Abstract
This study tested the efficacy of two school-based programs for prevention of body weight/fat gain in comparison to a control group, in all participants and in overweight children. The Louisiana (LA) Health study utilized a longitudinal, cluster randomized 3-arm controlled design, with 28 months of follow-up. Children (N=2060; M age = 10.5 years, SD = 1.2) from rural communities in Grades 4 to 6 participated in the study. 17 school clusters (M = 123 children/cluster) were randomly assigned to one of three prevention arms: 1) Primary Prevention (PP), an environmental modification program, 2) Primary + Secondary Prevention (PP+SP), the environmental program with an added classroom and internet education component, or 3) Control (C). Primary outcomes were changes in percent body fat and body mass index z scores. Secondary outcomes were changes in behaviors related to energy balance. Comparisons of PP, PP+SP, and C on changes in body fat and BMI z scores found no differences. PP and PP+SP study arms were combined to create an environmental modification arm (EM). Relative to C, EM decreased body fat for boys (−1.7% ± 0.38% versus −0.14% ± 0.69%) and attenuated fat gain for girls (2.9% ± 0.22% versus 3.93% ± 0.37%), but standardized effect sizes were relatively small (< 0.30). In conclusion, this school-based environmental modification programs had modest beneficial effects on changes in percent body fat. Addition of a classroom/internet program to the environmental program did not enhance weight/fat gain prevention, but did impact physical activity and social support in overweight children.
Over the past 20 years, the prevalence of childhood and adult obesity has increased in industrialized societies (1, 2). Obesity is associated with increased morbidity and mortality (3), is difficult to treat (4), and is associated with costly medical conditions (5). Hence, there is considerable need for effective methods to prevent obesity (6), and because obese children and adolescents tend to become obese adults (7), it is logical that preventive efforts target inappropriate weight gain in children and young adolescents (8).
Many obesity prevention programs have utilized environmental modifications in schools, to improve healthy nutrition, increase physical activity, and reduce sedentary behavior (9, 10). This approach is often conceptualized as a type of universal primary prevention, where all children are equally exposed to the intervention (11). In contrast, secondary prevention programs identify and target affected individuals (11). Secondary prevention has been viewed as impractical in non-clinical settings, e.g., schools, due to the potential stigmatization of overweight children and the amount of time and resources required for individual treatment. For the LA Health project, we developed a method for delivering secondary prevention in the school setting in the context of a primary prevention program so that overweight children (defined as BMI percentile ≥ 85) would not be “singled out” (12). By combining a classroom-based approach with environmental modifications of the school we created an approach that is conceptually similar to “multi-level or integrated” interventions that have recently been advocated as a means to develop more powerful approaches for the prevention and treatment of childhood obesity (13). Furthermore, the LA Health project selectively recruited students from rural communities (12). Lutfiyya et al (14) identified rural residency as a risk factor for obesity and called for obesity prevention research on this at-risk population. To our knowledge, the LA Health study is the first controlled study of school-based obesity prevention in rural children.
The study was designed to test the efficacy of a Primary Prevention program (PP) and a combination of PP and a Secondary Prevention (SP) program in comparison to a Control (C) group for prevention of weight/fat gain in the entire sample and overweight children. The PP intervention delivered a school-based obesity prevention program that modified the school environment (12). PP+SP added a classroom/Internet component to the environmental modification program (12). PP+SP was conceptualized as adding additional education and social support for changing behaviors related to energy balance (10, 12, 15), especially in overweight children. PP and PP+SP included the environmental modification (EM) program and the study was designed to test the efficacy of the EM program in comparison to C. The primary endpoints were changes (over 28 months) in percent body fat and body mass index (BMI) z scores. Primary aims of the LA Health study were to test the hypotheses that: 1) PP and PP+SP were more effective for weight/fat gain prevention than C in the entire study cohort, 2) EM was more effective than C for weight/fat gain prevention in the entire study cohort, and 3) PP+SP was more effective for weight/fat loss in comparison to PP and C in overweight children. Secondary aims were to test hypotheses related to changes in behaviors related to energy balance: 1) PP and PP+SP were more effective for behavior change than C in the entire study cohort, 2) EM was more effective than C for behavior change in the entire study cohort, and 3) PP+SP was more effective for behavior change in comparison to PP and C in overweight children.
Materials/Subjects and Methods
Participants
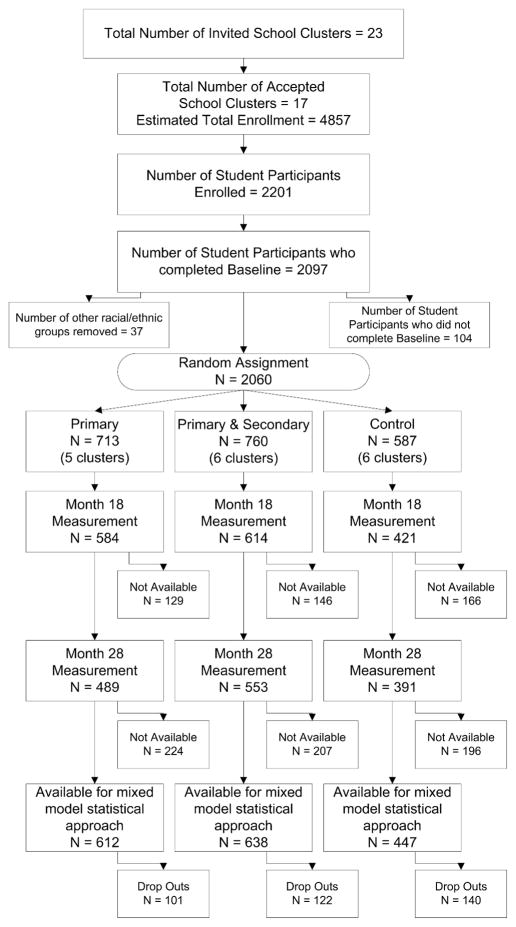
Williamson et al (12) described the recruitment of schools and participants. The LA Health study was approved by an Institutional Review Board. The parents of all child volunteers provided written informed consent and all child volunteers provided written assent to participate in the study. Figure 1 summarizes the flow of events starting with the number of school clusters that were considered for inclusion in the study to the number of children who were available for measurement at the end of the study (Month 28). A cohort of 2097 children enrolled in Grades 4–6 in 17 school systems were measured at baseline (12). Schools were grouped to create 17 school clusters, each an exclusive set of elementary schools and the middle or junior high schools into which they fed. After initiating the study, no attrition at the level of school or school cluster occurred. These 17 school clusters were randomly assigned to one of three arms: 1) PP (5 clusters), 2) PP+SP (6 clusters), or 3) C (6 clusters). In order to form two racial groups (for statistical analyses), we censored 37 (1.8% of the study cohort) children who reported race other than white/non-Hispanic, or African-American. Table 1 summarizes the resulting number and baseline characteristics of the children in the total cohort and in each treatment arm. At the end of 28 months, 363 children (17.6% of the baseline sample) were unavailable for follow-up measurement at Month 18 and/or 28. The demographic characteristics of the students who were unavailable for measurements at Months 18 and/or 28 did not differ from those who were available (p values > 0.25).
