Abstract
An 83-year-old woman was referred to our emergency department with acute urticaria and sudden shortness of breath approximately 30 min after taking rectal diclofenac potassium for lumbago. After treatment with adrenaline and corticosteroids, the patient became hemodynamically stable and left the hospital on the next day. She attended our hospital 1 week after the onset of anaphylaxis because of repeated postprandial epigastric pain. No abnormal lesions were found in endoscopy. Radiographic selective catheter angiography revealed chronic mesenteric ischemia caused by atherosclerosis and abundant collateral arteries between the celiac trunk, the superior mesenteric artery and the inferior mesenteric artery. Patients with chronic mesenteric ischemia usually present with a clinical syndrome characterized by painful abdominal cramps and colic occurring typically during the postprandial phase. Fear of eating resulted in malnutrition. She was prescribed proton pump inhibitor, digestants, anticholinergic agents, serine protease inhibitors, prokinetics, antiplatelet agents and transdermal nitroglycerin intermittently, but these had no beneficial effects. It was most probable that this patient with chronic atherosclerotic mesenteric ischemia was suffering from functional abdominal pain syndrome induced by anaphylaxis. Since psychiatric disorders were associated with alterations in the processing of visceral sensation, we facilitated the patient's understanding of functional abdominal pain syndrome with the psychologist. Postprandial abdominal pain gradually faded after administration of these drugs and the patient left the hospital. Developing a satisfactory patient-physician relationship was considered more effective for the management of persistent abdominal pain caused by complicated mechanisms.
Key Words: Atherosclerosis, Mesenteric ischemia, Anaphylaxis, Functional abdominal pain syndrome, Patient-physician relationship
Introduction
Anaphylaxis is a severe acute allergic reaction, which can involve multiple organs and even pose an immediate threat to life. Epidemiological studies indicate that the prevalence of organ-specific allergic disorders such as allergic rhinitis, asthma and eczema has increased in recent decades in many western countries [1]. Anaphylaxis typically involves the cutaneous, respiratory and cardiovascular systems, presenting with urticaria, dyspnea, wheeze and hypotension. Involvement of the skin is reported in 80–90% of episodes, the respiratory tract in up to 70%, the gastrointestinal tract in up to 45%, the cardiovascular system in up to 45% and the central nervous system in up to 15% [2]. Although gastrointestinal symptoms, including nausea, vomiting, diarrhea and abdominal pain, sometimes occur transiently in some patients with anaphylaxis, persistent abdominal pain is rarely detected. Its prevalence is estimated at 0.05–2%, and the rate of occurrence appears to be increasing, mainly in young people [2]. Hospital-based studies suggest a death rate in the order of 1 per 100–200 episodes of anaphylaxis treated in an emergency department [3]. Death may occur from hypoxemia due to upper airway angioedema, bronchospasm and mucus plugging and/or shock due to massive vasodilation, fluid shift into the extravascular space and depressed myocardial function. Factors associated with increased risk of anaphylaxis include intercurrent infection, concomitant medication/foods (particularly α-blockers, β-blockers, angiotensin-converting enzyme inhibitors, nonsteroidal antiinflammatory drugs, alcohol or spicy food), high ambient temperatures and exercise.
Regardless of mechanism, the severity and mortality of anaphylaxis are affected by age, concomitant diseases (e.g. asthma, cardiovascular disorders or mastocytosis) and concurrent medication. Atherosclerosis is considered one of the risk factors for both cardiovascular events and mesenteric ischemia when anaphylaxis occurs. In general, although chronic atherosclerotic mesenteric ischemia is characterized by frequently unrecognized unspecific symptoms and even though significant degrees of splanchnic artery stenosis usually remain asymptomatic for many years [4], allergic reactions may cause abdominal symptoms through vasospasms of the splanchnic artery or embolism. Allergic reactions can lead to bowel ischemia as a result of arterial contraction in patients with atherosclerosis because the intestine receives 10–20% of the cardiac output when fasting and up to 35% after a meal. The hemodynamic explanation is a vascular steal from the intestine to the gastric circulation stimulated by food placed in the stomach. However, cases with bowel ischemia related to anaphylaxis have been rarely reported. We experienced an elderly case with chronic atherosclerotic mesenteric ischemia who started to develop the symptoms just after anaphylaxis although the association between anaphylaxis and chronic atherosclerotic mesenteric ischemia has been unclear.
