Abstract
We report a case of duodenal varix bleeding as a long term complication of balloon occluded retrograde transvenous obliteration (BRTO), which was successfully treated with a transjugular intrahepatic portosystemic shunt (TIPS). A 57-year-old man was admitted to the emergency room suffering from melena. He had undergone BRTO to treat gastric varix bleeding 5 mo before admission. Endoscopy and a computed tomography (CT) scan showed complete obliteration of the gastric varix, but the nodular varices in the second portion of the duodenum expanded after BRTO, and spurting blood was seen. TIPS was performed for treatment of duodenal variceal bleeding, because attempts at endoscopic varix ligation were unsuccessful. The postoperative course was uneventful and the patient was discharged without complications. A follow up CT scan obtained 21 mo after TIPS revealed a patent TIPS tract and complete obliteration of duodenal varices, but multinodular hepatocellular carcinoma had developed. He died of hepatic failure 28 mo after TIPS.
Keywords: Duodenal variceal bleeding, Balloon occluded retrograde transvenous obliteration, Transjugular intrahepatic portosystemic shunt
INTRODUCTION
Balloon-occluded retrograde transvenous obliteration (BRTO) is minimally invasive and effective in patients with gastric variceal bleeding[1-5]. Although BRTO achieves excellent prevention of recurrent bleeding with few complications, its long-term efficacy and safety have not been full evaluated. In particular, aggravation of esophageal varices and portal hypertension have been proposed as serious complications of BRTO. There have also been reports that BRTO may aggravate esophageal varices[2,6-8]. However, there are no reports concerning the deterioration of pre-existing duodenal varices by BRTO. Here, we describe our clinical experience of successfully treating bleeding duodenal varices with a transjugular-intrahepatic portosystemic shunt (TIPS) and transcatheter embolization.
CASE REPORT
A 57-year-old man was admitted with a history of melena and intermittent hematochezia. He was hepatitis B virus-positive and had liver cirrhosis. Five mo before admission, an emergency endoscopic examination revealed gastric varices with active bleeding. Endoscopic variceal ligation (EVL) was performed to control variceal bleeding. A tiny nodular varix without bleeding was found in the second portion of the duodenum at that time (Figure 1A). Computed tomography (CT) showed dilated gastric varices with a gastrorenal shunt (Figure 1B). BRTO was performed to prevent recurrent gastric variceal bleeding (Figure 1C). The patient did not have any further bleeding events until our examination. At the time of admission, his blood pressure was 112/56 mmHg, heart rate was 115/min, and respiratory rate was 24/min with symptomatic orthostatic hypotension. No abnormalities were noticed on cardiac and respiratory examinations, except tachycardia. Laboratory tests performed on admission revealed a hemoglobin of 5.9 g/dL, a hematocrit of 17.4%, and a thrombocyte count of 1.6 × 104/mL. The total serum protein and albumin level were 5.5 g/dL and 2.7 g/dL, respectively. Other laboratory data included total bilirubin (0.7 mg/dL) and aspartate aminotransferase [AST: 321 IU/L (normal < 40 IU)]. An emergency endoscopic examination revealed a small, linear esophageal varix without evidence of recent bleeding. In the second portion of the duodenum, the nodular varices had expanded after BRTO and hematocystic spots with fresh blood were seen (Figure 2A). A CT scan showed complete obliteration of gastric varices, but the duodenal varices were aggravated (Figure 2B and C). EVL was done at that site, but the bleeding continued. Therefore, a TIPS was created according to standard procedures. Portography during the TIPS operation revealed a large duodenal varix originating from the superior mesenteric vein and draining into the gonadal vein (Figure 3A). The TIPS tract was created and the vein feeding the duodenal varix was embolized using three metallic coils. The portosystemic gradient was 30 mmHg, which decreased to 12 mmHg after TIPS, and portography showed the disappearance of duodenal variceal flow (Figure 3B). The postoperative course was uneventful. The patient was discharged without complications, and he remained in a stable condition. A follow-up CT scan obtained 21 mo after TIPS revealed a patent TIPS tract and complete obliteration of duodenal varices; however, multinodular hepatocellular carcinoma had developed (Figure 4A and B). He died of hepatic failure 28 mo after TIPS.
Figure 1.
