Abstract
Heterotopic pancreas is mostly found incidentally, and adenocarcinoma arising from heterotopic pancreas appears to be extremely rare. A case of a 46-year-old woman with adenocarcinoma arising from intrahepatic heterotopic pancreas is reported herein. Computed tomography demonstrated a mass located in the bile duct of the left hepatic lobe. Pathological examination revealed a moderately differentiated adenocarcinoma arising from intrahepatic heterotopic pancreas with nerve infiltration. This may be the first reported case of adenocarcinoma arising from intrahepatic heterotopic pancreas.
Keywords: Heterotopic pancreas, Liver, Biliary tract, Adenocarcinoma
INTRODUCTION
The heterotopic pancreas is defined as aberrant pancreatic tissue without vascular, neural or anatomic continuity with the normal pancreas[1]. The incidence of heterotopic pancreas in autopsy studies is approximately 0.5%-13.7%[2]. Heterotopic pancreatic tissues can be found anywhere in the gastrointestinal tract and the predilection site is the stomach, duodenum and jejunum[3]. Unusual sites include the biliary system and liver[4]. Carcinoma within heterotopic pancreatic tissues is rare, and about 31 well-documented cases have been reported in the literature[5]. We present a case with malignant transformation in heterotopic pancreas of the intra-hepatic biliary tract. To our knowledge, no case of adenocarcinoma arising in the intrahepatic heterotopic pancreas has been described previously.
CASE REPORT
A 45-year-old woman who had been healthy underwent a routine medical check-up in our hospital. The physical examination was normal. Laboratory tests revealed elevated values of γ glutamyl transpeptidase, but normal aspartatate aminotransferase and alanine aminotransferase. The tumor markers including α fetoprotein, carcinoembryonic antigen, CA125 and CA-19-9 were all within normal ranges. Hepatitis virus markers were negative. Ultrasound showed the dilatation of the bile ducts of left hepatic lobe. Abdominal computed tomography (CT) scan revealed a mass located in the bile duct of left hepatic lobe near the hepatic hilus, which had no enhancement in arterial and portal venous, but clear enchancement in delayed phase (Figure 1). Dilatation of the bile ducts of left hepatic lobe was observed up to the periphery of the liver. CT scan and ultrasound failed to demonstrate any pancreatic lesion. A radical resection was performed under the clinical impression of cholangiocarcinoma. She underwent left hepatic and caudate lobectomy and resection of the gallbladder. Postoperative recovery was uneventful.
Figure 1.
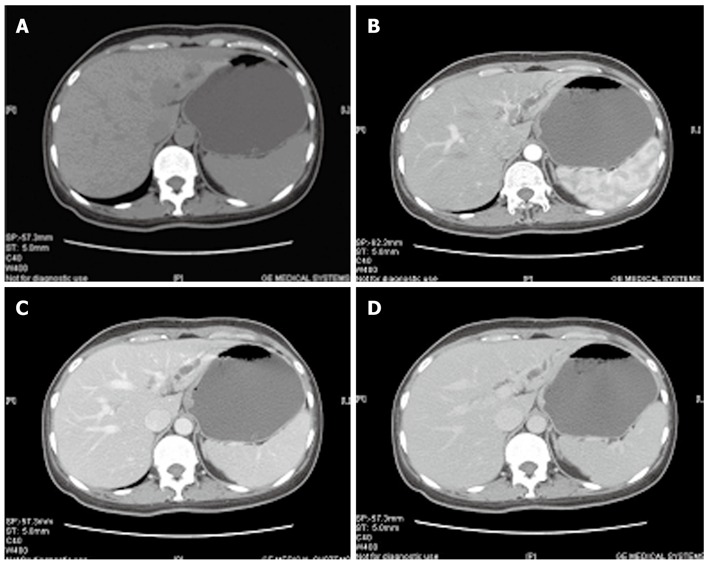
Computed tomography scan shows the dilatation of the bile ducts of left hepatic lobe and a mass located in the bile duct of left hepatic lobe. A-D: Computed tomography scan of abdomen showing dilatation of the bile ducts of left hepatic lobe and a mass located in the bile duct of left hepatic lobe near the hepatic hilus.
Gross examination revealed a firm, gray, nodular mass measuring 3.0 cm × 2.0 cm × 2.0 cm, which was located in the bile duct of left hepatic lobe near the hepatic hilus and had a uniform cut surface without hemorrhage or necrosis. The bile duct of left hepatic lobe was also dilated with a maximum circumference of 0.9 cm. Histologically, the pancreatic tissue consisted of acinar cells and centroacinar cells, and ductal elements were often situated around the acini (Figure 2A). The acinar cells contained eosinophilic granules (Figure 2B). The histological diagnosis was consistent with a moderately differentiated adenocarcinoma arising from intrahepatic heterotopic pancreas (Figure 2C and D).