Case Report
An 83-year-old woman who had a past history of abdominal migraine in adolescence was referred to our emergency department with acute urticaria and sudden shortness of breath approximately 30 min after taking rectal diclofenac potassium for lumbago. Severe hypotension (70/46 mm Hg) and an arterial oxygen saturation of 80% were observed upon arrival at the emergency room. After being given 0.3 mg of subcutaneous adrenaline and 500 mg of intravenous corticosteroids, the patient became hemodynamically stable and left the hospital on the next day.
After a few days’ development of anaphylaxis, the patient experienced epigastric pain especially after meals. The patient attended our hospital 1 week after the onset of anaphylaxis because of repeated epigastric pain. The pain was located in the epigastric area, starting 30 min after meals and lasting 60–120 min. She had no change in bowel habits, nausea, diarrhea or fever. Typically, the patient had 1–2 formal stools per day. The patient's medical history included hypertension, hyperlipidemia, bronchial asthma and osteoporosis. Her medication included amlodipine besilate, olmesartan medoxomil, magnesium oxide, pravastatin sodium, lansoprazole, inhaled tiotropium bromide hydrate and inhaled betamethasone/D-chlorpheniramine maleate. Because of postprandial abdominal pain, fear of eating led to a 6 kg weight loss in the 2 months after anaphylaxis. The patient was hospitalized again for further examination and treatment for repeated postprandial abdominal pain.
Physical examination was unremarkable. Blood pressure was 130/62 mm Hg in both arms and heart rate was 80/min. Temperature was 36.6°C. Head and neck examination was normal. There were no crackles, wheezes or murmur. On abdominal examination she had slight tenderness around the umbilicus with no audible bruit, masses or hepatosplenomegaly. Initial laboratory investigations (table 1) revealed normal values for complete and differential blood counts, erythrocyte sedimentation rate, serum albumin, liver enzymes and urinalysis. A serum inflammation marker, CRP, was not increased and all tumor markers measured