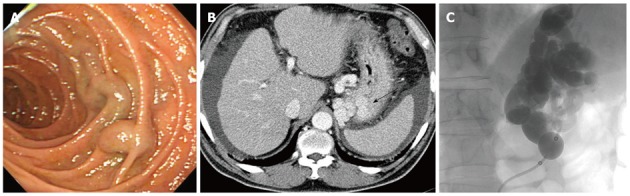
Endoscopic variceal ligation was performed to control variceal bleeding. A: Tiny nodular varices with no bleeding were found at the duodenum second portion; B: Enhanced computed tomography scan showing large gastric varices (arrow); C: Balloon occluded retrograde transvenous obliteration was successfully performed.
Figure 2.
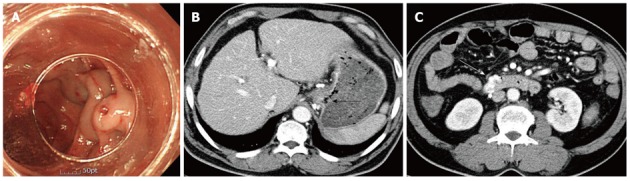
An emergency endoscopic examination revealed a small, linear esophageal varices without evidence of recent bleeding. A: In the second portion of the duodenum, nodular varices expanded before balloon occluded retrograde transvenous obliteration and presented with hematocystic spots; B, C: Enhanced computed tomography scan obtained 5 mo after balloon occluded retrograde transvenous obliteration revealing complete obliteration of gastric varices (black arrow); however, duodenal varices were aggravated (white arrow).
Figure 3.
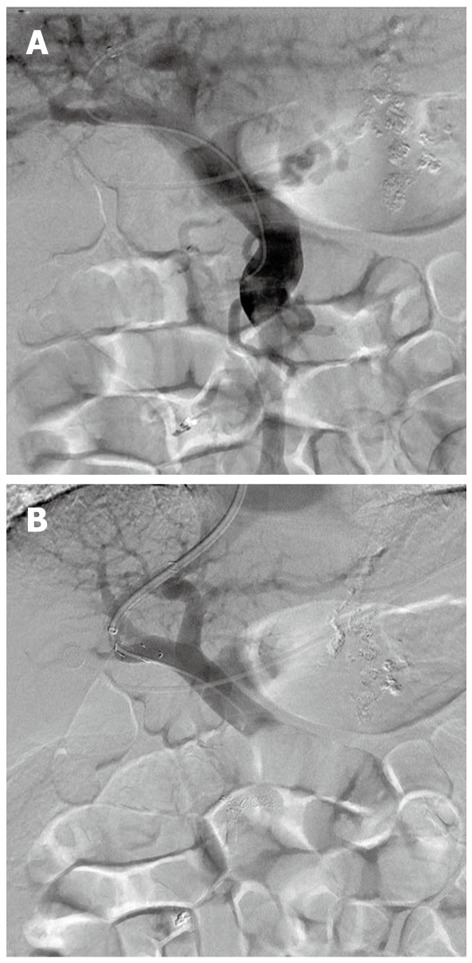
Transjugular intrahepatic portosystemic shunt was created according to standard procedures. A: Portogram showing duodenal variceal flow; B: After transjugular intrahepatic portosystemic shunt and coil embolization of duodenal varices, variceal flow disappeared.
Figure 4.
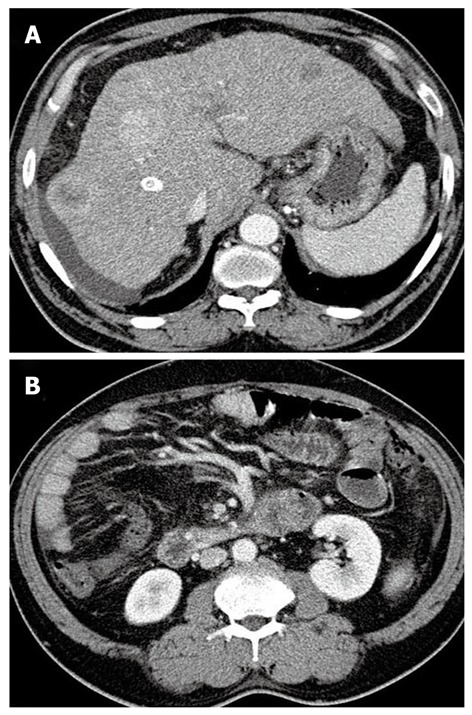
A follow-up computed tomography scan was obtained 21 mo after transjugular intrahepatic portosystemic shunt. A, B: Enhanced computed tomography scan shows a still patent transjugular portosystemic shunt tract and complete improvement of duodenal varices. Note the appearance of multinodular hepatocellular carcinomas in the liver.
