Abstract
Background
Stimulated by the WHO Framework Convention on Tobacco Control, many countries in Latin America adopted comprehensive smoke-free policies. In March 2006, Uruguay became the first Latin American country to adopt 100% smoke-free national legislation, which ended smoking in all indoor public places and workplaces, including restaurants and bars. The objective of this study was to evaluate trends in hospital admissions for cardiovascular disease 2 years before and 2 years after the policy was implemented in Uruguay.
Methods
Reports of hospital admissions for acute myocardial infarction (AMI) (International Classification of Disease-10 I21) from 37 hospitals (79% of all hospital admissions in the country), representing the period 2 years before and 2 years after the adoption of a nationwide smoke-free policy in Uruguay (between 1 March 2004 and 29 February 2008), were reviewed. A time series analysis was undertaken to compare the average monthly number of events of hospital admission for AMI before and after the smoke-free law.
Results
A total of 7949 hospital admissions for AMI were identified during the 4-year study period. Two years after the smoke-free policy was enacted, hospital admissions for AMI fell by 22%. The same pattern and roughly the same magnitude of reduction in AMI admissions were observed for patients seen in public and private hospitals, men, women and people aged 40–65 years and older than 65 years.
Conclusions
The national smoke-free policy implemented in Uruguay in 2006 was associated with a significant reduction in hospital admissions for AMI.
INTRODUCTION
Until the mid-2000s, indoor smoking was the norm in most countries of Latin America. However, stimulated mostly by the 2001 Pan American Health Organization’s Smoke-free Americas Initiative1 and by the 2003 WHO Framework Convention on Tobacco Control, many countries and subnational jurisdictions have adopted comprehensive indoor smoking restrictions. In March 2006, Uruguay (population 3 400 000) became the first Latin American country to adopt a comprehensive smoke-free national legislation, which ended smoking in all indoor public places and workplaces, including restaurants and bars. Panama (2008), Colombia (2009), Guatemala (2009), Honduras (2011), Peru (2011) and Venezuela (2011) have followed the example of Uruguay adopting 100% smoke-free legislation at the national level. Ecuador (2011) approved a 100% smoke-free policy, which is expected to be implemented later in 2012. In addition, several subnational jurisdictions (states/ provinces and/or cities) in Argentina, Brazil and Mexico have enacted such policies. This paper reports the results of a study to investigate the impact on cardiovascular health of Uruguay’s smoke-free policy adopted in 2006.
We hypothesised that rates of acute myocardial infarction (AMI) hospital admissions would be reduced in Uruguay after implementation of the smoke-free law consistent with other reports in the scientific literature. Studies conducted in high-income countries (in national and subnational jurisdictions) in North America (USA and Canada) and in Western Europe have reported reductions in hospital admissions for AMI after the adoption of a comprehensive smoke-free policy. Three independent meta-analyses, two conducted in 2009 and a third one in 2010, showed an overall effect of 17% decrease in AMI incidence after 1 year with the effect growing with time.2-4 In addition, one study conducted in Argentina comparing Santa Fe (a 100% smoke-free province) with Buenos Aires city (partial smoking restrictions) as a control showed a reduction of 13% in hospital admissions for acute coronary syndrome (ACS) in Santa Fe.5
It is well known that second-hand smoke (SHS) is an important source of indoor air pollution that increases exposure to fine particles, which in turn increase the risk of the occurrence of AMI. Several studies have shown reductions in fine particles (PM2.5, an indicator of exposure to SHS) following implementation of a comprehensive smoke-free law (eg, smoke-free policy in all indoor public places and workplaces).6 In 2010, the Institute of Medicine concluded that the observed reductions in AMI admissions were consistent with the biology of AMI indicating a causal relationship between indoor smoke-free and decreased risk of AMI.7
This study is the first of this type conducted at the national level in a middle-income country in Latin America to examine trends in AMI hospital admissions associated with the implementation of a smoke-free policy. We hypothesised that the adoption of the public policy would be associated with a reduction in hospital admissions rates for AMI.
