Abstract
OBJECTIVE:
We investigated the association between smoke-free laws and asthma prevalence, symptoms, and severity among nonsmoking youth (aged 3–15 years).
METHODS:
We examined data from the 1999–2006 National Health and Nutrition Examination Survey, a cross-sectional survey designed to monitor the health and nutritional status of the US population. Survey locations were dichotomized as having or not having at least 1 smoke-free workplace, restaurant, or bar law at the county or state level that covered the entire county population. Asthma prevalence was assessed as self-reported current asthma and as ever having asthma with current symptoms. Asthmatic symptoms included persistent wheeze, chronic night cough, and wheeze-medication use. We also examined asthma severity (asthma attack or emergency-department visit for asthma) and persistent ear infection.
RESULTS:
Smoke-free laws were not associated with current asthma but were significantly associated with lower odds of asthmatic symptoms (odds ratio [OR]: 0.67 [95% confidence interval (CI): 0.48–0.93]) among nonsmoking youth. The association between smoke-free laws and ever having asthma with current symptoms approached significance (OR: 0.74 [95% CI: 0.53–1.03]). Smoke-free laws were associated with lower odds of asthma attacks (OR: 0.66 [95% CI: 0.28–1.56]) and emergency-department visits for asthma (OR: 0.55 [95% CI: 0.27–1.13]), although these results were not statistically significant.
CONCLUSIONS:
Our results suggest that smoke-free laws reduce asthmatic symptoms, including persistent wheeze, chronic night cough, and wheeze-medication use in nonsmoking youth.
Keywords: asthma, tobacco control policy, children, adolescents, National Health and Nutrition Examination Survey
WHAT'S KNOWN ON THIS SUBJECT:
Smoke-free laws reduce exposure to secondhand smoke, as measured by cotinine, in both adults and children. In adults, smoke-free laws have been associated with reductions in health outcomes such as respiratory symptoms and acute myocardial infarctions, as well.
WHAT THIS STUDY ADDS:
This study examined the association between smoke-free laws and health in children and adolescents. Health outcomes that have been associated with exposure to secondhand smoke in children include prevalence of asthma, asthmatic symptoms, asthma severity, and ear infection.
Secondhand smoke has been associated with a number of respiratory conditions in children and adolescents. In the 2006 Surgeon General's report,1 it was concluded that there was sufficient evidence that parental smoking causes lower-respiratory illnesses, middle-ear disease, cough, phlegm, wheeze, breathlessness, and prevalent asthma.
Among children with asthma, exposure to secondhand smoke can trigger an asthma attack.1 It has been estimated that exposure to secondhand smoke worsens the condition of 400 000 to 1 million children with asthma.2 Common symptoms of an asthma attack include coughing, wheezing, and shortness of breath.
It is well established that smoke-free laws reduce exposure to secondhand smoke in adults.3–17 Evidence shows that smoke-free laws also reduce exposure to secondhand smoke in children and adolescents18,19 by reducing the overall amount of secondhand smoke in a community and by reducing the amount of smoking in the home,20,21 the primary source of secondhand smoke exposure for children.22–25 Although smoke-free laws have been shown to be associated with a number of respiratory illnesses13–17 and acute myocardial infarction26–28 in adults, the evidence for the effects of smoke-free laws on the health of children is limited.29
We previously showed that smoke-free laws were associated with lower cotinine levels in children and adolescents.19 In the current study, we examined the association between smoke-free laws and health outcomes, including prevalence of asthma, asthma-related symptoms, and asthma severity among children and adolescents using data from the 1999–2006 National Health and Nutrition Examination Survey (NHANES).
METHODS
Data Source
The NHANES, conducted by the National Center for Health Statistics, is a series of cross-sectional surveys designed to monitor the health and nutrition status of the US population. Participants are selected through a complex, multistage, probability-cluster design. From 1999–2006, adolescents aged 12–19 years, adults aged 60 years or older, low-income subjects, Mexican American people, and non-Hispanic black people were oversampled to improve the reliability and precision of estimates for these groups.30 Public-use data files were released in 2-year cycles (1999–2000, 2001–2002, 2003–2004, and 2005–2006).
The NHANES consisted of a household interview and a standardized physical examination conducted in a mobile examination center. The household interview included questions about demographic characteristics, health history, health-related behaviors, and medical conditions. In general, subjects aged 16 or older were interviewed directly. A responsible adult provided information for participants younger than age 16 years. Signed informed consent was obtained for all participants. For NHANES 1999–2006, there were 50 939 subjects selected for the sample, 41 474 subjects were interviewed (81.4%), and 39 352 (77.3%) were examined in the mobile examination center.
