Abstract
Probe-based confocal laser endomicroscopy (pCLE) is a novel imaging technique which utilizes a low-power laser light passed through a fiber-optic bundle, within a miniprobe that is advanced into the working channel, to obtain microscopic images of the mucosa. This allows the endoscopist to evaluate the microarchitecture of the gastrointestinal epithelium in real time. At this time pCLE cannot replace histopathology, but it can provide diagnostic information as well as guide therapeutic management in patients with Barrett's esophagus (BE) with high-grade dysplasia (HGD). We describe a retrospective case series in which four patients with BE and biopsy-proven HGD underwent endoscopy with pCLE to direct real-time endoscopic ablation therapy and/or endoscopic mucosal resection (EMR), which was performed in conjunction with pCLE. All four patients had pCLE showing features of HGD. After either EMR or radiofrequency ablation (RFA), pCLE was again used to evaluate the margins after therapy to assure accuracy. In one case, pCLE had features of dysplasia at the margin and further repeat EMR was immediately performed. Another case had a normal-appearing esophagus, but pCLE found features of BE in discrete areas and targeted biopsies were performed, which confirmed BE. This patient subsequently underwent RFA therapy of the residual areas of BE. In conclusion, in patients with BE and dysplasia, pCLE is an effective tool used to target biopsies, guide endoscopic therapy and assess the accuracy of EMR or RFA.
Key Words: Barrett's esophagus, Probe-based confocal laser, Endomicroscopy, High-grade dysplasia, Low-grade dysplasia
Introduction
Confocal laser endomicroscopy (CLE) is a novel imaging technique which utilizes a low-power laser light passed through a fiber-optic bundle to obtain microscopic images of the mucosa. This allows the endoscopist to evaluate the microarchitecture of the epithelium and lamina propria in real time and can provide in vivo, real-time diagnostic information and also guide therapeutic management. To obtain these high-contrast images, CLE requires contrast injection prior to imaging with an agent such as fluorescein, which has been shown to be safe in several studies [1, 2, 3]. There are currently two devices for CLE, one in which the laser is integrated into the distal tip of an upper endoscope or colonoscope and allows full use of the working channel at the same time (developed by Pentax, Tokyo, Japan). The second system, called probe-based confocal laser endomicroscopy (pCLE; Cellvizio, Mauna Kea Technologies, Paris, France) utilizes a confocal miniprobe which is passed down the working channel of a conventional endoscope, including the side viewing endoscope [4]. In other works, pCLE has been used to distinguish between hyperplastic, adenomatous and neoplastic colon polyps, and to evaluate early gastric cancers, celiac sprue, pancreatic neoplasms, biliary diseases and Barrett's esophagus (BE) [5, 6, 7, 8, 9, 10].
BE is defined as metaplasia of the esophageal epithelium with replacement of the normal squamous epithelium by columnar epithelium containing goblet cells. These changes are also referred to as intestinal metaplasia [11]. BE is associated with an increased risk of developing esophageal adenocarcinoma, the incidence of which has increased dramatically over the past several decades [12, 13, 14, 15, 16]. Once diagnosed, esophageal adenocarcinoma has a poor prognosis with a less than a 25% five-year survival after a diagnosis of locally advanced disease [17]. BE can range from having no histologic evidence of cellular atypia (nondysplastic metaplasia) to low-grade dysplasia (LGD) on through to high-grade dysplasia (HGD). The efficacy of Barrett's surveillance to detect early neoplasia is controversial and the optimal care of patients with dysplastic BE is unclear, but improvement in surveillance techniques may improve sensitivity and also guide endoscopic management of these neoplastic lesions. There have been several recent developments in endoscopic therapy of LGD, HGD and intramucosal carcinoma using combined techniques of endoscopic mucosal resection (EMR) and endoscopic ablation therapies such as radiofrequency ablation (RFA). More recently, an international prospective randomized controlled trial by Sharma et al. [18] concluded that pCLE combined with high-definition white light examination (HD-WLE) significantly improved the ability to detect neoplasia in BE patients compared with HD-WLE alone. The authors suggested that this finding may allow better informed decisions to be made for the management and subsequent treatment of BE patients. In this article, we describe a retrospective case series in which four patients (table 1) with BE and biopsy-proven HGD underwent endoscopy with pCLE to direct real-time endoscopic ablation therapy and/or EMR, which was performed in conjunction with real-time pCLE.
