Abstract
Exposure to traumatic events often results in severe distress which may elicit self-medication behaviors. Yet, some individuals exposed to trauma do not develop post-traumatic stress symptoms and comorbid addictive impulses. In the wake of traumatic events, psychological processes like thought suppression and mindfulness may modulate post-traumatic stress and craving for substances. We examined the differential roles of mindfulness and suppression in comorbid post-traumatic stress and craving in a sample of 125 persons with extensive trauma histories and psychiatric symptoms in residential treatment for substance dependence. Results indicated that thought suppression, rather than extent of trauma history, significantly predicted post-traumatic stress symptom severity while dispositional mindfulness significantly predicted both post-traumatic stress symptoms and craving. In multiple regression models, mindfulness and thought suppression combined explained nearly half of the variance in post-traumatic stress symptoms and one-quarter of the variance in substance craving. Moreover, multivariate path analysis indicated that prior traumatic experience was associated with greater thought suppression, which in turn was correlated with increased post-traumatic stress symptoms and drug craving, whereas dispositional mindfulness was associated with decreased suppression, post-traumatic stress, and craving. The maladaptive strategy of thought suppression appears to be linked with adverse psychological consequences of traumatic life events. In contrast, dispositional mindfulness appears to be a protective factor that buffers individuals from experiencing more severe post-traumatic stress symptoms and craving.
Keywords: craving, comorbidity, mindfulness, post-traumatic stress, thought suppression
1. Introduction
Exposure to traumatic life events often results in adverse psychological and behavioral consequences. Yet, not all individuals exposed to severe adversities develop clinical symptoms (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). How is it that people facing similar stressors can have such markedly different outcomes and resiliencies? Transactional models (c.f., Lazarus & Folkman, 1984) propose that the stress reaction is mediated by appraisal and coping processes. According to this theoretical perspective, the emotional response to the stressor is modulated by cognitive responses, which, in turn, modify the stress appraisal and influence subsequent affective and behavioral reactions. Thus, cognitive coping processes may be conceptualized as being situated in a feedback circuit which may attenuate, sustain, or exacerbate the stress reaction and its consequences over time.
Many individuals exposed to traumatic life events cope with trauma through the use of psychoactive substances. Indeed, data from the National Epidemiologic Survey on Alcohol and Related Conditions indicate that approximately 20% of individuals with post-traumatic stress disorder (PTSD) use substances to relieve their symptoms (Leeies, Pagura, Sareen, & Bolton, 2010). Trauma exposure is associated with heightened risk for developing substance use disorders (Jacobsen, Southwick, & Kosten, 2001). Moreover, men and women with post-traumatic stress disorder (PTSD) exhibit more than twice the rate of substance abuse and dependence than persons without PTSD (Breslau, Davis, & Schultz, 2003; Mills, Teesson, Ross, & Peters, 2006). Furthermore, clinical anecdotes point to the likelihood that traumatized individuals use psychoactive substances as means of self-medicating the dysphoric mood, intrusive cognitions, and psychophysiological sequelae of trauma (Khantzian, 1997). Situations that evoke and involve negative emotion are the most commonly cited precipitants of relapse (Lowman, Allen, & Stout, 1996). The temporary relief obtained via the anxiolytic properties of select psychoactive agents may become a powerful negative reinforcer (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004), leading to entrenchment of this coping pattern as an addictive response that may be reactivated by subsequent stressors (Garland, Boettiger, & Howard, 2011).
Thus, when persons with histories of using substances to cope with stress and negative affect are confronted with a stressor, this encounter may elicit a powerful conditioned response, subjectively experienced as craving (Ludwig & Wikler, 1974; Poulos, Hinson, & Siegel, 1981; Skinner & Aubin, 2010; Stewart, De Wit, & Eikelboom, 1984). The craving experience is characterized as involving a sense of dysphoria or anxiety coupled with distressing somatic sensations (Bergquist, Fox, & Sinha, 2010), and is marked by intrusive images and thoughts about the desired substance (Merikle, 1999). In response to such intrusions, persons may initiate substance use, or they may attempt to inhibit or ignore the drive to use. Tiffany (1990) posited that when addicts attempt to suppress the automatic, conditioned appetitive response, they experience an upwelling of craving that may become so unpleasant that the individual consumes the substance in an effort to relieve craving-induced distress.
The suppression of unwanted thoughts and feelings is a cognitive strategy that may also be used to cope with trauma. Exposure to traumatic events may trigger post-traumatic stress disorder (PTSD), characterized by recurrent, distressing symptoms, including intrusive cognitions, images, memories, and emotions associated with the original trauma (Dunmore, Clark, & Ehlers, 2001; Ehlers et al., 2002; Greenberg, 1995; Holmes, Grey, & Young, 2005). In an attempt to cope with such intrusions, individuals may engage in attempts to suppress the unwanted thoughts or feelings. Ironically, suppression may foster the intrusive trauma-related cognitions that are the hallmark of PTSD (Tull, Gratz, Salters, & Roemer, 2004), by interfering with the emotional processing of the traumatic memory and preventing its successful integration into long-term memory (Elzinga & Bremner, 2002; Foa & Kozak, 1986) and mediating the influence of negative moods on PTSD symptoms (Rosenthal, Cheavens, Lynch, & Follette, 2006). In this respect, thought suppression significantly predicts the occurrence of PTSD one and even three years after a motor vehicle accident (Ehlers, Mayou, & Bryant, 1998; Mayou, Ehlers, & Bryant, 2002). Deliberate thought suppression in laboratory settings has also been shown to exacerbate intrusive thoughts related to the original trauma; for instance, experimental induction of suppression of thoughts related to a motor vehicle accident resulted in a transient decrease in thoughts about the trauma, followed by a resurgence of twice as many thoughts related to the accident than the pre-suppression level (Beck, Gudmundsdottir, Palyo, Miller, & Grant, 2006).