Figure 1.
CONSORT flow chart that illustrates the recruitment, random assignment, and retention of participants in the LA Health study. Recruitment of schools was described in greater detail by Williamson et al. (12) Six school clusters declined to participate in the study. The decisions by the school administrators of these six clusters were unique to each school system, but none refused to participate because the focus of the project was healthy weight, eating, and activity.
Table 1.
Baseline characteristics of the participants in the study cohort.
| Primary | Primary +Secondary | Control | Total Sample | |||||
|---|---|---|---|---|---|---|---|---|
| N | 713 | 760 | 587 | 2060 | ||||
| n | % | n | % | N | % | n | % | |
| Gender | ||||||||
| Female | 419 | 58.8 | 435 | 57.2 | 352 | 60.0 | 1206 | 58.5 |
| Male | 294 | 41.2 | 325 | 42.8 | 235 | 40.0 | 854 | 41.5 |
| Race | ||||||||
| White | 264 | 37.0 | 229 | 30.1 | 157 | 26.8 | 650 | 31.6 |
| African-American | 449 | 63.0 | 531 | 69.9 | 430 | 73.2 | 1410 | 68.4 |
| BMI | ||||||||
| Underweight/Normal | 369 | 51.7 | 442 | 58.2 | 329 | 56.0 | 1140 | 55.3 |
| Overweight/Obese | 344 | 48.3 | 318 | 41.8 | 258 | 44.0 | 920 | 44.7 |
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |||||
| Age | 10.5 (1.2 ) | 10.5 (1.2 ) | 10.6 (1.2 ) | 10.5 (1.2 ) | ||||
| BMI percentile | 70.3 (30.4) | 68.4 (29.3) | 70.6 (28.3) | 69.7 (29.5) | ||||
| BMI z score | 0.83 (1.22) | 0.71 (1.13) | 0.82 (1.12) | 0.78 (1.16) | ||||
| Body fat percent | 26.4 (11.9) | 24.4 (11.1) | 25.1 (11.5) | 25.3 (11.5) | ||||
Information on the Participating Schools
The actual number of schools that participated in the study varied over the three academic years due to changes in grade levels of the participants, e.g., in Year 1, 33 schools participated and in Year 3, 39 schools participated. At baseline, one cluster had 4 schools, four clusters had 3 schools, five clusters had 2 schools, and seven clusters had only 1 school. As shown in Figure 1, rate of enrollment was 2201 out of 4857 children in all schools (45.3% enrollment rate).
Outcome Assessment Strategy
Baseline assessment was conducted after the completion of recruitment and prior to randomization of schools to the intervention arms (Fall 2006). The remaining assessments occurred at the end of school in Years 2 (2008, after 18 months of intervention; M18) and 3 (2009, after 28 months of intervention; M28). Assessments were scheduled for two school clusters per week and measurements were conducted by two independent assessment teams who traveled together. At baseline, height, weight, and percent body fat were measured for 2060 white and African-American children; at M18, these measures were obtained for 1613 children and at M28, 1429 children were assessed for primary endpoints. Questionnaire measures (SAPAC and DSS) were obtained on > 99% of available children at each measurement period. At baseline, 97.8% of the volunteers were available for measurement of food intake using digital photography; at M18 (93.8%) and at M28 (87.8%) food intake was measured for most of the available children.
Measurement of Outcomes
Primary endpoints were changes in percent body fat and BMI z scores. Secondary endpoints were changes in behaviors related to energy balance: dietary intake, physical activity, and sedentary behavior. The order of assessment was randomly assigned for each school cluster prior to the baseline assessment, and this schedule was followed for the other two assessment periods, with minor deviations. Each assessment period required an average of 15 weeks (range = 14 to 16 weeks).
Primary Outcome Measures
Body fat
We measured body weight and impedance using bare footed participants on the Tanita Body Composition Analyzer (model TBF-310) and automatically recorded body fat and fat-free mass using a laptop computer. Prior to body impedance measurement, children did not fast and were not provided with specific instructions related to hydration. In children, estimates of body fat using body impedance are within 2% of DXA estimates of percent body fat and are very stable (16).
Body Mass Index z scores
Height and weight of each child were measured, in normal school clothing, without shoes and socks. Height was measured using a stadiometer. Weight was measured using the scale of the Tanita TBF 310. Height and weight were converted to body mass index (kg/m2) and, using the 2003 NHANES database, BMI was converted to z scores based on gender and age, an approach that has been used in studies of changes in body weight in growing children (17).
Measures of Behavior Related to Energy Balance
Digital photography of food selections and food intake
On three consecutive days, the digital photography method was used to measure food selections and food intake of students enrolled in the study. At lunch, foods selected by the students prior to eating and after eating were photographed using two (Sony DCR-TRV22) digital video cameras. One camera was used to photograph incoming trays (food selection), and the second camera was used for photographing outgoing trays (plate waste). Differences between food selections and plate waste defined food intake. Digital photographs of the reference portion, food selection, and plate waste for test meals were captured and incorporated into a computer application designed for estimation of food portions in digital photographs. Methods used in previous studies with adults (18) and children (19) were employed. These studies (18, 19) have reported that the methods are reliable, accurate, and sensitive to treatment effects. Additional details about these methods and results can be found in the online supplement.
Self-reported physical activity
Using the Self-Administered Physical Activity Checklist (SAPAC), children reported the number of hours they spent in physical activity and sedentary activities before, during, and after school (20). This self-report measure of physical activity has been correlated with measures of exercise intensity and objective measures of activity using accelerometers (20). The LA Health study included a sub-study (n = 275 at baseline) using accelerometers to measure duration of different levels of physical activity and sedentary behavior. This sub-study* found weak and inconsistent correlations between measures of physical activity and sedentary behavior measured by the SAPAC, when correlated with similar measures from accelerometers. These findings indicate that the SAPAC and accelerometers were measuring different aspects of physical activity and sedentary behavior.
