adult disorders of self-regulation, including cluster B personality disorders. These results support the hypothesis that the CBCL-DP measures poor self-regulation.
Keywords: juvenile bipolar disorder, ADHD, CBCL, temperament, JTCI
Introduction
The boundaries between temperament and psychopathology have been difficult to disentangle and continue to be an active area of research. There is evidence that pure continuum models between a particular trait and a corresponding disorder may be overly simplistic [1,2]. In response, some researchers have begun examining profiles of temperament that encompass multiple dimensions. Using the Juvenile Temperament and Character Inventory JTCI [3], we have previously demonstrated that a small group of children show a particular profile characterized by high Novelty Seeking, high Harm Avoidance, low Persistence, and low Reward Dependence. This “disengaged” profile is furthermore related to impaired competency and adaptive function as compared to a “moderate” group with average levels of all traits and a “steady” profile characterized by low novelty seeking and high persistence [4]. Given that the disengaged profile seemed to index a “push-pull” phenomenon such that children are both attracted to novel situations but tend to be nervous and scared once in those novel situations, we hypothesized that this profile may represent in temperament terms the construct of impaired self-regulation or “Dysregulation”. Indeed, Tillman and colleagues have demonstrated that children with clinical levels of mood regulation problems display higher Novelty Seeking, lower Reward Dependence, and lower Persistence than normal controls, consistent with the disengaged profile. Similar patterns have also been observed for children with ADHD [5].
From a psychopathology perspective, the concept of Dysregulation has been studied in several ways. As work on DSM-5 continues, there has been increased discussion in the literature about children with profound problems with mood dysregulation to the point where a new diagnosis has been suggested to characterize these children [6]. This “top-down” approach has some advantages in that the separation from other DSM-5 diagnoses can be assured. An alternative to using this approach is to use a “bottom-up” approach – to let children be classified into categories of behavior empirically based purely on the symptoms that they report. One such “bottom-up” approach to psychopathological Dysregulation has been to use the Child Behavior Checklist-Dysregulation Profile (CBCL-DP) [7,8,9,10,11,12,13]. This profile, defined as peaks on CBCL scales of attention problems, aggressive behavior, and anxious-depression has been demonstrated to be a useful index of self-regulatory problems in multiple domains [9,14,15,16] and suicidality [7,17]. Children with this profile are at high risk for poor outcomes in adulthood with recent work demonstrating an odds ratio of 11.6 for drug abuse disorders in children with the CBCL-DP from a general population sample who were followed-up 14 years later as adults [18]. While the characteristics of children with this psychopathological profile have been examined from a behavioral genetic [10,11], molecular genetic [12,13,19], phenotypic [20,21], and longitudinal perspective [14,15,18,22], there has been no previous attempt to define this profile in temperamental constructs.
To investigate this issue, the current study examines the temperamental characteristics of children with the CBCL-DP. We hypothesized that children who had the psychopathological profile of the CBCL-DP would be much more likely to have a “disengaged” temperamental profile, suggesting self-regulatory problems. To account for the possibility that this temperament profile simply captures those with a higher psychiatric load in general, we chose to compare children with the CBCL-DP to children with other profiles of psychopathology.
Materials and Methods
Subjects
The participants for this investigation came from a family study conducted in the northeastern United States that was designed to examine the genetic and environmental contributions to attention and aggression. Details of this sample are described in more detail elsewhere [4]. Inclusionary criteria were: (1) proband child between the ages of 6 and 18; (2) proband child living with at least one biological parent; and (3) proband child with at least one sibling between the ages of 6 and 18. If families were able to meet those requirements, they were then sent parent-rater Child Behavior Checklists (CBCLs) to assess levels of behavior problems. Four target groups of probands were sought based on the CBCL. These groups included subjects with (1) T scores greater than 67 on the attention problems (AP) scale and less then 60 on the aggressive behavior (AG) scale; (2) T scores greater than 67 on AG but less than 60 on AP; (3) T scores greater than 67 on both scales; and (4) T scores less than 60 on both scales. Siblings were not subject to any of the T score restrictions placed on probands. The sample was almost exclusively Caucasian with an average score of 6.38 (SD= 2.15) on the Hollingshead SES scale.[23] This included 382 primarily Caucasian (82%) children (46% female) from 193 families. The mean age of the sample was 10.9 (SD=3.1, range = 5–18). All parents provided informed consent and all children provided assent. The data collection was approved by the Institutional Review Board.
