Abstract
AIMS
To explore variance in reporting continence information obtained by telephone survey with face-to-face clinician interview in a clinical setting.
METHODS
As part of a cross-sectional, epidemiologic study of incontinence prevalence among Black and White women ages 35-64 years, randomly selected households were contacted from geographic areas of known racial composition. Of 2814 women who completed a 20-minute, 137-item telephone interview, 1702 were invited for future components of the study. A subset of these women was recruited for a clinical evaluation that was conducted within a mean of 82 days (SD 38 days) following the interviews. Prior to urodynamics testing, a clinician interview was conducted inquiring about continence status. The criterion for incontinence for both the telephone interview and the clinician interview was constant: twelve or more episodes of incontinence per year. Women whose subjective reports of continence information differed between telephone and clinician interviews were designated as “switchers”.
RESULTS
Of the 394 women (222 Black, 172 White) who completed the clinical portion, 24.6% (n=97) were switchers. Switchers were four times more likely to change from continent to incontinent (80.4% N=78) than from incontinent to continent (19.4%; N=19 p=.000) and nearly three times more likely to be Black (69% N=67) than White (31%; N=30 p=.001). Telephone qualitative interviews were completed with 72 of the switchers. The primary reason for switching was changes in women’s life circumstances such as variation in seasons, activities of daily living, and health status followed by increased awareness of leakage secondary to the phone interview.
CONCLUSION
One-time subjective telephone interviews assessing incontinence symptoms may underestimate the prevalence of incontinence especially among Black women.
Keywords: incontinence, prevalence, epidemiology, race differences, response difference, switching
Introduction
Urinary incontinence (UI) is a prevalent condition affecting approximately 15-30% of women (1-5). It is more common in women than men (3,4,6-8) and the estimated annual cost of managing it is over $26 billion (9). It is also a source of distress for those involved and is a major contributor to nursing home placement (10).
Enhanced treatment and management for incontinence has come from an improved understanding of its effects on every day life largely derived from community surveys that ask women about their continence status (3,11). The key variable in these analyses are continence status, often defined as 12 or more episodes of incontinence per year (3). When women are contacted to complete a survey, they answer questions about how often they leak, however this may not be a question that they have considered previously. Given the limited opportunity to reflect on their response, it is reasonable to expect that their response might be different if they had time to observe their continence more specifically and were asked the same question again.
Prior investigations of the incidence and prevalence of incontinence in community based populations of women have employed surveys conducted over the phone, in person face-to-face interviews (12) and by mail in surveys (13). Which method is used to assess continence status appears to be determined by the research design and numbers of women necessary to reach adequate power in the sample. In general the method used for assessment has not been subject to an evaluation of the reliability and validity of the method. Only one study has aimed to determine the incidence of incontinence among a Swedish population which evaluated the reproducibility of a woman’s continence status assessment over time. Samuelsson et al (14) repeated completion of a mail survey in a subset of women (N= 113) from their sample of 491 community based women two weeks apart. In this test, retest design, the authors found only 1 woman changed her continence status, going from being classified as incontinent to continent in her response to the question “Do you suffer from involuntary loss of urine?” Thus the authors concluded that they had excellent agreement (x= .98) and could depend on the initial responses to the question as being reliable. Missing in the literature over the last decade is a comparison of different techniques of assessment to determine a woman’s continence status. Whether face-to-face interviews compared to mailed surveys yield a more reliable or valid assessment of a woman’s continence status is unclear. Wenneberg (15) conducted an investigation assessing incidence and severity of incontinence using a mail in survey in a population of community dwelling women. A subset of the sample (N=140) was then invited to have a clinical examination completed to assess the validity of the mailed survey responses. These investigators found a 98% agreement between the women’s reported continence status and their determination of her continence status based on clinical examination. While the investigators concluded the mail in survey response provided by women in the sample represented a valid assessment of their continence status, the women were not interviewed as a measure of the reliability of their assessment over time.
The purpose of this study is to explore variance in reporting continence information obtained by telephone survey with a face-to-face physician interview in a clinical setting and determine the reasons behind the variance.
