Abstract
OBJECTIVE
This study examined substance use and mental health service utilization among a 3-year longitudinal sample of active rural stimulant users.
METHODS
One-step transition probabilities were constructed between the two types of service use for each consecutive pairs of interviews in order to examine the resulting steady-state probabilities among our multiple one-step transition matrices.
RESULTS
Most participants received no substance or mental health services. On average, the limiting probabilities for each state regardless of initial probabilities were 82% for having received neither services, 10% for receiving mental health but not substance use treatment, 6% for receiving substance use but not mental health treatment, and 2% for receiving both services.
CONCLUSIONS
Previous analyses with these data found that both mental health symptomatology and substance use declined over time,suggesting that need for services would also have declined. Many of the changes in drug use may have occurred without specialty treatment.
We know little regarding the use of substance use and mental health services by rural drug users, although research has suggested significant interrural variation in substance usetreatment utilization(1) but few rural/urban differences in alcohol treatment attendance.(2)Overall, relatively few individuals with substance use disorders seek formal treatment.(3-4)Substance use treatment is generally less available to rural residents,(1; 5) partly because some rural areas do not have local programs.
Persons with substance use problems use mental health treatment more than substance use treatment. For example, in the 2002 US National Survey on Drug Use and Health (NSDUH), 9.7% of adults with substance use disorders used specialty treatment in the past year as opposed to 22.4% who utilized mental health services.(6) One study of mostly urban individuals with co-occurring mental health and substance use disorders found greater subsequent mental health service use compared to substance use services.(7) We have little knowledge regarding the services use trajectories of rural substance usepopulations, whether these individuals move between substance use and mental healthservice sectors, or how utilization may vary over time.
The purpose of this report is to examine the rates of substance use and mental health service utilization over time among a longitudinal sample of rural stimulant (cocaine and methamphetamine) users.
METHODS
Data come from a natural history study of 710 stimulant users residing in rural counties of Arkansas, Kentucky, and Ohio.The sample is described in detail elsewhere.(8-9) Counties were classified as rural according to the U.S. Office of Management and Budget definition of a non-metropolitan county, or a county with a population of 50,000 or fewer persons. Participant eligibility criteria included: not in formal SU treatment within the past 30 days, being 18+ years old, use of cocaine and/or methamphetamine in the past 30 days, and having a verifiable address within one of the study counties.
Participants were recruited using Respondent-Driven Sampling, a variant of snowball sampling(10) described in earlier publications.(8) Study staff members recruited potential “seeds” through a variety of community activities and those who completed the baseline interview were asked to give referral coupons to people they knew who used drugs. Seeds received $10 per contact for up to three contacts but up to six referrals were allowed.
The study was approved by the pertinent institutional review boards and the researchers received a Certificate of Confidentiality. Trained research assistants conducted the written informed consent process and face-to-face baseline and follow-up interviews. Follow-up interviews were conducted at 6-month intervals for the next 36 months, culminating in a 73% final follow-up participation rate.
At each interview, participants were asked regarding their recent utilization of substance use treatment and mental health services. At baseline the interview specified within the last three years and subsequent follow-up interviews specified within the previous six months.
We constructed a matrix of individuals with all available services use data at each follow-upperiod(N=603 at 6-months; N=581 at 12-months; N=574 at 18-months; N=560 at 24-months; N-561 at 30-months; 519 at 36-months) over the 7-interview study. We constructed one-step transition probabilities between the two types of service use for each consecutive pairs of interviews using all possible respondents per pair. Our goal was to explore the long-run behavior across each one-step transition probability matrix. In other words, we wished to examine the resulting steady-state probabilities among our multiple one-step transition matrices.There was no assumption of time homogeneity.
RESULTS
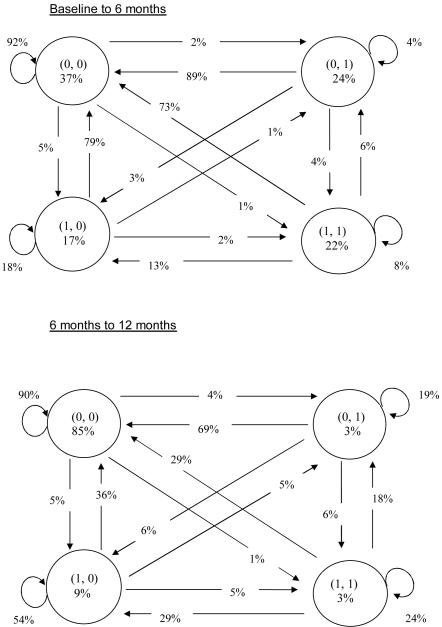
Only 37% of the 710 participants reported neither substanceuse normental health treatment in the previous 3 years at baseline; 22% had received both; 24% had received substance use treatment but no mental health treatment; and 17% mental healthonly (Figure 1, first diagram, data in circles). Ninety-two percent of these stayed in the same “state” at the 6-month interview (Figure 1, semi-circle besides the 0,0 circle). Overall, the transitions were from receipt of services at baseline to none in the intervening 6 months. These transitions, represented by lines between circles, showed that the majority of individuals who had received either mental health or substance use services in the prior 3 years did not receive either at 6 months; for example, 73% of those with both at baseline (1,1 circle) had received neither at 6 months, 13% received mental health services, and 6% received substance use services at 6 months. Repeated use of the same services occurred most often among those with mental health butno substance use services (1,0 circle). On average, the limiting probabilities for each state regardless of initial probabilities were82% for having received neither substance use nor mental health treatment, 10% for receiving mental health but not substance use treatment, 6% for receivingsubstance use but notmental health treatment, and 2% for receiving both services.