METHODS
Ethics review
A research protocol was reviewed and received ethics clearance through the Office of Research Subject Protection at Roswell Park Cancer Institute in Buffalo, New York, and at the School of Medicine, University of the Republic in Montevideo, Uruguay.
Study design
We performed an exhaustive medical record review that involved a time series analysis comparing number of events of hospital admissions for AMI in Uruguay from 2 years before (1 March 2004 to 28 February 2006) with number of events from 2 years after (1 March 2006 to 29 February 2008) the adoption of the smoke-free policy in 1 March 2006. The reviews were performed at each hospital by research assistants (physicians and nurses) who were specifically trained to do the record reviews by the investigator from the Centro de Investigación para la Epidemia del Tabaquismo (CIET, Center for Tobacco Epidemic Research) in Montevideo. A collection form was developed to extract the data, including identification number, admission date, hospital name, age, gender, ischaemic symptoms, cardiac markers, ECG changes, type of IAM (primary or secondary) and transfer to another hospital. At each hospital, a list of patients admitted for AMI was obtained, which was used as a guide by the research assistants who reviewed each medical record and filled the data in the collection form.
Outcome measure
The primary outcome variable measured was the number of events per month of hospital admissions for AMI. The primary analysis focused on AMI in persons who went to a hospital. We used the principal admission primary diagnosis for AMI, which in Uruguay is established by the attending physician at the time of discharge after both admission and evolution findings are evaluated. Codes were assigned by the hospital medical record technicians. In Uruguay, diagnosis are coded according to the International Classification of Disease, version 10 (ICD-10th) diagnostic codes I21.0–I21.9 for AMI. To avoid bias, we excluded secondary AMI diagnosis.
Diagnostic criteria for AMI includes symptoms (acute chest pain), ECG findings (eg, pathological Q waves) and elevation of serum enzymes (eg, raised troponin I or T concentrations or creatine phosphokinase activity MB fraction) at the time of admission (see box 1). Since the end of 2000, Uruguay adopted the new definition criteria for AMI following the recommendations of the Joint European Society of Cardiology/American College of Cardiology Committee, which includes the serum levels of troponin as a biomarker for diagnosis. Since 2002, all hospitals in Uruguay had already adopted this new diagnosis criterion. Since our study started in 2004, this change did not affect the estimation of the events.
Box 1 Diagnosis criteria for acute myocardial infarction.
Increase and/or decrease in cardiac biomarkers (eg, creatine phosphokinase MB fraction, troponin) with at least one value above the 99 percentile limit of the medical centre AND
- At least one of the following:
- Ischaemic symptoms (eg, chest pain)
- ECG changes indicating new ischaemia (eg, ST-T changes or new left bundle branch block)
- Development of pathological Q waves on ECG
- Imaging study of new loss of viable myocardium or new impairment of motility parietal or fresh thrombus found on angiography.
Setting and participants
We collected hospital admissions for AMI for all patients at least 20 years old with a primary diagnosis of AMI (ICD-10th code I21) admitted in 37 public and private hospitals (of a total of 44), accounting for 79% of all AMI admissions in the entire country. Six hospitals were excluded due to unavailability of reliable data of all patients admitted for AMI and one hospital because the data were inconsistent with the information provided by the National Fund of Resources (see below). Four are private institutions (two from Montevideo and two from the rest of the country) and three are public healthcare centres (two from Montevideo and one from the rest of the country). The characteristics of patients and AMI rates in the seven excluded hospitals were not compared with patient characteristics and AMI rates in the 37 included hospitals. Non-country residents and patients with AMI after a coronary angioplasty or bypass, or as a complication of another disease, were excluded.