Measures
The Junior Temperament and Character Inventory - Parent Version (JTCI) [3]
This instrument is based on the personality structure as described by Cloninger and colleagues and reflects the downward extension of the Temperament and Character Inventory (TCI) [24,25]. The JTCI is a widely used measure and has good psychometric properties [3]. It is comprised of 108 statements that the respondent rates as true or false based on how the person usually acts and feels. For this study, we assessed the four temperament dimensions of the JTCI, namely Novelty Seeking (NS), Harm Avoidance (HA), Reward Dependence (RD), and Persistence (P). NS relates to a tendency to seek out stimulation and is characterized by impulsivity, extravagance and disorderliness. HA refers to inhibitory behavior and contains elements of worry, shyness, and fatigability. RD considers the tendency to maintain behaviors and includes the degree of sentimentality, attachment and dependence. Finally, P reflects the ability of an individual to persevere despite obstacles or frustration. Mother-report of child temperament was used for the current investigation.
Child Behavior Checklist
Problem behavior was measured with the CBCL/6-18, a questionnaire of 118 items developed to measure problem behavior in 6 to 18 year old children (30) or the previous version of the CBCL/4-18 if aged 5 [26]. Mothers were asked to rate the behavior of the child over the preceding 6 months on a 3-point scale. The scores from the CBCL load onto 8 syndrome scales. The CBCL-DP phenotype has previously been defined for children with clinical elevations on three of these scales: attention problems (AP), aggressive behavior (AB), and anxious-depression (AD) [9]. One of the difficulties with previous examination of the CBCL-DP has been that various cutpoints can be applied to the three scales to determine who is or who is not in this group. For example, previous examinations have used a T-score cutpoint of anywhere between 60 and 70 or have used a summed score of the scales. Instead, here, we defined the CBCL-DP group using latent class analysis (LCA, see below), to identify clusters of individuals with statistical elevations on these three scales without imposing an arbitrary cutpoint.
Temperament profile
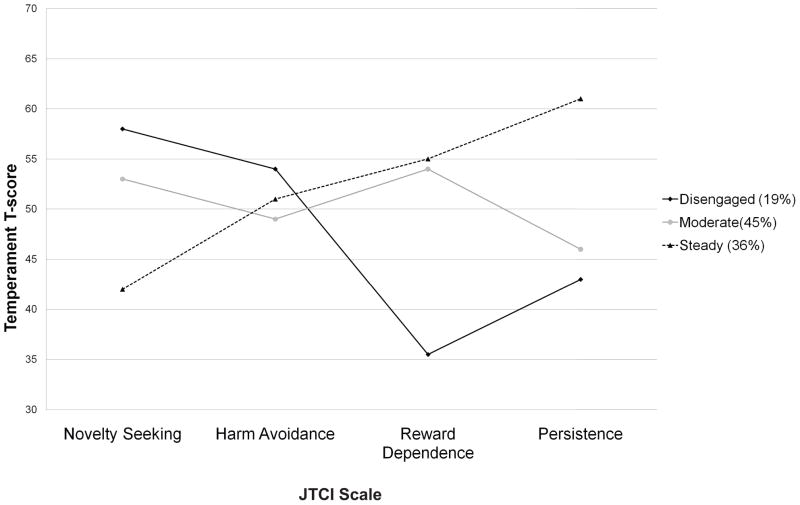
Rettew et al. (2008) (26) defined three latent profiles of child temperament: moderate, steady, and disengaged. Using LCA, each profile was characterized by varying loadings on four parent-rated temperament dimensions of the JTCI: novelty seeking (NS), harm avoidance (HA), reward dependence (RD), and persistence (P). These profiles are illustrated in Figure 1. Two variables representing temperament profiles were used in the current study: (1) probability of membership in the disengaged profile (a continuous variable ranging from 0–1 with a mean of .207, SD=.321); and (2) membership in the disengaged profile (dichotomous variable coded 1=disengaged, 0=member of either moderate or steady profile).
Figure 1.
Temperamental profiles (Based on Rettew et al. [4])
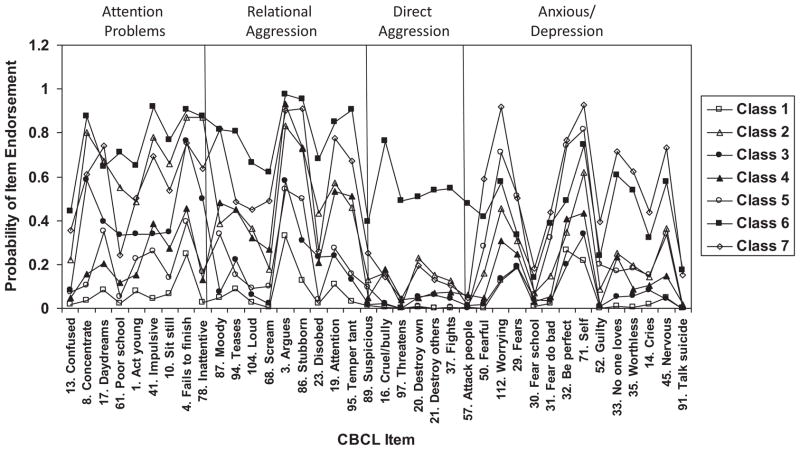
Psychopathology profile
From a previously described LCA [9], items from the three scales that comprise the DP (AP, AB, and AD) were entered, resulting in a seven class solution. These classes are shown in Figure 2. Table 1 provides the means on the AP, AB, and AD scales of the individual latent classes, referred to as C1-C7. This seven-class solution was most robust when sex was added as a covariate but age was not. Subsequently, the current analysis includes sex as a covariate but not age. See [9] for more details. The “Dysregulation Profile” class with elevated scores on AP, AB, and AD was identified as class C6 and there was a similar class, called C7, with similar elevated scores on many of the AP, AB, and AD items, but with but without direct aggression.
