Abstract
Background In India, coping mechanisms for inpatient care costs have been explored in rural areas, but seldom among urbanites. This study aims to explore and compare mechanisms employed by the urban and rural poor for coping with inpatient expenditures, in order to help identify formal mechanisms and policies to provide improved social protection for health care.
Methods A three-step methodology was used: (1) six focus-group discussions; (2) 800 exit survey interviews with users of public and private facilities in both urban and rural areas; and (3) 18 in-depth interviews with poor (below 30th percentile of socio-economic status) hospital users, to explore coping mechanisms in greater depth.
Results Users of public hospitals, in both urban and rural areas, were poor relative to users of private hospitals. Median expenditures per day were much higher at private than at public facilities. Most respondents using public facilities (in both urban and rural areas) were able to pay out of their savings or income; or by borrowing from friends, family or employer. Those using private facilities were more likely to report selling land or other assets as the primary source of coping (particularly in rural areas) and they were more likely to have to borrow money at interest (particularly in urban areas). Poor individuals who used private facilities cited as reasons their closer proximity and higher perceived quality of care.
Conclusions In India, national and state governments should invest in improving the quality and access of public first-referral hospitals. This should be done selectively—with a focus, for example, on rural areas and urban slum areas—in order to promote a more equitable distribution of resources. Policy makers should continue to explore and support efforts to provide financial protection through insurance mechanisms. Past experience suggests that these efforts must be carefully monitored to ensure that the poorer among the insured are able to access scheme benefits, and the quality and quantity of health care provided must be monitored and regulated.
Keywords: Hospitalization, expenditures, coping strategies, insurance, social capital, India
KEY MESSAGES.
In both urban and rural areas, respondents using public hospitals were poorer than those using private hospitals.
While most of those hospitalized at public facilities were able to pay out of savings or income, or by borrowing from friends, family or employer, individuals using private facilities were more likely to sell land or other assets (rural areas) and they were more likely to have to borrow money at interest (urban areas).
In India, national and state governments should invest in improving the quality and access of public first-referral hospitals. This should be done selectively—focusing on rural areas and urban slum areas—to promote a more equitable distribution of resources.
Introduction
The aim of this study is to explore mechanisms employed by the urban and rural poor for coping with inpatient expenditures, in order to help identify formal mechanisms and policies to provide improved social protection for health care for these populations.
Background
In India, health care costs, and those for inpatient care in particular, pose a barrier to seeking health care, and can be a major cause of indebtedness and impoverishment. Three-quarters (1999 to 2003 estimates) of total health care spending flows from individuals and households directly to health care providers (predominantly private) in the form of out-of-pocket payments (World Health Organization 2006a). On average, the poorest quintile of Indians is 2.6 times more likely than the richest to not seek medical treatment when ill, and only one-sixth as likely to be hospitalized (Peters et al. 2002). In India, 31.1% of individuals fall below the World Bank’s absolute poverty threshold of US$1.08 per day. Subtraction of out-of-pocket payments for health care increases the poverty headcount to 34.8%, representing over 37 million people (van Doorslaer et al. 2006). A study of more than 3000 households in 20 Gujarati villages found that, over 25 years, among all households that fell into poverty, ill health and related expenses were critical in 85% of cases (Krishna et al. 2003).
In Gujarat (as in all India), the poor are more likely than the rich to choose public rather than private inpatient facilities (Mahal et al. 2000). Nonetheless, 54.9% of all hospitalizations among the rural population below the poverty line (BPL) of Gujarat, and 51.1% of all hospitalizations among the urban BPL population, are in private hospitals.1 Hospital charges faced by the urban BPL population are higher than those faced by their rural counterparts, at both public and private facilities. For example, the average charge per day of hospitalization in a private facility, for BPL patients, is Rs. 125.7 in urban Gujarat compared with only Rs. 57.8 in rural Gujarat (Mahal et al. 2000).
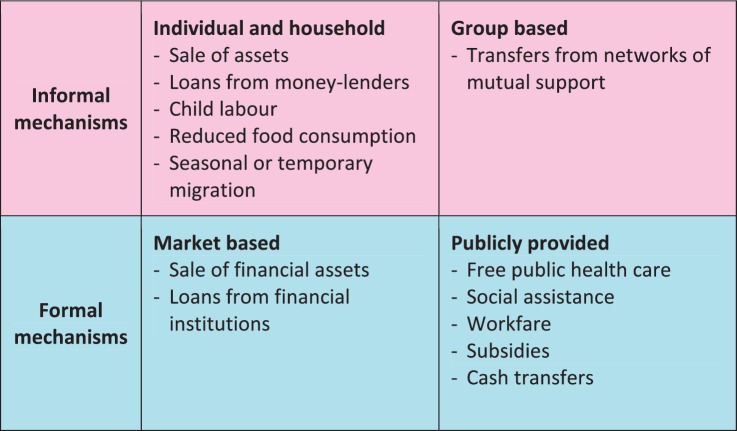
The term ‘coping strategies’ was coined during the 1980s in the literature on household responses to lack of food and nutrition. The term refers to the mechanisms or activities undertaken by members of a household that help them survive through a crisis situation (McIntyre and Thiede 2007). Figure 1 lists some of the measures available for coping with financial shocks. The strategies have been categorized as informal (or traditional) and formal, i.e. market-based or publicly provided (World Bank 2001). In India, formal mechanisms are largely inaccessible to the poor. In theory, government provision of universal and free health care should cover the poor, but in practice it often does not. Private-for-profit health insurance and government social insurance are geared primarily towards India’s formal sector, comprising less than 10% of the total population (Gupta and Trivedi 2005).
Figure 1.
Mechanisms for coping with financial shocks. Source: World Bank (2001)
There have been many studies of the informal mechanisms used by poor rural households for coping with financial shocks, and more specifically those related to medical expenditure (Rosenzweig 1988; Townsend 1994; Kochar 1995; Krishna et al. 2003). In rural areas, when a shock hits, people cope by selling livestock or other assets, or calling on support networks for transfers or loans. If these mechanisms fail or fall short, households may increase their labour supply, working more hours or involving more household members (women or children), or borrow from a private lender at high rates of interest. In Gujarat, the rates of interest on these loans start as high as 5–7% per month (Krishna et al. 2003). If all else fails, households reduce consumption—including the consumption of medical services and goods—and go hungry.
Far less is known about coping strategies among the poor living in urban areas, including those who have migrated from rural areas for work. It has, however, been argued that the strong social networks that provide mutual insurance in India are actually a deterrent to mobility, and explain rates of urbanization that are low relative to other low-income countries (Munshi and Rosenzweig 2005). These authors show, based on 1982 and 1999 survey data, that migration (not necessarily to urban areas, but away from one’s native village) is associated with a significantly lower probability of receiving loans from friends or family. International literature suggests that those who have migrated for work are particularly vulnerable as they are more likely to work longer hours, live and work in poorer conditions, be socially isolated and lack access to basic amenities (International Organisation for Migration 2005). In 2002, a World Bank consultation highlighted the fact that, despite a growing population of urban poor (27% of 285 million people), for whom many health indicators are as bad or worse than for poor rural populations, there has been little analytical work on health issues of the urban poor (World Bank 2002).