Social Support from Teachers
We hypothesized that PP and/or PP+SP would result in higher levels of perceived social support from teachers for behavior change (12). To assess this impact, we selected the Children’s Dietary Social Support scale (DSS) (21). The DSS is a self-report measure of perceived social support for healthy dietary choices. The scale assesses support from family, friends, and teachers. Satisfactory internal consistency and concurrent validity as a measure of social support for diet-related behavior have been reported (21). We only report on changes in teacher support in this paper. Estimates of internal consistency (Coefficient alpha) were satisfactory at all three measurements (baseline = 0.73, M18 = 0.79, M28 = 0.82).
Socio-demographic Variables
The age, sex, and race of each child were self-reported by a parent or guardian of the child who provided written consent to participate in the study. Age of the child was verified from school records. Enrollment in the free or reduced-cost lunch program was used as an indicator of socioeconomic status (22). Based on data from the school lunch program, 77.0% of the participants were classified as low SES, 7.5% were classified as low to moderate SES, and 15.4% were classified as moderate to high SES. For purposes of comparison, 81.7% of the total student population in the 33 schools at baseline was classified as low SES.
Prevention Programs
As noted earlier, school clusters were randomly assigned to one of three study arms: PP, PP+SP, and C. The prevention programs have been described in other papers (12, 23). Program materials for PP and SP may be obtained at http://www.pbrc.edu. The names of the two prevention programs were derived from the distinction between universal primary prevention and targeted secondary prevention (12). We recognize that these names (Primary and Secondary Prevention) may not be universally accepted as appropriate, but we maintain the use of these names to remain consistent across publications related to the LA Health study (12, 23). The term secondary prevention was selected as the name for the classroom/Internet program since it instructed overweight children (at baseline) to lose body weight/fat (12, 23). Non-overweight children exposed to the program were instructed to maintain current body weight/fat.
Primary Prevention
The Primary Prevention program modified the school environment to promote healthy nutrition and physical activity with three primary objectives: 1) modify environmental cues related to healthy eating and activity, 2) modify the cafeteria food service program, and 3) modify the physical education programs as described in the SPARK study (24) and to reduce sedentary behavior (25). The program used an environmental approach that was developed and tested in the Wise Mind study (19). Dietary and physical activity goals of the program were guided by recommendations from the American Academy of Pediatrics (26). Dietary goals included: five fruits and vegetables per day, < 30% of dietary energy from total fat, < 10% of dietary energy from saturated fat, and 20 to 30 grams of fiber/day. The contents of vending machines were modified using this guideline--at least 50% of foods available in vending machines were required to meet all of the following dietary criteria: 1) ≤ 150 kcal, 2) < 35 total kcal from fat, 3) < 10% of total fat from saturated fat, 4) ≤ 30 g of sugar per serving, and 5) ≤ 360 mg of sodium per serving. Activity goals were: 1) 60 minutes of moderate to vigorous activity per day and 2) < two hours per day of television viewing and video game play.
Primary + Secondary prevention
This intervention arm combined SP (23) with PP (identical to the Primary Prevention program described above). SP employed a classroom instruction component combined with an internet-based approach similar to the interventions that were developed and tested in the HIPTeens study (27) and other health behavior change studies in children (15). Internet-based obesity interventions have been associated with reduced utilization over time (28). To overcome this limitation, the internet intervention of this study was delivered as part of regular classroom instruction, combined with synchronous (online) internet counseling and asynchronous (email) communications for children and their parents. The website was programmed to recognize whether a participant was overweight or obese at baseline and slightly different programs were presented to overweight and non-overweight children (12, 23), which was effective for minimizing the potential for stigmatizing overweight children.
No-Intervention Control
The control group for the RCT received none of the prevention components that are hypothesized to yield weight gain prevention.
Delivery of the Programs Associated with the Three Arms
Integrity of the delivery of the prevention programs was evaluated using assessment methods (questionnaires and observation procedures for the school environment, teachers, and cafeteria staff) that measured different components of the three intervention arms (29). These process measures, developed specifically for the LA Health study, were found to be reliable (Coefficient Alphas ranged from 0.60 to 0.86, indicating satisfactory internal consistency) and valid (inter-rater agreement ranged from 0.75 to 0.94 for content specificity of the items of each scale). The results indicated that exposure to the different intervention components associated with PP+SP, PP, and C study arms was rated by school and study personnel as yielding interventions that were unique (29).
Statistical Power Analysis
Statistical power analysis (12; power = 0.85) indicated that with 17 clusters, an average of 98 students per cluster were required at the end of the study to detect relatively small differences in measures of adiposity (e.g., < 0.12 for BMI z scores and < 1.2% differences in body fat percent between intervention arms for boys and girls. Recruitment of participants was based upon an assumption of 25% attrition rate for statistical analyses (12). The actual attrition rate was 17.5% and the effect sizes that were observed were consistent with the relatively small changes that were anticipated with the power analyses (12).
Statistical Methods
The seventeen school clusters were randomized to one of the three intervention arms following baseline data collection. A single-stage, mixed model statistical strategy was used to analyze the findings for students with baseline measurement and at least one (of two) follow-up measurements. This approach excluded children who were only available for baseline measurement (17.5% of the baseline cohort were unavailable for measurement primarily due to movement by the family out of the school district). The results were compared with results from a last observation carried forward (LOCF) intent-to-treat approach to evaluate the reliability of the findings and the same results were found. All primary and secondary endpoints reported in this paper were collected at the individual level. Changes from the baseline value to the follow-up measurements were utilized as the response variable and a mixed-model analysis was used to evaluate the intervention effect, with baseline values entered as covariates. The mixed model analyses controlled for the random effect of school clusters within intervention arms and intra-class correlations pertaining to the effects of school clusters are reported. For primary endpoints (percent body fat and BMI z scores), separate analyses for boys and girls were conducted since previous research on baseline data had found different distributions of percent body fat and BMI z scores for boys and girls (30). Race was a stratification factor for models analyzing primary endpoints. Thus, the basic statistical model for primary endpoints used a Group X Race X Time design. The basic statistical model for behaviors related to energy balance and for social support from teachers used a Group X Time design, co-varying race and sex. The indicator of socioeconomic status, (free, partially paid, or fully paid lunch status) was considered for inclusion in the statistical models. This measure was not entered, however, because it was significantly associated with minority status (χ2 = 292, p = 0.001; Contingency Coefficient = 0.35) and the confounding of the two variables could not be corrected. Results were interpreted using information derived from null hypothesis testing and effect sizes, as recommended by Cohen (31, 32) and Cortina and Landis (33). Standardized effect sizes (ES), similar to Cohen’s d for cluster randomized studies (34), are reported for each outcome measure at M28 and as an average across M18 and M28. Effect sizes were interpreted using the guidelines suggested by Cohen (31): small = 0.20, medium = 0.50, and large = 0.80. Focused tests of significance (35) were used in comparisons of two intervention arms. For null hypothesis testing involving two arms, alpha was set at p < 0.05. For effects involving three arms, alpha was adjusted to p < 0.02.