Figure 2.
Psychopathological classes (Based on Althoff et al. [9])
Table 1.
Mean CBCL Attention Problems, Aggressive Behavior, and Anxious-Depressed T-scores by psychopathology latent class.
| CBCL Psychopathology Class | AP Mean (SD) | AB Mean (SD) | AD Mean (SD) |
|---|---|---|---|
| Class 1 | 50.27 (1.85) | 50.06 (0.36) | 40.46 (1.56) |
| Class 2 | 62.39 (8.07) | 55.54 (4.69) | 55.49 (5.03) |
| Class 3 | 56.05 (5.57) | 50.49 (1.28) | 50.56 (1.55) |
| Class 4 | 51.18 (1.89) | 56.08 (6.15) | 52.59 (3.58) |
| Class 5 | 51.18 (3.09) | 50.47 (0.96) | 58.76 (5.91) |
| Class 6 (CBCL-DP) | 68.33 (10.28) | 73.33 (8.43) | 65.52 (10.43) |
| Class 7 | 65.65 (10.39) | 58.97 (7.03) | 69.14 (6.68) |
| Overall | 58.36 (10.14) | 57.68 (10.29) | 57.14 (9.57) |
Note. CBCL: Child Behavior Checklist; AP: Attention Problems; AB: Aggressive Behavior; AD: Anxious/Depressed; SD: Standard Deviation; CBCL-DP: CBCL-Dysregulation Profile.
Data Analyses
Descriptive Analyses
All descriptives were performed using SPSS 17.0 [27]. One-way ANOVAs were conducted to examine scores on the four temperament dimensions (NS, HA, RD, and P) by (1) the three latent JTCI temperament profiles and (2) the seven CBCL psychopathology classes. Since participants informants could be from the same family, Games-Howell post hoc analyses were conducted to account for the nested data.
Primary Analyses
To examine the main effects of psychopathology classes on the disengaged temperament profile dependent variable, and to account for the non-independence of these data (e.g., children within families), regression equations using Linear Mixed Models (LMM) analysis were employed, using the variance components covariance structure conducted in SPSS. Unlike General Linear Modeling procedures, LMM analysis models correlated errors that result from non-independent observations [28,29]. Family number was entered as the group variable to account for correlated errors of subjects within the same family. Probability of membership in the disengaged temperament profile (range = 0–1) was the dependent variable. Psychopathology class (coded 1–7) was the independent variable. In order to compare each class to the CBCL-DP, the class of primary interest, the psychopathology class variable was recoded such that the CBCL-DP class (Class 6) was the last (reference) category. Sex was included in the model as a covariate because it has been shown in previous research to be related to both the temperament profiles [4] and the psychopathology classes [9] used in this study. Because LMM allows only for comparisons against the reference category, post-hoc pair-wise comparisons using the Bonferroni correction were conducted to further explore differences in probability of membership in the disengaged temperament profile between psychopathology classes.
To provide additional descriptive information regarding the size of the relation between each psychopathology class and the disengaged temperament profile, odds ratios were calculated. Specifically, seven logistic regressions (one per psychopathology class) were conducted. For each regression, the dependent variable was disengaged temperament profile membership (1=member of disengaged profile, 0=member of another profile). The independent variable in each regression was a dichotomous class membership variable. For example, for the CBCL-DP class, the independent variable was coded such that 1=member of CBCL-DP and 0=member of another class. It should be emphasized that odds ratio calculations were conducted purely for descriptive purposes in order to obtain a more interpretable and clinically-relevant measure of effect than is available via LMM. The use of 7 separate regressions increases the probability of type I error (i.e., false positives) and thus in cases where LMM and odds ratio tests disagreed, LMM was weighted more heavily in interpretation of results.