Methods
Study setting
The study was conducted in Vadodara District, Gujarat State, between October 2007 and December 2008. Vadodara District has a population of 3.6 million people, 52.1% of whom are male and 47.9% female (Office of the Registrar General 2001). The district’s only city, Vadodara, is the third largest city in the state of Gujarat and the sixteenth largest in India (UNDP and World Bank 1999). In 2001, the urban population of Vadodara accounted for 45% (1 647 317) of the total district population. Like many other Indian cities, Vadodara is growing rapidly, from only 950 000 in 1981, to 1.3 million in 1991 and 3.6 million in 2001 (Office of the Registrar General 2001). The dominant industries in Vadodara city are petrochemicals, fertilizers, pharmaceuticals, cotton textiles and machine tools. Agriculture predominates in rural areas, with the major crops being: rice, wheat, yellow peas, grams, oilseeds, groundnut, tobacco, cotton and sugarcane.
Step 1: Focus group discussions
Focus group discussions (FGDs) were conducted as the first step in a three-step methodology. The FGDs aimed to: (i) identify commonly used sources of inpatient care among poorer populations; and (ii) explore strategies for coping with the costs of inpatient care, to help develop a list of options for questions in a hospital exit survey. Three FGDs were conducted in urban areas and three in rural areas. In Vadodara city, three different urban slum areas were purposefully selected. Vadodara slum areas are quite segregated according to the State of origin of the residents; our FGD groups consisted of migrants from Uttar Pradesh, Rajasthan and Maharashtra. Eight to 12 adult respondents (>18 years of age) were included in each FGD, including both men and women, and only those who had experienced hospitalization within the previous year and had migrated to the city within the last 5 years, as recent migrants were expected to be the most vulnerable to the costs of health care. In rural areas, three sub-districts (out of 12 in Vadodara) were randomly selected, and within each sub-district a poor residential area (usually a ‘para’ or neighbourhood) on the periphery of a village was purposefully selected. Group size and inclusion/exclusion criteria were the same as in urban areas, with the exclusion of the migration criterion.
FGDs were conducted in the Gujarati language by the Principal Investigator (RJ) and with the permission of respondents, recorded using a digital video recorder. They were transcribed in English, and analysed and coded in MS Word.
Step 2: Exit surveys
The goals of the exit survey were: (i) to document costs of hospitalization (both medical and non-medical) at private and public facilities, and in urban and rural areas; (ii) to explore the utilization of different coping strategies; and (iii) to identify poor households who could be interviewed, in-depth, in the final step of field-work.
Eight-hundred respondents were sought, with equal numbers in urban and rural areas, and equal numbers using the public and private hospitals that were most commonly mentioned in the focus-group discussions. In rural areas, respondents had to be resident in the three sub-districts included in Step 1. Urban respondents had to be resident in Vadodara city. In both urban and rural areas, hospitals were purposively selected based on frequency of use reported by respondents in the FGDs. The rural hospitals tended to be much smaller than the urban facilities; hospitals had to have a minimum of 15 inpatient beds in order to be included in the study.
One hundred exit surveys were conducted at each of four urban hospitals (two public and two private). Given the smaller size of rural hospitals, interviews had to be conducted at six facilities (three public and three private), with 65–70 respondents per hospital. Potential respondents were identified by having hospital administrators provide a list of patients to be discharged on the day of exit interviews. Exit interviews were restricted to those hospitalized in general wards (thus excluding those who paid extra—both at public and private facilities—to stay in private rooms). Patients (and their families) were approached for interviews immediately after they made their payments and had received their discharge cards. In order to be included in the exit surveys, respondents had to be: (i) older than 18 years of age; (ii) hospitalized for more than 24 hours; and (iii) resident in the corresponding area (either urban or rural) at the time of the interview (for example, residents of a rural village hospitalized in urban facilities were excluded from the study).
Interviews were conducted inside hospital premises by RJ and three trained investigators. Data were collected using an interview schedule which was filled out by the interviewer. The following data were collected:
Place of residence and place of origin;
Details as to when they moved to their current place of residence;
Cause of hospitalization;
Expenditures on hospitalization, with breakdown by type of costs, e.g. medicines, doctors’ fees, etc;
Indicators of socio-economic status.
In most cases the patient was interviewed (generally with their accompanying family present). In those cases where patients were unable to respond (for example, if the patient remained ill or unresponsive at the time of discharge) we interviewed an accompanying household member instead. As anticipated, 800 exit interviews were conducted. In no case did potential respondents refuse to participate in the interviews.
Data were double-entered into an Excel database, and cross-checked for any inconsistencies. Analyses were conducted using the statistical software STATA. As a proxy for wealth, we constructed a socio-economic status (SES) index based on household assets and utilities, allowing the weights of these assets to be determined by principal components analysis (PCA) (Filmer and Pritchett 2001). All 26 assets and utilities variables from the survey were retained in the index (see Appendix 1) and weighted based on PCA. Twenty-one categorical variables were converted to dichotomous variables as this provided for greater discrimination amongst poorer households. Ultimately, the index comprised 25 dichotomous variables and one continuous variable (number of rooms). The index was validated by examining the likelihood of ownership of specific assets (or utilities) by decile. For example, it can be seen that no respondent below the 50th percentile reported owning a refrigerator, compared with 65% of respondents in the wealthiest decile (Appendix 1). Respondents were grouped by quintile or decile; in both cases the 1st was the poorest.
Step 3: In-depth interviews
After the exit surveys, 18 in-depth interviews were carried out in order to explore further household coping strategies. We aimed to interview people from the poorest three deciles by SES. The respondents were stratified according to type of hospital used (half had used public facilities and half private), place of residence (6 rural and 12 urban), and within urban areas, migration status (6 non-migrants and 6 recent migrants) (Figure 2).2
Figure 2.
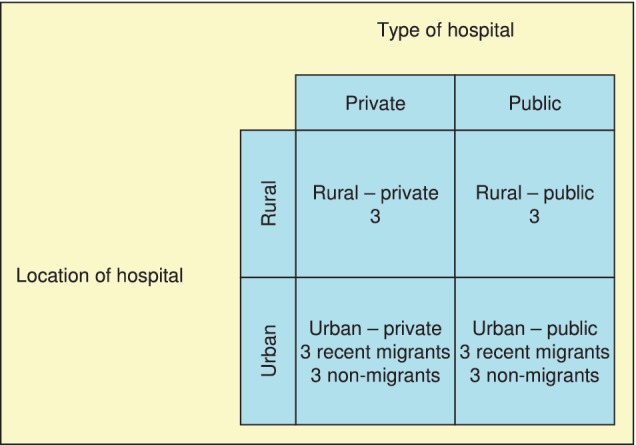
Distribution of in-depth interview respondents
All interviews were conducted in Gujarati by RJ with the assistance of one trained investigator. For all interviews, the spouse or other family members were present as well as the hospitalized person. A semi-structured interview guide was used. Interviews were recorded, with the permission of respondents, using a digital video recorder, transcribed in English, and analysed and coded in MS Word.