Materials and Methods
This study was a secondary analysis from a larger study called Establishing the Prevalence of Incontinence (EPI) that was conducted at the University of Michigan (16). The research protocol was approved by the Institutional Review Board of the University of Michigan Medical School. A full description of the materials and methods of the parent study are found in Fenner et al (16). Steps of the study are described in Table I. In brief, the study population included community-dwelling Black and White women ages 35-64 years from three southeast Michigan counties. The sample was derived from 12,541 telephone numbers and addresses purchased from a commercial survey sampling firm that were all located throughout southeastern Michigan in regions that would allow for adequate representation of both Blacks and Whites. Prior to telephone contact, informational brochures and letters of introduction were mailed to the addresses. The letters included this introductory statement: (The) EPI Study will explore aspects of women’s health and daily life. We are particularly interested in learning more about bladder control problems (urinary incontinence). This statement prepared potential participants about the topic that would be discussed. Shortly thereafter, trained female professional telephone interviewers called households and interviewed eligible women. Eligibility criteria included being a woman between the ages of 35 and 64, who self-identified as Black or White, and who had not been pregnant in the past 12 months.
Table I.
Study Design and Timeline
| Phase | Description | Total N | Black | White |
|---|---|---|---|---|
| 1 | Assessment of Continence Status in Telephone Interview for Eligible Black or White Women | 2,814 | 1,922 | 892 |
| 2 | Invitation to Participate in Further Components of Study Design based on Racial Identity and Continence Status. | 1,702 | 1,086 | 616 |
| BI=259 | WI=268 | |||
| BC=825 | WC=347 | |||
| 3 | Continence Diary and Clinical Assessment including Urodynamic Testing for Black or White Women. After completion of a three day diary and prior to completing any physical examination or testing, the continence status questions were repeated | 394 | 222 | 172 |
| 4 | Following the Clinical Examination Visit, the “Switchers” Phenomenon was noted for Black or White Women. | 97 | 67 | 30 |
| Follow up phone calls to the participants who were “Switchers” were conducted. To identify reasons for switching, open-ended questions were asked followed by structured questions. | 72 | 50 | 22 | |
The interview assessed respondents’ demographic characteristics, health history, lifestyle factors, obstetric and gynecologic history, and continence status. During the interview women were asked to quantify the amount of leakage. Women were classified as continent or incontinent based on their answers to the following questions:
“Because this information is so important, I want to be sure that we identify any urine loss, even a small amount for only a few days. Other than a few drops right after urinating, have you involuntarily lost or leaked any amount of urine during the past twelve months?”
If yes, “In the past twelve months, did you lose urine at least twelve times or did you lose urine fewer than twelve times?
Women who answered never leaking in the past 12 months or leaking fewer than 12 times in the past twelve months were considered “Continent”. Women who answered that they leaked at least twelve times in the past twelve months were considered “Incontinent” (3). This definition has been used in prior clinical assessments of women’s experience with incontinence and while it does not use any leakage as the defining feature of incontinence as with the International Continence Society definition (17), it does provide a consistent measure that is used across other investigations.
Of 2,814 women interviewed by trained female survey personnel in a 20 minute structured interview, 1,702 were invited to participate in future components and further contact to consider undergoing clinical examination. A subset of these women were then invited to come into the clinical setting for a separate visit that included a history, physical examination and urodynamic assessment after having completed a 3-day frequency and volume diary (18). Women’s race and continence classifications, as reported during the interview phase, were used to achieve targeted group sizes necessary to answer the parent study mechanistic questions concerning urinary incontinence (Targeted group: 115 Black Incontinent, 50 Black Continent, 115 White Incontinent, and 50 White Continent).
On the day of the clinic exam, prior to physical examination, diary review or testing, they completed a face-to-face interview with a trained clinician examiner who was blinded to the woman’s prior self-reported continence status from the telephone interview. Each woman’s self-reported continence status was once again assessed during this history taking session. An assessment of “Continent” or “Incontinent” was based on the same criteria as the telephone interview. Women who answered that they never leaked or leaked less than twelve times in the past year were considered “Continent”. Women who reported leaking at least twelve times in the past year were considered “Incontinent”.
Each woman’s answers to both the telephone and clinician interviews were later compared and form the basis for this study. Any woman whose self-reported continence status changed from the telephone interview to the clinician interview was considered a “Switcher”. For example, a woman who reported never leaking on the telephone interview and then reported leaking once per day to the clinician was considered a “Switcher”.
