Abstract
Background
Carcinosarcoma is an exceptionally rare and poorly differentiated kind of breast neoplasm with only few published reports in the literature.
Case Report
We report a case of breast carcinosarcoma in a 26-year-old Chinese female patient, presenting as multiple lumps in a single breast. A nipple-sparing modified radical mastectomy was performed. The patient is now in her 7th postoperative month and disease-free.
Conclusion
Carcinosarcoma is challenging to diagnose preoperatively, even with core needle biopsy histopathology. Modified radical mastectomy is an efficient and practical operative treatment. Application of adjuvant therapy should be based on the proportion of carcinomatous component of the lesion in pathological test. Careful periodic follow-up after the initial treatment is strongly recommended.
Keywords: Carcinosarcoma, Breast
Abstract
Hintergrund
Das Karzinosarkom ist ein äußerst seltener und schlecht differenzierter Mammatumor, und bisher existieren nur wenige Berichte in der Literatur.
Fallbericht
Wir berichten von einer 26-jährigen chinesischen Patientin mit Karzinosarkom der Brust, welches sich als multiple Knoten in nur einer Brust darstellte. Es wurde eine brustwarzenerhaltende modifiziert radikale Mastektomie durchgeführt. Die Patientin ist mittlerweile im 7. postoperativen Monat und weiterhin krankheitsfrei.
Schlussfolgerung
Karzinosarkome sind präoperativ selbst durch die histopathologische Untersuchung von Hohlnadelbiopsien schwierig zu diagnostizieren. Die modifizierte radikale Mastektomie stellt eine effektive und praktische chirurgische Behandlung dar. Der Einsatz adjuvanter Therapien sollte sich nach dem pathologischen Anteil der karzinomatösen Komponente in der Läsion richten. Gewissenhaftes und regelmäßiges Follow-up im Anschluss an die initiale Therapie wird dringend empfohlen.
Introduction
The term carcinosarcoma is used to describe the biphasic malignant neoplasm which contains both carcinomatous and sarcomatous elements without a transitional zone. Carcinosarcomas occur in various organs throughout the body. Breast is an exceptionally rare primary site for carcinosarcoma. It accounts for less than 2% of the total incidence of all breast malignancies [1]. Here, we present a further case of breast carcinosarcoma in a Chinese female, who is the youngest patient reported in the literature so far, that presented as multiple lumps in a single breast.
Case Report
A 26-year-old woman presented with a complaint of a lump in the left breast of 2 years duration. During the 2-year period, she had noticed that the mass augmented gradually but had disregarded this. 2 days before presenting to our hospital, diabrosis with exudation was observed on the surface of the mass. The patient had a suspicious fibroadenoma history in this area. On physical examination, an irregularly shaped malleable mass measuring 12 × 10 cm was found in the inferior outer quadrant of the left breast with a 2 × 2 cm ulcer on the surface. Bilateral axillary examination revealed no lymphadenopathy. Sonography detected an 11 × 8 cm isoechoic mass in the left breast with a 4.7 × 1.1 cm hypoechoic area within the mass. Ultrasound examination of the bilateral axillary fossa was unremarkable. Considering the volume of the mass, no mammogram was suggested. Based on clinical manifestations, the mass had previously been clinically suspected as a cystosarcoma phyllodes or fibroadenoma.