Ethical approval
Ethical approval was obtained from the Ethics Committee of The London School of Hygiene and Tropical Medicine and from the Health Commissioner of Gujarat State. Free and informed consent of all respondents was obtained; this consent was taken in verbal rather than written form, given high rates of illiteracy in Gujarat State.
Results
Exit surveys
Table 1 describes the surveyed population, and highlights the main differences between urban and rural respondents, and users of public and private facilities. A majority of respondents were male. Urban respondents and users of private facilities were more likely to be male than their counterparts in rural areas and at public facilities. Distribution of the surveyed population by quintiles of SES suggests that rural respondents were poorer than urban, and users of public facilities poorer than those using private facilities. A slightly higher percentage of urban residents reported having moved to their current place of residence within the last year (8% vs 2%). The broad categories of illnesses reported by respondents differed little between urban and rural areas. However, respondents at public facilities were more likely to report infectious ailments as the primary cause of hospitalization (in rural areas), were more likely to report non-infectious ailments (both in urban and in rural areas) and were less likely to report accidents and injuries. The median duration of hospital stay differed little between urban and rural areas, but was shorter at public facilities (5 days) than at private facilities (7 days).
Table 1.
Description of study population, by place of residence and type of hospital used (percentage distributions unless otherwise indicated), Vadodara, India
| Urban |
Rural |
|||||
|---|---|---|---|---|---|---|
| Public | Private | Total | Public | Private | Total | |
| Gender | (n = 200) | (n = 200) | (n = 400) | (n = 200) | (n = 200) | (n = 400) |
| Male | 55.5 | 75.5 | 65.5 | 52.5 | 68.5 | 60.5 |
| Female | 44.5 | 24.5 | 34.5 | 47.5 | 31.5 | 39.5 |
| SES | (n = 199) | (n = 200) | (n = 399) | (n = 199) | (n = 199) | (n = 398) |
| 1 | 22.61 | 2.50 | 12.53 | 38.19 | 18.09 | 28.14 |
| 2 | 23.62 | 9.50 | 16.54 | 23.62 | 23.12 | 23.37 |
| 3 | 26.13 | 14.50 | 20.30 | 13.07 | 26.13 | 19.60 |
| 4 | 17.59 | 30.50 | 24.06 | 17.09 | 14.07 | 15.58 |
| 5 | 10.05 | 43.50 | 26.57 | 8.04 | 18.59 | 13.32 |
| Migrant status | (n = 200) | (n = 200) | (n = 400) | (n = 200) | (n = 200) | (n = 400) |
| Recent migrant (<1 year) | 5.5 | 10.5 | 8 | 1 | 3 | 2 |
| Non-migrant (resident >1 year) | 94.5 | 89.5 | 92 | 99 | 97 | 98 |
| Primary cause of hospitalization | (n = 200) | (n = 200) | (n = 400) | (n = 200) | (n = 200) | (n = 400) |
| Infectious | 42 | 41.5 | 41.75 | 49.5 | 38.5 | 44.00 |
| Non-infectious | 48 | 30.0 | 39.00 | 43.0 | 34.5 | 38.75 |
| Injuries | 10 | 28.5 | 19.25 | 7.5 | 27.0 | 17.25 |
| Days of hospitalization (median) | (n = 200) | (n = 200) | (n = 400) | (n = 200) | (n = 200) | (n = 400) |
| 5 | 7 | 6 | 5 | 7 | 5 | |
Table 2 describes the hospital expenditures reported by exit survey respondents. The median expenditure per day was almost three times as high among urban residents (Rs. 395) relative to rural residents (Rs. 138). Expenditures per day were higher at private vs public facilities, and this difference was especially marked in urban areas. Medicine fees were an important component of total costs in both urban and rural areas. Doctors’ fees were a more important component of the costs at private vs public facilities. Among non-medical fees, the costs of food and travel were particularly important components of total costs at rural public facilities (at 12.4% and 17.6% of total costs, respectively).
Table 2.
Expenditures on hospitalization, by place of residence and type of hospital used, Vadodara, India
| Urban |
Rural |
|||||
|---|---|---|---|---|---|---|
| Public | Private | Total | Public | Private | Total | |
| Observations | 198 | 198 | 396 | 200 | 200 | 400 |
| Median total expenditures (Rs.) | 677.5 | 4330.5 | 2525 | 390 | 1530 | 910 |
| Median daily total expenditures (Rs./d) | 119.5 | 629.72 | 394.44 | 93.75 | 277.64 | 138.33 |
| % breakdown of total expenditures | ||||||
| Medical fees | ||||||
| Doctors’ fees | 0.2 | 31.8 | 24.9 | 2.6 | 19.2 | 16.3 |
| Medicine fees | 55.5 | 25.3 | 31.9 | 51.5 | 40.4 | 42.3 |
| Bed fees | 0.5 | 14.4 | 11.4 | 4.3 | 14.2 | 12.5 |
| Laboratory fees | 21.6 | 9.5 | 12.1 | 4.8 | 8.3 | 7.7 |
| Ambulance charges | 1.1 | 0.5 | 0.6 | 0.4 | 0.1 | 0.1 |
| Other | 5.5 | 8.8 | 8.1 | 6.0 | 6.9 | 6.7 |
| Sub-total | 84.5 | 90.3 | 89.1 | 69.7 | 89.1 | 85.7 |
| Non-medical fees | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Food | 6.3 | 5.4 | 5.6 | 12.4 | 5.4 | 6.6 |
| Travel | 9.0 | 4.3 | 5.3 | 17.6 | 5.5 | 7.6 |
| Lodging | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Other | 0.2 | 0.0 | 0.0 | 0.3 | 0.0 | 0.1 |
| Sub-total | 15.5 | 9.7 | 10.9 | 30.3 | 10.9 | 14.3 |
| Total fees | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
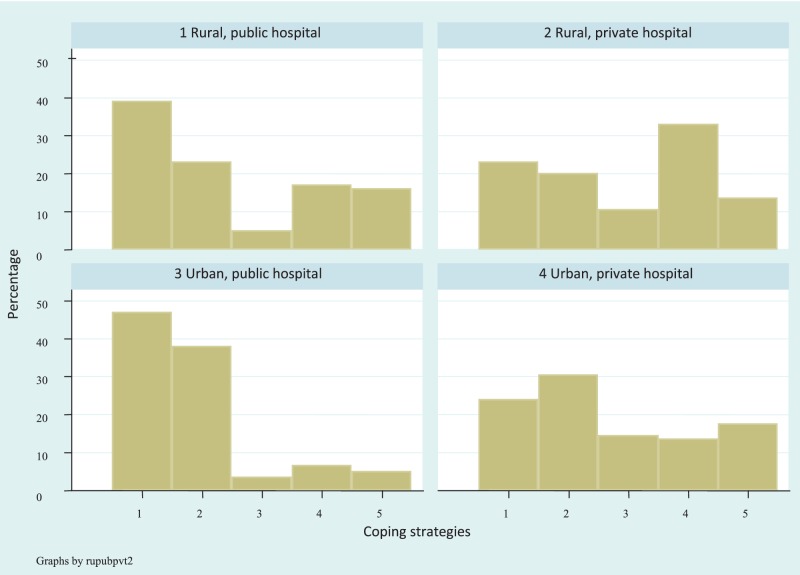
Figure 3 provides an overview of the different (primary) coping strategies reported by exit survey respondents. It is clear that for hospitalizations at public facilities (both in urban and in rural areas) most respondents were able to pay out of their savings or income, or by borrowing from friends, family or employer. For hospitalization at private facilities, these were also common means of paying. But relative to users of public facilities, those using private facilities were more likely to report selling land or other assets as the primary source of coping (particularly in rural areas), and they were more likely to have to borrow money at interest (particularly in urban areas).