The direction of switching was analyzed. Women could switch from continent to incontinent or from incontinent to continent. The direction of switching was determined using the following criteria:
Continent to Incontinent: Women who reported either never leaking or leaking less than twelve times per year on the telephone interview, then reported leaking twelve or more times per year to the clinician.
Incontinent to Continent: Women who reported leaking twelve or more times per year on the telephone interview, then reported either never leaking or leaking less than twelve times per year to the clinician.
All women who experienced episodes of incontinence were asked the total number of episodes. All of the data from the prior steps study design were entered into SPSS and descriptive statistics completed.
Women who were identified as switchers were later contacted by follow-up phone call by two research assistants and asked why they changed continence status. The follow-up interviews began with an open-ended question asking a woman why she had reported being either incontinent (leaking 12 or more times pear year) or continent on the phone but during the exam with the clinician they reported the opposite. They were asked “In your own words can you explain why you reported this difference?” This was followed by specific questions to assess the women’s understanding of incontinence, and the effects of the various phases of the study that might have an impact on why they switched their reports including the time between the telephone interview and the clinic exam, effects of the telephone interview, effects of the voiding diary, effects of the mode of questioning (telephone v. face-to-face) and effects of the interviewer (telephone interviewer v. clinician).
The interview responses were recorded in writing and a complete transcript of all the responses were available for review by the research team. A process of content analysis as outlined by Morgan (19) was applied to the responses. Statements made in response to the open ended question were termed “initial responses” and formed the basis for open coding categories independent of the specific questions that were asked about possible reasons for the switching that were identified apriori by the investigators. The frequency of endorsing specific reasons for switching (saying “yes that has an effect on why I changed my answer”) were tallied and compared to the open ended coding categories. The initial response categories, together with the answers to the specific questions were termed “all responses” and were reviewed for an overall understanding of the reasons women switched their status between the initial phone interview and the face-to-face clinical examination.
Results
In the parent study, the overall prevalence of incontinence for the total sample (N=2,814) was 26.5% (16). The mean frequency of incontinence by race in the parent project was 14.9 episodes per month for White women (N=892) and 14.8 episodes per month for Black women (N=1922) while the prevalence was 14.6% in Black women compared to 33.1% in White women. Of the 394 women completing the clinic exam, nearly one-fourth were “Switchers” (24.6%, N=97) (Figure 1). Switchers in this sample were four times more likely to change from Continent to Incontinent (80.4% N=78) than from Incontinent to Continent (19.4%, N=19; p<.01). The mean time interval between the initial phone interview contact and the conduct of the clinical examination was 82 days (SD 38 days) for the full sample and did not differ between the two groups of those who switched and those who did not switch.
Figure 1.
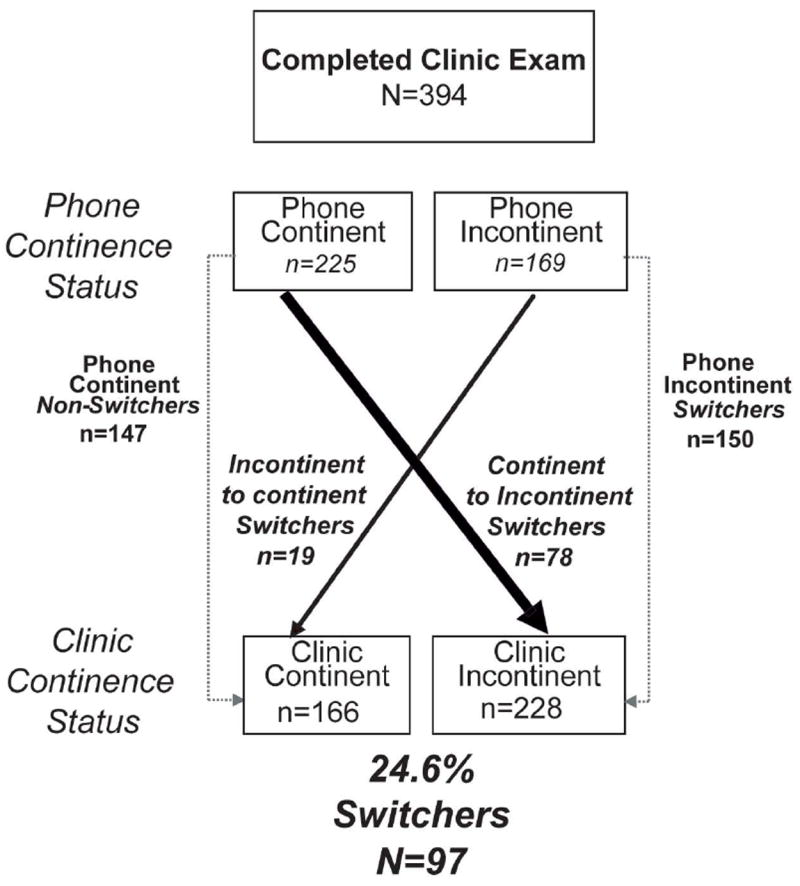
Flow diagram of phone interviews, clinic exams, diagnoses, and switching patterns.