Table 1.
Baseline patient characteristics
| Case | Age | Gender | Length of Barrett's | Prior dysplasia (per biopsy) | Prior endoscopic treatment |
|---|---|---|---|---|---|
| 1 | 71 | M | 4 cm, circumferential | HGD | prior EMR |
| 2 | 66 | M | 3 cm, circumferential, few short tongues | HGD | prior EMR |
| 3 | 80 | F | 10 cm, circumferential but noncontiguous | LGD and HGD | prior RFA and EMR |
| 4 | 67 | M | 6 cm (distal 4 cm circumferential, two 2 cm tongues extending proximally) | LGD and HGD | prior RFA and EMR |
M = Male; F = female.
Patients and Methods
All endoscopies and pCLE were performed under general anesthesia by one experienced gastroenterologist (D.V.G.). A standard upper endoscopy (esophagogastroduodenoscopy) was first performed in all cases with WLE using a high-definition diagnostic upper endoscope (EG2990i HD; Pentax of America, Montvale, N.J., USA). pCLE was then performed after intravenous injection of 2.5 ml of 10% fluorescein. A GastroFlex UHD Confocal MiniprobeTM (Cellvizio, Mauna Kea Technologies) was inserted through the working channel of the endoscope and the probe was positioned on the margins of the previously resected area to examine for areas of intestinal metaplasia, dysplasia, and early cancer.
The examiner was trained on the CLE criteria for assessment of BE, dysplasia, and esophageal neoplasm. During the procedure, foci were characterized by pCLE as having normal squamous epithelium, Barrett's metaplasia, or dysplasia. Normal esophageal mucosa has stacked layers of squamous epithelium, while Barrett's metaplasia appears as organized columnar epithelium with a regular vascular pattern, normal villous gland architecture, and with dark, hypodense round structures representing goblet cells. LGD, HGD and neoplasm are a continuum characterized by progressively increasing cellular disorganization, variable cell height/thickness, disruption of normal villous gland pattern and fusion of glands.
Results
Case 1
A 71-year-old male patient was referred with a 4 cm segment of BE with biopsy-proven LGD demonstrated 1 year earlier. A repeat 6 month surveillance endoscopy confirmed the diagnosis of BE with LGD. Subsequent follow-up endoscopy revealed two noncontiguous sub-centimeter regions of nodularity within the Barrett's segment. The nodularity was addressed with EMR via the Wilson-Cook Duette band ligation and snare system (Duette multiband mucosectomy, Cook Medical, Winston Salem, N.C., USA); three resections were performed. Pathology demonstrated HGD extending to the margins of the resected specimen. After careful discussion, the patient decided to proceed with endoscopic treatment. A repeat endoscopy again demonstrated a single sub-centimeter region of nodularity within the BE segment (fig. 1a). pCLE was then performed on the distal esophagus. The esophageal nodularity was evaluated by positioning the tip of the confocal miniprobe on the suspicious lesion and corresponding images demonstrated dysplasia embedded within intestinal metaplasia. EMR of the mucosal nodularity was performed. pCLE was again employed along the resection margins. Inspection demonstrated irregular glands and cellular disorganization consistent with dysplasia (fig. 1b). As further dysplasia was identified and there were concerns for residual mucosal nodularity at the margin, further EMR overlapping adjacent to the original dysplastic resection margin was performed, and follow-up pathology confirmed HGD (fig. 1c). pCLE was again used to evaluate the margins of the resection and demonstrated intestinal metaplasia without residual dysplasia. Endoscopically, there appeared to be complete mucosal resection of the nodular area. Following EMR, during the same endoscopic session HALO-90TM (Halo 360 and Halo 90, BARRX, Sunnyvale, Calif., USA) RFA was performed on the remaining Barrett's segment. After the ablation therapy was performed, pCLE was simultaneously employed in the esophagus alongside the HALO-90 RFA catheter confirming eradication of the Barrett's metaplasia in the treatment zones (fig. 1d). Of note, this technique was used to aid in the positioning of the HALO-RFA and to assess the efficacy of endoscopic therapy, but pCLE images were not acquired during active ablation therapy.