Results
Baseline Characteristics
Table 1 summarizes the characteristics of the participants in the study cohort and in the three prevention programs at baseline. The study cohort was composed primarily of African-American children (68.4%) and a majority (58.5%) of the sample was girls. For comparisons to baseline data in Table 1, the average age at the end of the study was 12.9 years (standard deviation: 1.2 years); the percent girls was 59%; 31.5% of the children were white; and mean BMI percentile score was 70.4 (SD = 28.2). Findings pertaining to baseline adiposity measures have been described by Williamson et al. (30).
Changes in Percent Body Fat and Weight
Comparison of changes in percent body fat in PP, PP+SP, and C indicated no differences for boys (F = 2.47, df = 2,14, p = .12) or girls (F = 2.68, df = 2,14, p = .11). Comparison of changes in BMI z scores in PP versus PP+SP indicated no differences for boys (F =.42, df =2,14, p =.67) or girls (F =2.30, df =2,14, p =.14). Table 2 summarizes these findings. ESs were generally small (< 0.35).
Table 2.
Changes in percent body fat and BMI z over time as a function of three prevention arms.
| Group | Adjusted Changes: M18 | Adjusted Changes: M28 | Overall Changes | F(arm) (2, 14) | Effect Size
|
||||
|---|---|---|---|---|---|---|---|---|---|
| Pair | M28 | Average | |||||||
| %Body Fat | Boys | PP | −0.86(0.63) | −1.7(0.66) | −1.3(0.59) | 2.47 | PP vs PP+PS | 0.09 | 0.11 |
| PP+PS | −1.8(0.58) | −2.3(0.59) | −2.0(0.54) | P vs C | −0.20 | −0.17 | |||
| C | 0.09(0.73) | −0.30(0.75) | −0.11(0.68) | PP+PS vs C | −0.33 | −0.31 | |||
| Girls | PP | 1.9(0.41) | 3.7(0.42) | 2.8(0.34) | 2.68 | PP vs PP+PS | −0.04 | −0.04 | |
| PP+PS | 2.1(0.39) | 3.9(0.39) | 3.0(0.32) | P vs C | −0.23 | −0.21 | |||
| C | 3.0(0.46) | 4.9(0.46) | 3.9(0.39) | PP+PS vs C | −0.21 | −0.19 | |||
| BMI z | Boys | PP | 0.029(0.035) | 0.017(0.037) | 0.022(0.033) | 0.42 | PP vs PP+PS | −0.03 | 0.03 |
| PP+PS | −0.008(0.032) | 0.028(0.033) | 0.01(0.03) | P vs C | −0.10 | −0.07 | |||
| C | 0.050(0.043) | 0.060(0.045) | 0.055(0.04) | PP+PS vs C | −0.07 | −0.10 | |||
| Girls | PP | 0.012(0.022) | 0.022(0.023) | 0.017(0.021) | 2.30 | PP vs PP+PS | −0.15 | −0.12 | |
| PP+PS | 0.051(0.022) | 0.088(0.023) | 0.069(0.021) | P vs C | −0.15 | −0.13 | |||
| C | 0.063(0.027) | 0.088(0.027) | 0.076(0.025) | PP+PS vs C | 0.00 | −0.02 | |||
Note: PP = Primary Prevention, PP+PS = Primary + Secondary Prevention, C = Control.
Changes are adjusted means (SE).
F values are arm main effects. Reported F values were not statistically significant (P > .05); therefore post-hoc tests were not conducted.
E.S.: Effect size is the standardized mean difference δT appropriate for cluster randomized designs (34).
Intra-class correlations ranged from 0.0005 to 0.026.
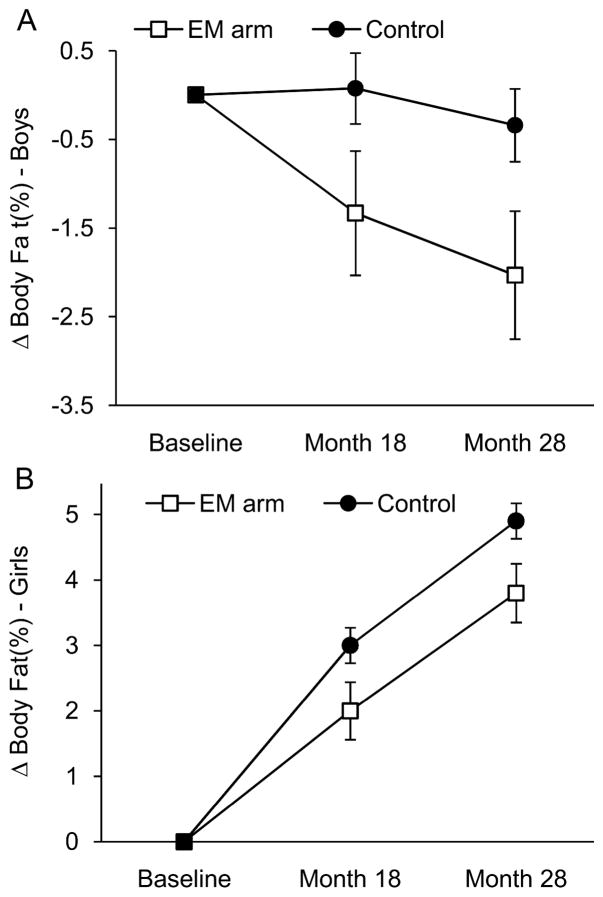
For changes in percent body fat in boys, main effects for EM in comparison to C approached statistical significance (F = 4.26, df = 1,15, p = 0.057). The LOCF analysis confirmed the significance of this null hypothesis test, F (1,15) = 4.55, p < 0.05. For girls, the difference between EM and C was also statistically significant (F= 5.64, df = 1,15, p = 0.03). The effects of EM on percent body fat are illustrated in Figure 2A and B. Table 3 summarizes the findings for arm main effects related to changes in percent body fat and BMI z scores. Mean reduction in percent body fat for boys in the EM arm was −1.7% ± 0.38% (p = 0.0004); whereas in C, mean change was −0.14% ± 0.69%, and did not differ from baseline (p = 0.84). For girls, percent body fat increased over time, regardless of prevention arm (F= 41.84, df = 1,15, p < 0.0001). The average change in percent body fat for girls in the EM arm was 2.9% ± 0.22%; for girls in C, mean increased percent body fat was 3.93% ± 0.37%.
Figure 2.
Changes in percent body fat over time as a function of intervention arm (Abbreviations: EM arm = Primary Prevention combined with Primary + Secondary Prevention). Panel A depicts changes for boys and panel B depicts changes for girls.