Quality control review
In each hospital, 10% of medical records were randomly selected and audited to confirm the AMI diagnosis. The CIET investigators reviewed the medical records randomly selected from the total hospital discharge registry with an AMI diagnosis to check the quality of data collection. The medical records with AMI diagnosis not confirmed (diagnoses criteria not fulfilled; see box 1) were between 0% and 1.8% (median 1.3%) in all but one of the 37 hospitals, which had an error rate of 3.4%. All medical records were reviewed for that hospital. We verified all records and included only those who had AMI diagnosis according to the protocol definition.
Not all AMI cases get admitted to a hospital and not all hospitals participated in our study. To examine trends in AMI rates not included in hospital admission records from our study, we compared the discharge hospital data with a reliable national database, the Fondo Nacional de Recursos (National Fund of Resources), which provides financial coverage to all interventional cardiovascular procedures performed in the country. Using the patient national identification number, we discarded duplicated data in patients admitted in more than one hospital in relation to the same AMI.
Statistical analysis
We tested for an effect of the smoke-free law using a multiple linear regression for the number of AMIs per month with the independent variables time (a continuous variable measured in years, with time 0 at March 2006, the month the smoke-free law took effect), a dummy variable (Law) set to 1 beginning in March 2006 when the smoke-free law took effect and 0 before then and 11 effects coded dummy variables for month to account for seasonal variation in the number of AMIs each month. (For example, the variable time is 10/12=0.83 for January 2007, the 10th month when the law was in effect.) With this coding, the constant in the regression equation is an estimate of the number of AMI admissions in March 2006, when the law took effect, the Law variable estimates any constant shift in the number of monthly AMIs after the law compared to before the law and the law by time interaction estimates changes in time trend in the number of monthly AMIs (ie, a slope change).
The same analysis was done for the average age of people admitted with AMIs to test whether the results were affected by population changes. We examined an autocorrelation plot for the residuals and it did not indicate any problem with higher serial autocorrelations.
We also investigated three alternative statistical analyses. To reduce the number of variables in the regression equation, we fit a model coding seasonality into four quarters (with three dummy variables) rather than 12 months (with 11 dummy variables), for a total of six independent variables, which yields eight data points per variable. We also fit ARIMA and negative binomial regression models using the same independent variables as the main time series linear regression.
The α level used to assess statistical significance was 0.05. Linear regressions were done with Minitab V.14, and the ARIMA and negative binomial regressions were done with Stata V.10.
RESULTS
We reviewed a total of 7949 medical records with confirmed AMI between 1 March 2004 and 29 February 2008, of which 65% were men and 35% were women.
Table 1 summarises the results of the regression analysis. The values of R2 indicate reasonable fits, and the Durbine–Watson statistics do not suggest serial correlation in the residuals. Two years after the smoke-free policy adoption in enclosed public places and workplaces, hospital admissions for AMI were reduced by 22% (approximately 550 cases per year were prevented). Figure 1 shows the total number of AMI events per month during the 4-year period of the data collection.
Table 1.
Results from regression analysis for monthly number of AMIs per month
| Population | Constant | Time (years)* |
Post law | Time after law (years)† |
R2 | Durbin– Watson statistic |
Percentage drop in monthly admissions‡ |
|---|---|---|---|---|---|---|---|
| All | 167±7 | 5.48±0.92 (0.364) |
−35.9±10.1 (0.001) |
−6.37±7.79 (0.419) |
0.70 | 2.43 | 22% |
| Private | 118±5 | −5.37±4.35 (0.225) |
−26.1±7.4 (0.001) |
9.83±5.70 (0.094) |
0.75 | 2.17 | 22% |
| Public | 68±3 | 10.85±2.89 (0.001) |
−9.8±4.9 (0.054) |
−16.21±3.79 (0.001) |
0.59 | 2.20 | 14%§ |
| Male | 121±6 | 2.66±5.23 (0.614) |
−23.9±8.8 (0.012) |
−3.33±6.85 (0.630) |
0.58 | 2.59 | 20% |
| Female | 66±3 | 2.82±2.63 (0.291) |
−12.5±4.4 (0.008) |
−3.05±3.44 (0.382) |
0.61 | 1.88 | 19% |
| Age under 40 |
3±0.5 | 0.50±0.44 (0.260) |
−1.36±0.74 (0.076) |
−0.68±0.58 (0.250) |
0.51 | 2.14 | − ¶ |
| Age 40–65 | 79±4 | −1.35±3.12 (0.669) |
−11.68±5.28 (0.034) |
0.78±4.10 (0.850) |
0.59 | 2.41 | 15% |
| Age over 65 |
105±5 | 6.32±4.34 (0.154) |
−22.9±7.3 (0.004) |
−6.48±5.68 (0.262) |
0.64 | 2.33 | 22% |
| Average Age |
66.5±0.4 | 0.27±0.35 (0.448) |
0.10±0.60 (0.874) |
−0.27±0.46 (0.560) |
0.38 | 2.01 | – |
Grey shading indicates statistically significant results. n=48.