Figure 3.
Strategies used for coping with hospitalization costs, by place of residence and type of hospital used, Vadodara, India. Legend (for x axis): 1 = Savings or income; 2 = Borrowed from friends, family or employer; 3 = Borrowed on interest, from moneylender or bank; 4 = Sold land or other assets; 5 = Other (including ‘did extra labour’, ‘don’t know’) (n = 200; 200; 200; 200)
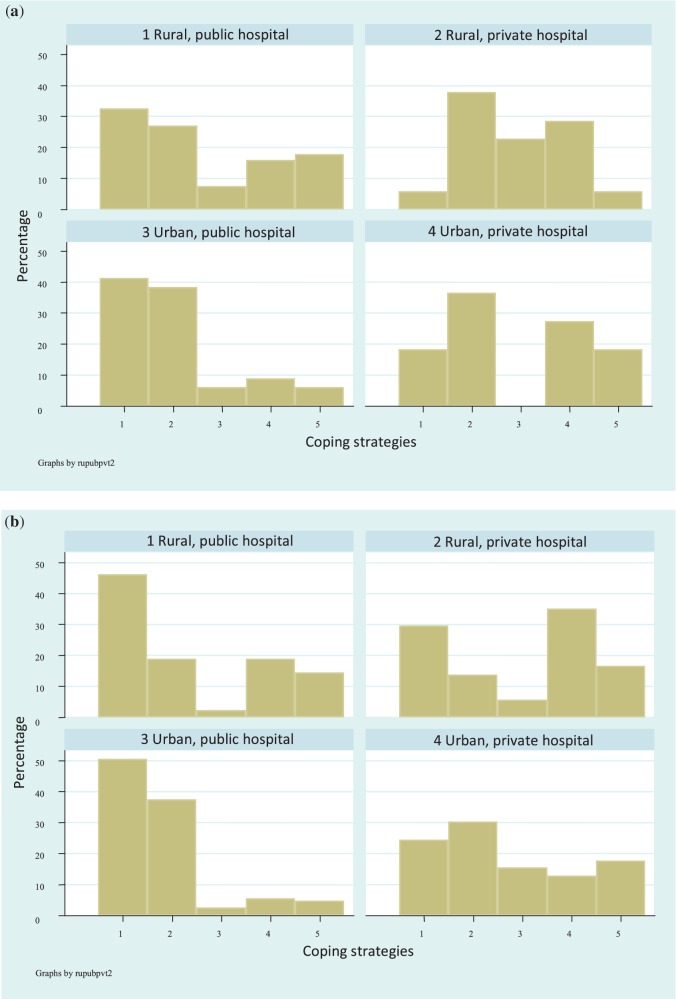
Differences in coping strategies between the poorest 30% of respondents and the less poor 70% are illustrated in Figures 4a and 4b.3 In general, there seems to be remarkably little difference in primary coping strategies between the poor and the less poor who used public facilities, although there was a slightly greater reliance on savings and income amongst the less poor 70%. Among rural, private hospital users, the poorest 30% were much more likely than the less poor 70% to have borrowed from friends, family and relatives, or to have borrowed money on interest, and less likely to have relied on savings and income. It is difficult to comment on ‘poor–less poor’ differences among those using urban, private hospitals, as only 11 respondents falling below the 30th decile used these facilities.
Figure 4.
(a) Strategies used for coping with hospitalization costs: poorest 30%, by place of residence and type of hospital used (n = 108; 53; 68; 11), (b) Strategies used for coping with hospitalization costs: wealthiest 70%, by place of residence and type of hospital used (n = 91; 146; 131; 189). Legend (for x axis): 1 = Savings or income; 2 = Borrowed from friends, family or employer; 3 = Borrowed on interest, from moneylender or bank; 4 = Sold land or other assets; 5 = Other (including ‘did extra labour’, ‘don’t know’).
In-depth interviews
Table 3 provides a description of the 18 in-depth interview respondents (references to respondents provided below correspond to the respondent identification numbers in this table).
Table 3.
Description of 18 in-depth interview respondents
| No. | City/sub-dist. | Gender | Place of origin | Hospital | Cause of hospitalization | Tot. Exp. (Rs.) | Primary coping strategy used | Age | Occupation | Decile |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Vadodara | M | Within Gujarat | Public | Fever of unknown origin | 535 | Savings/income | 18 | Rag picker | 1 |
| 2 | Vadodara | M | Within Gujarat | Public | Asthma | 330 | Borrowed from friends/relatives/employer | 60 | Retired | 2 |
| 3 | Vadodara | F | Uttar Pradesh | Public | Anaemia | 660 | Sold gold/silver jewellery | 19 | Labourer | 3 |
| 4 | Vadodara | M | Rajasthan | Private | Malaria | 1550 | Borrowed from friends/relatives/employer | 28 | Salaried | 3 |
| 5 | Vadodara | F | Rajasthan | Private | Dengue fever | 2250 | Borrowed from friends/relatives/employer | 21 | Housewife | 4 |
| 6 | Vadodara | F | Rajasthan | Private | Hysterectomy | 5300 | Savings/income | 33 | Housewife | 4 |
| 7 | Vadodara | M | (non-migrant) | Public | Blood pressure | 900 | Borrowed from friends/relatives/employer | 30 | Unemployed | 1 |
| 8 | Vadodara | F | (non-migrant) | Public | Gastroenteritis | 600 | Borrowed from friends/relatives/employer | 18 | Self-employed | 2 |
| 9 | Vadodara | M | (non-migrant) | Public | General weakness | 1500 | Borrowed from friends/relatives/employer | 32 | Unemployed | 3 |
| 10 | Vadodara | M | (non-migrant) | Private | Diabetes | 23300 | Savings/income | 55 | Self-employed | 2 |
| 11 | Vadodara | F | (non-migrant) | Private | Accident/injury/fracture | 4640 | Sold land or other assets | 28 | Housewife | 2 |
| 12 | Vadodara | M | (non-migrant) | Private | Dental problem | 12700 | Borrowed from friends/relatives/employer | 47 | Self-employed | 4 |
| 13 | Padra | F | n.a. | Public | Delivery | 890 | Borrowed from friends/relatives/employer | 20 | Domestic worker | 1 |
| 14 | Dabhoi | F | n.a. | Public | Abortion | 275 | Savings/income | 30 | Housewife | 3 |
| 15 | Sankheda | M | n.a. | Public | Diarrhea/dysentery | 1560 | Borrowed from friends/relatives/employer | 40 | Domestic worker | 3 |
| 16 | Padra | M | n.a. | Private | Accident/injury/fracture | 26500 | Sold land or other assets | 40 | Casual wage labourer | 3 |
| 17 | Sankheda | F | n.a. | Private | Hysterectomy | 985 | Borrowed from moneylender on interest | 40 | Casual wage labourer | 1 |
| 18 | Dabhoi | M | n.a. | Private | Heart disease | 2500 | Sold land or other assets | 32 | Farm worker | 1 |
Poor people choose public facilities due to lower cost
In-depth interview respondents who used public facilities generally reported that they did so because these were perceived to be less costly than private hospitals.
