Abstract
Objectives
To document the transition to a totally one-stop (patient seen and treated in one appointment) wide-awake (local anaesthesia only) hand surgery service.
Design
Retrospective review of 10 year service with detailed analysis of last 1000 cases including process and cost-effectiveness and efficiency analysis.
Setting
Purpose-built CQC-certified day-case surgical facility where we have pioneered the UK's first totally one-stop wide-awake orthopaedic service.
Participants
Approximately five thousand orthopaedic patients treated in the last ten years.
Main outcome measures
Surgical outcomes, patient satisfaction and cost-effectiveness and efficiency.
Results
The OSWA model is safe, efficient and effective; with a low complication rate, extremely high patient satisfaction; and cost-savings to the NHS of 50–75% of the national tariff. The service saved the NHS approximately £750,000 for the 1000 cases presented; and over £2 million since the inception of the service.
Conclusions
A totally one-stop wide-awake hand surgery service is a practicable and feasible alternative to the conventional treatment pathway with benefits in terms of efficiency and cost-effectiveness.
Introduction
There is increasing emphasis on efficient, cost-effective, streamlined and non-hospital-based orthopaedic surgery services.
With the evolution of UK healthcare and commissioning coupled with contemporary (healthcare) economics: many surgical services are in jeopardy. We present a model which has saved the NHS a large amount of money in our region over the last ten years and which has the potential to do so countrywide. Furthermore, with increased efficiency and cost-savings the one-stop wide-awake model could be adapted to and secure a wide range of surgical services for NHS patients.
Orthopaedic surgery is increasingly provided in non-hospital settings. Many general practice (GP) surgeries provide a minor surgery service for procedures such as carpal tunnel decompression. Furthermore, the last decade has seen the proliferation of Independent Sector Treatment Centres which provide a range of orthopaedic services. Moreover, intermediate care and physiotherapy triage services are now juxtaposed between GPs and hospital specialists.
Over the last decade we have set-up and developed a total one-stop wide-awake upper limb orthopaedic surgery service in a primary care setting. The aims at service outset were to deliver safe and effective care under local anaesthesia in a purpose-built facility with associated time and cost savings, and maintaining high levels of patient satisfaction through streamlined and effective surgical care. This paper details infrastructure, scope, technical aspects and results of this service.
Methods and materials
Infrastructure
The Parkside Day Case Surgical Centre is a purpose-built CQC-certified facility comprising: one orthopaedic theatre, one waiting area and one clinic room plus limited service and maintenance areas. The facility is adjoined to an NHS GP surgery; and operates daily; with the one-stop orthopaedic service running on Mondays and Fridays. Patients are referred into the countywide Primary Care Surgical Scheme by their GP's or intermediate services using the choose and book system.
Once a referral is received, our clinical assistants contact the patient and the patient themselves chooses the date and time of the one-stop appointment. Because the entirety of the outpatient appointment and surgery are provided within one 30–45 minute slot there is ample capacity.
Our staff comprise: two consultant orthopaedic surgeons, one clinical manager, two theatre nurses, one healthcare support worker and two clinical assistants.
After the patient has chosen their slot, our clinical assistants book the operation provisionally (computerized). They then send the patient: a letter requiring patient to confirm the appointment, an information sheet and details of the service website plus a unique code. Patients can then log on to the website for their information and in order to enter their preoperative information securely. The preoperative information includes a general health questionnaire and the validated quick-DASH score. Patients may also request paper copies of all relevant information and forms. Staff cover is planned and notes are prepared. Lists are booked with an allowance of 30–45 minutes total time per one-stop management; this includes initial assessment and obtaining consent.
On the day of surgery the patient is seen by one or both consultants (MSKB & QMKB). The diagnosis is confirmed or otherwise. If otherwise, the consultant: discharges; refers for further treatment; or injects. If a patient presents with a bilateral condition, the second side is listed on the day for operation at the patient's convenience and no new referral is required. The surgeon has access to diagnostics if required.