Thus, suppression inadvertently results in a “rebound effect,” i.e., an increased rate of the thoughts and emotions it is directed against (Wegner, Schneider, Carter, & White, 1987; Wenzlaff & Wegner, 2000). This effect may be explained by Wegner’s ironic process theory (Wegner, 1994), which asserts that suppression involves two processes: a) a conscious search for cognitive contents consistent with the desired mental state, and b) an implicit monitoring process that searches continually for cognitions that are inconsistent with the desired state. When attention is automatically deployed in search of undesirable mental content to be replaced, the ensuing positive feedback loop leads to hyperaccessibility of unwanted cognitions (Wegner & Erber, 1992), amplifying their frequency and intensity under conditions of stress (Nixon, Cain, Nehmy, & Seymour, 2009). As a result, the intrusive and distressing nature of the target thoughts is magnified by the very process employed to avoid them (Abramowitz, Tolin, & Street, 2001).
When sustained over time, suppression may exhaust the capacity for self-regulation, which Baumeister and colleagues have characterized as a limited resource that is depleted through repeated acts of self-control (Baumeister, 2003; Muraven & Baumeister, 2000). Thus prolonged suppression of unwanted trauma-related thoughts may undermine subsequent cognitive control efforts (Pu, Schmeichel, & Demaree, 2010). Insofar as trauma and stress may trigger appetitive impulses, post-suppression rebound of trauma-related thoughts may reactivate the drive to use psychoactive substances while exhausting the resources to regulate it, resulting in impaired regulation of urges manifested in increased subjective craving.
In contrast, the adaptive psychological tendency of dispositional mindfulness, a mindset characterized by nonreactive awareness and acceptance (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Garland, Fredrickson, Kring, Johnson, Meyer, & Penn, 2010), may serve as a protective factor and mitigate the pathogenic cycle underpinning the co-occurrence of trauma and addiction. Indeed, in a recent study of undergraduates who had been exposed to traumatic events, Thompson and Waltz (2010) found that mindfulness was significantly inversely associated with post-traumatic stress avoidance symptoms. Other research has identified a robust negative correlation between dispositional mindfulness and thought suppression (Baer et al., 2006). Thus, rather than attempting to avoid or deny experience by suppressing unwanted cognitions or feelings, dispositionally mindful individuals tend to cope with stressful life events by adopting an attitude of nonjudgment, openness, and self-compassion towards their own thoughts and emotions. By coping with stress in this manner, dispositionally mindful persons are better able to extricate themselves from cognitive perseveration (Evans & Segerstrom, 2010), to regulate negative affective states (Coffey & Hartman, 2008), and to disengage attention from addictive cues (Garland, Boettiger, Gaylord, West Channon, & Howard, 2011). Conversely, persons with low levels of mindfulness (i.e., mindlessness) may tend to engage in habitual and counterproductive reactions (Langer, 1992) such as self-medicating traumatic intrusions with alcohol and drugs. Although of potentially considerable clinical importance, associations between dispositional mindfulness, thought suppression, post-traumatic stress symptoms, and craving remain understudied.
Given evidence for the roles of thought suppression and dispositional mindfulness in the cognitive mediation of traumatic stress and appetitive responses, we hypothesized that among substance dependent individuals with extensive trauma histories, a) thought suppression will be associated with elevated symptoms of post-traumatic stress and craving whereas b) dispositional mindfulness will be associated with lower levels of post-traumatic stress symptoms and craving. Furthermore, we hypothesized that c) thought suppression and dispositional mindfulness would statistically mediate the relationship between trauma history, post-traumatic stress symptoms, and craving. We expected that persons with extensive trauma histories would tend toward thought suppression which would partially account for their comparatively more severe post-traumatic stress symptoms and craving. In contrast, we expected individuals with higher levels of dispositional mindfulness to engage in less thought suppression which would partially account for their comparatively lower post-traumatic stress symptoms and craving. The present study provides an empirical test of these hypotheses by examining the proposed associations among a sample of persons with extensive trauma histories in residential treatment for substance dependence.
2. Materials and Methods
2.1 Procedure
Participants were recruited from a residential treatment facility in the Southeastern U.S. serving persons with co-occurring substance dependence and psychiatric disorders. Prior to participating in the research assessment, participants had resided in a therapeutic milieu for six weeks, during which time they were offered vocational training, given peer support, and provided with psychoeducation on biopsychosocial factors in addiction. No other interventions were administered at this time. The research team met with potential participants to explain the purpose of the study, and to assure them that confidentiality would be maintained throughout the research process. Participation in the study was completely voluntary, and participants gave informed consent prior to engaging in research. After consenting, participants completed a set of validated assessment instruments (see section 2.3). Upon completing the research assessment detailed in the present study, participants were engaged in formal, evidence-based interventions for substance use disorders and trauma treatment. However, the present study focused on a cross-sectional analysis of data obtained prior to the start of these interventions. This study was conducted in accordance with the Declaration of Helsinki.
To satisfy study inclusion criteria, potential participants had to meet DSM-IV criteria for one or more substance dependence diagnoses. Substance dependence and other Axis I disorders were diagnosed by licensed and trained clinicians with experience making psychiatric and addiction diagnoses. Clinicians conducted semi-structured psychiatric interviews based on the Mini-International Neuropsychiatric Interview (Sheehan et al., 1998). Potential participants were excluded from the study if they were actively psychotic or homicidal. All participants had abstained from using drugs or alcohol for six weeks prior to the research assessment.