“Because we did not have money, we had to go to the public hospital. We heard that they do not charge services at the public hospital.” (Respondent 1)
While this was the most common reason for choosing a public facility, some reported that even the fees charged at the public facility were unaffordable.
“We chose the public hospital because they would provide treatment for free. But even they charged money … five hundred rupees … How can we afford to pay this amount?” (Respondent 14)
Reasons for using private facilities
Respondents cited a number of reasons for using private hospitals. The most commonly cited reason was that the private hospital was nearby to the respondent’s home:
“(We chose the private hospital) only because it was nearby and she (Respondent 11) was in a great deal of pain. It was an emergency and the first hospital that I thought of was this nearby private hospital.” (Relative of respondent 11)
Several respondents also expressed the belief that private hospitals are of higher quality than public:
“We do not use the public hospital, as the treatment given there is not good. It is very dirty and unhygienic. The private hospital is very clean and well maintained.” (Respondent 18)
Poor people rely on multiple coping strategies.
Respondents generally reported using multiple (two or more) different strategies for coping with the costs of hospitalization. Respondent 8, for example, was a young woman from Vadodara city, hospitalized in a public facility for gastroenteritis. In order to cover the cost of the hospital stay—Rs. 600—the family drew on their savings and borrowed money from relatives:
“I bought medicines using the money I borrowed from him (my brother) … I took 400 rupees from my brother, and I gave approximately 100 rupees from my own (savings). As well, I later borrowed 100 rupees from another relative in order to pay the medical shop.” (Mother of respondent 4)
Respondent 1, a recent migrant to Vadodara, was also hospitalized in a public hospital, for fever of unknown origin. His family, who earn a living by selling rags and scraps salvaged from garbage, drew on savings and sold a small amount of jewellery:
“… we paid using our own money—money that we had saved for Diwali … We also had to pawn our belongings. We pawned a silver ornament that was on my son’s leg. We removed (that ornament) and pawned it … Now it is gone. I could not repay the money (to the pawn-broker) so we lost the ornament.” (Sister-in-law of respondent 1)
Poor who use public facilities can pay from savings, income or relying on social networks
As was suggested by the exit survey data, respondents who used public hospitals could generally cope with the costs either through their savings and income or through borrowing from friends, family or employers:
“We paid using money that we had saved for Diwali. We do not have any relatives from whom we can borrow.” (Respondent 1)
Poor who use private facilities use different coping strategies (viz. a viz. those who use public)
Poor respondents who used private facilities were more likely to report having borrowed money on interest or selling assets. This was the case, for example, for the following respondent who reported total expenditures of Rs. 26 500:
“He (my brother) owns land, which he mortgaged. We paid the money that we got after mortgaging the land. Even today I don’t have any money saved. I roll cigarettes every day and earn money from this. But I spend this money on medicines.” (Respondent 16)
Key differences in coping strategies between urban and rural poor
In the in-depth interviews, respondents from rural areas were more likely to report having borrowed from family members, while those in urban areas were more likely to have borrowed from friends or employers. The following urban respondent, for example, borrowed from neighbours:
“I borrowed some money from my neighbours … And we don’t even have much income so that we can save (to repay this loan). Our neighbours are our best friends … We have not been here for long, however they have been very helpful.” (Respondent 4)
In several cases, the rural poor reported selling or mortgaging land in order to cope with the costs of hospitalization (e.g. respondents 16 and 18) while some urbanites reported selling other assets:
“Sister, what can people like us do? She (Respondent 3) had two gold earrings, and I had to sell off one of these. I got 1400 rupees for the earring.” (Spouse of respondent 3)
Key differences in coping strategies among recent migrants
Recent migrants to urban areas were less likely than permanent residents to report borrowing from relatives. For example, the following two respondents, both long-term residents of Vadodara city, borrowed from family:
“My brother helped me a lot. I bought medicines with the money I borrowed from him.” (Respondent 8)
“We told my cousin about her (Respondent 11’s) hospitalization and he immediately came over. I told him that I would need some money, so he went back and arranged for money.” (Spouse of respondent 11)
In contrast, the following respondents, who had recently migrated to Vadodara city, used other coping strategies:
“We don’t know anyone here, so who would give us money? … All our relatives are back at our village … So we had to sell our belongings.” (Respondent 3)
“I cook at someone’s home. I asked this employer for money to pay for my hospital expenses. They were very helpful … Our employers are (like) our relatives. Our real relatives are far away so they (the employers) are the ones who help us first.” (Respondent 5)
Discussion and conclusions
Summary of findings
Users of public hospitals, in both urban and rural areas, were poor relative to users of private hospitals. Median expenditures per day were higher at private vs public facilities, and this difference was especially marked in urban areas. For hospitalizations at public facilities (both in urban and in rural areas), most respondents were able to pay out of their savings or income; or by borrowing from friends, family or employer. Those using private facilities were more likely to report selling land or other assets as the primary source of coping (particularly in rural areas) and they were more likely to have to borrow money at interest (particularly in urban areas). In-depth interview respondents (those below the 30th percentile of SES) who used public hospitals often did so because of their lower perceived cost. Poor respondents reported using multiple different coping strategies. Respondents from urban areas were more likely to have borrowed from friends or employers, while those in rural areas were more likely to report having borrowed from family members. Recent migrants to urban areas were less likely than permanent residents to report borrowing from relatives, but in some cases were able to borrow from neighbours or employers.
Discussion
Studies that have focused on the costs of inpatient care in India, and the related coping strategies, are relatively few. Consistent with previous studies, the current study suggests that the poor depend predominantly on the public sector for inpatient care. Peters et al. (based on National Sample Survey Organisation data) concluded that the poor rely on public hospitals more than the rich (Peters et al. 2002). For the poorest 25% of the population, 61% of hospitalizations are in public hospitals. Despite this, wealthier populations capture a disproportionate share of public health spending. For example, the richest quintile received more than three times the public subsidy received by the poorest quintile. In part, this reflects the much higher rates of hospitalization among the non-poor—the richest quintile of the population is six times more likely to have been hospitalized (in either a public or private facility) (Peters et al. 2002, p. 219).