Numbers following ± are SEs.
Numbers in parenthesis are p values.
Coefficients for effects coded month dummy variables not shown.
Time in years is set to 0 for March 2006 for each month, the month that the smoke-free law went into effect.
Law × time interaction.
Post law coefficient divided by constant.
This percentage underestimates the effect because the number of AMI admissions falls over time.
The change was not statistically significant.
AMI, acute myocardial infarction.
Figure 1.
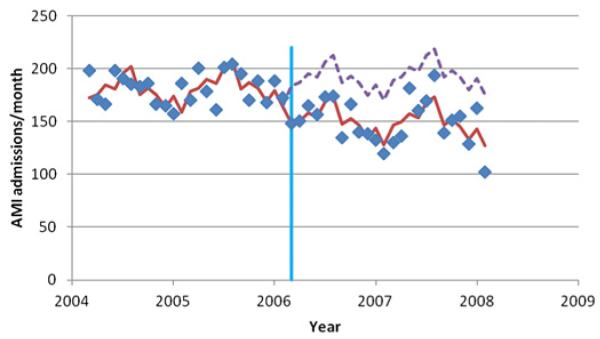
The solid line shows the total number of acute myocardial infarction (AMI) events per month in Uruguay from 1 March 2004 to 29 February 2008. The dashed line is the counterfactual of no law obtained by setting the ‘law’ dummy to zero in the regression equation. The vertical line indicates the date of the smoke-free policy implementation (1 March 2006). This figure is produced in colour in the online journal—please visit the website to view the colour figure.
Except for public hospitals, there was no underlying time trend in the number of seasonally adjusted monthly AMI admissions. There was a significant drop of −35.9±10.1 (SE) AMIs/month following implementation of the law compared to the seasonally adjusted average (as of March 2006, the constant in the regression equation) of 167±7 AMIs/month, a 22% drop. There was no evidence that this effect increased or diminished over time following the law (the coefficient associated with time after the law, ie, the time × law interaction, was not significant).
Similar results were observed for private hospitals, men, women and people aged 40e65 years and older than 65 years, with reductions in monthly AMI admissions between 15% and 22%. There was a non-significant trend towards fewer monthly AMIs in people younger than 40 years (p=0.076).
The law was also associated with fewer admissions to public hospitals, but the pattern differed from private hospitals. Whereas the number of monthly admissions was stable over time in the private hospitals, the number of AMIs was increasing before the law, a trend that was reversed following the law.
There was no association with the age of patients with time or the passage of the law, indicating that population age changes over time did not contribute to these results.
The alternative statistical analyses yielded the same conclusions as the main analysis. The multiple linear regressions with four quarters (instead of 12 months) to account for seasonality resulted in an estimate of the immediate effect of the law that was essentially the same as the main model: −37.192±9.831 (SE) AMIs/month (p<0.001) for the quarterly model versus −35.89±10.06 (p<0.001) for the monthly model. The ARIMA model yielded a similar estimate for the immediate effect of the law as the two linear regression models: −29.56±7.87 (p<0.001). The negative binomial regression yielded an incidence rate ratio following the law of 0.84 (95% CI 0.78 to 0.91, p<0.0005). None of these models found a significant effect of time after the law.