Results
Descriptive Analyses
Examining the temperament profiles, there were significant differences between them on all temperamental dimensions in one-way ANOVAs: NS (F(2)=406.17, p<.001), HA (F(2)=4.48, p<.05), RD (F(2)=73.99, p<.001), and P (F(2)=257.40, p<.001). There were also significant differences on the temperamental dimensions among the psychopathology classes in one-way ANOVA: NS (F(2)=46.07, p<.001), HA (F(2)=15.17, p<.001), RD (F(2)=10.22, p<.001), and P (F(2)=19.59, p<.001). Mean NS, HA, RD, and P T-scores for each temperament profile and psychopathology class are shown in Table 2. Games-Howell post-hoc comparisons showed that the CBCL-DP (Class 6) had significantly higher NS (ps<.001) than all other psychopathology profiles. HA scores for the CBCL-DP were significantly higher compared to Classes 1, and 3 (ps<.01), and significantly lower than Class 7 (p<.01). RD scores for the CBCL-DP were significantly lower than those of Classes 1, 3, 4, and 5 (ps<.01). Finally, CBCL-DP P scores were significantly lower than those of Classes 1, 4, and 5 (ps<.001). No other comparisons with the CBCL-DP class were significant. Table 3 demonstrates the numbers of children classified into the three temperamental profiles as a function of psychopathology class.
Table 2.
Mean temperament scores for latent temperament profiles and psychopathology classes
| CBCL Psychopathology Class |
Temperament Dimension |
|||
|---|---|---|---|---|
| NS Mean (SD) | HA Mean (SD) | RD Mean (SD) | P Mean (SD) | |
| Class 1 | 43.42(6.91) | 46.25(7.88) | 53.41(7.57) | 56.28(8.61) |
| Class 2 | 51.81(8.12) | 49.48(10.01) | 48.62(9.49) | 45.07(8.36) |
| Class 3 | 48.97(7.07) | 43.92(6.82) | 53.36(8.51) | 47.37(7.54) |
| Class 4 | 49.25(7.91) | 47.98(9.96) | 50.92(10.78) | 53.38(9.49) |
| Class 5 | 41.50(6.31) | 55.74(8.36) | 53.35(8.43) | 56.84(10.55) |
| Class 6 (CBCL-DP) | 60.22(7.96) | 52.26(10.51) | 43.71(10.32) | 45.07(8.25) |
| Class 7 | 45.24(8.79) | 59.34(8.49) | 49.20(10.32) | 49.83(9.37) |
| Temperament Profile | ||||
| Steady | 38.28(4.54) | 52.30(9.97) | 54.15(8.31) | 60.62(6.96) |
| Moderate | 51.44(6.37) | 48.94(9.83) | 51.57(8.28) | 48.90(7.51) |
| Disengaged | 62.07(6.14) | 49.51(10.21) | 40.00(9.76) | 38.81(3.43) |
Note: CBCL: Child Behavior Checklist; NS: Novelty Seeking; HA: Harm Avoidance; RD: Reward Dependence; P: Persistence; SD: Standard Deviation; CBCL-DP: Child Behavior Checklist- Dysregulation Profile.
Table 3.
Cross-tabulations of psychopathology classes, sex, and temperament profiles
| CBCL Psychopathology Class | Sex | Temperament Profile | ||||
|---|---|---|---|---|---|---|
| Male | Female | Steady | Moderate | Disengaged | Total | |
| C1 | 41 | 44 | 39 | 44 | 2 | 85 |
| C2 | 42 | 15 | 41 | 3 | 13 | 57 |
| C3 | 25 | 15 | 27 | 6 | 7 | 40 |
| C4 | 19 | 30 | 31 | 12 | 6 | 49 |
| C5 | 12 | 19 | 10 | 21 | 0 | 31 |
| C6 (CBCL-DP) | 56 | 27 | 38 | 3 | 42 | 83 |
| C7 | 9 | 27 | 21 | 12 | 3 | 36 |
| Total | 204 | 177 | 207 | 101 | 73 | 381 |
Note. CBCL: Child Behavior Checklist; CBCL-DP: CBCL-Dysregulation Profile
Primary Analyses
LMM revealed that psychopathology latent class and sex were both significantly associated with endorsement of the disengaged temperament profile (see Table 4). While all seven psychopathology classes were significantly associated with the disengaged profile in either a positive or a negative direction, Bonferroni-corrected post hoc analyses illustrated that members of the CBCL-DP class (C6) were significantly more likely to have a disengaged temperament profile compared to the other six profiles (ps<0.001). Specifically, 51% of the CBCL-DP class had the disengaged temperament profile, whereas the prevalence of the disengaged temperament profile among the other CBCL classes was much lower, ranging from 0% (C5) to 23% (C2) (also see Table 3). Additionally, C2 (a class with moderate levels of co-occurring AB, AP, and AD) was significantly more likely to belong to the disengaged temperament profile than both C1 (the no or few symptoms class) and C5 (a class predominated by AD) (ps<0.001). LMM results indicated that boys had a higher probability of belonging to the disengaged class compared to girls.