On the one hand, use of (nominally) free public health care services is a common strategy for coping, protecting households from potentially burdensome health care costs. This is consistent with findings in other countries where consumers can choose between public and private sectors. Russell, for example, found that ‘public health care services, free at the point of delivery in Colombo (Sri Lanka) protected the majority of poor households against high direct cost burdens, particularly the potentially high costs of hospital inpatient care and regular treatment of chronic illness’ (Russell 2008, p. 112–3). Nonetheless, as is the case in many other low- and middle-income countries, there are significant out-of-pocket costs even at public facilities (McIntyre et al. 2006).
Given the much higher total costs incurred by those using private hospitals, it is interesting that the poorest (particularly in rural areas) do not rely on public hospitals to an even greater extent. The findings suggest that access and quality are among the main reasons that poorer people turn to the private sector for inpatient care. Many previous studies have found that India’s public health care sector is rife with problems (Peters et al. 2002). Among these problems are poor management, low service quality, staffing limitations (particularly in remote, rural areas), and limited drugs and supplies.
This study finds the median daily hospital expenditures to be almost three times higher among urban than rural respondents, and that this difference is due largely to higher daily expenditures at private hospitals. This is consistent with the findings of some previous studies. For example, the World Health Survey, conducted in 2003, found that the mean annual household expenditure on health care (goods and services) was Rs. 3304 in rural areas and Rs. 6384 in urban areas (World Health Organization 2006b), and the 60th round of the National Sample Survey (conducted in 2004) found that the average cost of a hospitalization was Rs. 6225 among rural respondents and Rs. 9367 among urban residents (National Sample Survey Organisation 2006). The difference found in our study may be explained in part by higher urban incomes. While data are not available for Vadodara district, according to the 63rd round of the National Sample Survey (2006–07) the monthly per capita consumption expenditure (MCPE) was Rs. 797 in rural Gujarat and Rs. 1422 in urban Gujarat (National Sample Survey Organisation 2008). The difference may also be due in part to higher quality (or more intensive) services provided at private hospitals in urban vs rural areas.
This study confirms that people often borrow from friends, family or employers to cope with the direct costs of inpatient care. Borrowing from one’s social networks to cope with medical costs is common in other settings (McIntyre et al. 2006). The current study suggests that the poor in urban areas (including recent migrants) may be more likely to rely on employers or neighbours rather than relatives, but this finding is based upon very few observations. This study did not add evidence to Russell’s finding that lower-income households had weaker social networks and could access fewer financial resources (Russell 2008). The findings are, however, consistent with those of Flores et al. (2008), who found that even the poorest households in the poorest districts of India coped with medical expenditures through borrowing and drawing on savings.
Aside from use of public health services, very few survey respondents reported use of formal social protection mechanisms. India’s National Health Policy (2002) encouraged the setting up of private insurance companies and the introduction of government-funded district-based insurance schemes on a pilot basis (MOHFW 2002). In India, 75–85 million people are at present covered by health insurance—approximately 8% of the total population (Matthies and Cahill 2004; Gupta and Trivedi 2005). Social (mandatory) health insurance in India consists of coverage by the Employee State Insurance Scheme (ESIS) and Central Government Health Scheme (CGHS). The private insurance sector has grown tremendously in recent years; the number of people covered under voluntary, private health insurance schemes increased rapidly from 1995–96 to 2002–03, by 29% per annum (Gupta 2004). Community-based health insurance schemes (CBHI) cover only 3 million people (Gupta and Trivedi 2005), although the number of such schemes is increasing. The private and community-based schemes primarily cover hospital care, and are usually subject to caps (i.e. limited indemnity) or deductibles.
The findings of this study suggest that there are several policy options that should be pursued in order to protect the poor from the costs of inpatient care. Governments should invest in improving the quality and access of public first-referral hospitals. This should be done in a selective manner—with a focus, for example, on rural areas and urban slum areas—in order to promote a more equitable distribution of resources. In fact, the Government of India is already making efforts to improve access to quality health care in urban slum areas under the National Urban Health Mission (2008–2012) (MOHFW 2008). Similarly, the National Rural Health Mission (2005–2012) aims to improve health care in rural areas of 18 states deemed to have the weakest infrastructure, in part by strengthening rural hospitals (MOHFW 2005; Mudur 2005). Given that these two schemes are still being implemented, it is unclear how successful they will be.
Efforts must also be made to reduce the cost of inpatient care at public facilities; this can be done in part by ensuring the availability of basic drugs and supplies at first-referral hospitals. Policy makers should continue to explore and support efforts to provide financial protection through insurance mechanisms. The Indian government and individual state governments are indeed pursuing expansions in publicly funded (or subsidized) coverage for rural populations as well as other vulnerable populations. For example, in April 2008, the Government of India launched the Rashtriya Swasthya Bima Yojana (RSBY). This voluntary scheme targets the 300 million people who are below the poverty line. In return for a premium of Rs. 30 per person per year, coverage is provided for hospitalization (either at public or private facilities), capped at Rs. 30 000 per family per year (Bhattacharjya and Sapra 2008). The balance of the premium, Rs. 750 per person per year, is to be borne by central and state governments. By the end of 2009, almost 9 million households were enrolled in the scheme (Ministry of Labour and Employment, undated) though this still represents a tiny proportion of the target population.
Past experience suggests that these efforts must be carefully monitored to ensure that the poorer among the insured are able to access scheme benefits, and that the quality and quantity of health care provided has to be monitored and regulated. In particular, there needs to be further discussion and debate as to whether or not it is a good idea to use public funding to improve financial access to private hospitals (as is occurring under the RSBY). In the absence of systems for monitoring and regulating private hospitals, such schemes risk exposing poor people to care that is unnecessary, of poor quality, or unnecessarily expensive. A study by Ranson and John (2001) documented the problem of unnecessary hysterectomies, often of poor quality, performed on members of a community-based health insurance scheme.
This study also suggests several areas where additional research is required. These include:
Further study of health care costs in urban areas, to extend understanding beyond the one city studied here;
Longitudinal assessments of the costs of medical care—both direct and indirect—and coping strategies;
Documenting interventions that have been successful in improving the quality (or reducing the cost) of care at public facilities, and the factors that have contributed to success;
Further research—possibly including larger, representative samples—exploring the challenges faced, and coping strategies used, by migrant workers and their families;
Studies of social networks—for example, how these networks are affected by new, formal risk-sharing mechanisms (like the RSBY) and factors that help or hinder social networks in rapidly expanding urban areas;
Further studies on strategic purchasing, to ensure that health care purchases by insurers are of acceptable quality and reasonable cost.
Strengths and weaknesses of the methodology
The main strength of the methodology is that it employed both qualitative and quantitative methods. This helped, for example, to ensure that the questions on coping strategies included in the exit survey were culturally and contextually appropriate (as they had been reported by participants in the preceding focus group discussions), and it enabled verification of exit survey findings through in-depth interviews with select respondents. Data on hospital expenditures and coping strategies are likely to have been recalled with good accuracy given that they were collected right at the time of discharge from hospital. This is one of very few Indian studies where investigators have been granted permission to conduct such an exit survey on the premises of both public and private hospitals. Finally, because the exit survey and in-depth interviews purposefully included strata of urban respondents, this is one of very few Indian studies that provide data on coping strategies among urbanites.