DISCUSSION
The national smoke-free policy implemented in Uruguay in 2006 was associated with a significant reduction in hospital admissions for AMI. This result is consistent with similar observational studies conducted in other countries and subnational jurisdictions that have found a reduction in AMI following implementation of a smoke-free policy.2-4 The implementation of comprehensive smoke-free policies has generally been followed by rapid declines in hospital admissions for AMI, averaging 17% 1 year after the laws took effect and growing to about 30% after 3 years.8 In fact, our study found a reduction of 22% after 2 years of the implementation of the law. A quantitative comparison of our results with the studies included in the meta-analyses confirmed that results from Uruguay (a middle-income country) are well within the range of studies from high-income countries from North America and Europe.9-19 The results of this study are also consistent with that predicted by reducing exposure to a high concentration of inhalable smoke particles based on the recent Institute of Medicine report.7 The report examined the various biological mechanisms, whereby exposure to SHS can exert detrimental effects on cardiovascular health. The report concluded that there is sufficient evidence to support the biological plausibility of a causal relationship between SHS exposure and AMI as well as between the implementation of indoor smoke-free policies and decreased risk of AMI.
A study assessing the indoor air quality of indoor public places in Uruguay before and after the smoke-free law showed that the concentration of particles of 2.5 μ in diameter (PM2.5) decreased dramatically after the implementation of the law (from 210 to 18 μg/m3).6 Another study measuring air nicotine concentrations in indoor public places and workplaces in Montevideo showed a reduction from 0.75 mg/m3 in 2002 to 0.07 μg/m3 in 2007 (overall reduction of 91%).20 The International Tobacco Control Policy Evaluation Project (ITC Project), a survey of a cohort of adult smokers conducted in Uruguay after the implementation of the smoke-free law, showed that exposure to SHS in various public venues decreased as a result of the policy.21,22 These three studies confirmed that Uruguay reached and maintains a high level of compliance of its smoke-free policy, resulting in low levels of SHS exposure in public places and workplaces.
The WHO/US Centers for Disease Control and Prevention (CDC) Global Adults Tobacco Survey conducted in Uruguay in 2009 showed an adult (15 years and older) smoking prevalence of 25% (30.7% of men and 19.8% of women)23 similar to a national survey conducted by CIET in 2008 that revealed an adult smoking prevalence of 24.8% (29.4% of men and 20.9% of women).24 A national survey conducted by the Junta Nacional de Drogas (National Committee of Drugs) in 1998, 2001 and 2006 had showed a smoking prevalence of 32.5%, 32.3% and 31.8%, respectively.24 These data show a stable prevalence between 1998 and 2006 (before the law was adopted) and a decrease in the smoking prevalence of around 7 points since 2006 (year of the implementation of the law).