2.2 Participants
A total of 125 individuals who met criteria for one or more substance dependence diagnoses (mean age 38.7, SD = 10.0; 51.5% African American, 39.6% Caucasian; 92% male) agreed to participate in the study, while 13 individuals who met study criteria declined to participate due to lack of interest or scheduling conflicts. The majority of study participants met DSM-IV criteria for cocaine (n = 69, 55.2%) and/or alcohol dependence (n = 66, 52.8%); comparatively fewer participants could be diagnosed with dependence on marijuana (n = 46, 36.8%), heroin (n = 14, 11.2%), and opioids (n = 8, 6.4%), benzodiazepines (n = 6, 4.8%), or amphetamines (n = 5, 4.0%). Many participants met criteria for psychiatric disorders: 35 (28%) participants were diagnosed with major depressive disorder, 11 were diagnosed with generalized anxiety disorder, 6 (4.8%) were diagnosed with bipolar disorder, 1 (0.8%) was diagnosed with a simple phobia, 1 (0.8%) was diagnosed with social anxiety disorder (n = 1, 0.8%), and 14 (11.2%) were diagnosed with another Axis I or II disorder (e.g., personality disorders, attention-deficit-and-hyperactivity disorder). Furthermore, 23 (18.4%) met full diagnostic criteria for PTSD, as established by clinical interview and corroborated with scores from the PTSD Checklist-Civilian Version (see the Measures section below; Weathers et al., 1993). The PTSD Checklist-Civilian Version was used to provide a quantitative estimate of PTSD symptoms.
2.3 Measures
2.3.1 Trauma history
Participants were asked whether or not they had ever experienced each of 10 traumatic events in their lifetime, including: “witnessed someone severely injured or killed in person”; “having been badly hurt or in danger of being badly hurt”; “had something very bad or terrifying happen to you”; “hit by someone who was trying to hurt you”; “been mugged by a weapon or by force”; “attacked with a weapon or by someone trying to hurt or kill you”; “witnessed someone be severely beaten”; “been sexually touched against your will”; “forced to watch sex acts done by another person”; and “forced to do sex acts against your will.” A variable measuring extent of trauma history was calculated by summing the number of affirmative responses to ever having experienced a given category of lifetime trauma (α = .660). For example, if a participant had responded “yes” to having ever “witnessed someone severely injured or killed in person,” “having been badly hurt or in danger of being badly hurt,” and “had something very bad or terrifying happen to you,” they would score a 3 on the trauma history variable.
2.3.2 Post-traumatic stress symptoms
Post-traumatic stress symptoms were assessed with the 17-item PTSD Checklist-Civilian version (PCL-C; Weathers et al., 1993). Participants rated how much they had been bothered by PTSD criterion symptoms as outlined by the DSM-IV over the past month on a Likert scale (1 = not at all, 5 = extremely). A total post-traumatic stress symptom score was calculated by summing responses to each item (α = .915). Responses on the PCL-C reflected post-traumatic stress symptoms resulting from the experience of traumatic events endorsed on the abovementioned measure of trauma history. According to the cutoffs established by Harrington and Newman (2007) via receiver–operator characteristic curve (RO C) analysis, a score of 44 or higher on the PCL-C may be considered to be diagnostic for PTSD among treatment-seeking individuals with substance use disorders. In the present study, all participants who were diagnosed with PTSD according to the clinical interview evidenced PCL-C scores ≥ 44.
2.3.3 Thought suppression
Chronic thought suppression, the counterproductive tendency to avoid or suppress undesirable cognitions and emotions, was assessed with the 15-item White Bear Suppression Inventory (Wegner & Zanakos, 1994) (α = .895). Participants indicated their level of agreement (1 = strongly disagree, 5 = strongly agree) with items such as “I always try to put problems out of mind” and “I often do things to distract myself from my thoughts.” Items were summed to produce a total score, with higher scores indicative of greater trait thought suppression.
2.3.4 Dispositional mindfulness
The Five Facet Mindfulness Questionnaire was used to measure dispositional mindfulness. This scale is comprised of 39 Likert-type items tapping various facets of mindfulness: nonreactivity to inner experience (tapped by items such as “I watch my feelings without getting lost in them”), observing and attending to experience (“I pay attention to sensations, such as the wind in my hair or the sun on my face”), describing and discriminating emotional experiences (“I’m good at finding words to describe my feelings”), nonjudging of experience (“I tell myself I shouldn’t be feeling the way that I am feeling”), and acting with awareness (“I find myself doing things without paying attention”) (Baer, Smith, Hopkins, Krietemeyer, & Toney 2006). Items are summed to produce a total dispositional mindfulness score (α = .924).
2.3.5 Craving
Substance craving was assessed with an adapted version of the Penn Alcohol Craving Scale (Flannery et al., 2001), modified to assess craving for alcohol and other psychoactive substances. The original Penn Alcohol Craving Scale includes five question items that assess the duration, frequency and intensity of craving for alcohol on a 7 -point scale (in the present study, α = .894). In the version adapted for this study the item structure was maintained for the original five items but five additional items were rephrased to inquire about craving for drugs other than alcohol. For Example item 1 of PACS “How often have you thought about drinking or how good a drink would make you feel?” was modified to “How often have you thought getting high, or about how good getting high would make you feel?” These adapted items were summed to create a total drug craving score (α = .895). Then the adapted drug craving items were summed with the alcohol craving items to compute a total substance craving score across all 10 items (α = .910).
2.4 Statistical analyses
Pearson product-moment correlations were used to examine zero-order correlations between study variables. Multiple linear regression analyses were used to test our first and second hypotheses by examining the differential roles of dispositional mindfulness and thought suppression as predictors of post-traumatic stress symptoms and substance craving. In both the regression model predicting post-traumatic stress symptoms and the model predicting craving, number of traumatic events was entered as a covariate in step one. Thought suppression and dispositional mindfulness were entered in step two. Collinearity diagnostics were assessed using conventional cutoffs (tolerance > .20, variance inflation factor < 5.0) to ensure that no multicollinearity was present. In addition, student’s t-tests were used to compare participants who met diagnostic criteria for PTSD (according to established PCL-C cutoffs) to those who did not across trauma history, thought suppression, dispositional mindfulness, and craving variables.