Table 3.
Changes in percent body fat and BMI z over time as a function of EM versus C.
| Group | Adjusted Change: M18 | Adjusted Change: M28 | Average Changes | EM vs C: M28
|
EM vs C: Average
|
||||
|---|---|---|---|---|---|---|---|---|---|
| Difference | E.S. | Difference | E.S. | ||||||
| %Body Fat | Boys | EM | −1.3(0.41) | −2.0(0.42) | −1.7(0.38) | −1.7 | −0.25 | −1.6* | −0.23 |
| C | 0.08(0.71) | −0.34(0.72) | −0.14(0.69) | ||||||
| Girls | EM | 2.0(0.27) | 3.8(0.27) | 2.9(0.22) | −0.9 | −0.27 | −1.0# | −0.23 | |
| C | 3.0(0.44) | 4.9(0.45) | 3.9(0.37) | ||||||
| BMI z | Boys | EM | 0.009(0.022) | 0.024(0.023) | 0.017(0.020) | −0.034 | −0.08 | −0.037 | −0.08 |
| C | 0.048(0.041) | 0.058(0.042) | 0.053(0.038) | ||||||
| Girls | EM | 0.030(0.023) | 0.053(0.024) | 0.042(0.015) | −0.035 | −0.08 | −0.034 | −0.08 | |
| C | 0.063(0.023) | 0.088(0.024) | 0.076(0.025) | ||||||
Note: EM arm = Primary Prevention combined with Primary + Secondary Prevention; C = Control.
Changes are adjusted means (SE).
Associated p value is .057;
associated p value is .031.
E.S.: Effect size is the standardized mean difference δT appropriate for cluster randomized designs (34).
Intra-class correlations ranged from 0.0005 to 0.02.
Changes in BMI z scores as a function of EM in comparison to the C were not observed for boys (F = 0.79, df = 1,15, p = 0.39). Also, no interaction effects involving intervention arms were found to be significant for boys (p values > .14). For girls, a significant interaction of study arm, race, and time was found (F = 6.85, df = 1,10, p = 0.03). Post-hoc tests found that at M28, only for white girls, the EM arm differed from the Control arm (p = 0.04). The interaction effect is shown in Figure 1 of the online supplement. At M28, mean BMI z change scores for white girls in EM (M = 0.04 ± 0.03) were lower than BMI z change scores for white girls in the Control arm (M = 0.17 ± 0.05; p = 0.04). Main arm effects for boys and girls are summarized in Table 3. ESs for changes in percent body fat and BMI z scores were generally small (−0.08 to −0.27).
Differential changes in percent body fat (Boys: F = 0.92, df = 2,14, p = 0.42; Girls: F = 1.99, df = 2,14, p = 0.17) or BMI z scores (Boys: F = 0.25, df = 2,14, p = 0.78; Girls (F = 0.93, df = 2,14, p = 0.42) of overweight children were not observed across the three study arms. ESs were generally small (−0.31 to 0.15). See Table 1 of the online supplement for details of these analyses.
Changes in Behaviors related to Energy Balance
Findings for comparisons of PP, PP+SP, and C for the entire sample are summarized in Table 4. No differences between PP+SP and PP and C were found for changes in food intake, physical activity, or sedentary behavior.
Table 4.
Changes in secondary outcome measures over time as a function of three prevention arms.
| Group | Adjusted Changes: M18 | Adjusted Changes: M28 | Overall Changes | F (arm) (2, 14) | Effect Size
|
|||
|---|---|---|---|---|---|---|---|---|
| Pair | M28 | Average | ||||||
| Total Energy Intake (kcal) | PP | −38.3(31.6) | −127(31.8) | −82.9(22.6) | 1.36 | PP vs PP+PS | −0.23 | −0.23 |
| PP+PS | 4.5(28.9) | −84.2(29.0) | −39.8(20.7) | P vs C | −0.39 | −0.23 | ||
| C | −24.1(29.6) | −50.4(29.8) | −37.3(21.3) | PP+PS vs C | −0.18 | −0.01 | ||
| Energy from Total Fat (kcal) | PP | −19.4(13.6) | −65.6(13.7) | −42.5(9.7) | 1.12 | PP vs PP+PS | −0.14 | −0.14 |
| PP+PS | −8.9(12.4) | −53.5(12.5) | −31.2(8.9) | P vs C | −0.49 | −0.22 | ||
| C | −23.6(12.7) | −21.8(12.8) | −22.7(8.9) | PP+PS vs C | −0.39 | −0.10 | ||
| Energy from Saturated Fat (kcal) | PP | −7.0(4.8) | −20.5(4.9) | −13.7(3.7) | 0.67 | PP vs PP+PS | −0.14 | −0.15 |
| PP+PS | −1.8(4.4) | −16.0(4.4) | −8.9(3.4) | P vs C | −0.34 | −0.16 | ||
| C | −7.6(4.5) | −9.3(4.5) | −8.4(3.4) | PP+PS vs C | −0.22 | −0.02 | ||
| Energy from Protein (kcal) | PP | −8.1(9.5) | −2.8(9.6) | −5.4(7.0) | 0.67 | PP vs PP+PS | −0.04 | −0.23 |
| PP+PS | 10.5(8.7) | −0.9(8.7) | 4.8(6.4) | P vs C | 0.02 | −0.05 | ||
| C | −2.0(8.8) | −4.0(8.8) | −3.0(6.4) | PP+PS vs C | 0.07 | 0.17 | ||
| Energy from Carbohydrate (kcal) | PP | −6.0(17.3) | −54.0(17.4) | −30.0(14.2) | 0.52 | PP vs PP+PS | −0.25 | −0.17 |
| PP+PS | 3.5(15.8) | −29.6(15.9) | −13.1(−1.0) | P vs C | −0.29 | −0.17 | ||
| C | −0.8(16.2) | −24.3(16.3) | −12.6(13.3) | PP+PS vs C | −0.05 | −0.00 | ||
| SAPAC: Physical Activity Time (min) | PP | −13.4(8.5) | −35.4(8.6) | −24.4(7.5) | 2.99 | PP vs PP+PS | −0.21 | −0.19 |
| PP+PS | 4.5(7.8) | −10.8(7.9) | −3.1(6.9) | P vs C | −0.02 | 0.00 | ||
| C | −14.5(9.1) | −32.8(9.2) | −23.6(8.2) | PP+PS vs C | 0.22 | 0.21 | ||
| SAPAC: Sedentary Behavior Time (min) | PP | −10.0(8.1) | −12.0(8.5) | −11.0(7.3) | 2.85 | PP vs PP+PS | 0.13 | 0.13 |
| PP+PS | −31.7(7.6) | −36.2(7.8) | −34.0(6.7) | P vs C | 0.09 | 0.05 | ||
| C | −11.8(9.7) | −27.0(9.9) | −19.4(8.9) | PP+PS vs C | −0.01 | −0.09 | ||
Note: PP = Primary Prevention, PP+PS = Primary + Secondary Prevention, C = Control.