Figure 2.
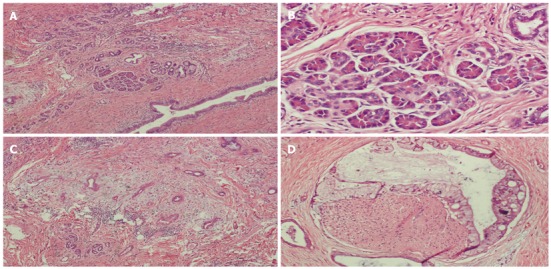
Histopathology shows the heterotopic pancreas and ductal adenocarcinoma arising from heterotopic pancreas. A: Histopathology showing the pancreatic tissue consisting of acinar cells and ductal elements [hematoxylin and eosin (HE), × 4]; B: Histopathology showing the acinar cells containing eosinophilic granules (HE, × 10); C: The solid area showing ductal adenocarcinoma arising from heterotopic pancreas with nerve infiltration (HE, × 4); D: The solid area showing ductal adenocarcinoma arising from heterotopic pancreas with nerve infiltration (HE, × 20).
DISCUSSION
Heterotopic pancreas was firstly described in 1727 by Jean Schultz and lacked anatomic or vascular connection with the main body of the pancreas. Although pancreatic heterotopia can be found virtually anywhere along the gastrointestinal tract, the most frequent sites are the stomach (27.5%), duodenum (25.5%), and jejunum (15.9%)[3]. It is also observed less frequently in the esophagus, spleen, gallbladder, biliary tract, liver and lung. Up to now, only eight cases of intrahepatic heterotopic pancreas have been reported, including a case of insular carcinoma probably arising from intrahepatic heterotopic pancreas[6], a case of hepatic and extrahepatic choledochal cysts[7], a case presenting as hepatic mass[8], a case of primary cholesterol hepatolithiasis[9,10], a case found in autopsy liver specimens[11], a case of cirrhosis[12], and a case of Caroli’s disease[13].
In 1909, Heinrich et al[14] classified heterotopic pancreas into three types. Type I is defined by the presence of ducts, acini and endocrine islets similar to those seen in normal pancreatic tissues. Type II contains a large number of acini, a few ducts and no islets. Type III is characterized by the presence of numerous ducts, a few acini, and no islets. The histological classification of the ectopic pancreatic tissue in the present case is type II, consisting of acini and a few ductal components.
Heterotopic pancreas is often found incidentally during surgery or endoscopy or clinically silent and benign. Malignant transformation in heterotopic pancreas is extremely rare. Thirty-one well-documented cases of carcinoma arising in a heterotopic pancreas were reviewed by Goodarzi[5]. The results showed that most tumors in the heterotopic pancreatic tissues occurred in the stomach and most of them were adenocarcinomas. The present case is the first case of adenocarcinoma arising from the intrahepatic heterotopic pancreas. Guillou et al[15] suggested that three criteria should be met for a carcinoma to be diagnosed as arising from the heterotypic pancreas. First, the tumor must be within or near the ectopic pancreatic tissue. Second, transition between pancreatic tissue and carcinoma must be observed. Third, the nonneoplastic pancreatic tissue should comprise acini, epithelial and ductal structures. The present case satisfied these three criteria.
A potential confusion is a primary intrahepatic cholangiocarcinoma with unrelated pancreatic heterotopia of the liver, which may happen if the heterotopic pancreasis is completely replaced by the adenocarcinoma or if the presence of pancreatic tissue can not be confirmed due to sampling. Furthermore, primary intrahepatic cholangiocarcinoma is associated with intrahepatic bile duct stones and chronic infection in most cases. Zhang et al[16] also demonstrated that the adenocarcinoma can arise from heterotopic pancreas. Extensive sampling of the specimen and a high index of suspicion for carcinoma arising from heterotopic pancreas can avoid this diagnostic confusion.
In conclusion, malignant transformation in heterotopic pancreas is extremely rare. Extensive sampling of the specimen and a high index of suspicion for carcinoma arising from heterotopic pancreas can provide accurate diagnosis.