DISCUSSION
Interventional treatments for variceal bleeding can be roughly classified into two types: Shunt occlusion and shunt creation. BRTO is representative of shunt occlusion therapies, and has been widely performed in Korea and Japan since it was introduced by Kanakawa in the mid-1990s[4]. It is an interventional radiological technique designed specifically for the treatment of gastric fundal varices with gastrorenal shunt. The principle of BRTO is to eradicate the gastric fundal varices by injecting sclerosant into the varices retrogradely with the balloon inflated in the draining veins, after insertion via the systemic circulation from the femoral or jugular vein. The sclerosant for BRTO is 5% ethanolamine oleate with iopamidol, which injures the endothelial cells of varicose veins and induces thrombosis in the varices. This technique controls gastric variceal bleeding effectively, with success rates of 76% to 92%[3]. Satisfactory results have been reported for managing variceal bleeding with improved liver function and hepatic encephalopathy[1,3,5,9,10]. Theoretically, shunt-obliterating therapies such as BRTO could increase portal blood flow and pressure, and thereafter increase the bleeding risk from other varices, except sclerosed varices. Therefore, aggravation of esophageal varices is a serious complication of BRTO[2,6-8]. A long-term consequence of BRTO is the development or worsening of esophageal varices (EV) resulting from increased portal pressure, which has been reported in 10% to 66% of procedures. In a recent study, worsening of EV was observed after BRTO, with aggravation rates of 27%, 58%, and 66% at 1 years, 3 years, and 5 years, respectively[2]. However, shunt creation therapy, such as TIPS, can decompress the portal pressure, and therefore can be used in the treatment of most complications of portal hypertension, except hepatic encephalopathy. These include acute esophageal variceal bleeding refractory to medical therapy, recurrent esophageal variceal bleeding, gastric variceal bleeding, ectopic variceal bleeding, portal hypertensive gastropathy, Budd-Chiari syndrome, refractory ascites, refractory hepatic hydrothorax, hepatorenal syndrome, hypersplenism, and pancreatic arteriovenous malformation[11]. Nevertheless, TIPS has two main drawbacks. One is aggravation of hepatic encephalopathy and the other is deterioration of hepatic function. Therefore, doing both BRTO and TIPS should compensate for each other’s weak points during treatment of variceal bleeding, because the two therapies are complementary.
Duodenal varices can develop in patients diagnosed with portal hypertension secondary to liver cirrhosis, portal vein thrombosis, schistosomiasis, chronic pancreatitis, and, rarely, pancreatic cancer. Although the bleeding is often severe and fatal, no definitive treatments or guidelines for bleeding duodenal varices have been established[12,13]. Several studies of endoscopic therapies, such as band ligation (BL) or sclerotherapy, have reported variable success rates[13]. However, BL cannot ligate duodenal varices larger than 15 mm[12]. In addition, BL does not completely disrupt the blood flow within varices, and the potential for recurrent bleeding remains[12]. Sclerotherapy has technical difficulties, including a non-ideal approach to the vessels when varices are located in the second portion of the duodenum[13].
The use of radiological interventions provides an alternative method for treating patients presenting with bleeding duodenal varices (DV). Several cases concerning the use of TIPS or BRTO for controlling duodenal variceal bleeding have been reported. Akazawa et al[12] reported a case of duodenal variceal bleeding managed with BRTO. In our patient, the duodenal variceal bleeding caused by BRTO could not be managed endoscopically. As a result, we performed TIPS and transcatheter embolization. In conclusion, BRTO is believed to be effective for controlling gastric variceal bleeding. However, it may increase the risk of coexisting EV, DV, and ectopic variceal bleeding. Using TIPS in combination with embolization, we successfully treated a patient with DV bleeding.