The demographic information for Switchers (N=97) is provided in Table II and educational level in Table III. When the groups were divided both by race and the continence status they reported on the phone interview compared to the face to face interview “Switchers” were nearly three times more likely to be Black (69% N=67) than White (31%; N=30 p=.001) (Figure 2). At the time of the clinic visit, Switchers (N=97) reported fewer incontinence episodes per year (median = 48) than non-Switchers (median=360; p<.01). However, it should be noted that this frequency of incontinence episodes was substantially higher than the twelve times per year cut-off. Continent to Incontinent Switchers in this sample (N=78) were twice as likely to report leaking 1-11 times per year on the telephone interview (73.1% N=57) than never leaking (26.9% N=21; p<.01). Incontinence to continent switchers had initially reported a mean frequency of leakage of 10 times per month (+/- 22.7, median 2, range 1-99 episodes per month), still well above the range of 12 times per year thus their change was unanticipated as the mean frequency rate was relatively high compared to our definition cut point of 12 episodes per year.
Table II.
Deomgraphics by Group
| Variable | TOTAL | Switcher | Non-Switcher | P Value |
|---|---|---|---|---|
| Age | 50.42 ± 8.14 | 50.08 ± 8.2 | 50.54 ± 8.13 | .9 |
| BMI | 32.5 ± 8.53 | 32.6 ± 8.31 | 32.48 ± 8.63 | .67 |
| Parity | 3.1 ± 2.3 | 3.16 ± 1.94 | 3.07 ± 2.42 | .01 |
| Vaginal Delivery | 2.24 ± 1.85 | 2.38 ± 1.67 | 2.19 ± 1.91 | .13 |
| Income | 53,583.2 ± 50159 | 47,743 ± 44,789 | 55,304 ± 51,611 | .2 |
Table III.
Educational Level by Group
| EDUCATION | <HS | HS | Some College | Grad College |
|---|---|---|---|---|
| TOTAL | 5.54 (18) | 24.62 (80) | 48.0 (156) | 21.85 (71) |
| Switcher | 3.08 (10) | 7.08 (23) | 13.54 (44) | 4.0 (13) |
| Non-Switcher | 2.46 (8) | 17.54 (57) | 34.46 (112) | 17.85 (58) |
p=.0172
Figure 2.
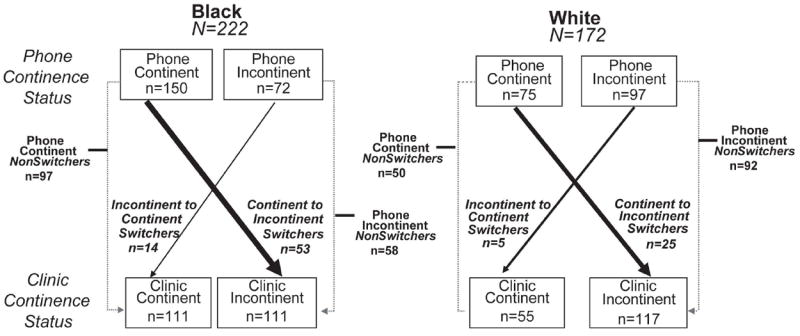
Switching patterns broken down by race.