All patients are given printed literature regarding pros and cons of various treatment options. Informed consent is obtained. All patients are at liberty to opt out of or defer one-stop treatment. The patient is gowned for the operation by the Healthcare Support Worker and is transferred to the theatre. The local anaesthetic is administered by the surgeon. No tourniquet is used. The scrub nurse prepares site and drapes whilst the surgeon scrubs (this allows time for the local anaesthetic to work without loss of operating time). All drapes, swabs, sundries and instruments are single use. Postoperatively a cotton wool and crepe dressing and a greater arm sling are applied.
The patient is given postoperative instructions regarding removal of sutures at their own surgery. The patient is given the consultant's e-mail address and the surgery contact number in case of problems. The postoperative notes entered onto the computer, faxed to referring GP and then sent in the post. Any histology is copied to their GP and the patient is informed. A follow-up audit questionnaire (available at http://www.onestopwideawake.org.uk) is sent to all patients, non-responders are encouraged to reply; and all feedback and outcomes are also freely reported by patients and OSWA staff via the website.
Scope
Local GPs and intermediate care providers are at liberty to refer a range of common orthopaedic conditions.
Surgery under local anaesthesia without tourniquet
Surgery is perfomed under local anaesthesia using: a lignocaine and adrenaline mix except for digits, where plain lignocaine is used; with no tourniquet. Diathermy is not used routinely. The standard is 5–10 ml of 2% lignocaine with adrenaline 1:200 000, which is drawn up with a 21 gauge needle and infiltrated with a 25 gauge needle.
Follow-up, audit and outcomes
We operate continuous audit processes. All patients are requested to contact us immediately in the case of any problems. We have an open access policy for all postoperative patients such that they may contact us via e-mail or telephone and we will see them on the next OSWA date or sooner if required. Follow-up questionnaires are sent out approximately 6 months post-surgery.
Results
For our last 1000 consecutive cases the breakdown of treatments performed is as follows:
| Carpal tunnel | 432 |
| Dupuytren's Contracture | 270 |
| Trigger Finger | 78 |
| Trigger Thumb | 26 |
| Ganglion Simple | 55 |
| Ganglion Complex | 42 |
| Removal of lump | 20 |
| Mucoid cyst | 15 |
| Ulnar Nerve Decompression | 10 |
| De Quervain's Decompression | 5 |
| Removal of Bursae | 7 |
| Injections* | 40 |
(*Trigger finger/thumb 21, OA thumb base 12, De Quervains Tenosynovitis 6, Carpal Tunnel 1)
Only complete audit cycles with follow-up data were included.
No cases were referred by the orthopaedic surgeon to a hospital doctor or to physiotherapy.
Two patients out of the thousand did not attend their original appointment, on account of exceptional circumstances, and they did attend the subsequent appointment.
Outcomes
There were three cases of confirmed superficial surgical site infection treated successfully with oral antibiotics and wound care, and fifteen cases of confirmed delayed wound healing. All of these cases were associated with the use of an absorbable skin suture we started to use in early 2011; and on account of ongoing audit this issue was recognized and rectified. As a result, only non-absorbable silk skin sutures, which we had used for many years prior to 2011, are now used exclusively.
There was one case of revision bilateral carpal tunnel decompression in a patient on whom we had performed bilateral carpal tunnel surgery previously. There were five recurrences of ganglia which were re-operated successfully. There were no intraoperative complications (e.g. neurovascular or tendon injury). There were no cases requiring finger amputation. Up to 10% of patients have minor short-medium term problems with the surgical site such as a tender scar, pillar pain (carpal tunnel) or hypertrophic scar which improve with time, exercise and scar massage. Over 99% of patients achieved a good-excellent outcome and were therefore satisfied with their OSWA treatment.
Efficiency
The total time per one-stop management did not exceed 45 minutes (range 30–45 minutes, mode 30 minutes and median 30 minutes), including initial assessment and obtaining consent. A mean of six one-stop treatments were performed per morning or afternoon session, with capacity for accommodating previously operated patients with problems, wound reviews etc. For bilateral conditions or multiply affected digits, further procedures were scheduled as necessary within 4–6 weeks of the original operation.
| Targets achieved | |
| One-Stop care achieved | 1000 cases |
| Wide-awake care achieved | 1000 cases |
| Referral to hospital for surgery | 0% |
| DNA rate | 0.2% |
| Litigation | 0% |
| Patient satisfaction rate | >99% |
| One-Stop treatment deferred for investigation | 0% |
| Cost saving to NHS per 1000 cases | £750,000 approx. |
GP/Intermediate care Referrals
The diagnosis was correct in over 90% of cases, with no significant difference between GP and intermediate care referrals.