Table 4.
Results of linear mixed model for disengaged temperament profile compared to psychopathology classes.
| F(df) | B | SE | β | |
|---|---|---|---|---|
| Intercept | 0.437 | 0.035 | 1.548** | |
| Psychopathology Class | 24.388 (373)** | |||
| C1 | −0.451 | 0.041 | 0.637** | |
| C2 | −0.215 | 0.045 | 0.806** | |
| C3 | −0.345 | 0.051 | 0.708** | |
| C4 | −0.349 | 0.048 | 0.705** | |
| C5 | −0.444 | 0.056 | 0.641** | |
| C7 | −0.342 | 0.054 | 0.710** | |
| C6 (CBCL-DP) | 0(a) | |||
| Sex | 8.544 (373)* | |||
| Male | 0.083 | 0.028 | 1.087* | |
| Female | 0(a) | |||
Note. a This parameter is set to zero because it is the reference category; b = unstandardized regression coefficient; SE = standard error; df = degrees of freedom;
p<0.05,
p<0.001
Odds ratios were calculated using disengaged temperament profile membership as the dependent variable and each psychopathology class as a predictor to better describe effect size (Table 5). The logistic regression using Class 5 as a predictor did not successfully converge due to zero members of this class belonging to the disengaged temperament profile. Results were generally consistent with LMM analyses. Those in the CBCL-DP class (C6) were 8.82 times more likely to belong to the disengaged temperament profile compared to youth in other psychopathology classes. Class 1 was significantly less likely to display a disengaged temperament profile compared to the other classes. The 95% confidence interval crossed 1 for the other classes, indicating that members of these other classes were no more or less likely to belong to the disengaged temperament profile. The odds ratio for sex demonstrated that boys were more likely than girls to belong to the disengaged temperament profile.
Table 5.
Odds ratios for membership in disengaged temperament profile by psychopathology class
| CBCL Psychopathology Class | Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| C1 | 0.076 | 0.018 | 0.318 |
| C2 | 1.3 | 0.659 | 2.564 |
| C3 | 0.884 | 0.374 | 2.086 |
| C4 | 0.552 | 0.225 | 1.351 |
| C5* | - | - | - |
| C6 (CBCL-DP) | 8.823 | 4.996 | 15.582 |
| C7 | 0.357 | 0.106 | 1.198 |
| sex | 0.363 | 0.207 | 0.636 |
None of the individuals loading highest on C5 also endorsed the disengaged profile
Discussion
The current findings indicate that youth with the CBCL-DP are significantly more likely than any of the comparison latent classes of psychopathology to display a “disengaged” temperamental pattern characterized by relatively high novelty seeking (NS), high harm avoidance (HA), low reward dependence (RD), and low persistence (P). This temperamental profile has been shown to be related to low functioning and increased psychopathology relative to other empirically-derived profiles [4].
High HA, which contains elements of shyness and reluctance to engage with peers or in new situations, may seem a counterintuitive characteristic for children who have been described as having “rage attacks”[30] or being “explosive”. On the basis of high aggressive behavior, these children do appear prone to destroy their own and others’ belongings, to threaten, to attack other people, etc. However, the finding of high HA in these children puts some of those behaviors in a slightly different light. Consistent with endorsement of externalizing problems (e.g., aggression, hyperactivity), these children are simultaneously rated highly on NS. They may enter into new situations readily and without apparent regard for the consequences of their actions, but once there and, unlike their peers with elevations in only the AB or AP scales, CBCL-DP children may be frightened, shy, and uncomfortable. Thus, these youth are prone to distress via both a temperamental “push” and “pull” (i.e., high NS and HA), but also have fewer temperamental resources available to help them delay gratification, cope with distress, and see difficult situations through to resolution. This temperamental profile is similar to those identified in adults with DSM-IV Cluster B personality disorders [31,32,33] and is consistent with reports that children with CBCL-DP develop Cluster B personality traits at higher rates than controls [14]. The occurrence of high NS, high HA, and low P among CBCL-DP youth is also consistent with previous studies (e.g., [16]) that suggest the profile is an indicator of disordered self-regulation.