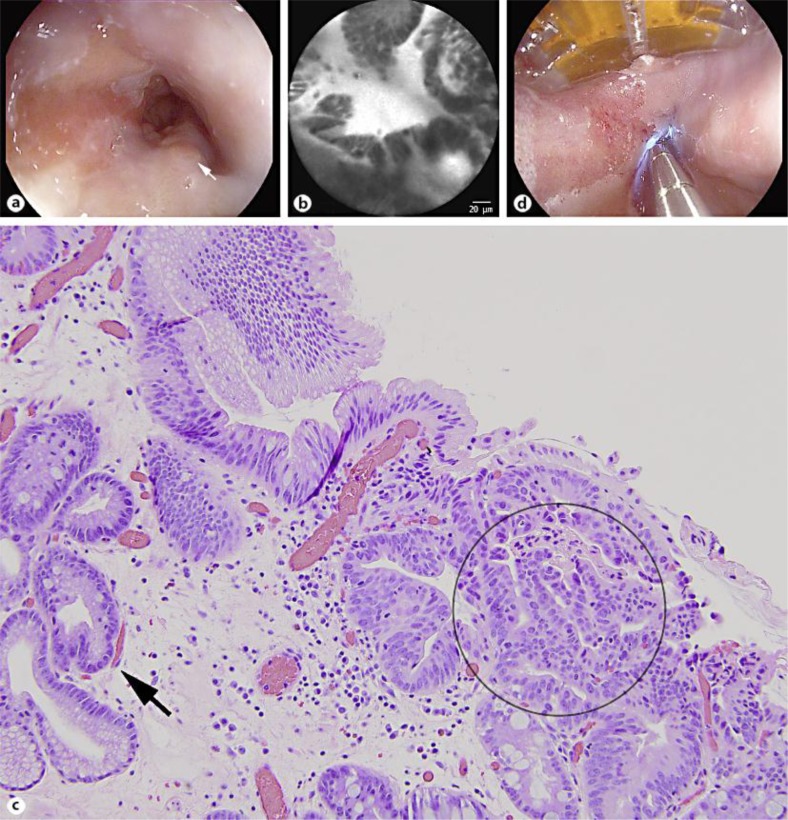
Fig. 1.
a Segment of BE with one region of nodularity (arrow). b Endomicroscopy image after EMR showing gland irregularity and cellular disorganization, representing residual dysplasia present at the resection margin. c Histology showing features of HGD including back-to-back glands, piled up nuclei, and loss of polarity (circle). The arrow shows BE without dysplasia. Magnification: ×20. d pCLE probe being used alongside the HALO-90 catheter to confirm eradication of dysplasia at margins after ablative therapy.
Case 2
A 66-year-old male veteran with a 3 cm segment of BE presented with biopsy-proven HGD. Medical comorbidities were felt to preclude esophagectomy. A surveillance examination demonstrated a 1 cm segment of nodular Barrett's mucosa. The nodule was removed via EMR again using the Wilson-Cook Duette system. Pathology confirmed HGD. Based on the size of the defect, RFA on the remaining Barrett's tissue was deferred. On subsequent examination, there was new nodularity appreciated at the gastroesophageal junction embedded within a Barrett's field. EMR was performed in a near circumferential manner around the gastroesophageal junction; four resections were performed. Pathology later confirmed HGD. RFA was again deferred based on the extent of resection. On a subsequent examination, no further nodularity was identified. pCLE was performed, revealing evidence of dysplasia within a larger contiguous 3 cm segment of intestinal metaplasia. RFA was performed on the Barrett's segment. Again, as in the first case, post treatment pCLE was performed with the probe placed along the HALO-90 RFA catheter, which demonstrated successful ablation therapy with no further remaining zones of residual dysplasia or Barrett's metaplasia. A 2-month surveillance endoscopic examination revealed significant regression of the Barrett's segment. However, there was a new contiguous 1-cm region of nodular Barrett's mucosa in the distal esophagus. pCLE demonstrated evidence of dysplasia within the nodular segment. Adjacent mucosa demonstrated changes consistent with intestinal metaplasia. EMR was performed on the nodular segment in a semi-circumferential manner; three resections were performed. Repeat pCLE demonstrated no evidence of residual dysplasia at the resection margins.