Footnotes
Peer reviewer: Dr. Antoni Farre, Hospital de la Santa Creu i Sant Pau, Av. Sant Antoni M Claret 167, 08025 Barcelona, Spain
S- Editor Gou SX L- Editor Ma JY E- Editor Zhang DN
References
- 1.Elsayes KM, Narra VR, Lewis JS, Abu El Abbas HA, Brown JJ. MRI of heterotopic pancreatic tissue in the spleen. AJR Am J Roentgenol. 2005;185:816–817. doi: 10.2214/ajr.185.3.01850816. [DOI] [PubMed] [Google Scholar]
- 2.Barbosa DE, Castro JJ, Dockerty MB, Waugh JM. Pancreatic heterotopia: review of the literature and report of 41 authenticated surgical cases, of which 25 were clinically significant. Surg Gynecol Obstet. 1946;82:525–542. [PubMed] [Google Scholar]
- 3.Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue. A study of 212 cases. Arch Surg. 1974;109:762–765. doi: 10.1001/archsurg.1974.01360060032010. [DOI] [PubMed] [Google Scholar]
- 4.Heer C, Pförtner M, Hamberger U, Raute-Kreinsen U, Hanraths M, Bartsch DK. [Heterotopic pancreatic tissue in the bifurcation of the bile duct: Rare diagnosis mimicking a Klatskin tumour] Chirurg. 2010;81:151–154. doi: 10.1007/s00104-009-1674-3. [DOI] [PubMed] [Google Scholar]
- 5.Goodarzi M, Rashid A, Maru D. Invasive ductal adenocarcinoma arising from pancreatic heterotopia in rectum: case report and review of literature. Hum Pathol. 2010;41:1809–1813. doi: 10.1016/j.humpath.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Ballinger J. Hypoglycemia from metastasizing insular carcinoma of aberrant pancreatic tissue in the liver. Arch Pathol. 1941;32:277–285. [Google Scholar]
- 7.Suzuki K, Uchida T, Nakayama H, Ugajin W, Inaniwa Y, Sugitani M, Mori Y. Heterotopic pancreatic tissue associated with intra- and extrahepatic choledochal cysts. Pathol Int. 1999;49:759–762. doi: 10.1046/j.1440-1827.1999.00930.x. [DOI] [PubMed] [Google Scholar]
- 8.Mobini J, Krouse TB, Cooper DR. Intrahepatic pancreatic heterotopia: review and report of a case presenting as an abdominal mass. Am J Dig Dis. 1974;19:64–70. doi: 10.1007/BF01073355. [DOI] [PubMed] [Google Scholar]
- 9.Fukueda M, Hamada N, Kaieda M, Kadono J, Nakamura N, Ishizaki N. [A case of heterotopic pancreas in the liver with primary cholesterol hepatolithiasis] Nihon Shokakibyo Gakkai Zasshi. 2000;97:1057–1061. [PubMed] [Google Scholar]
- 10.Cui Y, Ji M, Zhou JL, Li CL. Clinical Features of Ectopic Pancreas (Report of 11 Cases) Zhongguo Puwai Jichu Yu Linchuang Zazhi. 2006;13:712–713. [Google Scholar]
- 11.Terada T, Nakanuma Y, Kakita A. Pathologic observations of intrahepatic peribiliary glands in 1000 consecutive autopsy livers. Heterotopic pancreas in the liver. Gastroenterology. 1990;98:1333–1337. doi: 10.1016/s0016-5085(12)90353-4. [DOI] [PubMed] [Google Scholar]
- 12.Wolf HK, Burchette JL, Garcia JA, Michalopoulos G. Exocrine pancreatic tissue in human liver: a metaplastic process? Am J Surg Pathol. 1990;14:590–595. doi: 10.1097/00000478-199006000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Payan MJ, Choux R, Sahel J, Laugier R, Kennedy R, Sastre B, Sarles H. Caroli’s disease associated with pancreatic heterotopia and biliary papillomatosis. Histopathology. 1985;9:1001–1006. doi: 10.1111/j.1365-2559.1985.tb02884.x. [DOI] [PubMed] [Google Scholar]
- 14.Von Heinrich H. Ein beitrag zur histologie des sogen: akzessotischen pancreas. Virchows Arch Pathol Anat Histopathol. 1909;198:392–401. [Google Scholar]
- 15.Guillou L, Nordback P, Gerber C, Schneider RP. Ductal adenocarcinoma arising in a heterotopic pancreas situated in a hiatal hernia. Arch Pathol Lab Med. 1994;118:568–571. [PubMed] [Google Scholar]
- 16.Zhang L, Sanderson SO, Lloyd RV, Smyrk TC. Pancreatic intraepithelial neoplasia in heterotopic pancreas: evidence for the progression model of pancreatic ductal adenocarcinoma. Am J Surg Pathol. 2007;31:1191–1195. doi: 10.1097/PAS.0b013e31806841e1. [DOI] [PubMed] [Google Scholar]