Follow-up Calls
Of the 97 women who switched continence status, 72 were subsequently contacted and available for interview. Reasons for not participating in the interviews included being unable to contact or declining participation. The overall qualitative interview response rate was 74%. Table IV provides the responses to the initial open ended question of why their report changed. The most common reason for the change in reporting was that there was a variance in their life circumstance that led to different leakage (e.g. more coughing/sneezing due to a cold). Second most common was that they initially guessed on the phone interview and subsequently had more time to consider their answer (e.g. pressure to answer quickly, leakage too inconsistent to remember easily, didn’t think about it and just guessed).
Table IV.
Initial Response to question “Why did you switch?”* (N=72)
| Response | # respondents | % of all interviews* |
|---|---|---|
| Life circumstances changed between phone call and clinic exam | 36 | 50% |
| The initial response was a guess | 16 | 22% |
| Unable to recall why they reported a difference | 11 | 15% |
| Unclear on the definition of incontinence | 10 | 14% |
| The report was incorrect | 7 | 11% |
| Voiding diary increased awareness | 3 | 4% |
| Phone Interview Increased Awareness | 2 | 3% |
Some respondents gave more than one reason in their initial response
Table V shows a classification of women’s reasons for changing status that takes into account both the results of the open-ended initial question as well as the specific questions using the investigator generated reasons. As was true of the open-ended question, most women reported that something specific changed that led to different leakage or that there was an increased awareness after the initial phone interview. They also noted an increased awareness as a result of the voiding diary which was part of the parent study protocol which led them to revise their response. While most women endorsed these two primary reasons for changing their response, many women had multiple responses in multiple categories for both initial responses and responses to specific reasons thus demonstrating the complexity that occurs when someone is initially asked about their continence status. As a result, the percentages reported in Table V in either category total more than 100%. For the response category of “something changing in a woman’s life” circumstances, it is noted that the types of change vary widely. These include variation in activities of daily living such as no longer working, increasing or decreasing exercise, changes in health status (colds, allergies, coughs, urinary tract infections), having surgery, medication use, seasonal variance between assessments, the experience of stress, difference in drinking and voiding patterns, and changes ascribed to bodily variables such as weight loss, menopause and unexplained differences in actual leakage. Thus the category of “something changing in a woman’s life” is very broad but highly consistent with women’s actual life experiences over time and across seasons.
Table V.
Open Ended Initial and Directed Responses (N=72)
| Category | # Respondents | % All Interviews |
|---|---|---|
| Daily Activities Changed | 41 | 57% |
| Phone Interview Increased Awareness | 39 | 54% |
| Voiding Diary Increased Awareness | 36 | 50% |
| Guessed for the initial response | 27 | 38% |
| Did not understand the definition of Incontinence | 26 | 36% |
| Phone compared to Face Interview made a difference | 16 | 22% |
| Interviewer asking made a difference compared to a Physician asking | 11 | 15% |
| No Idea, “No Clue” | 10 | 14% |
| One of the Answers was incorrect | 8 | 11% |
Discussion
The finding that one-fourth of women completing both a phone interview and clinic exam switched their report of continence warrants consideration in interpreting the results of one-time telephone questionnaires for assessing incontinence. The predominant change noted was from the continent to incontinent status. The primary reasons women changed their status in this direction were two fold, first their life circumstances changed such that true variance was experienced between the phone and clinical interviews. The experience of seasonal allergies, illness, surgery, medication use, activity patterns, or other bodily changes caused a change in their experience of leaking. This phenomenon reflects the well known variability and dynamic nature of incontinence (12,14). Even though we ask questions in the context of what has happened during the last year, respondents seem to be influenced by their recent experience. Second, between the two interviews, women had become more attuned to their experience of leaking and noted it with more precision. Many women who changed their report said they originally guessed and subsequently became more aware of the condition following the phone interview which caused them to better recognize how often they leaked. Thus for some women the phone interview served as an impetus to attend to the actual frequency of incontinence that they experienced compared to having a subjective sense about how much it might be occurring.
For women who switched from incontinent to continent, we found that they changed their report of urine leakage because they did experience leakage inconsistently and less frequently than initially reported. This finding may reflect real variation in continence from one time to another and has been documented in other community based studies of the prevalence of incontinence over time (12,14). Overall the reasons for switching; life changes, increased awareness and variation in experience over time reflect the real life experience of incontinence which is quite variable from season to season, with changes in activity or health such that a quick answer to a single question about a woman’s continence status may not be as accurate.