Case 3
An 80-year-old woman with a history of long-segment BE (11 cm) with biopsy-proven multifocal HGD was referred to our institution for therapy. The patient had significant medical comorbidities including coronary artery disease, atrial fibrillation and cerebrovascular/peripheral vascular disease. She declined esophagectomy. In the prior year, she underwent HALO-360 RFA amidst three independent EMR treatments for nodular Barrett's with biopsy-proven HGD. pCLE was applied to the nodular mucosa, demonstrating evidence of HGD prior to EMR. A subsequent endoscopic evaluation demonstrated persistent, 5-cm-long segment BE without nodularity with earlier biopsies confirming regression to LGD. pCLE was performed on the Barrett's mucosa, demonstrating areas of intestinal metaplasia with features of dysplasia. HALO-360 RFA was applied to the entire 11 cm Barrett's segment. After HALO-360 ablation treatment was performed, the pCLE probe was introduced alongside and proximal to the HALO-360 balloon probe and the margin without evidence of intestinal metaplasia at the proximal ablation margins and cautery artifact consistent with treatment at the ablation zone. Again, it should be made clear that pCLE images were not obtained during active therapy. A 2-month follow-up protocol endoscopy demonstrated endoscopic regression of Barrett's with only residual islands seen, consistent with biopsy-proven intestinal metaplasia without dysplasia.
Case 4
A 67-year-old man presented with a longstanding history of endoscopically treated long-segment BE with biopsy-proven LGD and a focus of HGD. Surveillance biopsies following HALO-360 RFA demonstrated a focus of LGD in a residual region of Barrett's metaplasia at the distal esophagus. pCLE was performed, demonstrating features of dysplasia at the Barrett's segment. EMR was performed during the same endoscopic session using the Wilson-Cook Duette system; two resections were performed. Pathology confirmed a focus of HGD with surrounding LGD confined to the EMR nodular specimen without involvement of the resection margins. pCLE performed post EMR demonstrated only features of intestinal metaplasia without dysplasia. Again during the same endoscopic session, HALO-90 RFA was performed on residual islands of Barrett's mucosa in the distal esophagus, and real-time pCLE performed just after ablation therapy, with the probe based along the HALO-90 RFA catheter, did not demonstrate residual metaplasia or dysplasia. A subsequent surveillance examination 3 months later showed significant endoscopic regression with an irregular Z line, but without visual evidence of continuous BE. Few scattered islands were noted and pCLE was performed, demonstrating evidence of intestinal metaplasia without dysplasia. Target biopsies were performed and follow-up HALO-90 RFA was applied to treat residual metaplasia. Biopsy results confirmed intestinal metaplasia with no residual dysplasia.
Discussion
The role of BE surveillance and treatment of dysplasia in the setting of BE are still being debated, however mounting evidence shows that endoscopic therapy is a viable, and perhaps preferable, alternative to both surgery and surveillance in patients with HGD or early carcinoma [19, 20, 21]. This retrospective case series provides evidence that the ability of the endoscopists to identify dysplasia in real time using pCLE technology allows them to target dysplastic areas for therapeutic treatment, to locate residual posttherapeutic areas for re-treatment, and then to confirm that ablated/resected areas and margins are free of residual intestinal metaplasia or dysplasia.
Several studies have shown pCLE to be an important up-and-coming technology in the surveillance of BE and identification of dysplasia and early cancer. It is important to note that pCLE does not eliminate the need for biopsies, but it does allow for more targeted biopsies, potentially leading to a better disease characterization, fewer biopsies and more cost-effective surveillance [9, 22, 23]. Konda et al. [8] showed that pCLE can be used in real time to provide the endoscopist with additional information to aid with targeting EMR and to assess accuracy of EMR.