A time series analysis of ACS hospital admissions comparing Santa Fe province (100% smoke-free) with Buenos Aires city (smoking designated areas), before and after the implementation of the laws in each district, was conducted in Argentina in 2010. Results showed an immediate decrease in ACS admissions (−2.5 admissions per 100 000, p=0.03; 13% reduction) after implementation of the law in Santa Fe (compared with no change in Buenos Aires city), followed by a persistent decrease in admissions due to ACS (−0.26 admissions per 100 000 per month).5
According to the WHO/CDC Global Youth Tobacco Survey conducted in 2007, 50.5% of students lived in homes where others smoke.25 In 2009, Global Adults Tobacco Survey showed that 29.2% of adults were exposed to SHS at home at least weakly.23
Limitations
The study has some limitations that need to be noted. First, we were not able to assess the smoking status of the admitted patients and thus cannot confidently attribute the entire observed reduction in AMI hospital admissions solely to a change in exposure to SHS. Some smokers may have stopped smoking in response to the smoke-free law and other tobacco control measures implemented in Uruguay at about the same time. In 2006, another presidential decree was issued to implement pictorial health warning labels printed on 50% (later increased to the current 80%) of both main faces of the cigarette packages. The content of some of the warnings were related to the effects of SHS and in support of the newly implemented smoke-free policy. In addition, two education campaigns, ‘A million thanks’ (before the implementation) and ‘Smoke-free Uruguay’ (after the implementation), were carried out to support the law. Both the warning labels and the education campaigns might have contributed to the decrease in both the smoking prevalence and SHS exposure in public places. Second, we were not able to obtain individual information on other cardiovascular risk factors, such as cholesterol, diet, body mass index, family and personal history of coronary heart disease, exercise, alcohol intake, diabetes and hypertension. Thus, it is possible that there could be some other unmeasured risk factor for AMI that changed around the same time that the smoke-free law was implemented. Third, not all hospitals participated in the study and there may have been differences in AMI rates from the hospitals that were included in the study. Finally, we were not able to review the death certificates and therefore the patients who died before reaching the hospital were not captured for our study.
CONCLUSIONS
This study captured data for 79% of AMI hospital admissions in Uruguay for 4-year span, allowing us to examine trends in the rate of AMI 2 years before and after implementation of a comprehensive smoke-free law. Consistent with the findings of similar studies conducted elsewhere,2-4 the rate of AMI admissions decreased by 22% after the law was implemented. Whether this result is directly attributable to a reduction in SHS, less smoking by those who are active smokers or some combination is less apparent. However, the bottom line result leads us to the conclusion that implementation of comprehensive smoke-free policy results in a population-wide improvement in cardiovascular health at minimal cost.26
What this paper adds.
This research study is the first of this type conducted at the national level in a middle-income country in Latin America to examine trends in AMI hospital admissions associated with the implementation of a 100% smoke-free policy.
Acknowledgements
We thank Laura Roballo, Hugo Senra, Osvaldo Davyt, Olga Araújo and Amelia Correa from the CIET team for their contribution to the development of the study. We also thank the support from the Ministry of Health of Uruguay, the Uruguayan Society of Cardiology, the FEMI (Uruguayan Medical Federation) and the National Fund of Resources. Special thanks to Cheryl Rivard from the Survey Research and Data Acquisition Resource at Roswell Park Cancer Institute who contributed in performing statistical analysis.
Funding This research was funded by the Flight Attendant Medical Research Institute and the program project grant P01 CA138389 ‘Effectiveness of Tobacco Control Policies in High vs. Low Income Countries’ to Roswell Park Cancer Institute. ES and EB received funding from grant number 104399-1 of the Institute for Development Research Centre of Canada and a subsidy for independent research WS353475 by Pfizer Foundation of the United States. SAG was supported by the US National Cancer Institute (grant CA-61021). The funding agencies played no role in the conduct of the research or preparation of the manuscript.