Alternatively, the definition of continence status can be considered. According to the International Continence Society, the definition of incontinence is the experience of any leakage, regardless of amount or duration (17). This definition does not consider the potential implications of the leakage such as bother or life style impact which are important predictors of who would seek health care services for their condition (16). Regardless of the number of episodes chosen, if the condition of incontinence is considered as a dichotomous variable, meaning a women either has it or does not have it, then the swtichers phenomenon is important to consider. If a woman’s continence status is considered as a continuous variable in study designs, such that the dynamic nature is taken into account and actual episode of leaking are considered over time, then the potential risk of underestimation or overestimation of the presence of incontinence would be reduced.
In the parent project, a method of confirming the reliability and validity of the method of assessing incontinence status was not prospectively embedded in the design. The question of how face to face compared to telephone interviews compare in their stability of assessing continence status is unknown. Under the rubric of validation and reliability testing, comparisons between prior use of a survey in face to face interviews to now using it in phone surveys have been conducted for selected health conditions. Investigators have been able to demonstrate a high degree of agreement between the two methods in mental health research (20-22) in the assessment of activities of daily living post hospital discharge for community populations (23-24) and in the assessment of fecal incontinence (25) and dietary recall comparing telephone and household surveys in a rural setting (26). One theme within these studies is that when there is a difference for any section of the survey instrument, it was associated with a lesser assessment of the severity of the health condition. For example in the assessment of health related disability post hospital discharge, the group with the greatest degree of disability in face to face interviews provided a lesser assessment of their disability in the phone interview (24) suggesting that telephone interviews may underestimate the prevalence of more severe forms of a condition.
Specific to the experience of incontinence and activities of daily living, Geller et al conducted a validation study of the use of the Pelvic Floor Distress Inventory (PFDI) and the Pelvic Floor Impact Questionnaire (PFIQ) using both pencil and paper survey methods and telephone survey methods (27). In this investigation, the scores on the questionnaires were not significantly different and therefore the authors concluded their use in phone surveys would aid in expanding the state of the science related to the epidemlogical understanding of women’s experiences with pelvic floor disorders and their impact on their daily lives (27).
In contrast to the validation studies which were reported above, our goal in the parent study was to survey a community sample of women about the incidence of incontinence and then recruit from within that sample for women who met specific continence and racial identity criteria. This study is not and should not be interpreted as a validation study. The switchers’ phenomenon emerged as a practical matter in our attempts to follow our parent study protocol. The identification of the switcher phenomena was a secondary observation made in the process of evaluating our sample demographics and adherence to our study protocols which required a specified number of women based on their continence status. The switcher phenomenon affected our recruitment efforts and thus became a matter worth further exploration resulting in the telephone interview follow up. Our desire to learn more about why women changed their reports and whether there were study protocol changes we should make initially spurred the qualitative evaluation of the switchers phenomenon.
The opportunity to conduct one time phone or mailed surveys of larger numbers of women in community settings is critical to advancing our epidemiological understanding of the experience of incontinence. These results should not be seen as undermining the value of these studies, but rather as a way to understand how this type of large population information varies from the information available in more detailed clinical assessment. The findings point to the potential need for follow-up assessments either within the survey design or in the overall study design using more than one method or question to verify the actual experience of incontinence. It is also possible that more detailed questioning about the type of incontinence, stress, urge, mixed, or other, might have elicited more detailed consideration of their responses. Doing this detailed type of question in contrast to the more global assessment that was done in this study, is an option for future investigations. This may be necessary to account for initial guessing, heightened awareness, and actual changes affecting leakage which in turn reflect the real life experience of incontinence for many women. The practical constraints and costs of bringing women into the clinical setting as a follow up step in research protocols is acknowledged. As an alternative, the results of this study can be used to note that an underestimation may be a possible limitation of using the one time self report method of assessing a woman’s experience of incontinence. As demonstrated by this study, this limitation is particularly important to consider when comparing black and white women’s experiences of incontinence.