This analysis was restricted to nonsmoking participants (youths) aged 3–15 years. Nonsmokers were defined by both cotinine levels and self-reported smoking status. Youth with missing cotinine levels (n = 2091) were excluded. Participants with cotinine levels less than 15.0 ng/mL31 were considered to be nonsmokers (n = 9135). Youth aged 12–19 years answered questions themselves (not using a proxy) about tobacco or nicotine use in the 5 days before blood collection, using a computer-assisted personal interview. Youth who reported that they had used tobacco or nicotine in the previous 5 days or who were missing information on this variable were excluded (n = 324). Youth who were pregnant also were excluded (n = 11). This resulted in a final sample size of 8800 nonsmoking youth.
Outcomes
Four outcomes were examined: prevalence of asthma; asthmatic symptoms; ear infection; and asthma severity. Prevalence of asthma was first assessed as self-reported current asthma, defined as a positive answer to both of 2 questions: “Has a doctor or other health professional ever told you that you have asthma?” and “Do you still have asthma?”
Second, we defined ever having asthma with current symptoms as reporting ever having doctor-diagnosed asthma and at least 1 of the following self-reported symptoms in the previous year:
a total of 3 or more episodes of wheezing or whistling in the chest (persistent wheeze);
dry coughing at night that lasted 14 days or more, not counting a cough associated with a cold or chest infection (chronic night cough); or
medication prescribed by a doctor for wheezing or whistling (wheeze-medication use).
Persistent ear infection was defined as having had 3 or more ear infections in the previous year. This question was only asked in 1999–2004. Only participants with self-reported current asthma (n = 896) were asked questions about asthma severity. Youth who reported having an asthma attack (“During the past 12 months, have you had an episode of asthma or an asthma attack in the past year?”) or an emergency-department visit (“During the past 12 months have you had to visit an emergency department or urgent care center because of asthma?”) were considered to have severe asthma.
Exposure to Smoke-Free Laws
NHANES participants were classified into smoke-free law-coverage categories by their county and state of residence.8,19 From 1999 to 2006, NHANES sampled youth from 117 survey locations or counties. Information on state and local smoke-free laws was obtained for each county from a database of local and state indoor-air ordinances maintained by the American Nonsmoker's Rights Foundation.32 The American Nonsmoker's Rights Foundation list indicated smoke-free laws for workplaces, restaurants, and bars at the city, county, and state level. Locations classified as having a smoke-free law completely banned smoking and did not allow for separately ventilated smoking rooms, size exemptions, or allowed smoking in bars attached to restaurants. Laws only were included if they were enacted before the examination portion of the survey was administered.
Each county was categorized into 2 smoke-free law-coverage groups. Smoke-free counties (n = 26) had at least 1 smoke-free workplace, restaurant, or bar law at the county or state level that covered the entire county population. There were 91 counties without such a smoke-free law at the county or state level.
Covariates
Variables associated with smoke-free law enactment or asthma were included in each model, including age (3–5, 6–11, and 12–15 years), gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other), ratio of family income to poverty (above versus below poverty threshold), 2-year survey cycle, and region (West, Northeast, and South/Midwest combined because of small sample sizes).
Additional risk factors for asthma included in the models were household size (≥5 vs <5 residents), health insurance status in the previous year (yes or no), BMI (underweight/healthy, overweight, and obese on the basis of gender and age), mother's age at birth (<20, 20–24, 25–29, and ≥30 years), mother's smoking status during pregnancy (no, yes, yes but quit), and low birth weight (≤5.5 lb). Daycare or preschool attendance (ever) was collected in 1999–2004 and was used to adjust the ear infection analysis, which also was collected in 1999–2004.
We examined the association between smoke-free laws and respiratory outcomes stratified by exposure to secondhand smoke in the home. One member of each household was asked “Does anyone who lives here smoke cigarettes, cigars, or pipes anywhere inside this home?” If at least 1 person smoked inside the home, all members of that house were classified as having home secondhand smoke exposure.
Statistical Analysis
Data management was conducted by using SAS 9.1 (SAS Institute Inc, Cary, NC) and data analysis in SUDAAN 9.0 (Research Triangle Institute, Research Triangle Park, NC), which accounted for the multistage, probability-cluster design. Examination sample weights were used to account for differential probabilities of selection and for nonresponse. Variance estimates were calculated by using the Taylor linearization-with-replacement method. Differences in proportions were evaluated with a t test using a significance level of P < .05.
Publicly released data files provided masked variance units to estimate sampling errors.30 Masked variance units were created to comply with disclosure-avoidance principals that prohibit the public release of the primary sampling units. The exposure of interest, the smoke-free law-coverage category, was based on the true primary sampling units, and we used these strata variables, which are available through the National Center for Health Statistics Research Data Center (available at: www.cdc.gov/rdc), for calculating SEs for all estimates.
Weighted logistic regression was used to calculate unadjusted and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for the association between smoke-free laws and prevalent asthma, asthmatic symptoms, ear infection, and asthma severity. Effect modification by home secondhand smoke exposure and age was assessed by including an interaction term in the adjusted model.