In the 97 cases in which the diagnosis was revised, the breakdown was as follows:
10 cases of triggering digit not identified;
5 cases of triggering digit correctly identified but this was secondary to Dupuytren's Contracture;
5 cases of mucoid cyst not identified;
30 cases of carpal tunnel syndrome not identified;
23 cases of Dupuytren's contracture not identified;
14 cases of ganglion not identified;
- 10 cases of referred with pain without diagnosis, all injected, breakdown as follows:
- 3 OA thumb base;
- 4 De Quervains Tenosynovitis;
- 3 Trigger Finger.
All referred cases were appropriate for one-stop treatment. No cases were rejected or referred onward.
Efficiency and cost effectiveness versus conventional treatment pathway (Figures 1a–1e)
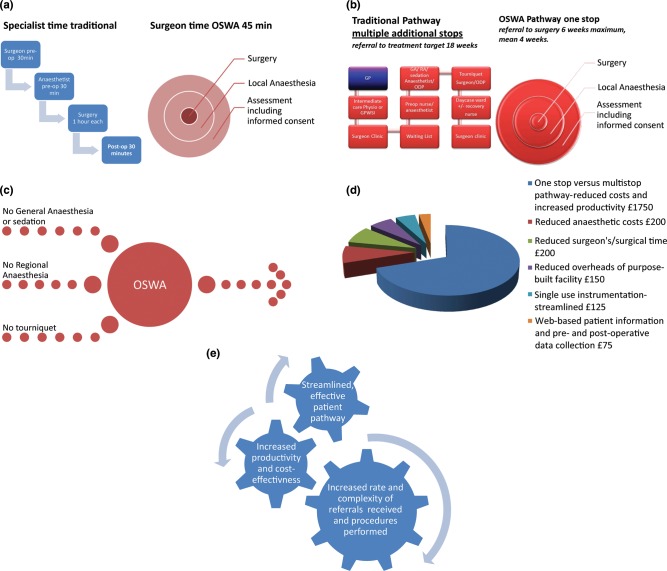
Figure 1.
Time and cost savings with OSWA approach. (a) Traditional versus OSWA Specialist's time. (b) Traditional versus OSWA pathway. (c) OSWA reduced theatre surgical time. (d) Breakdown of £2500 Dupuytren's cost saving per case. (e) OSWA service, efficiency and cost-effectiveness interlinkage
Our audit data confirms increased efficiency and cost-effectiveness with the OSWA approach: which overall is on account of the single-stop model and the purely local anaesthetic approach. More specific cost and efficiency savings are as follows.
The OSWA service centres upon complete surgical care delivered in one stop, that is: one episode only of 30–45 minutes of the surgeon's time (Figure 1a). Our audit data confirms all one thousand cases in the analysis had surgical care delivered within forty-five minutes. This contrasts with the conventional pathway for complex procedures (such as Dupuytren's contracture surgery, ulnar nerve decompression and complex ganglia) which will usually involve in excess of 3½ hours of specialist time: orthopaedic surgeon's preoperative consultations in the clinic and on the day of surgery (30 minutes); anaesthetic preoperative consultations including day of surgery (30 minutes); anaesthetist's clinical time in theatre (1 hour); surgeon's time in theatre (1 hour); postoperative specialist time (30 minutes).
The traditional pathway entails multiple ‘stops’ and an eighteen week target wait between receipt of referral and the completion of surgical care (Figure 1b). This contrasts with the OSWA model which involves one stop only, and our data confirms all patients receive their OSWA slot within six weeks of our receipt of referral, with a mean wait of four weeks between receipt of referral and delivery of OSWA surgical care.
The OSWA model consistently achieves complete surgical care within 45 minutes maximum management time. This is partly due to streamlining of the service as a whole, but in theatre time-savings are on account of obviating general or regional anaesthesia, sedation and tourniquets (Figure 1c).