Changes are adjusted means (SE).
F values are arm main effects. Reported F values are not statistically significant (P><.05); therefore no post-hoc tests were conducted.
E.S.: Effect size is the standardized mean difference δT appropriate for cluster randomized designs (34).
Intra-class correlations ranged from 0.15 to 0.38 for food intake data; and .05 for Physical Activity and .03 for Sedentary Behavior
In the comparisons of EM and C, a significant interaction of study arm and time was observed for changes in dietary fat intake (F = 4.86, df = 1,15, p = 0.04), illustrated in Figure 3. At M28, reductions in dietary fat intake in EM (M = −59.0 ± 9.0) were larger than those observed in C (M = 21.8 ± 12.4). Findings for arm effects are summarized in Table 2 of the online supplement; ES for total fat (−0.52) was medium in size at M28. ICCs for food intake data were relatively high (0.15 to 0.38) which indicates that food intake of students at a particular school was relatively highly correlated in comparison to the food intake of students at other schools.
Figure 3.
Changes in dietary fat intake over time as a function of intervention arm (Abbreviations: EM arm = Primary Prevention combined with Primary + Secondary Prevention).
Changes in self-reported physical activity and sedentary behavior (using the SAPAC) did not differ as a function of study arm (all p values > 0.05) and ESs were uniformly small (< 0.10). Summaries of these data can be seen in Table 2 of the online supplement.
The findings from analyses in overweight children are summarized in Table 5. Addition of SP to PP yielded maintenance of physical activity in comparison to the reductions of physical activity observed for the PP arm (F = 5.27, df = 2,14, p = 0.02). Similar findings were observed for sedentary behavior (F = 3.88, df = 2,14, p = 0.05), as illustrated in Figure 2 of the online supplement.
Table 5.
Changes in secondary outcome measures over time as a function of three prevention arms for students who were overweight at the baseline.
| Group | Adjusted Changes: M18 | Adjusted Changes: M28 | Overall Changes | F (arm) (2, 14) | Effect Size
|
|||
|---|---|---|---|---|---|---|---|---|
| Pair | M28 | Average | ||||||
| Total Energy Intake (kcal) | PP | −50.6(30.7) | −154.5(31.3) | −102.6(22.3) | 1.43 | PP vs PP+PS | −0.26 | −0.21 |
| PP+PS | −18.2(28.5) | −106.5(28.7) | −62.3(20.6) | P vs C | −0.50 | −0.26 | ||
| C | −47.9(30.4) | −58.7(30.5) | −53.3(22.2) | PP+PS vs C | −0.26 | −0.05 | ||
| Energy from Total Fat (kcal) | PP | −22.7(14.1) | −76.0(14.4) | −49.4(10.2) | 0.96 | PP vs PP+PS | −0.19 | −0.13 |
| PP+PS | −16.4(13.1) | −59.1(13.1) | −37.7(9.4) | P vs C | −0.42 | −0.21 | ||
| C | −35.7(13.8) | −23.8(13.8) | −29.8(10.0) | PP+PS vs C | −0.27 | −0.10 | ||
| Energy from Saturated Fat (kcal) | PP | −7.7(5.3) | −24.3(5.4) | −16.0(4.2) | 0.50 | PP vs PP+PS | −0.17 | −0.12 |
| PP+PS | −5.0(4.9) | −18.4(4.9) | −11.7(3.9) | P vs C | −0.43 | −0.16 | ||
| C | −11.5(5.1) | −9.4(5.1) | −10.5(4.0) | PP+PS vs C | −0.30 | −0.04 | ||
| Energy from Protein (kcal) | PP | −9.9(9.8) | −5.4(9.9) | −7.6(7.5) | 0.60 | PP vs PP+PS | −0.05 | −0.22 |
| PP+PS | 8.4(9.0) | −3.0(9.1) | 2.7(6.8) | P vs C | −0.01 | −0.05 | ||
| C | −6.0(9.4) | −4.9(9.4) | −5.4(7.1) | PP+PS vs C | −0.04 | −0.17 | ||
| Energy from Carbohydrate (kcal) | PP | −14.4(16.0) | −69.0(16.4) | −41.7(13.7) | 0.66 | PP vs PP+PS | −0.27 | −0.15 |
| PP+PS | −10.5(14.9) | −44.4(15.0) | −27.4(12.6) | P vs C | −0.38 | −0.22 | ||
| C | −8.8(16.0) | −31.7(16.0) | −20.2(13.4) | PP+PS vs C | −0.12 | −0.07 | ||
| SAPAC: Physical Activity Time (min) | PP | −19.1(7.5) | −40.3(7.7) | −29.7(5.9) | 5.27* | PP vs PP+PS | −0.22 | −0.22** |
| PP+PS | 5.9(7.2) | −14.6(7.3) | −4.3(5.6) | P vs C | −0.05 | −0.06 | ||
| C | −11.3(8.4) | −34.4(8.4) | −22.9(6.6) | PP+PS vs C | 0.19 | 0.19** | ||
| SAPAC: Sedentary Behavior (min) | PP | −12.8(9.1) | −25.9(9.6) | −19.3(7.8) | 3.88* | PP vs PP+PS | 0.12* | 0.16* |
| PP+PS | −47.5(9.0) | −48.0(9.5) | −47.7(7.7) | P vs C | 0.05 | 0.04 | ||
| C | −15.0(10.8) | −35.1(11.0) | −25.0(5.8) | PP+PS vs C | −0.08 | −0.14 | ||
Note: PP = Primary Prevention, PP+PS = Primary + Secondary Prevention; C = Control
Changes are adjusted means (SE).
F values are arm main effects. Reported F values are all non-significant (P < .05). Post-doc comparisons that were statistically significant are marked:
P < .05;
P < .02.
E.S.: Effect size is the standardized mean difference δT appropriate for cluster randomized designs (34).
Intra-class correlations ranged from 0.12 to 0.40 for food intake data; and were .01 for Physical Activity and .03 for Sedentary Behavior
Change in Perceived Social Support for Dietary Changes
PP+SP was associated with improved support from teachers for dietary changes in comparison to PP (ES at M28 = .34) and C (ES at M28 = .45) in the entire sample, F = 17.1, df = 2, 14, p=.0002. Similar findings were observed in overweight children; PP+SP in comparison to PP and C, was associated with improved social support from teachers F = 15.5, df = 2, 14, p=.0003. Figures 3A and 3B in the online supplement illustrate these effects.