Figure 1.
Transitional Probabilities
Six-month transitions were similar (Figure 1, 2nd diagram for 6-12 months; other diagrams available from the corresponding author). The majority of the transitions were from having received services in the earlier interview to no services at the next interview. If continuing services were obtained, they were more likely to be for mental health than substance use treatment.Over the other pairs of consecutive interviews, the relationships remained the essentially the same. The resulting steady-state probabilities were consistent with our final set of probabilities at the 36-months follow-up: 82% for having received neither substance use nor mental health treatment, 9% for receiving mental health but not substance use treatment, 7% for receivingsubstance use but notmental health treatment,and 2% for receiving both services.
DISCUSSION
We found that the majority of participants who completed all 7 interviews were most likely to receive no substance use or mental health services while participating in the study. More received mental health services compared to substance use services, and only a few who received mental health services later transitioned into substance use services. The large decline in service use from baseline to 6 month follow-up is at least partially the result of the baseline measure covering 3 years of service use.
Participants in this study reported a range of mental health and substance use severity (8-9) and many would not have been appropriate for either of these services. While 83% met DSM-IV criteria for a drug use disorder and 57% an alcohol use disorder at baseline, the rates dropped to 30% and 26% at 36 months (data not shown). Similarly, we previously found with these data that mental health symptomatology also declined over time,(9) suggesting that need for mental health services would also have declined. However, our data show that relatively few obtained substance use services, suggesting that many of the changes in drug use may have occurred without specialty treatment. We have previously found significant among-site variation in substance use treatment as well as perceived need for treatment(1) that appear to be descriptively associated with substantially increased travel distance for available services in the state with the lowest treatment rate (data not shown), which may have accounted for overall lower treatment rates. We suspect that the greater use of mental health services may be partly accounted for by the more compelling urgencies of mental health issues (e.g., depression) compared to those arising from substance use, but these differences require further research. Data from the 2006 NSDUH(11) also found substantially more treatment seeking for mental health than substance use (39.6% compared to 2.8%) among those with substance use disorders and serious psychological distress.
These analyses do not tell us which participants were more likely to receive mental health compared to substance use services and analysis of this issue is ongoing. Subsequent analysis will explore potential predictors of the trajectories. Overall, we know much more regarding use of substance use services by substance users(1-2) than about mental health service use by substance users.
Study attrition was greatest for younger individuals, whites, males, unmarried individuals, and those with higher incomes, but we found little evidence of differences in severity of substance use.(9) Prior research with this sample found no association between age, race, gender, and treatment entry for substance use.(1)
(0, 0) Mental Health no, Substance Use treatment no
(0, 1) Mental Health no, Substance Use treatment yes
(1, 0) Mental Health yes, Substance Use treatment no
(1, 1) Mental Health yes, Substance Use treatment yes
Acknowledgements
This research was supported by National Institute on Drug Abuse grants R01 DA15363 and R01 DA14340.
Footnotes
Disclosures of Conflicts of Interest: The authors have no disclosures.
References
- 1.Carlson RG, Sexton R, Falck R, et al. Predictors of substance abuse treatment entry among rural illicit stimulant users in Ohio, Arkansas, and Kentucky. Substance Abuse. 2010;31:1–7. doi: 10.1080/08897070903442459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Booth BM, Kirchner J, Fortney J, et al. Rural at-risk drinkers: Correlates and one-year use of alcohol treatment services. Journal of Studies on Alcohol. 2000;61:267–277. doi: 10.15288/jsa.2000.61.267. [DOI] [PubMed] [Google Scholar]
- 3.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 4.Compton WM, Thomas YF, Stinson FS, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 5.Borders TF, Booth BM. Research on rural residence and access to drug abuse services: Where are we and where do we go? Journal of Rural Health. 2007;23(supp):79–83. doi: 10.1111/j.1748-0361.2007.00128.x. [DOI] [PubMed] [Google Scholar]
- 6.Majabai R. Use of specialty substance abuse and mental health services in adults with substance use disorders in the community. Drug & Alcohol Dependence. 2005;78:345–354. doi: 10.1016/j.drugalcdep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Havassy BE, Alvidrez J, Mericle AA. Disparities in use of mental health and substance abuse services by persons with co-occurring disorders. 2009;60:217–223. doi: 10.1176/appi.ps.60.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Booth B, Leukefeld C, Falck R, et al. Correlates of rural methamphetamine and cocaine users: Results from a multistate community study. Journal of Studies on Alcohol. 2006;67:493–501. doi: 10.15288/jsa.2006.67.493. [DOI] [PubMed] [Google Scholar]
- 9.Booth BM, Curran G, Han x, et al. Longitudinal relationship between psychological distress and multiple substance use: Results from a three-year multisite natural-history study of rural stimulant users. Journal of Studies on Alcohol and Drugs. 2010;71:258–267. doi: 10.15288/jsad.2010.71.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44:74–199. [Google Scholar]
- 11.Substance Abuse and Mental Health Services Association National Survey on Drug Use and Health Report. 2006 http://oas.samhsa.gov/NSDUH/2k6NSDUH/2k6results.cfm.