Multivariate path analysis within a structural equation modeling framework, which provides simultaneous estimation of multiple linear equations, was conducted to examine the relationships proposed in our third hypothesis linking trauma history, thought suppression, dispositional mindfulness, post-traumatic stress symptoms, and substance craving. Path analysis has advantages over multiple regression analysis in that it allows the researcher to simultaneously estimate specific associations between multiple independent and dependent variables. In path analysis a variable can be represented as both a predictor and a criterion variable in the same model – unlike regression analysis where in any given model a variable must be either a predictor or criterion variable (Kline, 1998). Conducting separate regression analyses may also omit or ignore important intercorrelations among the criterion variables. AMOS 17.0 was used to calculate model parameters, and missing data were handled using full-information maximum likelihood estimation. Model fit was determined comparing fit indices to widely accepted cut-offs (Kline, 1998), including nonsignificant χ2 (p > .05), comparative fit index (CFI) > 0.90, and the root-mean square error of approximation (RMSEA) < 0.08.
3. Results
3.1 Prevalence of trauma in the sample
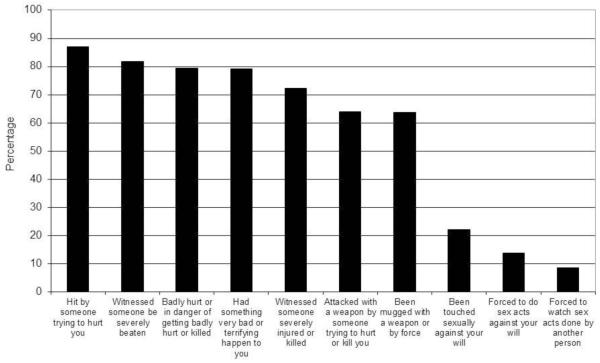
Participants reported having experienced a wide range of traumatic incidents (see Figure 1 for the lifetime prevalence of various traumatic experiences). Approximately 80% of participants reported having been struck by someone who had attempted to hurt them, having witnessed someone else being severely beaten, having been in danger of getting badly injured or killed, or experiencing a terrifying event. Nearly two thirds of participants had been mugged or attacked with a weapon. Fewer participants reported experiencing sexual abuse or rape. On average, participants had experienced 5.3 (SD = 2.1) different categories of traumatic life events.
Figure 1.
Lifetime prevalence of various traumatic experiences among study participants.
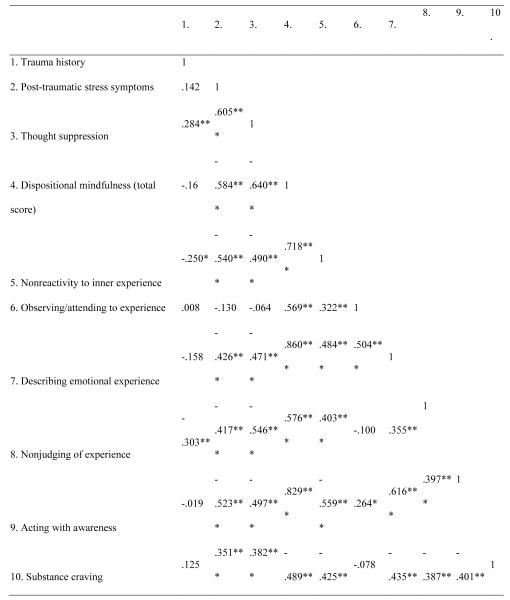
3.2 Bivariate correlations between trauma history, post-traumatic stress symptoms, thought suppression, dispositional mindfulness, and substance craving
Correlation coefficients for variables of interest are reported in Table 1. Extent of trauma history was significantly positively associated with thought suppression and significantly negatively associated with the dispositional mindfulness facets of nonreactivity and nonjudging, but was not correlated with post-traumatic stress symptoms or craving. Post-traumatic stress symptom level was significantly positively associated with thought suppression and craving, and significantly negatively associated with the total dispositional mindfulness score and the mindfulness facets of nonreactivity, nonjudging, describing emotional experience, and acting with awareness. Craving and thought suppression were also significantly negatively associated with dispositional mindfulness and these four mindfulness facets.
Table 1.
Bivariate Correlations Between Trauma History, Post-Traumatic Stress Symptoms, Thought Suppression, Dispositional Mindfulness, Mindfulness Facets, and Substance Craving in Adults with Substance Dependence Disorders
|
|
3.3 Relationship of trauma history, thought suppression, and dispositional mindfulness to post-traumatic stress symptoms
Multiple linear regression indicated that thought suppression and dispositional mindfulness significantly predicted post-traumatic stress symptom severity after controlling for extent of trauma history (see Table 2). Overall, the model explained nearly half of the variance in post-traumatic stress symptoms (Model R2 = .49).
Table 2.
Regression models of thought suppression and dispositional mindfulness on PTSD symptoms and craving.
| B | S.E. | Beta | t | |
|---|---|---|---|---|
| Outcome: Post-traumatic stress symptomsa | ||||
| Trauma history | −1.206 | .612 | −.173 | −1.970 |
| Thought suppression | .618 | .135 | .518 | 4.578*** |
| Dispositional mindfulness | −.182 | .069 | −.282 | −2.625* |
| Outcome: Cravingb | ||||
| Trauma history | −.152 | .611 | −.026 | −.249 |
| Thought suppression | .234 | .135 | .234 | 1.738 |
| Dispositional mindfulness | .185 | .069 | .344 | −2.683** |
p < .05
p < .10
p < .001
R2 = .49
R2 = .25. (N = 125).
3.4 Relationship of trauma history, thought suppression, and dispositional mindfulness to craving
Multiple linear regression indicated that dispositional mindfulness, rather than thought suppression or extent of trauma history, significantly predicted craving (see Table 2). Overall, the model explained one quarter of the variance in craving (Model R2 = .25).