Footnotes
Peer reviewer: Valentin Hans Fuhrmann, Associate Professor, Internal Medicine 3, Department of Gastroenterology and Hepatology, Medical University Vienna, Waehringer Guertel 18-20, Vienna A-1090, Austria
S- Editor Gou SX L- Editor Stewart GJ E- Editor Zhang DN
References
- 1.Matsumoto A, Hamamoto N, Nomura T, Hongou Y, Arisaka Y, Morikawa H, Hirata I, Katsu K. Balloon-occluded retrograde transvenous obliteration of high risk gastric fundal varices. Am J Gastroenterol. 1999;94:643–649. doi: 10.1111/j.1572-0241.1999.00928.x. [DOI] [PubMed] [Google Scholar]
- 2.Ninoi T, Nishida N, Kaminou T, Sakai Y, Kitayama T, Hamuro M, Yamada R, Nakamura K, Arakawa T, Inoue Y. Balloon-occluded retrograde transvenous obliteration of gastric varices with gastrorenal shunt: long-term follow-up in 78 patients. AJR Am J Roentgenol. 2005;184:1340–1346. doi: 10.2214/ajr.184.4.01841340. [DOI] [PubMed] [Google Scholar]
- 3.Choi YH, Yoon CJ, Park JH, Chung JW, Kwon JW, Choi GM. Balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding: its feasibility compared with transjugular intrahepatic portosystemic shunt. Korean J Radiol. 2003;4:109–116. doi: 10.3348/kjr.2003.4.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanagawa H, Mima S, Kouyama H, Gotoh K, Uchida T, Okuda K. Treatment of gastric fundal varices by balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 1996;11:51–58. doi: 10.1111/j.1440-1746.1996.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 5.Sonomura T, Sato M, Kishi K, Terada M, Shioyama Y, Kimura M, Suzuki K, Kutsukake Y, Ushimi T, Tanaka J, et al. Balloon-occluded retrograde transvenous obliteration for gastric varices: a feasibility study. Cardiovasc Intervent Radiol. 1998;21:27–30. doi: 10.1007/s002709900206. [DOI] [PubMed] [Google Scholar]
- 6.Cho SK, Shin SW, Yoo EY, Do YS, Park KB, Choo SW, Han H, Choo IW. The short-term effects of balloon-occluded retrograde transvenous obliteration, for treating gastric variceal bleeding, on portal hypertensive changes: a CT evaluation. Korean J Radiol. 2007;8:520–530. doi: 10.3348/kjr.2007.8.6.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Eight years of experience with transjugular retrograde obliteration for gastric varices with gastrorenal shunts. Surgery. 2001;129:414–420. doi: 10.1067/msy.2001.112000. [DOI] [PubMed] [Google Scholar]
- 8.Nishida N, Ninoi T, Kitayama T, Tokunaga M, Sakai Y, Hamuro M, Nakamura K, Inoue Y, Yamada R. Selective balloon-occluded retrograde transvenous obliteration of gastric varix with preservation of major portacaval shunt. AJR Am J Roentgenol. 2006;186:1155–1157. doi: 10.2214/AJR.04.1971. [DOI] [PubMed] [Google Scholar]
- 9.Akahane T, Iwasaki T, Kobayashi N, Tanabe N, Takahashi N, Gama H, Ishii M, Toyota T. Changes in liver function parameters after occlusion of gastrorenal shunts with balloon-occluded retrograde transvenous obliteration. Am J Gastroenterol. 1997;92:1026–1030. [PubMed] [Google Scholar]
- 10.Kawanaka H, Ohta M, Hashizume M, Tomikawa M, Higashi H, Kishihara F, Sugimachi K, Tokumatsu M. Portosystemic encephalopathy treated with balloon-occluded retrograde transvenous obliteration. Am J Gastroenterol. 1995;90:508–510. [PubMed] [Google Scholar]
- 11.Boyer TD, Haskal ZJ. American Association for the Study of Liver Diseases Practice Guidelines: the role of transjugular intrahepatic portosystemic shunt creation in the management of portal hypertension. J Vasc Interv Radiol. 2005;16:615–629. doi: 10.1097/01.RVI.0000157297.91510.21. [DOI] [PubMed] [Google Scholar]
- 12.Akazawa Y, Murata I, Yamao T, Yamakawa M, Kawano Y, Nomura N, Isomoto H, Mizuta Y, Murase K, Kohno S. Successful management of bleeding duodenal varices by endoscopic variceal ligation and balloon-occluded retrograde transvenous obliteration. Gastrointest Endosc. 2003;58:794–797. doi: 10.1016/s0016-5107(03)02008-x. [DOI] [PubMed] [Google Scholar]
- 13.Almeida JR, Trevisan L, Guerrazzi F, Mesquita MA, Ferraz JG, Montes CG, Kisilwzky NH, Yamanaka A, Soares EC. Bleeding duodenal varices successfully treated with TIPS. Dig Dis Sci. 2006;51:1738–1741. doi: 10.1007/s10620-006-9335-6. [DOI] [PubMed] [Google Scholar]