Regarding cost-effectiveness, the streamlined OSWA service is able to provide safe and effective care (see above) for 25–50% of the national tariff price. This is again linked to the streamlining and efficiency documented above and below. For Dupuytren's contracture, the local primary care Trust saves in the region of £2500 by commissioning via the OSWA service (versus the national tariff for single digit Dupuytren's surgery) . Our analysis demonstrates that we are able to pass on the savings to the NHS that we make through: a totally one-stop service; reduced anaesthetic costs; reduced specialist time; reduced overheads; single-use and streamlined instrumentation; and web-based patient information and, preoperative data collection (Figure 1d).
Finally, over the decade of service optimization we have increasingly seen the cycle of efficiency, productivity and scope (Figure 1e). Thus, as the service expands with the number, range and complexity of procedures performed, we are able to pass on increased cost savings to the NHS. Moreover, the extremely low DNA rate is a marker of our effective and streamlined service, and means that again our productivity hence cost effectiveness is maximized.
Discussion
With the evolution of healthcare provision there is increasing interest in daycase surgery, non-hospital surgical services and alternative treatment pathways.1 There are continuing efforts to optimize the link between GPs and orthopaedic services.2,3 Efficiency and cost-effectiveness are increasingly important. Over recent years, there has been increasing use of extended scope practitioners (physiotherapists) as a link between primary and secondary care.2,3 Advocates site short-term reduction in referrals to secondary care as a measure of success of these initiatives.2,3 Long-term outcomes are awaited.
Our model places an experienced orthopaedic surgeon in the primary care setting. Our ethos is to empower the GP and provide easy access to orthopaedic advice and treatment. Thus, for a patient with a musculoskeletal problem they can chose to treat themselves, refer to physiotherapy, refer to the one-stop pathway or refer to conventional secondary care. Other models place physiotherapists in between primary and secondary care; ours places secondary care experience and expertise within primary care.
Previous studies have demonstrated the potential of minor surgery in GP's surgeries.4 In Brown et al's study,4 four GPs performed various types of minor surgery on 513 patients with good outcomes. The service was cost-effective and efficient. Targeted orthopaedic training of GPs might enable a GP-led one-stop service.5 However, our model centres upon the provision of an experienced orthopaedic surgeon within primary care; and is designed to divest increasingly busy GPs of: difficult orthopaedic decisions, time-consuming therapeutic consultations and unnecessary obstacles to specialist input.
In our experience the quality of referrals is very high, as reflected in the 1000-case analysis. Because the one-stop service is all-encompassing, the onus is not on the GP or intermediate practitioner to make the definitive diagnosis. All patients referred in the above analysis were suitable for one-stop management and none were rejected or referred for in-hospital treatment.
We have optimized the one-stop pathway by building upon previous author's experiences of pilot one stop services.6 Thus, surgery is performed under local anaesthesia using no tourniquet. The tourniquet is probably the limiting factor in most upper limb orthopaedic practices, since it can only be tolerated for relatively short periods of time in a wide-awake patient. In our experience the tourniquet causes the patient unnecessary pain and this is substantiated by the literature.7 Our technique using adrenaline and local anaesthetic is proven.8–10 From our experience there are certain key points which much be adhered for successful one-stop wide-awake care (Tables 1 and 2). We have embraced and developed the one-stop care which has previously been described by others.11 Overall, we would suggest that the ethos and aims for successful one-stop wide-awake care are: to provide a consultant-led patient-centred specialist service in an informal, relaxed and efficient environment; with efficient but thorough patient care.
Table 1.
Keys to successful one-stop wide-awake management
| No tourniquets |
| • Too painful for the patient |
| • Unnecessary |
| Local anaesthetic technique |
| • 2% lignocaine with adrenaline 1:200,000 |
| • Plain lignocaine for digits |
| • Infiltrate in theatre prior to scrub to allow anaesthetic to work |
| Careful surgical dissection and meticulous technique |
| • Point bleeding managed with pressure from rolled small swab. |
| Experienced, small team with clear and defined roles |
| • Surgeon calls and sees patients: |
| ○ Simple health questionnaire brought to consultation by patient. |
| ○ Pre-consultation information sent to patient and provided in waiting area. |
| ○ Focused consultation with thorough discussion of pros and cons, and risks and benefits of treatment. |
| • Healthcare support worker manages patient flow and acts as ‘runner’ |
| • Theatre nurse manages instruments |
| Compact functional outpatients and theatre space |
| • Waiting area juxtaposed between clinic room and theatre space |
| Single use surgical equipment |
| • See Table 2 |
| Experienced and efficient support staff; with patients' self-selected one-stop slots (minimizes DNAs). |
| Capacity and adequacy: two full days of one-stop management per week; 6 one-stop patients per session plus capacity to see any patients with problems. |
| Efficient, thorough evidence-based treatment with robust audit and governance facilities/mechanizms/processes. |
Table 2.