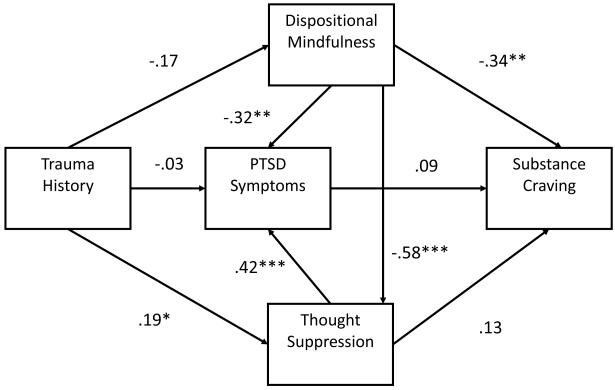
3.5 Multivariate path analysis
Our multivariate path model (see Figure 2) exhibited excellent empirical fit, χ2/df = .05, p = .82; CFI = 1.00; RMSEA = .00 (.00, .15). Participants with more extensive trauma histories had a greater tendency to engage in thought suppression, which in turn was correlated with more severe post-traumatic stress symptoms. In contrast, the association between extent of trauma history and dispositional mindfulness was non-significant. Yet, participants reporting higher levels of dispositional mindfulness tended to engage in less thought suppression, which in turn was associated with less severe post-traumatic stress symptoms. Similarly, persons with higher levels of dispositional mindfulness tended to report less craving, although this association was not accounted for by thought suppression.
Figure 2.
Multivariate path model depicting relationships between trauma history, post-traumatic stress symptoms, thought suppression, dispositional mindfulness, and craving among a sample of substance dependent adults (N = 125). * p < .05, ** p < .01, *** p < .001.
3.5 Differences in trauma history, thought suppression, dispositional mindfulness, and craving between individuals with and without PTSD
We compared the 23 participants who met diagnostic criteria for PTSD (as determined by clinical interview and corroborated by PCL-C scores above the cutoff score of 44 previously established by ROC analysis (Harrington & Newman, 2007) to those who did not (n = 102) across trauma history, thought suppression, dispositional mindfulness, and craving variables. Due to the unequal subsample size, we used Levene’s test to assess the homogeneity of variances between the PTSD and non-PTSD groups, and used adjusted t-test calculations when equal variances could not be assumed. Participants who met diagnostic criteria for PTSD evidenced significantly higher levels of thought suppression (p < .001, d = 1.38) and craving (p = .001, d = .81), and significantly lower levels of dispositional mindfulness (p < .001, d = 1.43), than participants who did not meet criteria for PTSD. In contrast, there were no significant differences in trauma history between participants who did and did not meet criteria for PTSD (p = .95, d = .43).
4. Discussion
Current study findings revealed that among a sample of treatment-seeking individuals with comorbid substance dependence, psychiatric disorders, and extensive trauma histories, thought suppression was significantly associated with post-traumatic stress symptoms, whereas lifetime exposure to traumatic events was not. In contrast, dispositional mindfulness was significantly inversely associated with post-traumatic stress symptoms and craving. Although the present data is cross-sectional and cannot be used to establish causal relations, study findings are consistent with the notion that the manner in which one cognitively copes with traumatic events is robustly associated with the co-occurrence of post-traumatic stress and addictive urges.
Indeed, while nearly 61% of men and 51% of women in the U.S. report having experienced at least one traumatic event during their lives, the lifetime occurrence of PTSD ranges between 6% and 9% (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Hence, the majority of people who experience trauma do not develop PTSD, in spite of having been exposed to severely adverse and often life-threatening events. Our own data support these observations; in the present sample, substance dependent individuals who met diagnostic criteria for PTSD had similar trauma histories to those who did not meet criteria for PTSD. Conversely, study participants with PTSD could be distinguished from their counterparts with regard to their greater tendency toward engaging in thought suppression, their lower levels of dispositional mindfulness, and their more severe craving for drugs and alcohol. Such findings point to a central proposition of transactional stress and coping theory (Lazarus & Folkman, 1984): it is not the stressor event itself, but rather the way in which the event is appraised and coped with, that determines the magnitude and quality of the stress reaction. In line with this proposition, among victims of childhood sexual abuse, variation in post-traumatic stress symptom severity is better accounted for by the use of avoidance than by the severity of the original trauma (Batten, Follette, & Aban, 2001; Polusny & Follette, 1995; Rosenthal, Rasmussen Hall, Palm, Batten, & Follette, 2005).
Our path analytic findings highlight the potential importance of cognitive factors in the mediation of post-traumatic stress symptoms and craving for psychoactive substances. Study results indicate that among substance dependent individuals exposed to traumatic life events, the association between trauma exposure and post-traumatic stress symptoms was statistically mediated by thought suppression. Hence, the extent to which these individuals engaged in thought suppression following trauma exposure partially accounted for the magnitude of their post-traumatic stress symptoms. Furthermore, the inverse association between dispositional mindfulness and post-traumatic stress symptoms was also statistically mediated by thought suppression. Substance dependent individuals exposed to trauma who reported higher levels of dispositional mindfulness tended to engage in less thought suppression, which in turn was related to their lower levels of post-traumatic stress symptoms. Although we identified a significant zero-order correlation between post-traumatic stress symptoms and craving, this relationship became non-significant when we accounted for potential cognitive mediating variables in our multivariate model. Contrary to our expectations, thought suppression did not statistically mediate the association between post-traumatic stress and craving. In contrast, dispositional mindfulness remained inversely associated with craving when a number of other variable relationships were controlled in the model, attesting to the robustness of the association between mindfulness and appetitive regulation.