As self-regulation is a fundamental developmental process, the presence of peaks on attention problems, aggressive behavior, and anxious-depression may be seen in many child and adolescent diagnoses. Given that youth with the CBCL-DP may require a high level of psychiatric care [18] later in life, the ability to identify potential precursors to the development of this impairing syndrome is critical. Prospective study designs are needed to determine whether this temperamental profile can be identified early in development before psychopathology develops or reaches clinically significant levels. Should such studies confirm the relation of early disengaged temperament with later CBCL-DP, prevention efforts can be used to enhance coping skills and self- regulation strategies to decrease risk for CBCL-DP. Given previous work demonstrating the significant shared and unique environmental contributions to the expression of the CBCL-DP found most prominent in early childhood [10,11], early intervention in childhood could have tremendous psychosocial benefits.
These findings might also help to describe the likely clinical presentation of youth with the CBCL-DP. In the clinic, a child with the CBCL-DP might be expected to present as a somewhat reluctant contributor to the examination. Interested in the novelty of the situation and hyperactive by nature (high NS), his initial reluctance may be observed as shyness or timidity (high HA). Outside the office, impulsive lashing-out may be reported in situations both when the child is more comfortable and when the child’s anxiety overwhelms his decreased regulatory capacity. In response to clinician recommendations, there may also be a reduced ability to stick with the goals that are set for him (low P). Difficulty navigating out of such responses may be compounded when one considers that one or both of his parents may have a similar temperamental profile (given the high heritability): a possible example of what may be described as a poor “fit”. Clearly this lack of fit may be one contributor to a poor outcome in a child’s life [34].
There are limitations to our study. First, this was a cross-sectional study and thus causality, or direction of effect, cannot be confirmed. Additional research studies, including prospective investigations of these associations, are necessary to better determine causation. Relatedly, while the boundary between temperament and personality remains unclear, temperament is generally thought to precede personality and contribute to its development [35,36]. Both constructs have been found to be moderately stable, although certainly not unwavering over time [37,38]. Second, method invariance associated with the use of only mother reports could have artificially inflated associations. Replication studies should implement multiple informant and observational methods of assessment to address this limitation. Finally, the sample used in this study was originally selected in order to study attention problems and aggression in clinically-referred youth and their families. Therefore, our findings may not be generalizeable to the general population and should be replicated in more representative community and clinical samples. It is important to note, however, that the sample also included unaffected siblings of the clinic-referred probands, which does improve generalizability.
Summary
The current study employed a person-centered approach to the analysis of temperament and psychopathology (i.e., LPA & LCA). The advantages of using a person-centered approaches to data analysis to complement a more traditional variable-centered approaches have been outlined in previous literature [39]. These methods allowed us to capture the heterogeneity in individual patterns of temperament and psychopathology in a way that is not possible using traditional variable-centered approaches. These person-centered data analytic approaches provided a means by which we could utilize previously established empirically-derived patterns of traits and behaviors that have been suggested by other studies, deriving these constructs primarily from theory (e.g., [40]). The convergence of these methods, resulting in empirically-identified person-centered profiles and classes consistent with theory and variable-centered analyses (e.g., [16]), further supports the use of the CBCL-DP to measure poor self-regulation, measured here by temperament. Pending replication and examination of temperament and the CBCL-DP longitudinally, we believe that clinical applications targeting pre-clinical levels of the CBCL-DP and/or the related temperamental profile (i.e., disengaged) can have a significant impact on the prevention of not only clinical levels of CBCL-DP, but also of suicidal behavior, substance use disorders, and mood and anxiety disorders [18].
References
- 1.Rettew DC, Copeland W, Stanger C, Hudziak JJ. Associations Between Temperament and DSM-IV Externalizing Disorders in Children and Adolescents. J Dev Behav Pediatr. 2004;25:383–391. doi: 10.1097/00004703-200412000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rettew DC, Doyle AC, Kwan M, Stanger C, Hudziak JJ. Exploring the boundary between temperament and generalized anxiety disorder: a receiver operating characteristic analysis. J Anxiety Disord. 2006;20:931–945. doi: 10.1016/j.janxdis.2006.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luby JL, Svrakic DM, McCallum K, Przybeck TR, Cloninger CR. The Junior Temperament and Character Inventory: preliminary validation of a child self-report measure. Psychol Rep. 1999;84:1127–1138. doi: 10.2466/pr0.1999.84.3c.1127. [DOI] [PubMed] [Google Scholar]
- 4.Rettew DC, Althoff RR, Dumenci L, Ayer L, Hudziak JJ. Latent profiles of temperament and their relations to psychopathology and wellness. J Am Acad Child Adolesc Psychiatry. 2008;47:273–281. doi: 10.1097/CHI.0b013e318160b403. [DOI] [PubMed] [Google Scholar]
- 5.Tillman R, Geller B, Craney JL, Bolhofner K, Williams M, Zimerman B, et al. Temperament and character factors in a prepubertal and early adolescent bipolar disorder phenotype compared to attention deficit hyperactive and normal controls. J Child Adolesc Psychopharmacol. 2003;13:531–543. doi: 10.1089/104454603322724922. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. [Website accessed November 17 2011];DSM-5 Development. 2011 http://www.dsm5.org/proposedrevision/pages/proposedrevision.aspx?rid=397.
