Abstract
Pluripotent and multipotent stem cells adopt an osteoblastic phenotype when cultured in environments that enhance their osteogenic potential. Embryonic stem cells differentiated as embryoid bodies (EBs) in osteogenic medium containing β-glycerophosphate exhibit increased expression of bone markers, indicating that cells are osteoblastic. Interestingly, 1α,25-dihydroxyvitaminD3 (1,25D) enhances the osteogenic phenotype not just in EBs but also in multipotent adult mesenchymal stem cells (MSCs). 1,25D acts on osteoblasts via classical vitamin D receptors (VDR) and via a membrane 1,25D-binding protein [protein disulfide isomerase family A, member 3 (PDIA3)], which activates protein kinase C -signaling. The aims of this study were to determine whether these receptors are regulated during osteogenic differentiation of stem cells and if stem cells and differentiated progeny are responsive to 1,25D. mRNA and protein levels for VDR, PDIA3, and osteoblast-associated proteins were measured in undifferentiated cells and in cells treated with osteogenic medium. Mouse EBs expressed both VDR and PDIA3, but VDR increased as cells underwent osteogenic differentiation. Human MSCs expressed Pdia3 at constant levels throughout differentiation, but VDR increased in cells treated with osteogenic medium. These results suggest that both 1,25D signaling mechanisms are important, with PDIA3 playing a greater role during early events and VDR playing a greater role in later stages of differentiation. Understanding these coordinated events provide a powerful tool to control pluripotent and multipotent stem cell differentiation through induction medium.
Introduction
One goal of regenerative medicine is to provide a source of cells with potential to proliferate, thereby increasing the available pool, and to differentiate into specific lineages of interest. Embryonic stem cells (ESCs) are pluripotent cells derived from the inner cell mass of a preimplantation blastocyst [1,2]. ESCs can be indefinitely maintained in culture under appropriate conditions without losing their pluripotent phenotype. They also have the unique ability to differentiate into cell types comprising all 3 germ lineages, including cardiomyocytes, chondrocytes, osteoblasts, adipocytes, endothelial cells, or neurons [3–5]. In addition to their use in tissue engineering and regenerative therapies [6–9], ESCs have been used as an in vitro model to study early stages of cellular differentiation. ESCs spontaneously form 3-dimensional cell aggregates in suspension culture conditions and differentiate in the form of “embryoid bodies” (EBs) [10–13]. EBs undergo morphogenic events similar to normal embryogenesis, and simultaneously yield cell types from endoderm, ectoderm, and mesoderm germ layers [14,15]. Differentiation of ESCs and EBs to specific phenotypes can be induced by supplementing culture medium with specific stimulatory or inhibitory agents and molecules [16–18].
Multipotent adult stem cells, also commonly referred to as somatic stem cells, are found in diverse tissues or organs and have the capacity to divide and differentiate into several cell phenotypes. The most studied adult stem cells are mesenchymal stem cells (MSCs). MSCs are present in all tissues of mesenchymal origin, but the most commonly used are MSCs isolated from bone marrow. Like ESCs, MSCs have been studied for their potential applications in regenerative therapies, mainly in orthopedics to regenerate cartilage, tendon, and bone because of their propensity to differentiate into musculoskeletal cell types [19].
Although there are a number of protocols that promote the differentiation of ESCs and MSCs into osteoblasts, most studies indicate that this can be achieved by establishing an environment rich in phosphate, which results in formation of a mineralized extracellular matrix [20,21]. The most commonly used osteogenic medium (OM) formulations contain β-glycerophosphate (BGP), dexamethasone, and ascorbic acid [22–24]. Some studies have shown that addition of the vitamin D metabolite 1α,25-dihydroxy vitamin D3 (1α,25(OH)2D3) to OM enhances osteoblastic differentiation of stem cells [25,26]. 1α,25(OH)2D3 plays an important role in calcium and phosphate homeostasis and both catabolic and anabolic effects of this hormone have been demonstrated in bone cells [27]. Moreover, 1α,25(OH)2D3 regulates the expression of bone marker genes like Runx2, collagen type I, osteocalcin (Ocn), and bone sialoprotein in osteoblasts [28,29], indicating that it plays a role in their differentiation.