We present a case series describing pCLE being used in conjunction with the HALO apparatus to target therapy and confirm successful mucosal resection and RFA of dysplastic lesions in BE. In each patient described above, the pCLE imaging was used prior to endoscopic therapy to identify areas of concern, guide targeted biopsies and target additional therapy to that area. pCLE was then used again after both EMR and HALO RFA to assess the accuracy and completeness of each therapy (table 2). Limitations to this study include the limited number of patients and that using pCLE after ablation is not well studied. Moreover, post therapy cauterization effect may make it difficult to distinguish whether mucosa is sufficiently ablated; thus, at this time pCLE cannot necessarily be used to predict the treatment effect of RFA.
Table 2.
Summary of results of pCLE findings and endoscopic therapy
| Case | WLE findings | pCLE before | Therapy | pCLE after | Pathology |
|---|---|---|---|---|---|
| 1 | <1 cm nodule in field of BE | dysplasia present | EMR and HALO-RFA | dysplasia present after first EMR | confirmed HGD, negative margins |
| 2 | Nodular mucosa in BE | dysplasia present | EMR with HALO-RFA | no dysplasia after EMR | BE with HGD |
| 3 | Nodular mucosa in BE | dysplasia present | EMR | no dysplasia at margins, BE present | BE with HGD |
| 4 | History of HGD and BE, but no endoscopic BE now | features of BE | biopsies of suspected BE | not performed | BE confirmed |
CLE is an emerging technology with a potential to aid the endoscopist in the diagnosis and treatment of several gastrointestinal maladies, including BE, but much research remains to be done. In patients with BE and dysplasia, pCLE is an effective tool used to target biopsies, obtain a comprehensive disease characterization, guide endoscopic therapy and assess the accuracy of EMR or RFA. This case series can serve as the impetus for a pilot study or other large, multicenter, prospective trials to establish the feasibility and technique of using real-time pCLE in conjunction with EMR and RFA during the same session in order to guide therapy of Barrett's with dysplasia.
Disclosure Statement
None of the authors have any conflicts of interest to disclose.
References
- 1.Paramsothy S, Leong RW. Endoscopy: fluorescein contrast in confocal laser endomicroscopy. Nat Rev Gastroenterol Hepatol. 2010;7:366–368. doi: 10.1038/nrgastro.2010.83. [DOI] [PubMed] [Google Scholar]
- 2.Wallace MB, Meining A, Canto MI, et al. The safety of intravenous fluorescein for confocal laser endomicroscopy in the gastrointestinal tract. Aliment Pharmacol Ther. 2010;31:548–552. doi: 10.1111/j.1365-2036.2009.04207.x. [DOI] [PubMed] [Google Scholar]
- 3.Becker V, van den Broek FJ, Buchner AM, et al. Optimal fluorescein dose for intravenous application in miniprobe-based confocal laser scanning microscopy in pigs. J Biophotonics. 2011;4:108–113. doi: 10.1002/jbio.201000028. [DOI] [PubMed] [Google Scholar]
- 4.Othman MO, Wallace MB. Confocal laser endomicroscopy: is it prime time? J Clin Gastroenterol. 2011;45:205–206. doi: 10.1097/MCG.0b013e31820776e6. [DOI] [PubMed] [Google Scholar]
- 5.Li WB, Zuo XL, Li CQ, et al. Diagnostic value of confocal laser endomicroscopy for gastric superficial cancerous lesions. Gut. 2011;60:299–306. doi: 10.1136/gut.2010.223586. [DOI] [PubMed] [Google Scholar]
- 6.Buchner AM, Shahid MW, Heckman MG, et al. Comparison of probe-based confocal laser endomicroscopy with virtual chromoendoscopy for classification of colon polyps. Gastroenterology. 2010;138:834–842. doi: 10.1053/j.gastro.2009.10.053. [DOI] [PubMed] [Google Scholar]