RESULTS
A total of 2227 (21%) of 8800 participants lived in a smoke-free county. There was a higher percentage of certain demographic groups in smoke-free counties, including youth from the later survey cycles, Mexican American youth, youth from the West or Northeast, and youth who lived without a smoker in the home (Table 1).
TABLE 1.
Weighted Percentage (SE) of Nonsmoking Youth Living in a County With a Smoke-Free Law, According to Covariates: Ages 3 to 15 Years, NHANES 1999–2006
| Sample Size, n | Total Percentage (SE) | Percentage (SE) With a Smoke-Free Law | Pa | |
|---|---|---|---|---|
| Total | 8800 | 20.9 (3.2) | ||
| Year | ||||
| 1999–2000 | 2112 | 21.8 (1.6) | 11.8 (3.6)b | Reference |
| 2001–2002 | 2407 | 28.0 (2.1) | 20.4 (8.5)b | .40 |
| 2003–2004 | 2130 | 25.2 (1.5) | 24.3 (7.7)b | .15 |
| 2005–2006 | 2151 | 25.0 (1.9) | 26.2 (6.0) | .04 |
| Gender | ||||
| Male | 4407 | 52.3 (0.78) | 21.1 (3.2) | Reference |
| Female | 4393 | 47.7 (0.78) | 20.8 (3.5) | .83 |
| Age, y | ||||
| 3–5 | 1582 | 18.8 (0.48) | 21.0 (4.1) | Reference |
| 6–11 | 3575 | 49.3 (0.78) | 20.3 (3.0) | .66 |
| 12–15 | 3643 | 31.9 (0.77) | 22.0 (3.4) | .53 |
| Household size | ||||
| ≥5 | 4863 | 46.9 (1.1) | 24.6 (4.5) | Reference |
| <5 | 3937 | 53.1 (1.1) | 17.7 (2.6) | .05 |
| Race/ethnicity | ||||
| Non-Hispanic black | 2776 | 15.0 (1.2) | 10.6 (2.6) | .09 |
| Non-Hispanic white | 2248 | 59.0 (1.8) | 17.6 (3.9) | Reference |
| Mexican American | 3018 | 13.4 (0.9) | 38.7 (4.4) | <.001 |
| Other | 758 | 12.6 (1.1) | 30.2 (5.5) | .004 |
| Ratio of income to poverty | ||||
| Below poverty level | 2747 | 23.3 (1.2) | 20.5 (3.3) | Reference |
| Above poverty level | 5520 | 76.7 (1.2) | 21.1 (3.4) | .74 |
| Region | ||||
| South/Midwest | 5019 | 58.9 (3.4) | 3.1 (2.3)b | <.001 |
| Northeast | 1191 | 15.6 (1.2) | 29.6 (8.5)b | .06 |
| West | 2590 | 25.5 (3.1) | 56.8 (11.0) | Reference |
| Health insurance | ||||
| Yes | 7264 | 87.4 (1.0) | 21.3 (3.3) | Reference |
| No | 1451 | 12.6 (1.0) | 19.0 (3.5) | .32 |
| BMI | ||||
| Underweight/healthy weight | 5464 | 65.8 (1.1) | 21.4 (3.8) | Reference |
| Overweight | 1445 | 16.1 (0.5) | 21.9 (3.2) | .76 |
| Obese | 1818 | 18.1 (0.9) | 19.1 (2.3) | .45 |
| Mother's age at birth, y | ||||
| <20 | 1559 | 13.6 (0.6) | 14.7 (2.3) | Reference |
| 20–24 | 2562 | 26.3 (0.9) | 18.2 (2.8) | .03 |
| 25–29 | 2296 | 28.6 (0.9) | 20.1 (3.4) | .008 |
| >30 | 2275 | 31.5 (1.2) | 26.7 (3.9) | <.001 |
| Mother smoked during pregnancy | ||||
| Yes | 780 | 11.3 (0.8) | 13.6 (2.6) | .001 |
| Yes but quit | 459 | 6.7 (0.3) | 17.4 (3.6) | .06 |
| No | 7421 | 82.1 (0.9) | 22.4 (3.4) | Reference |
| Low birth weight, lb | ||||
| <5.5 | 1089 | 11.2 (0.6) | 22.2 (3.4) | Reference |
| ≥5.5 | 7621 | 88.8 (0.6) | 20.7 (3.3) | .53 |
| Ever attend day care (1999–2004) | ||||
| Yes | 4406 | 72.1 (1.2) | 18.5 (4.0) | Reference |
| No | 2230 | 27.9 (1.2) | 21.1 (4.7) | .30 |
| Home secondhand smoke exposure | ||||
| Yes | 1769 | 21.9 (1.2) | 10.9 (2.3) | Reference |
| No | 6956 | 78.1 (1.2) | 23.8 (3.7) | <.001 |
P value (t test) to test the null hypothesis of no differences in the percentage with a smoke-free law.
Does not meet the standard of statistical reliability and precision (relative SE [SE/percent]) > 30%).