The study has a number of methodological shortcomings. First, because respondents were identified by exit survey (as opposed to a house-to-house survey, for example) the study excludes those who may have required hospitalization, but who chose not to seek care or who sought outpatient care only. Thus, the study may have excluded the very poor who did not seek care. Second, the exit survey was non-random, and the respondents therefore may not represent the wider population of hospitalized persons in Vadodara district. There is likely to be considerable variation in costs between different private hospitals, so selection of different facilities may have led to different results. Respondents at any one facility were non-randomly selected; respondents were interviewed during the same season and over a period of only a few days, and patients were excluded from the sample if they had used a private inpatient room rather than a general hospital ward. Third, there may be limits to the extent to which study findings can be generalized to other districts or states, given, for example, that Vadodara district is fast-growing and urban relative to many others. Fourth, the exit survey did not explore indirect costs (i.e. loss of household productive labour time and income). And the in-depth interviews, because they were cross-sectional, were more likely to capture fairly discrete and memorable coping strategies (e.g. borrowing from a money lender), and less likely to capture, for example, small reductions in household consumption or increases in time spent in productive labour.
Funding
This work was funded by the Wellcome Trust, United Kingdom (Grant number GR080101MA).
Conflict of interest
None declared.
Acknowledgements
We wish to thank Dr V R Muraleedharan (IITM, Chennai) and his team for their support throughout this project. Thank you to Nicola Lord (LSHTM) for logistical support. We thank Dr Amarjeet Singh, Commissioner of Health, Gujarat, for permitting us to carry out the study at the public hospitals. We are particularly grateful to the hospital representatives and staff who gave us support for the exit survey interviews. Also, thanks to the staff of Baroda Citizens Council, who helped us identify recent migrants and conduct focus group discussions with them. We also take this opportunity to extend our gratitude to the Faculty of Social Work, Vadodara who provided work space during the project. Most importantly, we wish to thank the field investigators who assisted in data collection; and all the respondents for sharing their experiences and responding to our questions.
Appendix 1.
List of 26 assets and utilities variables included in the socio-economic status (SES) index, showing responses for each decile (1st being the poorest and 10th being the least poor)
| No. | Variable | Deciles of SES |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| Number of observations (n = 797) | 80 | 82 | 78 | 81 | 78 | 81 | 81 | 77 | 80 | 79 | |
| 1 | Ownership of house | 68.75 | 65.85 | 73.08 | 70.37 | 73.08 | 71.60 | 58.02 | 63.64 | 66.25 | 75.95 |
| 2 | Housing with brick/stone with cement plaster | 12.50 | 15.85 | 20.51 | 41.98 | 62.82 | 58.02 | 58.02 | 87.01 | 81.25 | 96.20 |
| 3 | Owns electricity connection | 52.50 | 86.59 | 85.90 | 92.59 | 89.74 | 83.95 | 75.31 | 80.52 | 77.50 | 84.81 |
| 4 | Gas/kerosene as cooking source | 1.25 | 18.29 | 19.48 | 39.51 | 48.72 | 54.32 | 72.84 | 68.83 | 90.00 | 94.94 |
| 5 | Own mattresses | 8.75 | 20.73 | 44.87 | 53.09 | 60.26 | 79.01 | 74.07 | 89.61 | 96.25 | 98.73 |
| 6 | Own cot/bed | 27.50 | 54.88 | 89.74 | 87.65 | 93.59 | 97.53 | 95.06 | 97.40 | 98.75 | 100 |
| 7 | Own wristwatch | 37.50 | 64.63 | 88.46 | 95.06 | 93.59 | 90.12 | 95.06 | 98.70 | 98.75 | 100.00 |
| 8 | Own fans | 26.25 | 87.80 | 87.18 | 96.30 | 100.00 | 98.77 | 100.00 | 98.70 | 100.00 | 100.00 |
| 9 | Own radios | 8.75 | 37.80 | 28.21 | 41.98 | 47.44 | 61.73 | 51.85 | 48.05 | 57.50 | 79.75 |
| 10 | Own television | 0.00 | 6.10 | 8.97 | 25.93 | 46.15 | 69.14 | 85.19 | 93.51 | 100.0 | 100.0 |
| 11 | Own refrigerator | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1.23 | 6.17 | 15.58 | 45.00 | 64.56 |
| 12 | Own sewing machine | 0.00 | 1.22 | 0.00 | 1.23 | 5.13 | 6.17 | 8.64 | 15.58 | 5.00 | 8.86 |
| 13 | Own telephones | 0.00 | 0.00 | 0.00 | 1.23 | 0.00 | 1.23 | 3.70 | 15.58 | 31.25 | 94.94 |
| 14 | Own mobile-phones | 0.00 | 3.66 | 11.54 | 29.63 | 34.62 | 58.02 | 83.95 | 89.61 | 97.50 | 100.00 |
| 15 | Own two-wheelers | 0.00 | 0.00 | 0.00 | 0.00 | 1.28 | 1.23 | 9.88 | 36.36 | 83.75 | 100.00 |
| 16 | Own tractors | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1.23 | 2.60 | 3.75 | 12.66 |
| 17 | Own buffaloes | 17.50 | 24.39 | 24.36 | 30.86 | 24.36 | 23.46 | 12.35 | 14.29 | 11.25 | 15.19 |
| 18 | Own cows | 1.25 | 7.32 | 8.97 | 9.88 | 6.41 | 11.11 | 4.94 | 5.19 | 6.25 | 6.33 |
| 19 | Own bulls | 1.25 | 8.54 | 12.82 | 19.75 | 16.67 | 11.11 | 6.17 | 11.69 | 7.50 | 16.46 |
| 20 | Own pada | 0.00 | 2.44 | 1.28 | 1.23 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 21 | Own goats | 33.75 | 21.95 | 14.10 | 17.28 | 14.10 | 6.17 | 2.47 | 6.49 | 1.25 | 1.27 |
| 22 | Own hens | 2.50 | 2.44 | 1.28 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 23 | Own bullock carts | 0.00 | 0.00 | 3.85 | 6.17 | 2.53 | 3.70 | 6.17 | 6.49 | 3.75 | 11.39 |
| 24 | Own shops | 0.00 | 1.22 | 3.85 | 2.47 | 6.41 | 9.88 | 18.52 | 23.38 | 27.50 | 26.58 |
| 25 | Own lauri | 1.25 | 7.32 | 5.13 | 7.41 | 6.41 | 6.17 | 12.35 | 11.69 | 10.00 | 6.33 |
| 26 | Total no. of rooms | 1.1 | 1.3625 | 1.6875 | 1.5949 | 1.7375 | 1.9024 | 2.1299 | 2.125 | 2.325 | 3.3797 |
Endnotes
1 The poverty line is set for each state, and represents the level of consumer expenditure per capita required to ensure a calorie intake of 2100 per day in urban areas and 2400 per day in rural areas. In 1995–96, it was estimated that 20.5% of Gujarat’s rural population, and 30.7% of the urban population, were BPL.