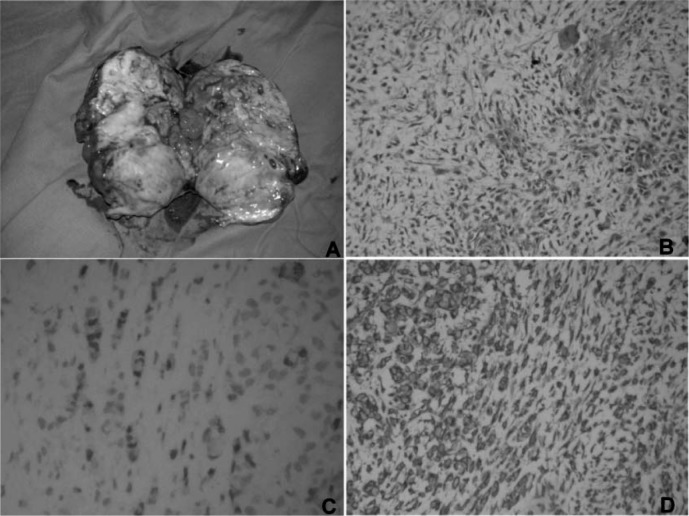
A lumpectomy was performed, and another small lesion measuring 2 × 2 cm beside the large mass was also resected. On macroscopic examination, the surgical sample of the bigger lesion was 12 × 10 cm in dimension with a grayish-white cut surface and cystic-solid features (fig. 1A). The surgical samples were identified as phyllodes tumor with active growth and mesenchymal atypia by intraoperative rapid frozen section diagnosis. Comprehensive histological and immunohistochemical examinations confirmed both masses as extensive areas of malignant phyllodes tumor with invasive and poorly differentiated carcinoma (fig. 1B). None of the microscopic fields contained evidence of transition between the 2 elements. Immunohistochemical examinations revealed neither hormonal receptor nor CerbB-2 positivity in both components; positive reactions for cytokeratins (CK (pan), CK5/6, CAM5.2) were noted in the epithelial component (fig 1C) but not in the sarcomatous cells. Both components were positive for vimentin (fig 1D). Both lesions were diagnosed as breast carcinosarcoma. A nipple-sparing modified radical mastectomy was performed in the left breast. Histological and immunohistochemical examination revealed another small lesion (2 × 2 cm) in the mastectomy sample which was also a carcinosarcoma. Ipsilateral axillary lymph nodes showed no metastasis of either the carcinomatous or sarcomatous component. The patient's preoperative chest X-ray, abdominal computed tomography, and bone scan were normal, and she was diagnosed as having breast carcinosarcoma (pT3N0M0 stage IIB). Adjuvant chemotherapy and radiotherapy were suggested but refused by the patient. The patient is now in her 7th postoperative month, and remains disease-free.
Fig. 1.
Pathological examination of the lesion. A Macroscopic view; B Hematoxylin-eosin staining (×200) revealed malignant phyllodes tumor with invasive, poorly differentiated carcinoma; C Immunohistochemistry (×400) revealed positivity for CK-pan of the invasive, poorly differentiated carcinomatous component but not of the sarcomatous component; D Immunohistochemistry (×200) revealed positivity for vimentin of both components.
Discussion
Carcinosarcoma is an exceptionally rare and poorly differentiated breast neoplasm characterized by biphasic cell differentiation possessing carcinomatous components and malignant mesenchymal elements without definite evidence of transition between the two [2]. The incidence of breast carcinosarcoma is 0.1–0.2% of all breast malignancies [3, 4], which is in accordance with the statistics of our hospital; 2 cases of carcinosarcoma out of 1,425 newly diagnosed breast neoplasms (incidence 0.14%) were retrospectively analyzed between 2001 and 2010 in our hospital. The age at primary diagnosis ranges from 32 to 77 [5, 6] according to the literature. Our patient was diagnosed at age 26, which is the youngest recorded age yet. Breast lumps are the most common complaint; however, this is the first recorded case of a patient presenting with multiple lumps all of which were diagnosed as carcinosarcoma.
Mammography, sonography, and magnetic resonance mammography are frequently used breast imaging techniques in the diagnosis of breast neoplasms [7]. However, all 3 techniques have unsatisfactory specificity in the diagnosis of breast carcinosarcoma. Fine needle biopsy or core biopsy are frequently used techniques in the preoperative diagnosis of breast neoplasms. However, presurgical diagnosis can be challenging [8]. Frozen section diagnosis of breast lumps is of high accuracy, with a sensitivity and specificity of more than 90 and 99%, respectively [9, 10]. However, in breast carcinosarcoma, there may be some limitations to frozen section diagnosis as seen in the present case, as the small selected piece of tissue for frozen section diagnosis is unable to represent the overall profile of the tumor.
The histogenesis of breast carcinosarcoma is still a matter of debate. A single totipotent cell with biphasic differentiation has been proven to be attributed to the development of carcinosarcoma [11]. Myoepithelial cells and myofibroblastic metaplasia are also thought to be responsible for the origination of carcinosarcoma [12]. On the other hand, several cases arising from preexisting fibroadenomas or phyllodes tumors [13] have been reported previously. In the present patient, a suspicious pre-existing fibroadenoma coupled with a phyllodes-type structure in the surgical sample would confirm that the development of carcinosarcoma was attributable to the pre-existing fibroadenoma.
On pathologic examination, the existences of both epithelial and mesenchymal components is variable [13], and distinct positive reactions are displayed in immunohistochemical examination. Carcinosarcoma should be differentiated from other metaplastic carcinomas. The most important evidence is the non-existent region of transition between the 2 elements [7]. Thus, a thorough pathological search for the transitional area is paramount. Carcinosarcoma can also presents as malignant phyllodes tumor accompanied by malignant epithelial components which may constitute only a small proportion of the entire carcinosarcoma [7]. The pathological manifestation in the present patient was also malignant phyllodes tumor with a poorly differentiated carcinomatous component. Such presentation will frequently be misdiagnosed by pathologists as sarcoma, especially if sampling is insufficient or microscopic investigation inadequate.