- 7.Zambelli A, Villanacci V, Buscarini E, et al. Confocal laser endomicroscopy in celiac disease: description of findings in two cases. Endoscopy. 2007;39:1018–1020. doi: 10.1055/s-2007-966783. [DOI] [PubMed] [Google Scholar]
- 8.Konda VJ, Chennat JS, Hart J, Waxman I. Confocal laser endomicroscopy: potential in the management of Barrett's esophagus. Dis Esophagus. 2010;23:E21–E31. doi: 10.1111/j.1442-2050.2010.01088.x. [DOI] [PubMed] [Google Scholar]
- 9.Pohl H, Rosch T, Vieth M, et al. Miniprobe confocal laser microscopy for the detection of invisible neoplasia in patients with Barrett's oesophagus. Gut. 2008;57:1648–1653. doi: 10.1136/gut.2008.157461. [DOI] [PubMed] [Google Scholar]
- 10.Meining A, Phillip V, Gaa J, et al. Pancreaticoscopy with miniprobe-based confocal laser-scanning microscopy of an intraductal papillary mucinous neoplasm (with video) Gastrointest Endosc. 2009;69:11 1178–1180. doi: 10.1016/j.gie.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Spechler SJ. Clinical practice. Barrett's esophagus. N Engl J Med. 2002;346:836–842. doi: 10.1056/NEJMcp012118. [DOI] [PubMed] [Google Scholar]
- 12.Brown LM, Devesa SS. Epidemiologic trends in esophageal and gastric cancer in the United States. Surg Oncol Clin N Am. 2002;11:235–256. doi: 10.1016/s1055-3207(02)00002-9. [DOI] [PubMed] [Google Scholar]
- 13.Drewitz DJ, Sampliner RE, Garewal HS. The incidence of adenocarcinoma in Barrett's esophagus: a prospective study of 170 patients followed 4.8 years. Am J Gastroenterol. 1997;92:212–215. [PubMed] [Google Scholar]
- 14.O'Connor JB, Falk GW, Richter JE. The incidence of adenocarcinoma and dysplasia in Barrett's esophagus: report on the Cleveland Clinic Barrett's Esophagus Registry. Am J Gastroenterol. 1999;94:16 2037–2042. doi: 10.1111/j.1572-0241.1999.01275.x. [DOI] [PubMed] [Google Scholar]
- 15.el-Serag HB. The epidemic of esophageal adenocarcinoma. Gastroenterol Clin North Am. 2002;31:18 421–440, viii. doi: 10.1016/s0889-8553(02)00016-x. [DOI] [PubMed] [Google Scholar]
- 16.Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005;97:142–146. doi: 10.1093/jnci/dji024. [DOI] [PubMed] [Google Scholar]
- 17.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 18.Sharma P, Meining AR, Coron E, et al. Real-time increased detection of neoplastic tissue in Barrett's esophagus with probe-based confocal laser endomicroscopy: final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2011;74:465–472. doi: 10.1016/j.gie.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaheen NJ, Overholt BF, Sampliner RE, et al. Durability of radiofrequency ablation in Barrett's esophagus with dysplasia. Gastroenterology. 2011;141:460–468. doi: 10.1053/j.gastro.2011.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett's esophagus with dysplasia. N Engl J Med. 2009;360:2277–2288. doi: 10.1056/NEJMoa0808145. [DOI] [PubMed] [Google Scholar]
- 21.Bulsiewicz WJ, Shaheen NJ. The role of radiofrequency ablation in the management of Barrett's esophagus. Gastrointest Endosc Clin N Am. 2011;21:95–109. doi: 10.1016/j.giec.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Bajbouj M, Vieth M, Rosch T, et al. Probe-based confocal laser endomicroscopy compared with standard four-quadrant biopsy for evaluation of neoplasia in Barrett's esophagus. Endoscopy. 2010;42:435–440. doi: 10.1055/s-0029-1244194. [DOI] [PubMed] [Google Scholar]
- 23.Wallace MB, Sharma P, Lightdale C, et al. Preliminary accuracy and interobserver agreement for the detection of intraepithelial neoplasia in Barrett's esophagus with probe-based confocal laser endomicroscopy. Gastrointest Endosc. 2010;72:19–24. doi: 10.1016/j.gie.2010.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]