APPENDIX 1
Participating centres and investigators
AMECOM: Frank Torres; AMEDRIN: Hugo Pini; Asociación Española: Edgardo Sandoya, Cristina Panizza; Asociación Médica de San José: MiriamÁlvarez, Fanny Bassignani; CAMDEL: Xavier Camps, María de losÁngeles González; CAMEDUR: Carlos Temperán, Yamandú Fernández; CAMOC: Dardo González, Osvaldo Davyt; CAMS Mercedes: Elbio Altieri; Casa de Galicia: Omar Montes de Oca, Osvaldo D’Alessandro; CASMU: Mónica Rigby; COMECA: Raúl Pereira, Carlos Pan; COMEFLO: Rafael Altieri, Mayra Larrauri; COMEPA: Mario Rodríguez Verde; CRAME: Edgardo Núñez; CRAMI: Pedro Banchero; GREMEDA: Enrique Dieste, Mónica Forastiero; Hospital Británico: Gabriel Vanerio; Hospital Central de las Fuerzas Armadas: Néstor Zefferino, Andrea Martins; Hospital de Clínicas: Alejandro Cuesta, Nicolás Blanchet,Álvaro Pérez; Hospital Evangélico: Pedro Amonte, Sandra Saratsola, Teodora Cabrera; Hospital de Florida: Julio Pontet; Hospital de Las Piedras: Silvia Ramón, Raúl Cuello; Hospital Maciel: José Patritti, Andrés Marino, Sebastián Massaferro; Hospital de Maldonado: Edgardo Núñez; Hospital de Minas: Xavier Camps, María de losÁngeles González; Hospital Pasteur: Beatriz Murguía; Hospital Policial: Jorge Gerez, Pamela Enrique, Gabriela Bello; Hospital de Trinidad: Rafael Altieri, Mayra Larrauri; MSP Artigas: Enrique Dieste, Mónica Forastiero; MSP Durazno: Carlos Temperán; MSP Mercedes: Elbio Altieri; MSP San José: Ana de los Santos; MSP Salto: Néstor Campos, Diego Tambucho, MUCAM: Enrique Spera, Judith Santos; ORAMECO: Walter Finozzi, Virginia Rossi; Sanatorio IMPASA: Fernando Kuster, Adriana Rodríguez, Olga Araújo; Sociedad Médico Quirúrgica de Salto: Néstor Campos, Diego Tambucho.
Footnotes
Contributors EMS initiated the collaborative project, designed data collection tools, monitored data collection, analysed the data and drafted and revised the paper. He is guarantor. ES implemented the study in Uruguay, monitored data collection, designed data collection tools, cleaned and analysed the data and drafted and revised the paper. AH wrote the statistical analysis plan, analysed the data and revised the draft paper. EB implemented the study in Uruguay, monitored data collection and revised the draft paper. SAG wrote the statistical analysis plan, analysed the data and revised the draft paper. KMC analysed the data and revised the draft paper.
Competing interests None.
Ethics approval Ethics approval was approved by Office of Research Subject Protection at Roswell Park Cancer Institute in Buffalo, New York, and at the School of Medicine, University of the Republic in Montevideo, Uruguay.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Sebrie EM, Schoj V, Glantz SA. Smokefree environments in Latin America: on the road to real change? Prev Control. 2008;3:21–35. doi: 10.1016/j.precon.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis. J Am Coll Cardiol. 2009;54:1249–55. doi: 10.1016/j.jacc.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 3.Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation. 2009;120:137–39. doi: 10.1161/CIRCULATIONAHA.109.870691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackay DF, Irfan MO, Haw S, et al. Meta-analysis of the effect of comprehensive smoke-free legislation on acute coronary events. Heart. 2010;96:1525–30. doi: 10.1136/hrt.2010.199026. [DOI] [PubMed] [Google Scholar]
- 5.Ferrante D, Linetzky B, Virgolini M, et al. Reduction in hospital admissions for acute coronary syndrome after the successful implementation of 100% smoke-free legislation in Argentina: a comparison with partial smoking restrictions. Tob Control. doi: 10.1136/tc.2010.042325. Published Online First: 20 May 2011. [DOI] [PubMed] [Google Scholar]
- 6.Hyland A, Travers MJ, Dresler C, et al. A 32-country comparison of tobacco smoke derived particle levels in indoor public places. Tob Control. 2008;17:159–65. doi: 10.1136/tc.2007.020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine of the National Academies . Secondhand smoke exposure and cardiovascular effects: Making sense of the evidence. Institute of Medicine of the National Academies; Washington, DC: 2009. [PubMed] [Google Scholar]