Discussion
The primary finding of the LA Health study was that prevention arms that modified the school environment (EM) to promote healthy eating, increase physical activity, and decrease sedentary behavior were effective for reducing percent body fat in boys, attenuating percent body fat gain in girls, and preventing weight gain (as defined by BMI z scores) in white girls. Addition of the classroom/Internet (Secondary Prevention) program to the environmental modification (Primary Prevention) program had no significant effects on measures of adiposity, but was associated with better maintenance of physical activity and enhancement of teacher support for dietary changes in overweight children. These findings suggest that the classroom/Internet program may be most applicable to interventions that emphasize changes in physical activity of overweight children and enhancement of social support from teachers. Thus, we conclude that a classroom/Internet approach may affect some behavioral changes, but it did not provide additional changes in adiposity, when compared to the environmental modification program alone.
It is somewhat difficult to answer why the addition of the SP program did not have significant effects on measures of adiposity. Process measures (29) confirmed that the students were exposed to the internet and classroom components of SP and statistical power analyses indicated that the study was powered to find relatively small effects associated with each of the intervention arms. We can speculate, however. Other school-based prevention studies have reported changes in measures of physical activity and/or dietary behavior with no changes in measures of adiposity (9, 19), so it may be somewhat easier to change behaviors in comparison to body weight or fat. Changes in behavior may precede changes in body weight/fat. Also, it is possible that teachers were not able to implement the SP program with the intensity and consistency that is required to yield significant changes in body weight/fat in overweight or non-overweight children. Other possible explanations are: 1) parental involvement was not optimal, 2) 28 months of intervention may have been insufficient, and 3) recidivism during summer breaks may have weakened the results. Tests of these potential explanations are needed.
The LA Health study was one of only a few studies that included measures of percent body fat and BMI, which enables a comparison of these two endpoints as sensitive outcome measures in childhood obesity prevention studies. Examination of the standardized effect sizes associated with both primary outcome measures (see Table 3) suggest a slight advantage for sensitivity of change in percent body fat as opposed to changes in BMI z scores which measure changes in total body mass, as opposed to one component (body fat) of total body mass.
The LA Health study found modest evidence for prevention of weight/fat gain and improvement of healthy nutrition and physical activity through participation in a school-based intervention that targeted the entire student population. These findings are consistent with those recently reported by the HEALTHY study (36), which found modest beneficial effects of an environmental modification program on measures of body size and waist circumference. The LA Health study also found that the EM arm resulted in reduced intake of dietary fat, which is consistent with the results of several earlier studies (19, 37, 38, 39).
These findings should be interpreted in the context of the limitations of the study. The study cohort was not a representative sample of children in the U.S; the children were recruited from schools in rural areas of Louisiana with a majority from poor African-American families. The racial and ethnic diversity of the study cohort was limited to African-American and white/non-Hispanic children from Grades 4 to 6 in Year 1 and Grades 6 to 8 in Year 3. The study tested the efficacy of two types of obesity prevention programs and though they were labeled Primary and Secondary prevention, they should not be viewed as the only types of primary and secondary obesity prevention programs that could be developed and tested.
We conclude that the enthusiasm that might be generated by these modest positive findings should be tempered by the observation that results have been inconsistent across studies (9, 10) and that the overall results of this study indicated that the effect sizes were relatively small, even when beneficial effects were found, e.g., EM versus C for changes in percent body fat. Based upon these observations, we caution advocacy of untested school-based obesity prevention programs. Given the current evidence, we recommend that before widespread adoption of any school-based obesity prevention program, policy makers should insist that the program is properly evaluated using randomized controlled research methodology.
In summary, the EM program tested in the LA Health study yielded significant prevention of fat gain in boys and girls from rural communities, when compared to C. The addition of a secondary prevention program that utilized classroom instruction and an internet-based program yielded some additional changes in physical activity in overweight children and support from teachers for dietary changes. These behavioral changes did not yield additional reduction in adiposity or prevention of increased percent body fat. These findings, though positive, should be interpreted in the context of the relatively modest effect sizes attributable to the environmental intervention and the inconsistency of results across school-based obesity prevention studies (9, 10).
Supplementary Material
Acknowledgments
This project was supported by the National Institute for Child Health and Human Development of the National Institutes of Health (R01 HD048483) and the U.S. Department of Agriculture (58-6435-4-90). The clinical trial number for this project is: NCT00289315. In addition, this work was partially supported by the NORC Center Grant #1P30 DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by NIDDK, and C. Martin was supported by NIH grant K23 DK068052 (PI: C. Martin). We would like to express our appreciation to the schools, administrators, and students that participated in this obesity prevention study. Also, we acknowledge the support and assistance that we received from the Louisiana Board of Regents, the LA GEAR UP program, the Louisiana State Department of Education, and the Data and Safety Monitoring Board. Finally, we greatly appreciate the very hard work and dedication of the research staff of the LA Health study. Without the tremendous effort and support of all of these people, we could not have completed a study of this magnitude and scope.
Footnotes
Conflict of Interest
The authors disclose no conflicts of interest.
At baseline, no significant (p values > 0.05) correlations between SAPAC measures and measures of physical activity or sedentary behavior from accelerometers were found (r values < 0.10). At M18 and M28, the SAPAC measure of physical activity was significantly correlated with minutes of moderate to vigorous activity measured by accelerometers at M18 (r = 0.15) and at M28 (r = 0.23). The SAPAC measure of sedentary behavior was correlated (r = 0.16) with minutes of light activity measured by accelerometers at M18, but at M28, this correlation was not significant (r = 0.05, p > 0.05).