Typical Equipment Required and Practical Considerations (All single use)
| Basic | ✓ Hand table |
|---|---|
| ✓ 1 small drape ✓ 1 large drape ✓ 1 extremity drape ✓ Scalpel plus 1 × 15 blade ✓ Fine toothed forceps ✓ 1 pack of small swabs ✓ 1 × 5ml syringe ✓ 1 × 21 gauge needle ✓ 1 × 25 gauge needle ✓ 5ml × 2% lignocaine with adrenaline 1:200 000 ✓ 1 × melanin dressing ✓ 1 pack dressing gauze ✓ 4 inch crepe bandage ✓ 1 × 3–0 silk skin suture & needle holder |
|
| Carpal Tunnel Decompression | ✓ Self-retainer with ratchet (Wests) ✓ Second blade ✓ MacDonald dissector |
| Dupuytren's Contracture | ✓ Alice forceps ✓ Small skin hooks × 2 ✓ Large skins hooks × 2 |
| Ganglion Simple | ✓ cat's-paw retractors |
| Ganglion Complex (radial artery territory, large dorsal wrist ganglia) |
✓ Bipolar diathermy |
| Triggering Digit | ✓ cat's-paw ratractors |
| Ulnar nerve decompression | ✓ 1 × small sandbag ✓ 1 × large sandbag ✓ Nerve hook plus blunt and sharp scissors ✓ cat's-paw retractors |
| De Quervain's release | ✓ cat's-paw retractors |
| Mucous Cyst | ✓ single skin hooks ✓ small curette/ spoon |
| Available as necessary | ✓ Artery forceps/ clips/ mosquito forceps ✓ Range of sutures ✓ Langenbeck retractors ✓ Nibblers ✓ Osteotomes ✓ Tendon/nerve hooks |
| Surgery on Digits | ✓ Finger dressings (elasticated) ✓ 2 inch crepe bandage ✓ 5 ml × 2% lignocaine plain |
In our experience, and indeed for the 1000 cases presented, orthopaedic cases referred to the one-stop service did not require in-hospital treatment, physiotherapy or further tests. Through the one-stop wide-awake service the GP has easy and prompt access to a definitive orthopaedic opinion and treatment. For the 1000 cases presented, one-stop management was not deferred or postponed on account of investigation. For most of the conditions we treat, an experienced consultant will make a clinical diagnosis. Carpal and cubital tunnel syndrome are clinical diagnoses.12 Often the GP has organized nerve conduction studies prior to the referral; and in any case the ‘Biro test’, which one of the senior authors (QMKB) developed, can be performed easily during the one-stop consultation as a useful adjunct.13 We suggest one-stop care is ideal for the conditions listed above. We recently treated a case of Dupuytren's contracture who was referred to intermediate care, had X-rays and an ultrasound scan and was referred to us after a delay of six months; who quite rightly asked why the referral had not been made to the one-stop service initially.
Increasingly, more complex cases are being performed through a one-stop wide-awake approach. Whilst two North American studies9,10 have demonstrated that selective Dupuytren's fasciectomy under local anaesthesia is safe and effective, we are, as far as we are aware, the only Dupuytren's service in the UK which offers surgery under local anaesthesia for all stages of the contracture including revisions (Figure 2). Clearly, an experienced surgeon needs to steadily adapt his or her technique to successful wide-awake surgery. The ethos is to provide a consultant surgeon-led total one-stop wide-awake orthopaedic service rather than a service which offers selective operations under local anaesthesia. This in turn results in increased productivity, efficiency and cost-saving. We are increasingly using the service website for delivery of patient information and data collection for outcomes, audit and governance. This again saves time and reduces costs; and in our experience the modern patient appreciates a service with web support.