- 7.Volk HE, Todd RD. Does the Child Behavior Checklist juvenile bipolar disorder phenotype identify bipolar disorder? Biol Psychiatry. 2007;62:115–120. doi: 10.1016/j.biopsych.2006.05.036. [DOI] [PubMed] [Google Scholar]
- 8.Mick E, Biederman J, Pandina G, Faraone SV. A preliminary meta-analysis of the child behavior checklist in pediatric bipolar disorder. Biol Psychiatry. 2003;53:1021–1027. doi: 10.1016/s0006-3223(03)00234-8. [DOI] [PubMed] [Google Scholar]
- 9.van Domburgh L, Loeber R, Bezemer D, Stallings R, Stouthamer-Loeber M. Childhood predictors of desistance and level of persistence in offending in early onset offenders. J Abnorm Child Psychol. 2009;37:967–980. doi: 10.1007/s10802-009-9329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hudziak JJ, Althoff RR, Derks EM, Faraone SV, Boomsma DI. Prevalence and genetic architecture of Child Behavior Checklist-juvenile bipolar disorder. Biol Psychiatry. 2005;58:562–568. doi: 10.1016/j.biopsych.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 11.Boomsma DI, Rebollo I, Derks EM, van Beijsterveldt TC, Althoff RR, Rettew DC, et al. Longitudinal stability of the CBCL-juvenile bipolar disorder phenotype: A study in Dutch twins. Biol Psychiatry. 2006;60:912–920. doi: 10.1016/j.biopsych.2006.02.028. [DOI] [PubMed] [Google Scholar]
- 12.McGough JJ, Loo SK, McCracken JT, Dang J, Clark S, Nelson SF, et al. CBCL Pediatric Bipolar Disorder Profile and ADHD: Comorbidity and Quantitative Trait Loci Analysis. J Am Acad Child Adolesc Psychiatry. 2008;47:1151–1157. doi: 10.1097/CHI.0b013e3181825a68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doyle AE, Biederman J, Ferreira MA, Wong P, Smoller JW, Faraone SV. Suggestive linkage of the child behavior checklist juvenile bipolar disorder phenotype to 1p21, 6p21, and 8q21. J Am Acad Child Adolesc Psychiatry. 2010;49:378–387. [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer SE, Carlson GA, Youngstrom E, Ronsaville DS, Martinez PE, Gold PW, et al. Long-term outcomes of youth who manifested the CBCL-Pediatric Bipolar Disorder phenotype during childhood and/or adolescence. J Affect Disord. 2009;113:227–235. doi: 10.1016/j.jad.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 15.Biederman J, Petty CR, Monuteaux MC, Evans M, Parcell T, Faraone SV, et al. The child behavior checklist-pediatric bipolar disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: a longitudinal analysis. J Clin Psychiatry. 2009;70:732–740. doi: 10.4088/JCP.08m04821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayer L, Althoff R, Ivanova M, Rettew D, Waxler E, Sulman J, et al. Child Behavior Checklist Juvenile Bipolar Disorder (CBCL-JBD) and CBCL Posttraumatic Stress Problems (CBCL-PTSP) scales are measures of a single dysregulatory syndrome. J Child Psychol Psychiatry. 2009;50:1291–1300. doi: 10.1111/j.1469-7610.2009.02089.x. [DOI] [PubMed] [Google Scholar]
- 17.Althoff RR, Rettew DC, Faraone SV, Boomsma DI, Hudziak JJ. Latent class analysis shows strong heritability of the child behavior checklist-juvenile bipolar phenotype. Biol Psychiatry. 2006;60:903–911. doi: 10.1016/j.biopsych.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 18.Althoff RR, Verhulst F, Rettew DC, Hudziak JJ, van der Ende J. Adult Outcomes of Childhood Dysregulation: A 14-year Follow-up Study. J Am Acad Child Adolesc Psychiatry. 2010;49:1105–1116. doi: 10.1016/j.jaac.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mick E, McGough J, Loo S, Doyle AE, Wozniak J, Wilens TE, et al. Genome-wide association study of the child behavior checklist dysregulation profile. J Am Acad Child Adolesc Psychiatry. 2011;50:807–817. doi: 10.1016/j.jaac.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holtmann M, Duketis E, Goth K, Poustka L, Boelte S. Severe affective and behavioral dysregulation in youth is associated with increased serum TSH. J Affect Disord. 2010;121:184–188. doi: 10.1016/j.jad.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 21.Zepf FD, Wockel L, Poustka F, Holtmann M. Diminished 5-HT functioning in CBCL pediatric bipolar disorder-profiled ADHD patients versus normal ADHD: susceptibility to rapid tryptophan depletion influences reaction time performance. Hum Psychopharmacol. 2008;23:291–299. doi: 10.1002/hup.934. [DOI] [PubMed] [Google Scholar]