Self-reported Current Asthma and Severity
Self-reported current asthma was reported by 9.8% of youth. There was a similar percentage of youth living in smoke-free counties who self-reported having current asthma as those not living in smoke-free counties (10.0% and 9.7%, respectively) (Table 2). The unadjusted ORs for the association between smoke-free laws and self-reported current asthma were close to 1 (OR: 1.03 [95% CI: 0.81–1.30]). This association was not modified by secondhand smoke exposure at home or age.
TABLE 2.
Prevalence of Self-reported Current Asthma and Asthma Severity in the Previous Year and Association With Smoke-Free Laws Among Nonsmoking Youth Aged 3 to 15 Years, NHANES 1999–2006
| Living in a County |
OR (95% CI) |
|||
|---|---|---|---|---|
| Without a Smoke-Free Law | With a Smoke-Free Law | Unadjusted | Adjusteda | |
| Self-reported current asthma, n | 6573 | 2227 | — | — |
| Weighted % (SE) | 9.7 (0.5) | 10.0 (0.9) | 1.03 (0.81–1.30) | 1.08 (0.85–1.37) |
| Among self-reported current asthmatic subjects, n | 682 | 215 | — | — |
| Asthma attack, weighted % (SE) | 66.5 (3.5) | 63.5 (4.4) | 0.86 (0.51–1.45) | 0.66 (0.28–1.56) |
| Emergency-room visit, weighted % (SE) | 20.3 (1.9) | 17.7 (3.4) | 0.77 (0.43–1.39) | 0.55 (0.27–1.13) |
Adjusted for survey cycle, gender, age, race, ratio of income to poverty, region, health insurance, mother's age at birth, mother's smoking status during pregnancy, low birth weight, BMI, and household size.
Among youth with self-reported current asthma, 66% reported having an asthma attack and 20% reported going to the emergency department for their asthma attack. Adjusted for covariates, youth living in a smoke-free county had 0.66 (95% CI: 0.28–1.56) times the odds of having an asthma attack and 0.55 (95% CI: 0.27–1.13) times the odds of going to the emergency department for asthma (Table 2).
Ever Having Asthma With Current Symptoms and Asthmatic Symptoms
The percentage of youth reported as ever having asthma with current symptoms (7.2%) was slightly lower than the percentage of youth with self-reported current asthma (9.8%). Adjusted for covariates, youth living in smoke-free counties had 0.74 (95% CI: 0.53–1.03) times the odds of ever having asthma with current symptoms compared with youth living in counties without smoke-free laws (Table 3).
TABLE 3.
Prevalence of Ever Having Asthma With Symptoms in the Previous Year and Association With Smoke-Free Laws Among Nonsmoking Youth Aged 3 to 15 Years, NHANES 1999–2006
| Weighted Percentage (SE) Living in a County |
OR (95% CI) |
|||
|---|---|---|---|---|
| Without a Smoke-Free Law (n = 6573) | With a Smoke-Free Law (n = 2227) | Unadjusted | Adjusteda | |
| Ever asthma with current symptomsb | 7.5 (0.5) | 5.9 (0.7) | 0.79 (0.58–1.07) | 0.74 (0.53–1.03) |
| Asthmatic symptomsb | 12.1 (0.6) | 8.4 (1.1) | 0.69 (0.50–0.95)c | 0.67 (0.48–0.93)c |
| Persistent wheeze | 6.4 (0.4) | 3.9 (0.7) | 0.57 (0.36–0.92)c | 0.58 (0.37–0.89)c |
| Chronic night cough | 3.1 (0.4) | 1.6 (0.4) | 0.57 (0.35–0.95)c | 0.43 (0.24–0.76)c |
| Wheeze-medication use | 9.3 (0.5) | 7.2 (0.9) | 0.76 (0.56–1.05) | 0.79 (0.58–1.05) |
| Persistent ear infections (≥3) (1999–2004) | 6.1 (0.5) | 3.4 (0.7) | 0.57 (0.33–0.98)c | 1.01 (0.50–2.05) |
Adjusted for survey cycle, gender, age, race, ratio of income to poverty, region, health insurance, mother's age at birth, mother's smoking status during pregnancy, low birth weight, BMI, and household size.
Persistent wheeze, chronic night cough, or wheeze-medication use.
Adjusted OR was additionally adjusted for ever attending daycare.
An estimated 11.4% of youth reported having asthmatic symptoms in the previous year, including persistent wheeze, chronic night cough, or wheeze-medication use. Youth living in smoke-free counties had fewer asthmatic symptoms (8.4%) compared with youth living in counties without smoke-free laws (12.1%) (Table 3), with an adjusted OR of 0.67 (95% CI: 0.48–0.93). Examining these symptoms individually, persistent wheeze and chronic night cough had slightly lower adjusted ORs than wheeze-medication use (Table 3). The association between smoke-free laws and asthmatic symptoms was similar for youth with current, previous, and no asthma (data not presented).