Figure 2.
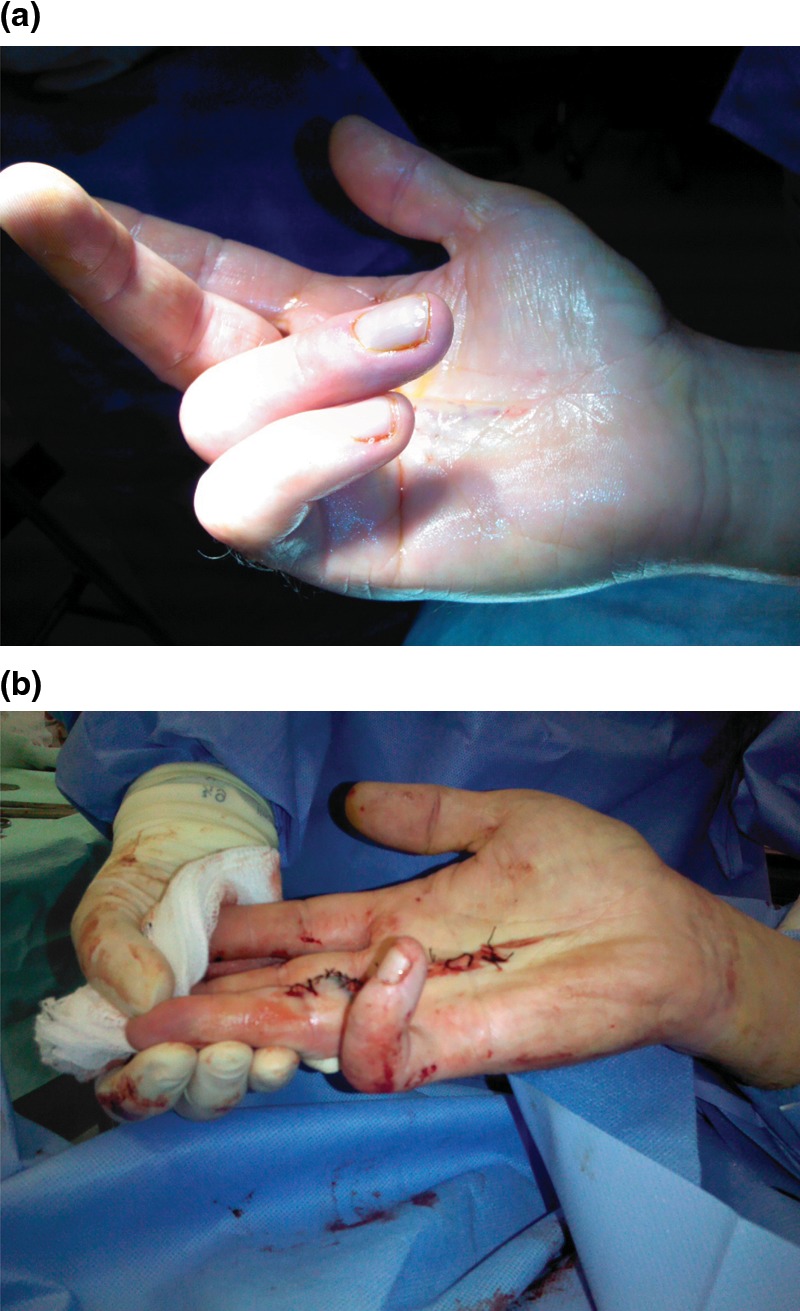
(a) and (b) 40-year-old man with recurrent ring finger Dupuytren's following surgery under general anaesthesia several years previously; immediate pre-and postoperative photographs
This study demonstrates that most upper limb orthopaedic problems can be successfully treated through a one-stop service run by an orthopaedic surgeon in primary care. We suggest that the model could be adapted to many other surgical specialties and subspecialties.