It is possible that the maladaptive strategy of thought suppression may inadvertently amplify post-traumatic stress symptoms through ironic processes (Wegner, 1994), which have been linked with depletion of neurocognitive resources needed to regulate implicit urges towards psychoactive substances (Garland et al., 2012). Conversely, dispositionally mindful individuals who cope by adopting a nonjudgmental awareness and acceptance of trauma-related thoughts and emotions may be less likely to develop post-traumatic stress symptoms and may have greater capacity to downregulate craving. Relatedly, research suggests that mindful acceptance mediates post-traumatic stress and self-medication motives (Vujanovic, Bonn-Miller, & Marlatt, 2011), while other studies have identified associations between dispositional mindfulness, addiction-related cognitive processes, and stress-precipitated substance cue-reactivity (Garland, 2011; Garland, Boettiger, Gaylord, et al., in press). Moreover, among substance users, decreases in thought suppression have been shown to mediate the effect of mindfulness training on substance use (Bowen, Witkiewitz, Dillworth, & Marlatt, 2007), and mindfulness training appears to attenuate the relationship between negative emotion and craving (Witkiewitz & Bowen, 2010). Furthermore, mindfulness training led to significantly reduced thought suppression that was correlated with decreased alcohol attentional bias and increased autonomic recovery from stress and addictive cues (Garland et al., 2010). On the contrary, lack of mindfulness (i.e., mindlessness, see Langer, 1992) may be a risk factor for persons with co-occurring disorders; indeed, study participants who scored low on the “acting with awareness” facet of the five facet mindfulness questionnaire tended to have higher levels of post-traumatic stress symptoms and craving, suggesting that habitual, reflexive responding can confer vulnerability to individuals in recovery. To be clear, the cross-sectional nature of the present study prevents causal explanations of the relationships posited by our regression and path models, and some of these relationships may in fact be bidirectional or recursive. Longitudinal, prospective investigations, clinical trials, and experimental laboratory research are needed to test causal models linking trauma history, thought suppression, post-traumatic stress symptoms, craving, and dispositional mindfulness. Future clinical trials could examine effects of mindfulness and thought suppression on the development of PTSD symptoms and drug craving after exposure to an adverse event.
While the path model tested in this study provides a general depiction of the cognitive processes connecting adverse psychiatric and substance-related outcomes to exposure to traumatic life events, future research should further detail each stage in the process. For example, although our path analyses suggest that higher levels of thought suppression are associated with elevated substance craving, the mechanisms that mediate this association remain unspecified. Studies suggest that thought suppression leads to hyperaccessibility of substance-related cognitions (Klein, 2007; Palfai, Monti, Colby, & Rohsenow, 1997). Furthermore, thought suppression may deplete the neurocognitive resources necessary for regulating craving and disengaging attention from substance-related cues as manifested by effects on autonomic cue-reactivity (Garland, Carter, Ropes, & Howard, 2012). Future research should integrate measures of attention (e.g., dot probe task, see Field & Cox, 2008; MacLeod, Mathews, & Tata, 1986), implicit cognition (e.g., emotional Stroop task, see Cox, Hogan, Kristian, & Race, 2002; Williams, Mathews, & MacLeod, 1996), and psychophysiological cue-reactivity (Carter & Tiffany, 1999) into path models linking trauma, post-traumatic stress, and craving. In addition, we did not have access to a measure of substance use frequency and quantity. Differences in the frequency and quantity of substance use might have accounted for some of the observed relationships, and therefore, future studies should control for these variables as model covariates.
The present study was also limited by the use of a relatively “low-resolution” measure of trauma history. Participants were queried with dichotomous items about whether they had ever experienced a broad spectrum of traumatic events in their lifetime. Had we utilized a measure of the exact number of traumatic events ever experienced, our analyses may have yielded different results. It may be, for instance, that persons meeting diagnostic criteria for PTSD had a higher total number of traumatic events, despite having experienced a near equivalent number of categories of traumatic events. Indeed, prior epidemiological studies have found that the number of traumatic events experienced is a significant predictor of PTSD (Breslau, Chilcoat, Kessler, & Davis, 1999; Perkonigg, Kessler, Storz, Wittchen, & others, 2000). Conversely, certain types of traumatic events may be most strongly predictive of PTSD (Norris, 1992). As such, current study findings and path models should be replicated using a more fine-grained measure of trauma history. However, it should be noted that when trauma history and severity of the current traumatic event are statistically controlled, cognitive factors continue to predict PTSD symptoms 6 and 9 months after the occurrence of a traumatic event (Dunmore et al., 2001). Thus, in spite of the aforementioned limitations, the present findings add to a growing body of research attesting to the importance of cognitive factors in mediating the association between trauma and both post-traumatic stress and craving.
To advance treatment development efforts, it is crucial to target cognitive risk mechanisms such as thought suppression that may mediate the effects of exposure to stressful and traumatic life events on addictive behavior. In turn, identification of malleable psychological processes like mindfulness that can counter risk mechanisms implicated in co-occurring disorders is a key step towards designing targeted interventions for persons in recovery from addiction.
Highlights.
Among addicts, mindfulness and thought suppression explained half of the variance in post-traumatic stress.
Mindfulness was inversely associated with craving.
Suppression and mindfulness mediate the effect of trauma history on PTSD and craving.
Acknowledgments
Role of the funding source
Support for the preparation of this article was provided by grant number DA032517 from the National Institute on Drug Abuse (NIDA) awarded to ELG. Support for the conduct of this research was provided by grant numbers TI 020489 from the Substance Abuse and Mental Health Services Administration (SAMHSA) awarded to ARL. Neither NIDA nor SAMHSA had any role in the study design, collection, analysis or interpretation of data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
With regard to our respective contributions to the present manuscript, ELG and ARL designed the study. ARL managed the data collection for the study. ELG reviewed the literature and undertook the statistical analysis. ELG and ARL both contributed to the development of the manuscript.
Conflict of Interest
All authors declare they have no conflicts of interest.