- 8.Glantz S, Gonzalez M. Effective tobacco control is key to rapid progress in reduction of non-communicable diseases. Lancet. doi: 10.1016/S0140-6736(11)60615-6. Published Online First: 28 September 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 2004;328:977–80. doi: 10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartecchi C, Alsever RN, Nevin-Woods C, et al. Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation. 2006;114:1490–6. doi: 10.1161/CIRCULATIONAHA.106.615245. [DOI] [PubMed] [Google Scholar]
- 11.Juster HR, Loomis BR, Hinman TM, et al. Declines in hospital admissions for acute myocardial infarction in New York state after implementation of a comprehensive smoking ban. Am J Public Health. 2007;97:2035–9. doi: 10.2105/AJPH.2006.099994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seo DC, Torabi MR. Reduced admissions for acute myocardial infarction associated with a public smoking ban: matched controlled study. J Drug Educ. 2007;37:217–26. doi: 10.2190/DE.37.3.a. [DOI] [PubMed] [Google Scholar]
- 13.Khuder SA, Milz S, Jordan T, et al. The impact of a smoking ban on hospital admissions for coronary heart disease. Prev Med. 2007;45:3–8. doi: 10.1016/j.ypmed.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Lemstra M, Neudorf C, Opondo J. Implications of a public smoking ban. Can J Public Health. 2008;99:62–5. doi: 10.1007/BF03403743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barone-Adesi F, Vizzini L, Merletti F, et al. Short-term effects of Italian smoking regulation on rates of hospital admission for acute myocardial infarction. Eur Heart J. 2006;27:2468–72. doi: 10.1093/eurheartj/ehl201. [DOI] [PubMed] [Google Scholar]
- 16.Cesaroni G, Forastiere F, Agabiti N, et al. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation. 2008;117:1183–8. doi: 10.1161/CIRCULATIONAHA.107.729889. [DOI] [PubMed] [Google Scholar]
- 17.Vasselli S, Papini P, Gaelone D, et al. Reduction incidence of myocardial infarction associated with a national legislative ban on smoking. Minerva Cardioangiol. 2008;56:197–203. [PubMed] [Google Scholar]
- 18.Pell JP, Haw S, Cobbe S, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359:482–91. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 19.Sims M, Maxwell R, Bauld L, et al. Short term impact of smoke-free legislation in England: retrospective analysis of hospital admissions for myocardial infarction. BMJ. 2010;340:c2161. doi: 10.1136/bmj.c2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blanco-Marquizo A, Goja B, Peruga A, et al. Reduction of secondhand tobacco smoke in public places following national smoke-free legislation in Uruguay. Tob Control. 2010;19:231–4. doi: 10.1136/tc.2009.034769. [DOI] [PubMed] [Google Scholar]
- 21.Thrasher JF, Boado M, Sebrie EM, et al. Smoke-free policies and the social acceptability of smoking in Uruguay and Mexico: findings from the international tobacco control policy evaluation project. Nicotine Tob Res. 2009;11:591–9. doi: 10.1093/ntr/ntp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.University of Waterloo. Universidad de la República. Centro de Investigación para la Epidemia del Tabaquismo. University of South Carolina. Roswell Park Cancer Institute . ITC Uruguay Survey Summary Waterloo. University of Waterloo, Universidad de la República, Centro de Investigación para la Epidemia del Tabaquismo, University of South Carolina, Roswell Park Cancer Institute; Ontario, Canada: 2010. [Google Scholar]
- 23.World Health Organization . CDC Glob Adult Tob Surv (GATS) Fact sheet Uruguay 2009. World Health Organization; 2010. [Google Scholar]
- 24.Sindicato Medico del Uruguay [Medical Union of Uruguay] Informe de la comision de tabaquismo del SMU: Tabaquismo en Uruguay. Sindicato Medico del Uruguay [Medical Union of Uruguay]; Montevideo: 2010. [Google Scholar]
- 25.World Health Organization . CDC Glob Youth Tob Surv (GYTS) Fact sheet Uruguay 2007. World Health Organization; 2007. [Google Scholar]
- 26.International Agency for Research on Cancer, WHO . IARC handbooks cancer prevention, tobacco control, Evaluating the Effectiveness of Smoke-free Policies. Vol. 13. Lyon; France: IARC: 2009. [Google Scholar]