We found a difference in the association between smoke-free laws and ever having asthma with symptoms by home secondhand smoke exposure, although the difference was not statistically significant (P value for interaction = .36) (Fig 1A). Youth who did not experience home secondhand smoke exposure had a stronger association between smoke-free laws and ever having asthma with current symptoms (OR: 0.67 [95% CI: 0.47–0.94]) compared with youth who did experience home secondhand smoke exposure (OR: 1.25 [95% CI: 0.50–3.16]). We found no difference in the association between smoke-free laws and asthmatic symptoms by home secondhand smoke exposure (Fig 1A).
FIGURE 1.
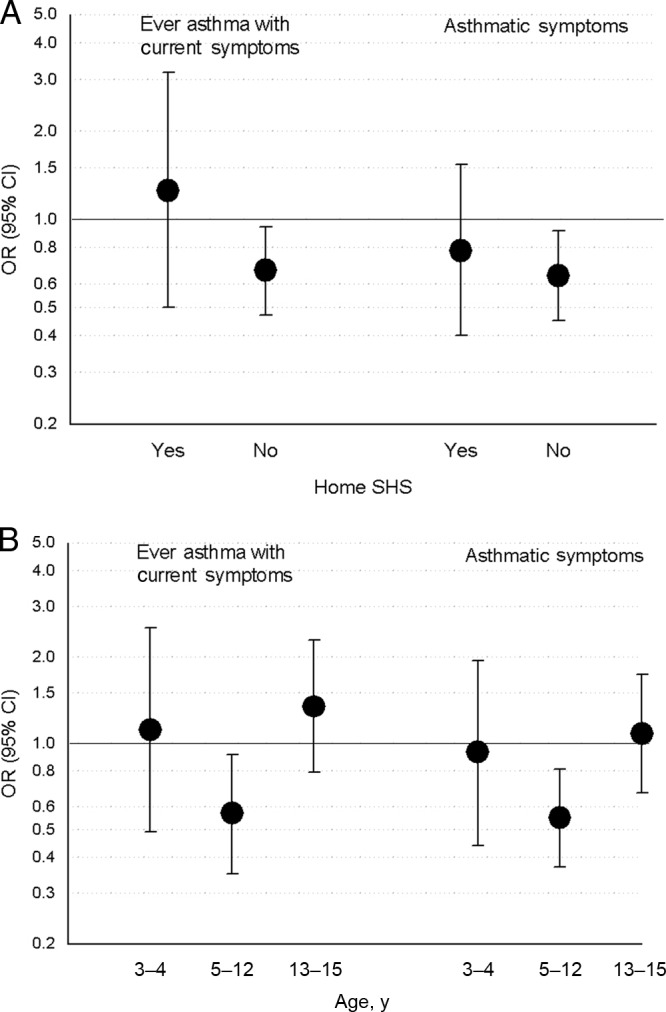
Association between smoke-free laws and ever having asthma with symptoms and asthmatic symptoms (persistent wheeze, chronic night cough, or wheeze-medication use) according to home secondhand smoke (SHS) exposure status (A) and age (B), NHANES 1999–2006. Data were adjusted for survey cycle, gender, age, race, ratio of income to poverty, region, health insurance, mother's age at birth, whether the mother smoked during pregnancy, low birth weight, BMI, and household size.
We found a stronger association between smoke-free laws and ever having asthma with current symptoms in children aged 5 to 12 years compared with children aged 3 to 4 and 13 to 15 years (Fig 1B), with adjusted ORs of 1.11 (95% CI: 0.49–2.52), 0.57 (95% CI: 0.35–0.91), and 1.34 (95% CI: 0.79–2.28) for ages 3 to 4, 5 to 12, and 13 to 15 years, respectively (P value for interaction = .16). A similar pattern was seen for the association between smoke-free laws and asthmatic symptoms, with adjusted ORs of 0.93 (95% CI: 0.44–1.94), 0.55 (95% CI: 0.37–0.81), and 1.08 (95% CI: 0.67–1.74) (P value for interaction = .05). Examining asthmatic symptoms individually, the associations between smoke-free laws and chronic night cough and wheeze-medication use followed a similar age pattern. However, the association between smoke-free laws and persistent wheeze was stronger for children aged 3 to 4 and 5 to 12 years compared with those who were aged 13 to 15 years. None of these interaction terms were statistically significant.
Persistent Ear Infection
Youth living in smoke-free counties had approximately half the prevalence of persistent ear infections in the previous year (3.4%) compared with youth living in counties without a smoke-free law (6.1%) (Table 3). However, after adjustment for covariates, this difference no longer persisted (adjusted OR: 1.01 [95% CI: 0.50–2.05]). Region accounted for the majority of this attenuation. Youth living in the South and Midwest were more likely to have persistent ear infection and were less likely to live in a smoke-free county. The OR adjusted for all covariates except region was 0.64 (95% CI: 0.37–1.10).