Effects of 1α,25(OH)2D3 in osteoblasts are mediated by 2 vitamin D receptors (VDR), the nuclear receptor [28] and a membrane-associated 1α,25(OH)2D3-binding protein called protein disulfide isomerase A3 (PDIA3, also known as ERp60, ERp57, Grp58, and 1,25-MARRS) [30–32]. In classical VDR activation, 1α,25(OH)2D3 is recognized by cytoplasmic VDR, which then dimerizes with the retinoic acid receptor. This complex binds to vitamin D responsive elements (VDREs) in target genes and induces expression of osteoblast markers as such Ocn and RUNX2 [33,34]. The interaction of 1α,25(OH)2D3 with PDIA3 in the membrane associated vitamin D receptor complex activates a rapid membrane-initiated signaling cascade that involves protein kinase C (PKC) and mitogen activated protein kinase activation, resulting in cellular events that modulate cell proliferation and differentiation [35–39].
The aims of this study were to evaluate the phenotype of stem cells during osteogenic induction and assess their response to exogenous 1α,25(OH)2D3. To do this, we examined 2 markers of osteoblastic differentiation: alkaline phosphatase specific activity, which is an early differentiation marker, and the amount of secreted Ocn, which is a late differentiation marker. In addition, we determined whether the cells possessed mRNA for VDR and PDIA3; whether they produced protein for these 1α,25(OH)2D3 receptors; the distribution of each receptor within the embryoid body; the functionality of PDIA3 with respect to PKC activation; and the functionality of VDR with respect to osteopontin expression. Finally, we assessed whether there were changes in receptor type during osteogenic differentiation of the EBs. We took advantage of a novel ESC culture system in which ESCs are grown under rotary culture conditions to form a homogeneous population of EBs [13,40]. The expression of receptors for 1α,25(OH)2D3 and the effects of 1α,25(OH)2D3 on EBs was then compared to MSCs to determine whether they are a general property of osteogenic differentiation of multipotent cells.
Materials and Methods
Embryoid body cell culture
Undifferentiated mouse ESCs (D3 line) were grown on tissue culture dishes coated with 0.1% gelatin. Cells were cultured in ESC medium consisting of Dulbecco's modification of Eagle's medium (DMEM; Mediatech, Manassas, VA) supplemented with 15% fetal bovine serum (FBS; Hyclone, Logan, UT), 1×nonessential amino acids (Mediatech), 100 U/mL penicillin/100 μg/mL streptomyocin/0.25 μg/mL amphotericin (GIBCO; Carlsbad, CA), 2 mM L-glutamine (Mediatech), 0.1 mM β-mercaptoethanol (Fisher, Fairlawn, NJ), and 103 U/mL of leukemia inhibitory factor (LIF; Chemicon, Temecula, CA). The medium was exchanged every 48 h, and cells were passaged with 0.05% trypsin before reaching 70% confluence, typically 3 days after initial seeding. Undifferentiated ESCs were inoculated into 100 mm bacteriological grade Petri dishes as a single cell suspension at 2×105 cells/ml in ESC medium without LIF and then cultured on rotary orbital shakers (Lab-Line Lab Rotator, Model #2314; Barnstead International, Dubuque, IA) at 40 rotations per min to form EBs as previously described [40]. To change medium, EBs were collected by gravity-induced sedimentation and 90% of the medium was exchanged with fresh ESC medium.
For samples treated with BGP (MP Biomedicals, Solon, OH), EBs were cultured with ESC culture medium supplemented with 10 mM BGP from day 5 through 14 after EB formation. In our experimental set up, the addition of BGP (2.5–10 mM) alone to mouse EBs in serum-containing medium appears to be the minimal essential ingredient to promote endogenous CaP mineralization within EBs and to induce a significant increase in the expression of several osteogenic-related genes by day 14 of differentiation (Runx-2, bone sialoprotein, Ocn, osteopontin) (data not shown). We have examined the effects of adding dexamethasone (10 nM) and ascorbic acid (50 μg/mL) to the osteogenic differentiation medium of EBs maintained in rotary orbital suspension culture but did not observe any substantial increase in osteogenic differentiation.
Embryoid body mRNA expression
We examined gene expression in EBs to determine whether levels of mRNA for key proteins were sensitive to osteoblastic differentiation. VDR and PDIA3 are receptors for 1α,25(OH)2D3; osteoprotegerin (OPG) is secreted by differentiated osteoblasts [41]; osteopontin is a 1α,25(OH)2D3-sensitive extracellular matrix protein that possesses a VDRE [42] and is regulated via PDIA3 [39]; and α2β1 integrin expression is associated with osteoblast differentiation through collagen type 1 recognition [43,44].