Treatment strategies of breast carcinosarcoma correspond to those of other common pathological types of breast cancer. Modified radical mastectomy is an efficient and practical choice in the treatment of breast carcinosarcoma [7, 9, 14], especially when the lesion is highly suspicious of malignancy or a definite diagnosis has already been made. The axillary nodes are one of the typical sites of metastasis (incidence 26%) from either the carcinomatous or sarcomatous component of the primary site [2, 11]. Thus, mastectomy coupled with axillary dissection is often performed in the surgical treatment of breast carcinosarcoma. With a view to potential breast reconstruction, we performed a nipple-sparing modified radical mastectomy, but lumpectomy and axillary dissection are also a possible choice of surgery. Chemotherapy and radiotherapy may be applied in various combinations as adjuvant therapy, [7]; however, the exact effects of chemotherapy or radiotherapy are still unknown due to the small number of cases. Adjuvant chemotherapy regimens often resemble those used in breast carcinoma, such as CMF (cyclophosphamide, methotrexate, 5-fluorouracil) [7, 11] and anthracycline/taxane-based combinations. However, evidence from existing clinical research into adjuvant chemotherapy in breast cancer suggests that CMF is less effective than anthracycline/taxane-based therapeutic combinations. We propose anthracycline/taxane-based regimens are suitable choices in the adjuvant chemotherapy of breast carcinosarcoma. In the present patient, the pathologic stage was pT3N0M0 (stage IIB) according to the 7th AJCC Cancer Staging Manual [15], and a combined adjuvant therapeutic strategy containing chemotherapy (docetaxel/doxorubicin/cyclophosphamide, every 21 days for 6 cycles) and radiotherapy was proposed. However, the patient refused to undergo this process. We suggest that the proportions of the 2 components may be a determinant in the application of adjuvant chemotherapy or radiotherapy, due to differences in reactivity between the 2 elements. As metaplastic tumors of the breast are usually poor in differentiation, hormone receptor and HER2-neu expression are negative in most cases [16, 17], and adjuvant hormone therapy is not suggested. In the present patient, hormone receptors also stained negative, and neither tamoxifen nor aromatase inhibitors were recommended. Monoclonal antibodies and small molecule inhibitors of the epidermal growth factor receptor (EGFR), such as gefitinib (ZD1839, Iressa®, AstraZeneca, Wedel, Germany) and cetuximab (Erbitux®, Merck KGaA, Darmstadt, Germany), may also be used in adjuvant therapy as the HER1/EGFR receptor is reported to be overexpressed [18].
The prognosis of breast carcinosarcoma is poor [4, 7, 9, 17, 19]. The cumulative 5-year survival rate is 49% [7]. As neoplastic cells often extend into the perivascular tissue and beyond the tumor capsule, local recurrence is common [3]. Hematogenous spread is the most common route of metastasis, and lung and pleura are the most common locations of distant metastasis [17]. If the recurrence is resectable, the prognosis can be improved, but due to the aggressive nature of the neoplasm, relapse can occur rapidly. Accordingly, careful periodic follow-up after the initial treatment is strongly recommended to detect metastasis and recurrence early.
In conclusion, as there is no accurate staging system for breast carcinosarcoma and only a limited number of cases, the exact effects of chemotherapy or radiotherapy are still unknown. We assume that the proportions of the 2 components may be a determinant for the application of adjuvant therapy. A careful periodic follow-up is paramount to detect metastasis and recurrence early and minimize mortality.
Disclosure Statement
Wei Tian has no conflict of interest. Dong Xu received research grants from National Natural Science Foundation of China (No. 30901741) and Zhejiang Provincial Natural Science Foundation of China (No. Y2080308).