DISCUSSION
We examined the associations between smoke-free laws and prevalent asthma, asthmatic symptoms, asthma severity, and persistent ear infection among children and adolescents in the United States. We did not find an association between smoke-free laws and self-reported current asthma. However, smoke-free laws were associated with lower odds of ever having asthma with current symptoms (OR: 0.74 [95% CI: 53–1.03]) and asthmatic symptoms (OR: 0.67 [95% CI: 0.48–0.93]). In addition, smoke-free laws were associated with a lower odds of asthma attacks (OR: 0.66 [96% CI: 0.28–1.56]) and emergency department visits for asthma (OR: 0.55 [95% CI: 0.27–1.13]), although these results were not statistically significant. These results suggest that smoke-free laws primarily reduce the symptoms associated with asthma but not the prevalence of asthma.
The associations between smoke-free laws and ever having asthma with current symptoms and asthmatic symptoms seemed to be modified by home secondhand smoke exposure and age (although the interaction terms were not statistically significant). Youth living without a smoker in the home seemed to have a stronger association between smoke-free laws and ever having asthma with current symptoms. That is, smoke-free laws that targeted exposures to secondhand smoke outside the home had more effect on these children and adolescents without concomitant exposure at home.
Although we did not have specific information on smoking policies within the home, research has shown that smoking only outside the home reduces, but does not eliminate, children's exposure to secondhand smoke.33,34
The association between smoke-free laws and ever having asthma with current symptoms and asthmatic symptoms was stronger among children ages 5 to 12 years compared with children ages 3 to 4 and 13 to 15 years. The interactions between smoke-free laws and age may be because of differences in the association between secondhand smoke exposure and asthmatic symptoms because we did not find a difference in the association between smoke-free laws and secondhand smoke exposure by age (results not shown). For example, the association between smoke-free laws and persistent wheeze was stronger among children aged 3 to 4 and 5 to 12 years compared with those aged 13 to 15 years. Using data from NHANES III, Mannino et al35 also found a slightly stronger association between secondhand smoke exposure and persistent wheeze for children aged 4 to 6 and 7 to 11 years compared with children aged 12 to 16 years. An alternative explanation is that there is limited power to detect interactions by home secondhand smoke exposure and age. Although our sample included 8800 youth, it is effectively a comparison of 26 counties with a smoke-free law to 91 counties without a smoke-free law.
We did not find an association between smoke-free laws and persistent ear infection. This was surprising given the strong evidence in the literature for a positive association between secondhand smoke and ear infection.1,36 The adjusted OR, not adjusting for region, approached significance (OR: 0.64 [95% CI: 0.37–1.10]).
LIMITATIONS
The county-specific definition of smoke-free laws is only an approximation of individual exposure to secondhand smoke outside the home. Misclassification of exposure to smoke-free laws was possible because county smoke-free laws may not capture individual exposure to these laws. In particular, counties with a city with smoke-free laws but no county-wide smoke-free law were classified by our definition as having no smoke-free laws. Hence, youth may have lived in the city covered by the smoke-free law and thus actually were covered by a smoke-free law. This potential misclassification of smoke-free law coverage was likely not associated with respiratory outcomes, thus not producing the observed protective association.
Misclassification of current asthma was possible because self-reports were not validated by objective measures or clinical evaluations. Parental reports generally reflect physician diagnosis, but physician diagnosis of respiratory illnesses may not be consistent across the country because it depends on access and use of medical care and on physician diagnostic practices.37,38 Examining asthma-related symptoms attempted to capture some of the undiagnosed cases of asthma.
Residual confounding is possible. Parental asthma is an important risk factor for asthma in children. NHANES 1999–2006 did not collect this information for children and adolescents aged younger than 20 years, so this risk factor could not be adjusted in our model. However, having a parent with asthma may be an intermediate on the pathway between smoke-free laws and asthma status in youth. In that case, we would not want to adjust for having a parent with asthma.
One other study examined the impact of smoke-free laws and health in children. After implementation of a smoke-free law in Lexington-Fayette County, Kentucky,29 emergency-department visits for asthma declined by 18% (95% CI: 4–29) among children aged 19 years or younger. We found an adjusted 45% (95% CI: −13 to 73) decrease in odds of emergency-department visits among youth with asthma associated with a smoke-free law.