2 For the purpose of this study, we considered recent migrants as those who had moved from their place of origin/birth (or usual residence) within the previous year (Census 2001). For the purpose of the in-depth interviews, non-migrants were those who had lived at their current place of residence since birth.
3 The latest poverty statistics for India suggest that in 1999–2000, 28.6% of the total population were living below the ‘national poverty line’ (World Bank 2010). We chose to compare coping strategies among the poorest 30% of respondents (vs the less poor 70%) as they might roughly be thought of as representing those who live below the poverty line (vs those who live above the poverty line). This is a rather arbitrary and imperfect cut-off, given that Gujarat does tend to perform slightly better than all-India on measures of poverty (and so is likely to have a poverty line lower than 30%) and, more importantly, given that respondents to the exit survey are not representative of the general population.
References
- Bhattacharjya AS, Sapra PK. Health insurance in China and India: segmented roles for public and private financing. Health Affairs (Millwood) 2008;27:1005–15. doi: 10.1377/hlthaff.27.4.1005. [DOI] [PubMed] [Google Scholar]
- Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Flores G, Krishnakumar J, O’Donnell O, Van Doorslaer E. Coping with health-care costs: implications for the measurement of catastrophic expenditures and poverty. Health Economics. 2008;17:1393–412. doi: 10.1002/hec.1338. [DOI] [PubMed] [Google Scholar]
- Gupta A. Wealth through health insurance: the way to sustainable development. IRDA Journal. 2004;2:24–5. [Google Scholar]
- Gupta I, Trivedi M. Social health insurance redefined: Health for all through coverage for all. Economic and Political Weekly. 2005;40:4132–40. [Google Scholar]
- International Organisation for Migration. Migration, Development and Poverty Reduction in Asia. Geneva: International Organisation for Migration; 2005. [Google Scholar]
- Kochar A. Explaining household vulnerability to idiosyncratic income shocks. American Economic Association Papers and Proceedings. 1995;85:159–64. [Google Scholar]
- Krishna A, Kapila M, Porwal M, Singh V. Falling into poverty in a high-growth state: escaping poverty and becoming poor in Gujarat villages. Economic and Political Weekly. 2003;38:5171–9. [Google Scholar]
- Mahal A, Singh J, Afridi F, et al. Who Benefits from Public Health Spending in India? New Delhi: National Council of Applied Economic Research (NCAER); 2000. [Google Scholar]
- Matthies S, Cahill KR. Lessons from across the World: how India can break barriers to develop health insurance. IRDA Journal. 2004;2:7–12. [Google Scholar]
- McIntyre D, Thiede M. Illness, health service costs and their consequences for households. In: Bennett S, Gilson L, Mills A, editors. Health, Economic Development and Household Poverty: From Understanding to Action. London: Routledge; 2007. [Google Scholar]
- McIntyre D, Thiede M, Dahlgren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Social Science & Medicine. 2006;62:858–65. doi: 10.1016/j.socscimed.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Ministry of Labour and Employment. Rashtriya Swasthya Bima Yojna. Undated. Online at: http://www.rsby.gov.in/, accessed 4 January 2010.
- MOHFW. National Health Policy 2002. New Delhi: Ministry of Health and Family Welfare, Government of India; 2002. [Google Scholar]
- MOHFW. New Delhi: Ministry of Health and Family Welfare, Government of India; 2005. National Rural Health Mission (2005–2012) Online at: http://www.mohfw.nic.in/NRHM/Documents/Mission_Document.pdf, accessed 4 January 2010. [Google Scholar]
- MOHFW. New Delhi: Ministry of Health and Family Welfare, Government of India; 2008. National Urban Health Mission (2008–2012) Online at: http://www.uhrc.in/downloads/Reports/NUHM-Draft.pdf, accessed 4 January 2010. [Google Scholar]
- Mudur G. India launches national rural health mission. British Medical Journal. 2005;330:920. doi: 10.1136/bmj.330.7497.920-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munshi K, Rosenzweig MR. Why is mobility in India so low? Social insurance, inequality, and growth. 2005. BREAD Working Paper No. 097. Durham, NC: Bureau for Research in Economic Analysis of Development (BREAD) [Google Scholar]
- National Sample Survey Organisation. Morbidity, health care and the condition of the aged: NSS 60th round. New Delhi: National Sample Survey Organisation, Government of India; 2006. Online at: http://www.mospi.gov.in/mospi_nsso_rept_pubn.htm, accessed 5 January 2010. [Google Scholar]
- National Sample Survey Organisation. Household Consumer Expenditure in India, NSS 63rd round, 2006-07. Report No. 527(63/1.0/1) New Delhi: National Sample Survey Organisation, Government of India; 2008. [Google Scholar]
- Office of the Registrar General. Census of India. New Delhi: Government of India; 2001. [Google Scholar]
- Peters DH, Yazbeck AS, Sharma RR, et al. Better Health Systems for India’s Poor: Findings, Analysis, and Options. Washington, DC: The World Bank; 2002. [Google Scholar]
- Ranson MK, John KR. Quality of hysterectomy care in rural Gujarat: the role of community-based health insurance. Health Policy and Planning. 2001;16:395–403. doi: 10.1093/heapol/16.4.395. [DOI] [PubMed] [Google Scholar]
- Rosenzweig MR. Risk, implicit contracts and the family in rural areas of low-income countries. The Economic Journal. 1988;98:1148–70. [Google Scholar]
- Russell S. Coping with the costs of illness: vulnerability and resilience among poor households in urban Sri Lanka. In: Bennett S, Gilson L, Mills A, editors. Health, Economic Development and Household Poverty: From Understanding to Action. London: Routledge; 2008. [Google Scholar]
- Townsend RM. Risk and insurance in village India. Econometrica. 1994;62:539–91. [Google Scholar]
- UNDP, World Bank. 1999.
- Van Doorslaer E, O’Donnell O, Rannan-Eliya RP, et al. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. The Lancet. 2006;368:1357–64. doi: 10.1016/S0140-6736(06)69560-3. [DOI] [PubMed] [Google Scholar]
- World Bank. World Development Report 2000/2001: Attacking Poverty. Oxford: Oxford University Press; 2001. [Google Scholar]
- World Bank. Health of the poor in urban India: a consultation, July, 2002. New Delhi: World Bank; 2002. [Google Scholar]
- World Bank. World Development Report 2010: Development and Climate Change. Washington, DC: World Bank; 2010. [Google Scholar]
- World Health Organization. The World Health Report 2006: Working Together for Health. Geneva: World Health Organization; 2006a. [Google Scholar]
- World Health Organization. World Health Survey: Report of India. 2006b. Online at: http://www.who.int/healthinfo/survey/whsind-india.pdf, accessed 4 January 2010.