Contributor Information
Eric Garland, Florida State University
Amelia Roberts-Lewis, University of North Carolina at Chapel Hill
References
- Abramowitz JS, Tolin DF, Street GP. Paradoxical effects of thought suppression: a meta-analysis of controlled studies. Clinical Psychology Review. 2001;21:683–703. doi: 10.1016/s0272-7358(00)00057-x. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Batten SV, Follette VM, Aban IB. Experiential avoidance and high-risk sexual behavior in survivors of child sexual abuse. Journal of Child Sexual Abuse. 2001;10:101–20. doi: 10.1300/j070v10n02_06. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Ego depletion and self-regulation failure: a resource model of self-control. Alcoholism: Clinical & Experimental Research. 2003;27:281–4. doi: 10.1097/01.ALC.0000060879.61384.A4. [DOI] [PubMed] [Google Scholar]
- Beck JG, Gudmundsdottir B, Palyo SA, Miller LM, Grant DM. Rebound effects following deliberate thought suppression: Does PTSD make a difference? Behavior Therapy. 2006;37:170–180. doi: 10.1016/j.beth.2005.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergquist KL, Fox HC, Sinha R. Self-reports of interoceptive responses during stress and drug cue-related experiences in cocaine- and alcohol-dependent individuals. Experimental and Clinical Psychopharmacology. 2010;18:229–37. doi: 10.1037/a0019451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Marlatt GA. The role of thought suppression in the relationship between mindfulness meditation and substance use. Addictive Behaviors. 2007;32:2324–2328. doi: 10.1016/j.addbeh.2007.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94:327–40. [PubMed] [Google Scholar]
- Coffey K, Hartman M. Mechanisms of action in the inverse relationship between mindfulness and psychological distress. Complementary Health Practice Review. 2008;13 [Google Scholar]
- Cox WM, Hogan LM, Kristian MR, Race JH. Alcohol attentional bias as a predictor of alcohol abusers’ treatment outcome. Drug and Alcohol Dependence. 2002;68:237–43. doi: 10.1016/s0376-8716(02)00219-3. [DOI] [PubMed] [Google Scholar]
- Dunmore E, Clark DM, Ehlers A. A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy. 2001;39:1063–1084. doi: 10.1016/s0005-7967(00)00088-7. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Hackmann A, Steil R, Clohessy S, Wenninger K, Winter H. The nature of intrusive memories after trauma: The warning signal hypothesis. Behaviour Research and Therapy. 2002;40:995–1002. doi: 10.1016/s0005-7967(01)00077-8. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Mayou RA, Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology. 1998;107:508. doi: 10.1037//0021-843x.107.3.508. [DOI] [PubMed] [Google Scholar]
- Elzinga BM, Bremner JD. Are the neural substrates of memory the final common pathway in posttraumatic stress disorder (PTSD)? Journal of Affective Disorders. 2002;70:1–17. doi: 10.1016/s0165-0327(01)00351-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DR, Segerstrom SC. Why do mindful people worry less? Cognitive Therapy and Research. 2011;35:497–504. [Google Scholar]
- Field M, Cox WM. Attentional bias in addictive behaviors: a review of its development, causes, and consequences. Drug and Alcohol Dependence. 2008;97:1–20. doi: 10.1016/j.drugalcdep.2008.03.030. [DOI] [PubMed] [Google Scholar]
- Flannery BA, Roberts AJ, Cooney N, Swift RM, Anton RF, Rohsenow DJ. The role of craving in alcohol use, dependence, and treatment. Alcoholism: Clinical and Experimental Research. 2001;25:299–308. [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20. [PubMed] [Google Scholar]
- Garland EL. Trait mindfulness predicts attentional and autonomic regulation of alcohol cue-reactivity. Journal of Psychophysiology. 2011;25:180–189. doi: 10.1027/0269-8803/a000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Howard MO. Targeting cognitive-affective risk mechanisms in stress-precipitated alcohol dependence: An integrated, biopsychosocial model of allostasis, automaticity, and addiction. Medical Hypotheses. 2011;76:745–754. doi: 10.1016/j.mehy.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Gaylord SA, West Channon V, Howard MO. Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol dependent adults. Cognitive Therapy and Research. doi: 10.1007/s10608-011-9378-7. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Carter K, Ropes K, Howard MO. Thought suppression, impaired regulation of urges, and Addiction-Stroop predict affect-modulated cue-reactivity among alcohol dependent adults. Biological Psychology. 2012;89:87–93. doi: 10.1016/j.biopsycho.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: Results from a randomized controlled pilot trial. Journal of Psychoactive Drugs. 2010;42:177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Fredrickson BL, Kring AM, Johnson DP, Meyer PS, Penn DL. Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review. 2010;30:849–864. doi: 10.1016/j.cpr.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg MA. Cognitive processing of traumas: The role of intrusive thoughts and reappraisals. Journal of Applied Social Psychology. 1995;25:1262–1296. [Google Scholar]
- Harrington T, Newman E. The psychometric utility of two self-report measures of PTSD among women substance users. Addictive Behaviors. 2007;32:2788–2798. doi: 10.1016/j.addbeh.2007.04.016. [DOI] [PubMed] [Google Scholar]
- Holmes EA, Grey N, Young KA. Intrusive images and “hotspots” of trauma memories in Posttraumatic Stress Disorder: an exploratory investigation of emotions and cognitive themes. Journal of Behavior Therapy and Experimental Psychiatry. 2005;36:3–17. doi: 10.1016/j.jbtep.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Klein AA. Suppression-induced hyperaccessibility of thoughts in abstinent alcoholics: a preliminary investigation. Behavior Research and Therapy. 2007;45:169–77. doi: 10.1016/j.brat.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford Press; NY: 1998. [Google Scholar]