were also normal. Lipid profile showed increased total cholesterol and triglyceride and normal HDL cholesterol levels (315, 151 and 65 mg/dl, respectively). Blood urea nitrogen and creatinine levels were elevated, indication the presence of chronic kidney disease. Both serum total and pancreatic amylase levels were also slightly increased. Fecal cytology revealed lots of red-orange-colored droplets which indicated that the feces contained inadequately absorbed lipid that was steatorrhea. The blood levels of D-dimer, FDP and fibrinogen were elevated at 2.1, 3.8 and 332 mg/dl, respectively.
Table 1.
Blood examination on admission
| Blood count | |
| White blood cells | 52,000/μl |
|
64% |
|
26% |
|
8.8% |
|
1.0% |
|
0.2% |
| Red blood cells | 368 × 104/μl |
| Hce:italicoglobin | 11.9 g/dl |
| Platelets | 22.9 × 104/μl |
| Blood clotting | |
| PT | 132% |
| APTT | 19.9 s (control 30 s) |
| Fibrinogen | 332 mg/dl |
| FDP | 3.8 μg/ml |
| D-dimer | 2.1 μg/ml |
| Blood chemistry | |
| Total protein | 7.3 g/dl |
| Albumin | 4.4 g/dl |
| AST | 20 IU/l |
| ALT | 16 IU/l |
| ALP | 183 IU/l |
| LDH | 231 IU/l |
| Urea nitrogen | 30 mg/dl |
| Creatinine | 1.35 mg/dl |
| Sodium | 137 mEq/l |
| Potassium | 5.0 mEq/l |
| Chloride | 103 mEq/l |
| Glucose | 95 mg/dl |
| CRP | 0.03 mg/dl |
| Stool examination | |
| Occult blood test | – |
| Triboulet reaction | + |
| Steatorrhea | + |
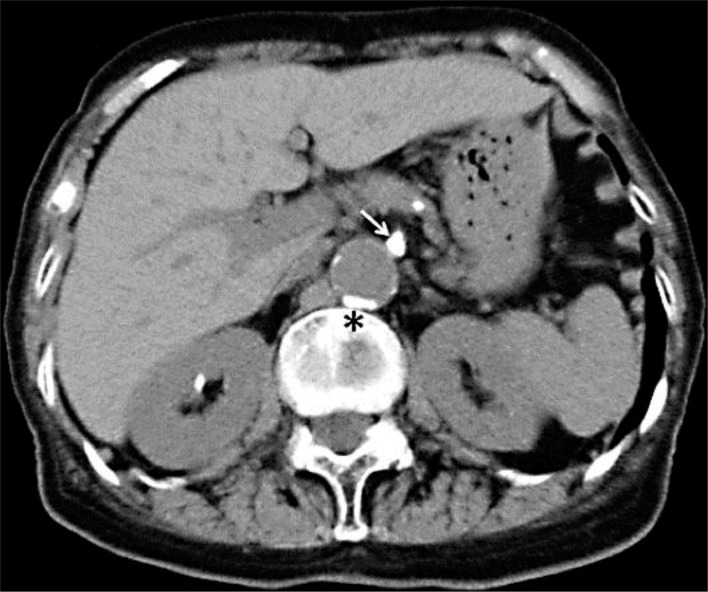
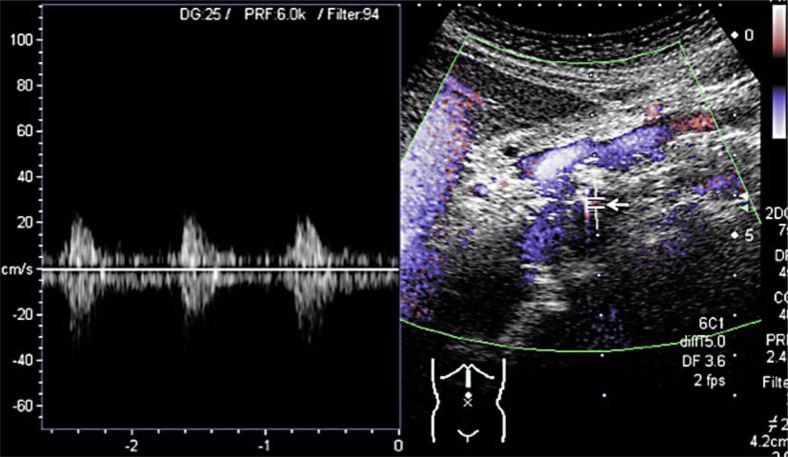
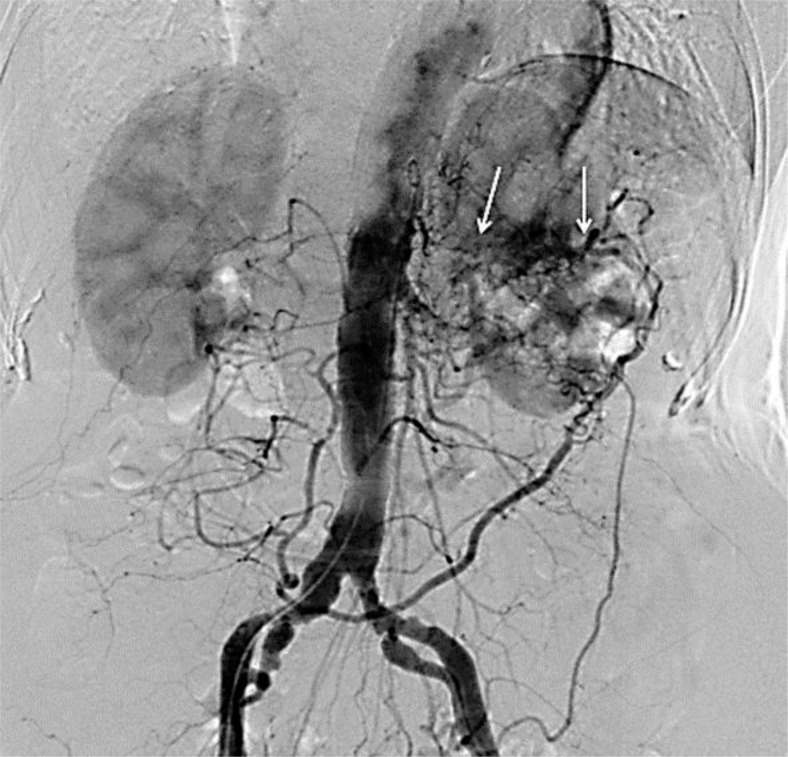
No abnormal lesions were found in esophagogastroscopy, capsule endoscopy or colonoscopy. All findings of abdominal computed tomography except atherosclerosis were also almost normal (fig. 1). Abdominal ultrasonography was unable to measure the velocity of the celiac artery due to calcification of the arterial wall (fig. 2). No other vascular abnormalities were seen on ultrasonography. Radiographic selective catheter angiography revealed chronic mesenteric ischemia caused by atherosclerosis and abundant collateral arteries between the celiac trunk, the superior mesenteric artery and the inferior mesenteric artery (fig. 3).