These results are consistent with other NHANES studies that have looked at cotinine and asthmatic symptoms in children.35,39 In NHANES III (1988–1994), youth with high levels of cotinine (compared with youth with low levels of cotinine) were more likely to have persistent wheeze (adjusted OR: 1.3 [95% CI 0.8–2.1])35 and moderate to severe asthma (adjusted OR: 2.7 [95% CI: 1.1–6.8]).39 Our results also are consistent with reviews of the effect of secondhand smoke on children's health, where there is stronger evidence for an association with asthmatic symptoms and severity than the onset of asthma.1,40
CONCLUSIONS
Cotinine levels have decreased by almost 60% (from 0.12 ng/mL in 1988–1994 to 0.05 ng/mL in 2003–2006) among children without exposure to secondhand smoke in the home.41 This reduction is likely because of the implementation of smoke-free laws. Currently, 74% of the population is covered by a smoke-free law.42
This study shows that not only are smoke-free laws associated with reduced exposure to secondhand smoke in children, but that they are associated with fewer respiratory symptoms as well. Youth living in a county with a smoke-free law had decreased odds of having respiratory symptoms (persistent wheeze, chronic night cough, or wheeze-mediation use) compared with youth living in a county without a smoke-free law. Eliminating exposure to secondhand smoke through the implementation of smoke-free laws may improve the respiratory health of children.
ACKNOWLEDGMENTS
This research was funded by the Flight Attendants Medical Research Institute Clinical Innovator Award. Dr Dove was supported, in part, by a National Institute of Environmental Health Sciences Training Program in Environmental Epidemiology (grant 2 T32 ES07069-26).
FINANCIAL DISCLOSURE: The authors have indicated that they have no personal financial relationships relevant to this article to disclose.
- NHANES
- National Health and Nutrition Examination Survey
- OR
- odds ratio
- CI
- confidence interval
REFERENCES
- 1. US Department of Health and Human Services The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, Office on Smoking and Health; 2006 [Google Scholar]
- 2. US Environmental Protection Agency Respiratory Health Effects of Passive Smoking: Lung Cancer and Other Disorders. Washington, DC: US Environmental Protection Agency; 1992. EPA publication EPA/600/6–90/006F [Google Scholar]
- 3. Repace J. Respirable particles and carcinogens in the air of Delaware hospitality venues before and after a smoking ban. J Occup Environ Med. 2004;46(9):887–905 [DOI] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention Indoor air quality in hospitality venues before and after implementation of a clean indoor air law: western New York, 2003. MMWR Morb Mortal Wkly Rep. 2004;53(44):1038–1041 [PubMed] [Google Scholar]
- 5. Connolly G, Carpenter C, Alpert HR, Skeer M. Evaluation of the Massachusetts smoke-free workplace law: a preliminary report. Available at: http://repositories.cdlib.org/context/tc/article/1180/type/pdf/viewcontent Accessed November 17, 2010
- 6. Repace JL, Hyde JN, Brugge D. Air pollution in Boston bars before and after a smoking ban. BMC Public Health. 2006;6:266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Valente P, Forastiere F, Bacosi A, et al. Exposure to fine and ultrafine particles from secondhand smoke in public places before and after the smoking ban, Italy 2005. Tob Control. 2007;16(5):312–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pickett MS, Schober SE, Brody DJ, Curtin LR, Giovino GA. Smoke-free laws and secondhand smoke exposure in US non-smoking adults, 1999–2002. Tob Control. 2006;15(4):302–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fernando D, Jefferson F, Woodward A, et al. Legislation reduces exposure to second-hand smoke in New Zealand bars by about 90%. Tob Control. 2007;16(4):235–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Farrelly MC, Nonnemaker JM, Chou R, Hyland A, Peterson KK, Bauer UE. Changes in hospitality workers' exposure to secondhand smoke following the implementation of New York's smoke-free law. Tob Control. 2005;14(4):236–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mulcahy M, Evans DS, Hammond SK, Repace JL, Byrne M. Secondhand smoke exposure and risk following the Irish smoking ban: an assessment of salivary cotinine concentrations in hotel workers and air nicotine levels in bars. Tob Control. 2005;14(6):384–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ. 2007;335(7619):549–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Allwright S, Paul G, Greiner B, et al. Legislation for smoke-free workplaces and health of bar workers in Ireland: before and after study. BMJ. 2005;331(7525):1117–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eisner MD, Smith AK, Blanc PD. Bartenders' respiratory health after establishment of smoke-free bars and taverns. JAMA. 1998;280(22):1909–1914 [DOI] [PubMed] [Google Scholar]
- 15. Menzies D, Nair A, Williamson PA, et al. Respiratory symptoms, pulmonary function, and markers of inflammation among bar workers before and after a legislative ban on smoking in public places. JAMA. 2006;296(14):1742–1748 [DOI] [PubMed] [Google Scholar]