References
- 1.Kaufinan MW, Marti JR, Gallager HS, Hoehn JL. Carcinoma of the breast with pseudosarcomatous metaplasia. Cancer. 1984;53:1908–1917. doi: 10.1002/1097-0142(19840501)53:9<1908::aid-cncr2820530917>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 2.Wargotz ES, Norris HJ. Metaplastic carcinomas of the breast. III. Carcinosarcoma. Cancer. 1989;64:1490–1499. doi: 10.1002/1097-0142(19891001)64:7<1490::aid-cncr2820640722>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 3.Bolton B, Sieunarine K. Carcinosarcoma: a rare tumour of the breast. Aust N Z J Surg. 1990;60:917–919. doi: 10.1111/j.1445-2197.1990.tb07501.x. [DOI] [PubMed] [Google Scholar]
- 4.Gogas J, Kouskos E, Markopoulos C, Mantas D, Antonopoulou Z, Kontzoglou K, Stamoulis J, Kyriakou V. Carcinosarcoma of the breast: report of two cases. Eur J Gynaecol Oncol. 2003;24:93–95. [PubMed] [Google Scholar]
- 5.Carstens HB, Cooke JL. Mammary carcinosarcoma presenting as rhabdomyosarcoma: an ultrastructural and immunocytochemical study. Ultrastruct Pathol. 1990;14:537–544. doi: 10.3109/01913129009076141. [DOI] [PubMed] [Google Scholar]
- 6.Laky D, Penciu M. Mammary carcinosarcoma with osteochondrosarcomatous differentiations. Rom J Morphol Embryol. 1993;39:149–152. [PubMed] [Google Scholar]
- 7.Tokudome N, Sakamoto G, Sakai T, Sarumaru S, Okuyama N, Hori F, Horii R, Akiyama F, Tanabe M, Saito K, Takahashi K, Kasumi F. A case of carcinosarcoma of the breast. Breast Cancer. 2005;12:149–153. doi: 10.1007/BF02966829. [DOI] [PubMed] [Google Scholar]
- 8.Hoda SA, Rosen PP. Observations on the pathologic diagnosis of selected unusual lesions in needle core biopsies of breast. Breast J. 2004;10:522–527. doi: 10.1111/j.1075-122X.2004.21412.x. [DOI] [PubMed] [Google Scholar]
- 9.Bianchi S, Palli D, Ciatto S, Galli M, Giorgi D, Vezzosi V, Del Turco MR, Cataliotti L, Cardona G, Zampi G. Accuracy and reliability of frozen section diagnosis in a series of 672 nonpalpable breast lesions. Am J Clin Pathol. 1995;103:199–205. doi: 10.1093/ajcp/103.2.199. [DOI] [PubMed] [Google Scholar]
- 10.Sultana N, Kayani N. Validity of frozen section in the diagnosis of breast lumps: 5 years experience at the Aga Khan University Hospital. J Pak Med Assoc. 2005;55:533–536. [PubMed] [Google Scholar]
- 11.Wada H, Enomoto T, Tsujimoto M, Nomura T, Murata Y, Shroyer KR. Carcinosarcoma of the breast: molecular-biological study for analysis of histogenesis. Hum Pathol. 1998;29:1324–1328. doi: 10.1016/s0046-8177(98)90266-0. [DOI] [PubMed] [Google Scholar]
- 12.Kurian KM, Al-Nafussi A. Sarcomatoid/metaplastic carcinoma of the breast: a clinicopathological study of 12 cases. Histopathology. 2002;40:58–64. doi: 10.1046/j.1365-2559.2002.01319.x. [DOI] [PubMed] [Google Scholar]
- 13.Harris M, Persaud V. Carcinosarcoma of the breast. J Pathol. 1974;112:99–105. doi: 10.1002/path.1711120205. [DOI] [PubMed] [Google Scholar]
- 14.Santiago Pérez JT, Pérez Vázquez MR, Rivera Valdespino Ade L, Gil Valdés D. Carcinosarcoma of the breast: a tumour with controversial histogenesis. Clin Transl Oncol. 2005;7:255–257. doi: 10.1007/BF02710172. [DOI] [PubMed] [Google Scholar]
- 15.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC Cancer Staging Manual. 7th ed. New York: Springer-Verlag; 2010. [Google Scholar]
- 16.Tse GM, Tan PH, Putti TC, Lui PC, Chaiwun B, Law BK. Metaplastic carcinoma of the breast: a clinicopathological review. J Clin Pathol. 2006;59:1079–1083. doi: 10.1136/jcp.2005.030536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kijima Y, Umekita Y, Yoshinaka H, Owaki T, Sakamoto A, Yoshida H, Aikou T. A case of breast carcinoma with cartilaginous and osseous metaplasia. Breast Cancer. 2006;13:214–219. doi: 10.2325/jbcs.13.214. [DOI] [PubMed] [Google Scholar]
- 18.Esses KM, Hagmaier RM, Blanchard SA, Lazarchick JJ, Riker AI. Carcinosarcoma of the breast: two case reports and review of the literature. Cases J. 2009;2:15. doi: 10.1186/1757-1626-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suspitsin EN, Sokolenko AP, Voskresenskiy DA, Ivantsov AO, Shelehova KV, Klimashevskiy VF, Matsko DE, Semiglazov VF, Imyanitov EN. Mixed epithelial/mesenchymal metaplastic carcinoma (carcinosarcoma) of the breast in BRCA1 carrier. Breast Cancer. 2011;18:137–140. doi: 10.1007/s12282-009-0105-0. [DOI] [PubMed] [Google Scholar]