Finally, this study’s population is very specific – women who were black or white, ages 35-64, not pregnant, living in Southeast Michigan who had agreed to a telephone interview as well as an invitation for a clinic exam who then completed the clinic exam. The population specificity should be considered in comparing these results to other communities or populations. The specific reasons for noting a greater difference between Black and White women’s switching rates is unclear. It is known in general the incidence rates of incontinence is lower in Black women (12,16) and such that the switching difference based on race may be secondary to less familiarity with the experience and potentially limited consideration of it as a problem within diverse community based sample of women. Further exploration and analysis is necessary to determine the comparability of this sample to other populations, including the women in this study who did not complete the clinic evaluation or who were not available for the telephone survey follow up. Further evaluation of the rationale for racial differences in response to the switching phenomenon are also indicated.
Conclusion
Based on the “Switcher” phenomenon, one-time subjective questionnaires assessing incontinence symptoms may underestimate incontinence prevalence and may not accurately capture many women’s actual life experiences with incontinence. Depending on the goal of an investigation this potential limitation should be considered in future study designs, particularly with racially mixed populations of women.
Acknowledgments
Funders
Financial Support for the project from National Institute of Child Health & Human Development 1 R01 HD/AG41123 with additional investigator support from Office for Research on Women’s Health SCOR on Sex and Gender Factors Affecting Women’s P50 HD044406
References
- 1.Brown JS, Grady D, Ouslander JG, Herzog AR, Varner RE, Posner SF. Prevalence of urinary incontinence and associated risk factors in postmenopausal women. Obstet Gynecol. 1999;94(1):66–70. doi: 10.1016/s0029-7844(99)00263-x. [DOI] [PubMed] [Google Scholar]
- 2.Burgio KL, Matthews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged women. J Urol. 1991;146:1255–9. doi: 10.1016/s0022-5347(17)38063-1. [DOI] [PubMed] [Google Scholar]
- 3.Diokno AC, Brock BM, Brown MB, Herzog AR. Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly. J Urol. 1986 Nov;136(5):1022–5. [PubMed] [Google Scholar]
- 4.Lagace EA, Hansen W, Hickner JM. Prevalence and severity of urinary incontinence in ambulatory adults: An UPRNet study. J Fam Practice. 1993;36:610–14. [PubMed] [Google Scholar]
- 5.Nygaard IE, Lemke JH. Urinary incontinence in rural older women: prevalence, incidence and remission. J Am Geriatr Soc. 1996;44:1049–54. doi: 10.1111/j.1532-5415.1996.tb02936.x. [DOI] [PubMed] [Google Scholar]
- 6.Brocklehurst JC. Urinary incontinence in the community-analysis of a MORI poll. Br Med J. 1993;306:832–4. doi: 10.1136/bmj.306.6881.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Brien J, Austin M, Sethi P, O’Boyle P. Urinary incontinence: Prevalence, need for treatment and effectiveness of interventions by nurses. Br Med J. 1991;303:1308–1312. doi: 10.1136/bmj.303.6813.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc. 1998;46(4):473–80. doi: 10.1111/j.1532-5415.1998.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 9.Wagner TH, Wu TW. Economic costs of urinary incontinence in 1995. Urol. 1998;51:355–61. doi: 10.1016/s0090-4295(97)00623-7. [DOI] [PubMed] [Google Scholar]
- 10.Coward RT, Horne C, Peek CW. Predicting nursing home admissions among incontinent older adults: a comparison of residential differences across six years. Gerontol. 1995;35:732–43. doi: 10.1093/geront/35.6.732. [DOI] [PubMed] [Google Scholar]
- 11.Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol. 2007 Jun;109(6):1396–403. doi: 10.1097/01.AOG.0000263469.68106.90. [DOI] [PubMed] [Google Scholar]