Fig. 1.
Abdominal computed tomography scan showed atherosclerosis in the celiac artery (arrow) and the descending aorta (asterisk).
Fig. 2.
Longitudinal ultrasonography of the celiac artery showed sclerosis of the arterial wall. The velocity of the celiac artery could not be measured due to calcification of the arterial wall (arrow).
Fig. 3.
Radiographic selective catheter angiography revealed chronic mesenteric ischemia caused by atherosclerosis and abundant collateral arteries (arrows) between the celiac trunk, the superior mesenteric artery and the inferior mesenteric artery.
The patient was prescribed proton pump inhibitor, digestants, anticholinergic agents and prokinetics intermittently, but these had no beneficial effects. Since steatorrhea was found by the results of fecal cytology and since blood tests showed elevated serum amylase levels suggesting potential exocrine pancreatic insufficiency, anticholinergic agents, serine protease inhibitors and pancrelipase were administered orally. However, postprandial abdominal pain did not improve even after starting these supplementations, or even under intravenous administration of scopolamine and/or hydroxyzine. Fear of eating resulted in malnutrition and temporally required central parenteral nutrition. Based on the finding of celiac atherosclerosis, the additional treatment with secondary preventive drugs including antiplatelet agents and transdermal nitroglycerin had no beneficial effects. It was most probable that this patient with chronic atherosclerotic mesenteric ischemia was suffering from functional abdominal pain syndrome induced by anaphylaxis.
Since psychiatric disorders were associated with alterations in the processing of visceral sensation in the patient, it was suggested that psychological treatment would be beneficial. Two weeks after admission, we facilitated the patient's understanding of functional abdominal pain syndrome with the psychologist and prescribed gabapentin and lorazepam. Postprandial abdominal pain gradually faded after administration of these drugs and the patient left the hospital.
Discussion
Acute mesenteric ischemia usually caused by embolism is characterized by a typical acute onset of diffuse abdominal pain, whereas chronic mesenteric ischemia is characterized by frequently unrecognized unspecific symptoms such as postprandial abdominal pain and unintended weight loss [4]. Patients with chronic mesenteric ischemia usually present with a clinical syndrome characterized by painful abdominal cramps and colic typically occurring during the postprandial phase [4]. Stenosis of visceral vessels, including the celiac artery, is usually well tolerated because of the abundant collateral circulation, leading to a potentially underdiagnosed condition. Radiographic selective catheter angiography revealed chronic mesenteric ischemia caused by atherosclerosis, and an elevated blood D-dimer level also suggested chronic mesenteric ischemia in our case. However, the onset of postprandial abdominal pain was clear and symptoms lasted for 2 months.