Clinicaltrials.gov Identifier: NCT00289315
References
- 1.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Rashid MN, Fuentes F, Touchon RC, Wehner PS. Obesity and the risk for cardiovascular disease. Prev Cardiol. 2003;6:42–47. doi: 10.1111/j.1520-037x.2003.01358.x. [DOI] [PubMed] [Google Scholar]
- 4.Wadden TA, Osei S. The treatment of obesity: An overview. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity treatment. Vol. 2002. New York: New York: 2002. pp. 229–248. [Google Scholar]
- 5.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 6.Kumanyika SK, Obarzanek E. Pathways to obesity prevention: report of a National Institutes of Health workshop. Obes Res. 2003;11:1263–1274. doi: 10.1038/oby.2003.172. [DOI] [PubMed] [Google Scholar]
- 7.Berkowitz RI, Stunkard AJ. Development of childhood obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. Vol. 2002. Guilford; New York: 2002. pp. 515–531. [Google Scholar]
- 8.Swinburn BA, de Silva-Sanigorski AM. Where to from here for preventing childhood obesity: an international perspective. Obesity (Silver Spring) 2010;18 (Suppl 1):S4–7. doi: 10.1038/oby.2009.424. [DOI] [PubMed] [Google Scholar]
- 9.Doak C, Heitmann BL, Summerbell C, Lissner L. Prevention of childhood obesity—what type of evidence should we consider relevant? Obesity Reviews. 2009;10:350–356. doi: 10.1111/j.1467-789X.2008.00550.x. [DOI] [PubMed] [Google Scholar]
- 10.DeBourdeaudhuij I, Cauwenberghe E, Spittaels H, et al. School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project. Obesity Reviews. 2011;12:205–216. doi: 10.1111/j.1467-789X.2009.00711.x. [DOI] [PubMed] [Google Scholar]
- 11.Zwiauer KF. Prevention and treatment of overweight and obesity in children and adolescents. Eur J Pediatr. 2000;159 (Suppl 1):S56–68. doi: 10.1007/pl00014367. [DOI] [PubMed] [Google Scholar]
- 12.Williamson DA, Champagne CM, Harsha D, et al. Louisiana (LA) health: design and methods for a childhood obesity prevention program in rural schools. Contemporary Clinical Trials. 2008;29:783–795. doi: 10.1016/j.cct.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epstein LH, Wrotniak BH. Future directions for pediatric obesity treatment. Obesity (Silver Spring) 2010;18 (Suppl 1):S8–12. doi: 10.1038/oby.2009.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lutfiyya MN, Lipsky MS, Wisdom-Behounek J, Inpanbutr-Martinkus M. Is rural residency a risk factor for overweight and obesity for U.S. children? Obesity (Silver Spring) 2007;15:2348–2356. doi: 10.1038/oby.2007.278. [DOI] [PubMed] [Google Scholar]
- 15.Crutzen R, de Nooijer J, Brouwer W, Oenema A, Brug J. Strategies to facilitate exposure to internet-delivered health behavior change interventions aimed at adolescents or young adults: A systematic review. Health Education & Behavior. 2011;38:49–62. doi: 10.1177/1090198110372878. [DOI] [PubMed] [Google Scholar]
- 16.Sung RY, Lau P, Yu CW, Lam PK, Nelson EA. Measurement of body fat using leg to leg bioimpedance. Arch Dis Child. 2001;85:263–267. doi: 10.1136/adc.85.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lumeng JC, Kaciroti N, Frisvold DE. Changes in body mass index z score over the course of the academic year among children attending Head Start. Acad Pediatr. 2010;10:179–186. doi: 10.1016/j.acap.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson DA, Allen HR, Martin PD, Alfonso AJ, Gerald B, Hunt A. Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Diet Assoc. 2003;103:1139–1145. doi: 10.1016/s0002-8223(03)00974-x. [DOI] [PubMed] [Google Scholar]
- 19.Williamson DA, Copeland AL, Anton SD, et al. Wise Mind project: a school-based environmental approach for preventing weight gain in children. Obesity (Silver Spring) 2007;15:906–917. doi: 10.1038/oby.2007.597. [DOI] [PubMed] [Google Scholar]
- 20.Sallis JF, Berry CC, Broyles SL, McKenzie TL, Nader PR. Variability and tracking of physical activity over 2 yr in young children. Med Sci Sports Exerc. 1995;27:1042–1049. doi: 10.1249/00005768-199507000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Parcel GS, Edmundson E, Perry CL, et al. Measurement of self-efficacy for diet-related behaviors among elementary school children. J Sch Health. 1995;65:23–27. doi: 10.1111/j.1746-1561.1995.tb03335.x. [DOI] [PubMed] [Google Scholar]
- 22.Vieweg VR, Johnston CH, Lanier JO, Fernandez A, Pandurangi AK. Correlation between high risk obesity groups and low socioeconomic status in school children. South Med J. 2007;100:8–13. doi: 10.1097/01.smj.0000253479.03665.6f. [DOI] [PubMed] [Google Scholar]
- 23.Gabriele JM, Stewart TM, Sample A, et al. Development of an Internet-Based Obesity Prevention Program for Children. J Diabetes Sci Technol. 2010;4:723–732. doi: 10.1177/193229681000400328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Hovell MF, Nader PR. Project SPARK. Effects of physical education on adiposity in children. Ann N Y Acad Sci. 1993;699:127–136. doi: 10.1111/j.1749-6632.1993.tb18844.x. [DOI] [PubMed] [Google Scholar]
- 25.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 26.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120 (Suppl 4):S229–253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 27.Williamson DA, Walden HM, White MA, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006;14:1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 28.Williamson DA, Walden H, York-Crowe E, Stewart TM. Internet-based treatment for pediatric obesity. In: Sothern M, Gordon S, von Almen T, editors. Handbook of Pediatric Obesity: Clinical Management. CRC Press; Boca Raton, FL: 2006. pp. 201–207. [Google Scholar]
- 29.Newton RL, Thomson J, Rau K, Duhe’ S, Sample A, Williamson DA. LA Health: Description of the development of process measures. American Journal of Health Promotion. in press. [Google Scholar]
- 30.Williamson DA, Champagne CM, Han H, et al. Increased obesity in children living in rural communities of Louisiana. Int J Pediatr Obes. 2009;4:160–165. doi: 10.1080/17477160802596148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 32.Cohen J. The earth is round (p <05) Amer Psychologist. 1994;49:997–1003. [Google Scholar]
- 33.Cortina JM, Landis RS. The earth is not round (p =00) Organizational Research Methods. 2011;14:332–349. [Google Scholar]
- 34.Hedges LV. Effect sizes in cluster-randomized designs. J of Educational and Behaioral Staistics. 2007;32:341–370. [Google Scholar]
- 35.Rosnow RL, Rosenthal R. Focused tests of significance and effect size estimation in counseling psychology. J of Counseling Psych. 1988;35:203–208. [Google Scholar]
- 36.Healthy Study Group. A school-based intervention for diabetes risk reduction. N Engl J Med. 2010;363:443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bartholomew JB, Jowers EM. Increasing frequency of lower-fat entrees offered at school lunch: an environmental change strategy to increase healthful selections. J Am Diet Assoc. 2006;106:248–252. doi: 10.1016/j.jada.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 38.Cunningham-Sabo L, Snyder MP, Anliker J, et al. Impact of the Pathways food service intervention on breakfast served in American-Indian schools. Prev Med. 2003;37:S46–54. doi: 10.1016/j.ypmed.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 39.Luepker RV, Perry CL, McKinlay SM, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. JAMA. 1996;275:768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.