- 12.Komesu Y, Rogers R, Schrader R, Lewis Incidence and remission of urinary inctontinence in a community-based population of women ≥50 years. Int Urogynecol J. 2009;20:581–589. doi: 10.1007/s00192-009-0838-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyles SH, Li H, Mori T, Osterweil P, Guise JM. Effect of Mode of Delivery on the incidence of urinary incontinence in primiparous women. Obstet Gyn. 2009;113(1):134–141. doi: 10.1097/AOG.0b013e318191bb37. [DOI] [PubMed] [Google Scholar]
- 14.Samuelsson E, Victor FTA, Svardsudd KF. Five-year incidence and remission rates of female urinary incontinence in Swedish population less than 65 years old. Am J Obstet Gynecol. 2000;183(3):568–574. doi: 10.1067/mob.2000.106763. [DOI] [PubMed] [Google Scholar]
- 15.Wennberg AL, Molander U, Magnus F, Edlund C, Peeker R, Milsom I. A longitudinal population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in women. European Urology. 2009;55:783–791. doi: 10.1016/j.eururo.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Fenner DE, Trowbridge ER, Patel DL, Fultz NH, Miller JM, Howard D, DeLancey JOL. Establishing the Prevalence of Incontinence Study: Racial Differences in Women’s Patterns of Urinary Incontinence. J Urol. 2008;179:1455–1460. doi: 10.1016/j.juro.2007.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardization of terminology of lower urinary tract function. Neurourol Urodyn. 1988;7:403–26. [PubMed] [Google Scholar]
- 18.Nygaard I, Holcomb R. Reproducibility of the seven-day voiding diary in women with stress urinary incontinence. Int Urogynecol J. 2000;11:15–7. doi: 10.1007/pl00004021. [DOI] [PubMed] [Google Scholar]
- 19.Morgan DL. Pearls, pith, and provocation: qualitative content analysis: a guide to paths not taken. Qualitative Health Research. 1993;3(1):112–121. doi: 10.1177/104973239300300107. [DOI] [PubMed] [Google Scholar]
- 20.Aneshensel CS, Frerichs RR, Clark VA, Yokopenic PA. Measuring depression in the community: a comparison of telephone and personal interviews. Public Opin Q. 1982;46(1):110–21. doi: 10.1086/268703. [DOI] [PubMed] [Google Scholar]
- 21.Sobin E, Weissman MM, Goldstein RB, Adams P. Diagnostic interviewing for family studies: comparing telephone and face to face methods for diagnosis of lifetime psychiatric disorders. Psychiatr Genet. 1993;3:227–233. [Google Scholar]
- 22.Aziz MM, Kenford S. Comparability of telephone and face to face interviews in assessing parients with post traumatic stress disorder. Journal of Psychiatric Pracitce. 2004;10(5):307–313. doi: 10.1097/00131746-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Crippa JA, de Lima Osorio F, Del-Ben CM, Filho AS, Freitas MC, Loureiro SR. Comparability between telephone and face-to-face structured clinical interview for DSM-IV in assessing social anxiety disorder. Perspect Psychiatr Care. 2008 Oct;44(4):241–7. doi: 10.1111/j.1744-6163.2008.00183.x. [DOI] [PubMed] [Google Scholar]
- 24.Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154(11):1593–8. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- 25.Korner-Bitensky N, Wood-Dauphinee S, Siemiatycki J, Shapiro S, Becker R. Health related information post discharge: telephone versus face-to-face interviewing. Arch Phys Med Rehabil. 1994 Dec;75(12):1287–96. [PubMed] [Google Scholar]
- 26.Korner-Bitensky N, Wood-Dauphinee S. Barthel Index Information elicited over the telephone. Is it reliable? Am J Phys Med Rehabil. 1995 Jan-Feb;74(1):9–18. doi: 10.1097/00002060-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Kwon S, Visco AG, Fitzgerald MP, Ye W, Whitehead WE. Validity and reliability of the Modified Manchester Health Queastionaire in assessing patients with fecal incontinence. Dis Colon Rectum. 2006;48:323–31. doi: 10.1007/s10350-004-0899-y. [DOI] [PubMed] [Google Scholar]
- 28.Bogle M, et al. Validity of a telephone-administered 24 hour dietary recall in telephone and non-telephone households in the rural lower Mississippi Delta region. J Am Diet Assoc. 2001 Feb;101(2):216–22. doi: 10.1016/S0002-8223(01)00056-6. [DOI] [PubMed] [Google Scholar]
- 29.Geller EJ, Barbee ER, Wu JM, et al. Validation of telephone administration of 2 condition-specific quality-of-life questionnaires. Am J Obstet Gynecol. 2007;197:632.e1–632.e4. doi: 10.1016/j.ajog.2007.08.019. [DOI] [PubMed] [Google Scholar]