Unlike abdominal angina, it has been well known that hypersensitivity reactions associated with underlying coronary artery disease are not rare. Allergic angina syndrome was described in 1991 [5] as ‘the coincidental occurrence of chest pain and allergic reactions accompanied by clinical and laboratory findings of classic angina pectoris caused by inflammatory mediators released during the allergic insult’. There are currently two variants of Kounis syndrome: the first is observed in patients with no cardiovascular risk factors and with healthy coronary arteries in which the inflammatory cascade triggered by the allergic insult causes a coronary vasospasm, the second is observed in patients with pre-existing atheromatous diseases. The existence of mastocytes in heart tissue and their participation in the anaphylactic reaction that triggers tachycardia, coronary vasoconstriction, dysfunctional ventricular contractility and blockade of arterioventricular conduction is well known. The key elements of organ allergic reaction are mast cells located in the heart [6]. Mast cells occur in considerably higher amounts in the intima and adventitia of vessels with pre-existing atheromatic lesions, particularly in marginal regions of atherosclerotic plaques. In place of plaque rupture, about 200 times more mast cells are found compared with surrounding vascular segments without atheromatic changes in patients with nonallergic acute myocardial infarction [7]. The histamine concentration and the number of mast cells in the arterial wall increase proportionally with the extent of atherosclerosis. Peptidases released from stimulated mast cells activate metalloproteinases which degrade connective tissue covering the atheromatic plaque. Moreover, prostaglandin D2, leukotrienes and angiotensin II influence contracted coronary vessels [8]. Applying the pathophysiologic mechanisms of Kounis syndrome to chronic mesenteric ischemia to explain the involvement of the gastrointestinal tract in anaphylactic reactions, the onset of postprandial abdominal pain just after anaphylaxis could be understood.
Acute intestinal ischemia stimulates visceral afferent nerves, but the mechanisms responsible for this excitation are not fully understood. Mast cells may participate in this process as they are known to signal to mesenteric afferents during intestinal anaphylaxis [9]. Kreis et al. [10] also reported that histamine potentially acts as a mediator in mast cell to afferent nerve communication in the small intestine. Histamine has been shown to stimulate nociceptive afferent fibers in a variety of tissues such as skin, joints and muscle. The gastrointestinal tract contains mechanisms that enable differentiation between nutrients indispensable to the organism and antigenic substances that signify a potential threat. Hypersensitivity reactions give rise to intestinal sensory and motor events that are designed to dilute and eventually eliminate the antigen from the gut. If activated mast cells are present around nociceptive afferent fibers, persistent postprandial abdominal pain can occur for a long time like in the present case. Acute gastrointestinal mucosal lesions have been reported. Although severe hemorrhagic gastritis and acute ischemic colitis following anaphylaxis were reported [11], there was no evidence that the damage to the mucosa or gut was direct or induced by the immune reaction. Furthermore, administration of adrenaline to treat anaphylactic shock might induce abdominal angina because adrenaline is capable of causing ventricular fibrillation and severe vasocontraction [12]. The effect of adrenaline ingested was probably secondary to the initial reaction as a joint vasocontraction factor in the vasospasm triggered by anaphylaxis.
Celiac artery compression syndrome is also known to be a rare cause of postprandial abdominal pain and unintended weight loss. The anatomical abnormalities in which the median arcuate ligament and the origin of the celiac artery are in abnormally close proximity may result in damage to the celiac nerve plexus or partial obstruction of blood flow through the celiac artery due to compression of the celiac artery during respiration [13]. There was no evidence that the median arcuate ligament compressed the celiac artery in computed tomography or angiography in the present case.
The current literature recommends conservative treatment in patients with asymptomatic chronic atherosclerotic mesenteric ischemia [14]. Medical treatment includes all aspects of secondary preventive drug treatment including statins, antiplatelet therapy, blood pressure control, blood glucose control and smoking cessation. During the last decade, although endovascular revascularization has replaced surgical revascularization as the therapy of choice, the patient and her family selected conservative treatment. For lack of confident diagnosis of chronic atherosclerotic mesenteric ischemia, the patient was treated conservatively for functional abdominal pain syndrome with gabapentin and lorazepam. In contrast to irritable bowel syndrome, treatment recommendations are empirical. The accepted basis for clinical management of functional abdominal pain syndrome relies on establishing an effective patient-physician relationship for clinical management [15]. We facilitated the patient's understanding of functional abdominal pain syndrome with the psychologist because factors contributing to an effective patient-physician relationship include empathy toward the patient, patient education, validation of the illness, reassurance, treatment negotiation and establishment of reasonable limits in time and effort. Postprandial abdominal pain gradually faded after establishing an effective patient-physician relationship. The psychiatrist suggested that her psychiatric symptoms would be diagnosed additionally as having ‘mental disorders due to a medical condition’.