- 22.Holtmann M, Buchmann AF, Esser G, Schmidt MH, Banaschewski T, Laucht M. The Child Behavior Checklist-Dysregulation Profile predicts substance use, suicidality, and functional impairment: a longitudinal analysis. J Child Psychol Psychiatry. 2011;52:139–147. doi: 10.1111/j.1469-7610.2010.02309.x. [DOI] [PubMed] [Google Scholar]
- 23.Hollingshead AB. Unpublished paper. Yale University, Department of Sociology; New Haven, CT: 1975. Four factor index of social status. [Google Scholar]
- 24.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. Temperament and Character Inventory: A Guide to Its Development and use. Center for Psychobiology of Personality Department of Psychiatry, Washington University; St. Louis, MO: 1994. [Google Scholar]
- 25.Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- 26.Achenbach TM. Manual for the Child Behavior Checklist/4–18. Department of Psychiatry, University of Vermont; Burlington, VT: 1991. [Google Scholar]
- 27.SPSS. SPSS for Windows, Rel. 15.0.1. SPSS Inc; Chicago, IL: 2006. [Google Scholar]
- 28.Hox JJ. Multilevel Analysis: Techniques and Applications. Routledge; New York, NY: 2010. [Google Scholar]
- 29.Hox JJ. Applied Multilevel Analysis. TT-Publikaties; Amsterdam, The Netherlands: 1995. [Google Scholar]
- 30.Carlson GA. Who are the children with severe mood dysregulation, a.k.a. “rages”? Am J Psychiatry. 2007;164:1140–1142. doi: 10.1176/appi.ajp.2007.07050830. [DOI] [PubMed] [Google Scholar]
- 31.Barnow S, Herpertz SC, Spitzer C, Stopsack M, Preuss UW, Grabe HJ, et al. Temperament and Character in Patients with Borderline Personality Disorder Taking Gender and Comorbidity into Account. Psychopathology. 2007;40:369–378. doi: 10.1159/000106467. [DOI] [PubMed] [Google Scholar]
- 32.Joyce PR, McKenzie JM, Luty SE, Mulder RT, Carter JD, Sullivan PF, et al. Temperament, childhood environment and psychopathology as risk factors for avoidant and borderline personality disorders. Aust N Z J Psychiatry. 2003;37:756–764. doi: 10.1080/j.1440-1614.2003.01263.x. [DOI] [PubMed] [Google Scholar]
- 33.Joyce PR, Mulder RT, Luty SE, McKenzie JM, Sullivan PF, Cloninger RC. Borderline personality disorder in major depression: symptomatology, temperament, character, differential drug response, and 6-month outcome. Compr Psychiatry. 2003;44:35–43. doi: 10.1053/comp.2003.50001. [DOI] [PubMed] [Google Scholar]
- 34.Rettew DC, Stanger C, McKee L, Doyle A, Hudziak JJ. Interactions between child and parent temperament and child behavior problems. Compr Psychiatry. 2006;47:412–420. doi: 10.1016/j.comppsych.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rettew DC, McKee L. Temperament and its role in developmental psychopathology. Harv Rev Psychiatry. 2005;13:14–27. doi: 10.1080/10673220590923146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rothbart MK, Ahadi SA. Temperament and the development of personality. J Abnorm Psychol. 1994;103:55–66. doi: 10.1037//0021-843x.103.1.55. [DOI] [PubMed] [Google Scholar]
- 37.Viken RJ, Rose RJ, Kaprio J, Koskenvuo M. A developmental genetic analysis of adult personality: extraversion and neuroticism from 18 to 59 years of age. J Pers Soc Psychol. 1994;66:722–730. doi: 10.1037//0022-3514.66.4.722. [DOI] [PubMed] [Google Scholar]
- 38.Kagan J. Galen’s prophecy : temperament in human nature. Basic Books; New York, NY: 1994. [Google Scholar]
- 39.von Eye A, Bogat GA, Rhodes JE. Variable-oriented and person-oriented perspectives of analysis: the example of alcohol consumption in adolescence. J Adolesc. 2006;29:981–1004. doi: 10.1016/j.adolescence.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 40.Biederman J, Wozniak J, Kiely K, Ablon S, Faraone S, Mick E, et al. CBCL clinical scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. J Am Acad Child Adolesc Psychiatry. 1995;34:464–471. [PubMed] [Google Scholar]