- 16. Eagan TM, Hetland J, Aaro LE. Decline in respiratory symptoms in service workers five months after a public smoking ban. Tob Control. 2006;15(3):242–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Larsson M, Boëthius G, Axelsson S, Montgomery SM. Exposure to environmental tobacco smoke and health effects among hospitality workers in Sweden: before and after the implementation of a smoke-free law. Scand J Work Environ Health. 2008;34(4):267–277 [DOI] [PubMed] [Google Scholar]
- 18. Akhtar PC, Currie DB, Currie CE, et al. Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ. 2007;335(7619):545–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dove MS, Dockery DW, Connolly GW. Smoke-free air laws and secondhand smoke exposure among nonsmoking youth, NHANES 1999–2006. Pediatrics. 2010;126(1):80–87 [DOI] [PubMed] [Google Scholar]
- 20. Akhtar PC, Haw SJ, Currie DB, Zachary R, Currie CE. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control. 2009;18(5):409–415 [DOI] [PubMed] [Google Scholar]
- 21. Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii42–iii50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mannino DM, Caraballo R, Benowitz N, Repace J. Predictors of cotinine levels in US children: data from the third national health and nutrition examination survey. Chest. 2001;120(3):718–724 [DOI] [PubMed] [Google Scholar]
- 23. Jarvis MJ, Goddard E, Higgins V, et al. Children's exposure to passive smoking in England since the 1980s: cotinine evidence from population surveys. BMJ. 2000;321(7257):343–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jarvis MJ, Strachan DP, Feyerabend C. Determinants of passive smoking in children in Edinburgh, Scotland. Am J Public Health. 1992;82(9):1225–1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jarvis MJ, McNeill AD, Bryant A, Russell MA. Factors determining exposure to passive smoking in young adults living at home: quantitative analysis using saliva cotinine concentrations. Int J Epidemiol. 1991;20(1):26–31 [DOI] [PubMed] [Google Scholar]
- 26. Glantz SA. Meta-analysis of the effects of smokefree laws on acute myocardial infarction: an update. Prev Med. 2008;47(4):452–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation. 2009;120(14):1373–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places. J Am Coll Cardiol. 2009;54(14):1249–1255 [DOI] [PubMed] [Google Scholar]
- 29. Rayens MK, Burkhart PV, Zhang M, et al. Reduction in asthma-related emergency department visits after implementation of a smoke-free law. J Allergy Clin Immunol. 2008;122(3):537–541 [DOI] [PubMed] [Google Scholar]
- 30. National Centers for Health Statistics National Health and Nutrition Examination Survey analytic guidelines. Available at: www.cdc.gov/nchs/data/nhanes/nhanes3/nh3gui.pdf Accessed November 30, 2007
- 31. Pirkle JL, Flegal KM, Bernert JT, Brody DJ, Etzel RA, Maurer KR. Exposure of the US population to environmental tobacco smoke. JAMA. 1996;275(16):1233–1240 [PubMed] [Google Scholar]
- 32. American Nonsmokers' Rights Foundation Chronological table of U.S. population protected by 100% smokefree state or local laws. Available at: www.no-smoke.org/pdf/effectivepopulationlist.pdf Accessed January 28, 2010
- 33. Matt GE, Quintana PJ, Hovell MF, et al. Households contaminated by environmental tobacco smoke: sources of infant exposures. Tob Control. 2004;13(1):29–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jarvis MJ, Mindell J, Gilmore A, Feyerabend C, West R. Smoke-free homes in England: prevalence, trends and validation by cotinine in children. Tob Control. 2009;18(6):491–495 [DOI] [PubMed] [Google Scholar]
- 35. Mannino DM, Moorman JE, Kingsley B, Rose D, Repace J. Health effects related to environmental tobacco smoke exposure in children in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Pediatr Adolesc Med. 2001;155(1):36–41 [DOI] [PubMed] [Google Scholar]
- 36. Strachan DP, Cook DG. Health effects of passive smoking: 4. parental smoking, middle ear disease and adenotonsillectomy in children. Thorax. 1998;53(1):50–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Silver EJ, Crain EF, Weiss KB. Burden of wheezing illness among U.S. children reported by parents not to have asthma. J Asthma. 1998;35(5):437–443 [DOI] [PubMed] [Google Scholar]
- 38. Yeatts K, Davis KJ, Sotir M, Herget C, Shy C. Who gets diagnosed with asthma? Frequent wheeze among adolescents with and without a diagnosis of asthma. Pediatrics. 2003;111(5 pt 1):1046–1054 [DOI] [PubMed] [Google Scholar]
- 39. Mannino DM, Homa DM, Redd SC. Involuntary smoking and asthma severity in children: data from the Third National Health and Nutrition Examination Survey. Chest. 2002;122(2):409–415 [DOI] [PubMed] [Google Scholar]
- 40. Strachan DP, Cook DG. Health effects of passive smoking: 6. parental smoking and childhood asthma: longitudinal and case-control studies. Thorax. 1998;53(3):204–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Marano C, Schober S, Brody D, Zhang C. Secondhand tobacco smoke exposure among children and adolescents: United States, 2003–2006. Pediatrics. 2009;124(5):1299–1305 [DOI] [PubMed] [Google Scholar]
- 42.American Nonsmokers' Rights Foundation. Overview list: how many smokefree laws? [Accessed January 28, 2010]. Available at: www.no-smoke.org/pdf/mediaordlist.pdf.