Over the last 10 years the county-wide primary care surgical scheme has evolved and progressed in tandem with our service. On the basis of the success of the total one-stop wide-awake approach to orthopaedic surgery, steadily more conditions have been deemed by the primary care trust as being (only) suitable for wide-awake treatment. Moreover, the success of our model is such that even complex conditions such as Dupuytren's Contracture are only treated in this setting across the county; unless exceptional circumstances can be demonstrated through a funding application. The number and complexity of referrals documented above, further reinforces the success of the model. Over the last few months the local PCT have started to commission ulnar nerve decompression via our approach, and we are now performing increasing numbers of this operation each week.
Our model is efficient and cost-effective with excellent outcomes and patient satisfaction; and has great potential in the context of modern and evolving healthcare services. The one-stop wide-awake model has the potential to secure surgical services for NHS patients through increased efficiency and vastly reduced costs.
DECLARATIONS
Competing Interests
None declared
Funding
No authors have received funding or sponsorship for this paper or the associated audit
Ethical approval
This is a retrospective audit and review of service hence no ethical approval has been sought
Guarantor
QB
Contributorship
All authors have contributed to this paper and have given permission for their names to be included as co-authors. The above authors have all contributed directly to the development of the OSWA service, the data collection for and authorship of the paper; hence all listed authors are contributors
Acknowledgements
Audit and all surgery performed at: Parkside One-Stop Wide-Awake, Orthopaedic Centre,Boston, Lincolnshire, PE21 6PF
Reviewer
Charlie Talbot
References
- 1.Iossifidis A, Bismil Q, Lakkireddi P, Mekala V, Nethirasigamani D, Menon G Total daycare shoulder surgery. Shoulder & Elbow 2009;1:25–28 [Google Scholar]
- 2.Evaluation of 'Closer to Home' Demonstration Sites http://www.npcrdc.ac.uk/Evaluation_of_Closer_to_Home_Demonstration_Sites.htm (last accessed 1 January 2010)
- 3.Hattam P, Smeatham A Evaluation of an orthopaedic screening service in primary care. Clin Perform Qual Health Care 1999;7:121–4 [PubMed] [Google Scholar]
- 4.Brown JS, Smith RR, Cantor T, Chesover D, Yearsley R General practitioners as providers of minor surgery–a success story? Br J Gen Pract 1997;47:205–10 PMCID: PMC1312943 [PMC free article] [PubMed] [Google Scholar]
- 5.Duckett S, Casserly H Orthopaedic GP Fellowship: does it work? Ann R Coll Surg Engl 2003;85:195–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kashani S, Muhtaseb M, Robinson F Analysis of 'one-stop' referral system for ophthalmic minor operations by GPs. Br J Gen Pract 2005;55:53–4 [PMC free article] [PubMed] [Google Scholar]
- 7.Røjskjær J, Foss NB, Kristensen BB No evidence for routine use of tourniquet during orthopaedic surgery. Ugeskr Laeger 2011;173:3097–100 [PubMed] [Google Scholar]
- 8.Gibson M Outpatient carpal tunnel decompression without tourniquet: a simple local anaesthetic technique. Ann R Coll Surg Engl 1990;72:408–9 [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson R, Higgins A, Conrad J, Bell M, Lalonde D The Wide-Awake Approach to Dupuytren's Disease: Fasciectomy under Local Anesthetic with Epinephrine. Hand (N Y). 2009. Nov 10. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Denkler K Dupuytren's fasciectomies in 60 consecutive digits using lidocaine with epinephrine and no tourniquet. Plast Reconstr Surg 2005;115:802–10 [DOI] [PubMed] [Google Scholar]
- 11.Gaskell A, McLaughlin A, Young E, McCristal K Direct optometrist referral of cataract patients into a pilot 'one-stop' cataract surgery facility. J R Coll Surg Edinb 2001;46:133–7 [PubMed] [Google Scholar]
- 12.Graham B The Value Added by Electrodiagnostic Testing in the Diagnosis of Carpal Tunnel Syndrome. The Journal of Bone and Joint Surgery (American) 2008;90:2587–93 [DOI] [PubMed] [Google Scholar]
- 13.Kumar A, Bismil Q, Morgan B, Ashbrooke A, Davies S, Solan M The ‘biro test’ for autonomic dysfunction in carpal tunnel syndrome. J Hand Surg Eur Vol 2008;33:355–7 [DOI] [PubMed] [Google Scholar]