The present case had asymptomatic chronic atherosclerotic mesenteric ischemia and anaphylaxis that changed to symptomatic one. Repeated postprandial abdominal pain caused symptom-specific anxiety, resulting in the need of psychological treatment with anxiolytic agents. In conclusion, developing a satisfactory patient-physician relationship was considered more effective for the management of persistent abdominal pain caused by complicated mechanisms.
References
- 1.Gupta R, Sheikh A, Strachan DP, et al. Burden of allergic disease in the UK: secondary analyses of national databases. Clin Exp Allergy. 2004;34:520–526. doi: 10.1111/j.1365-2222.2004.1935.x. [DOI] [PubMed] [Google Scholar]
- 2.Simons FE. Anaphylaxis. J Allergy Clin Immunol. 2010;152:S161–S181. doi: 10.1016/j.jaci.2009.12.981. [DOI] [PubMed] [Google Scholar]
- 3.Brown SGA. Clinical features and severity grading of anaphylaxis. J Allergy Clin Immunol. 2004;114:371–376. doi: 10.1016/j.jaci.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 4.Sreenarasimhaiah J. Chronic mesenteric ischemia. Best Pract Res Clin Gastroenterol. 2005;19:283–295. doi: 10.1016/j.bpg.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 6.Laine P, Kaartinen M, Penttilä A, et al. Association between myocardial infarction and the mast cells in the adventitia of the infarct-related coronary artery. Circulation. 1999;99:361–369. doi: 10.1161/01.cir.99.3.361. [DOI] [PubMed] [Google Scholar]
- 7.Kalsner S, Richards R. Coronary arteries of cardiac patients are hyperreactive and contain stores of amines: a mechanism for coronary spasm. Science. 1984;223:1435–1437. doi: 10.1126/science.6701530. [DOI] [PubMed] [Google Scholar]
- 8.Sinkiewicz W, Soba?ski P, Bartuzi Z. Allergic myocardial infarction. Cardiol J. 2008;15:220–225. [PubMed] [Google Scholar]
- 9.Jiang W, Kirkup AJ, Grundy D. Mast cells drive mesenteric afferent signalling during acute intestinal ischaemia. J Physiol. 2011;589:3867–3882. doi: 10.1113/jphysiol.2011.209478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kreis ME, Haupt W, Kirkup AJ, et al. Histamine sensitivity of mesenteric afferent nerves in the rat jejunum. Am J Physiol. 1998;275:G675–G680. doi: 10.1152/ajpgi.1998.275.4.G675. [DOI] [PubMed] [Google Scholar]
- 11.Fock S, Mense S. Excitatory effects of 5-hydroxytryptamine, histamine and potassium ions on muscular group IV afferent units: a comparison with bradykinin. Brain Res. 1976;105:459–469. doi: 10.1016/0006-8993(76)90593-x. [DOI] [PubMed] [Google Scholar]
- 12.Mueller UR. Cardiovascular disease and anaphylaxis. Curr Opin Allergy Clin Immunol. 2007;7:337–341. doi: 10.1097/ACI.0b013e328259c328. [DOI] [PubMed] [Google Scholar]
- 13.van Noord D, Kuipers EJ, Mensink PB. Single vessel abdominal arterial disease. Best Pract Res Clin Gastroenterol. 2009;23:49–60. doi: 10.1016/j.bpg.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 14.Thomas JH, Blake K, Pierce GE, et al. The clinical course of asymptomatic mesenteric arterial stenosis. J Vasc Surg. 1998;27:840–844. doi: 10.1016/s0741-5214(98)70263-0. [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA. Functional abdominal pain syndrome. Clin Gastroenterol Hepatol. 2004;2:353–365. doi: 10.1016/s1542-3565(04)00118-1. [DOI] [PubMed] [Google Scholar]