- Langer EJ. Matters of mind: Mindfulness/mindlessness in perspective. Consciousness and Cognition. 1992;1:289–305. [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- Leeis M, Pagura J, Sareen J, Bolton JM. The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depression and Anxiety. 2010;27:731–736. doi: 10.1002/da.20677. [DOI] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL. Replication and extension of Marlatt’s taxonomy of relapse precipitants: overview of procedures and results. Addiction. 1996;91:51–72. [PubMed] [Google Scholar]
- Ludwig AM, Wikler A. “Craving” and relapse to drink. Quarterly Journal of Studies on Alcohol. 1974;35:108–30. [PubMed] [Google Scholar]
- MacLeod C, Mathews A, Tata P. Attentional biases in emotional disorders. Journal of Abnormal Psychology. 1986;95:15–20. doi: 10.1037//0021-843x.95.1.15. [DOI] [PubMed] [Google Scholar]
- Mayou RA, Ehlers A, Bryant B. Posttraumatic stress disorder after motor vehicle accidents: 3-year follow-up of a prospective longitudinal study. Behavior Research and Therapy. 2002;40:665–675. doi: 10.1016/s0005-7967(01)00069-9. [DOI] [PubMed] [Google Scholar]
- Merikle EP. The subjective experience of craving: an exploratory analysis. Substance Use & Misuse. 1999;34:1101–1115. doi: 10.3109/10826089909039399. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of Mental Health and Well-Being. American Journal of Psychiatry. 2006;163:652. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychological Bulletin. 2000;126:247–59. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Cain N, Nehmy T, Seymour M. The influence of thought suppression and cognitive load on intrusions and memory processes following an analogue stressor. Behavior Therapy. 2009;40:368–379. doi: 10.1016/j.beth.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Norris FH. Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60:409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Palfai TP, Monti PM, Colby SM, Rohsenow DJ. Effects of suppressing the urge to drink on the accessibility of alcohol outcome expectancies. Behaviour Research and Therapy. 1997;35:59–65. doi: 10.1016/s0005-7967(96)00079-4. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Kessler RC, Storz S, Wittchen H. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica. 2000;101:46–59. doi: 10.1034/j.1600-0447.2000.101001046.x. others. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Follette VM. Long-term correlates of child sexual abuse: Theory and review of the empirical literature. Applied & Preventive Psychology. 1995;4:143–166. [Google Scholar]
- Poulos CX, Hinson RE, Siegel S. The role of Pavlovian processes in drug tolerance and dependence: Implications for treatment. Addictive Behaviors. 1981;6:205–211. doi: 10.1016/0306-4603(81)90018-6. [DOI] [PubMed] [Google Scholar]
- Pu J, Schmeichel BJ, Demaree HA. Cardiac vagal control predicts spontaneous regulation of negative emotional expression and subsequent cognitive performance. Biological Psychology. 2010;84:531–540. [Google Scholar]
- Rosenthal MZ, Rasmussen Hall MA, Palm KM, Batten SV, Follette VM. Chronic avoidance helps explain the relationship between severity of childhood sexual abuse and psychological distress in adulthood. Journal of Child Sexual Abuse. 2005;4:25–41. doi: 10.1300/J070v14n04_02. [DOI] [PubMed] [Google Scholar]
- Rosenthal MZ, Cheavens JS, Lynch TR, Follette V. Thought suppression mediates the relationship between negative mood at PTSD in sexually assaulted women. Journal of Traumatic Stress. 2006;19:741–745. doi: 10.1002/jts.20162. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Supplement 20):22–33. [PubMed] [Google Scholar]
- Skinner MD, Aubin H-J. Craving’s place in addiction theory: Contributions of the major models. Neuroscience & Biobehavioral Reviews. 2010;34:606–623. doi: 10.1016/j.neubiorev.2009.11.024. [DOI] [PubMed] [Google Scholar]
- Stewart J, De Wit H, Eikelboom R. Role of unconditioned and conditioned drug effects in the self-administration of opiates and stimulants. Psychological Review. 1984;91:251. [PubMed] [Google Scholar]
- Thompson BL, Waltz J. Mindfulness and experiential avoidance as predictors of posttraumatic stress disorder avoidance symptom severity. Journal of Anxiety Disorders. 2010;24:409–415. doi: 10.1016/j.janxdis.2010.02.005. [DOI] [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychological Review. 1990;97:147–68. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tull MT, Gratz KL, Salters K, Roemer L. The role of experiential avoidance in posttraumatic stress symptoms and symptoms of depression, anxiety, and somatization. The Journal of Nervous and Mental Disease. 2004;192:754. doi: 10.1097/01.nmd.0000144694.30121.89. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Marlatt GA. Posttraumatic stress and alcohol use coping motives among a trauma-exposed community sample: The mediating role of non-judgmental acceptance. Addictive Behaviors. 2011;36:707–712. doi: 10.1016/j.addbeh.2011.01.033. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility; Annual meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993; others. [Google Scholar]
- Wegner DM. Ironic processes of mental control. Psychological Review. 1994;101:34–52. doi: 10.1037/0033-295x.101.1.34. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Erber R. The hyperaccessibility of suppressed thoughts. Journal of Personality and Social Psychology. 1992;63:903. [Google Scholar]
- Wegner DM, Zanakos S. Chronic thought suppression. Journal of Personality. 1994;62:616–40. doi: 10.1111/j.1467-6494.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, White TL. Paradoxical effects of thought suppression. Journal of Personality and Social Psychology. 1987;53:5–13. doi: 10.1037//0022-3514.53.1.5. [DOI] [PubMed] [Google Scholar]
- Wenzlaff RM, Wegner DM. Thought suppression. Annual Review of Psychology. 2000;51:59–91. doi: 10.1146/annurev.psych.51.1.59. [DOI] [PubMed] [Google Scholar]
- Williams JM, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychological Bulletin. 1996;120:3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving and substance use following a randomized trial of Mindfulness-Based Relapse Prevention. Journal of Consulting and Clinical Psychology. 2010;78:362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]