RNA was harvested from EBs immediately after formation (day 0) or from EBs cultured for 7 or 14 days in basal medium or medium supplemented with BGP using a TRIzol® (Invitrogen, Carlsbad, CA) extraction method and was quantified using a NanoDrop spectrophotometer (Thermo Scientific, Waltham, MA). mRNA was amplified using reverse transcription (OmniScript RT, Qiagen, Valencia, CA) and random oligomers (Promega, Madison, WI). Starting quantities of mRNA were determined using SybrGreen chemistry (BioRad Laboratories, Hercules, CA) in an iQ5 Imaging System (BioRad). Untreated cells were used to generate a standard curve for each gene of interest and values for each sample extrapolated. Expression of mRNA was measured for mouse Vdr, Pdia3, Tnfsf11 (the gene that codes for OPG), osteopontin (Opn), integrin alpha 2 (Itga2), and integrin beta 1 (Itgb1) (primer sequences listed in Table 1). Gene expression was normalized to expression of glyceraldehyde-3-phosphate dehydrogenase (Gapdh) per 1 μg mRNA.
Table 1.
Primer Sequences Used in Real-Time Quantitative Polymerase Chain Reaction Analysis
| Vdr | F | AGG CAG GCA GAA GAG ATG AG |
| R | AGG GAT GAT GGG TAG GTT GTG | |
| Pdia3 | F | CCA ATG ATG TGC CTT CTC |
| R | TGT GCC TTC TTC TTC TTC | |
| Tnfsf11 | F | CGC CAA CAT TTG CTT TCG |
| R | TGC TCC CTC CTT TCA TCA | |
| Opn | F | AAC TCT TCC AAG CAA TTC C |
| R | TCT CAT CAG ACT CAT CCG | |
| Itga2 | F | ACT GTT CAA GGA GGA GAC |
| R | GGT CAA AGG CTT GTT TAG G | |
| Itgb1 | F | ATT ACT CAG ATC CAA CCA C |
| R | TCC TCC TCA TTT CAT TCA TC | |
| Gapdh | F | TTC AAC GGC ACA GTC AAG G |
| R | TCT CGC TCC TGG AAG ATG G |
Western blots of VDR and PDIA3
Western blots of VDR and PDIA3 were performed to validate the presence of these proteins in the EBs. Treated EBs were lyzed in 300μL radioimmunoprecipitation assay buffer (RIPA) buffer and resolved on 4%–20% Tris glycine gels (LongLife; NuSep, Bogart, GA) using gel electrophoresis. Proteins were transferred from the gel onto a nitrocellulose membrane using the iBlot® Dry Blotting transfer method (Invitrogen, Carlsbad, CA). Membranes were blocked against nonspecific interactions by incubating in phosphate buffered saline (PBS) containing 1% bovine serum albumin (BSA) for 1 h. Membranes were then incubated overnight using specific primary antibodies against PDIA3 (sc-18620, Santa Cruz Biotechnology, Santa Cruz, CA), VDR (sc-1008, Santa Cruz Biotechnology), or glyceraldehyde 3-phosphate dehydrogenase (GAPDH, MAB374, Millipore, Billerica, MA). After incubation, membranes were washed 3 times using PBS with 0.05% Tween-20 and then incubated in 1% BSA in PBS with either goat anti-rabbit or goat anti-mouse horseradish peroxidase-conjugated secondary antibodies (Bio-Rad Laboratories) for 1 h. Membranes were washed 3 times in 0.05% Tween-20 in PBS. Blots were developed using SuperSignal West Pico Chemiluminescent System (Thermo Fisher Scientific, Rockford, IL). Membranes were imaged using VersaDoc imaging system (Bio-Rad Laboratories). Pixel intensity of bands was quantified using Quantity One Software (Bio-Rad Laboratories) and normalized to pixel intensity of GAPDH.
Immunohistochemistry
Immunohistochemistry was performed to assess the distribution of PDIA3 and VDR in the EBs. EBs were fixed in 10% formalin for 35 min, rinsed in PBS, embedded in Histogel (Richard Allen Scientific, Kalamazoo, MI), processed, and embedded in paraffin. For each sample, 5μm sections were taken every 50μm and affixed to positively charged glass slides. Deparaffinized slides were used for staining. Samples were stained with antibodies against PDIA3 and VDR, with Alexa Fluor 488 phalloidin (Invitrogen) to stain actin filaments, and 4′,6-diamidino-2-phenylindole to stain the nucleus (Invitrogen).
Osteogenic protein production
In addition to verifying that the EBs expressed mRNAs for proteins associated with osteoblastic differentiation, we quantified production of secreted proteins by immunoassay. After 14 days culture in control medium or medium supplemented with BGP, EBs were treated for 24 h with 10 nM 1α,25(OH)2D3 (Enzo Life Sciences, Plymouth Meeting, PA). The dose of 1α,25(OH)2D3 was based on previous studies examining the effects of the vitamin D metabolite on differentiation of ESCs into mineralizing osteoblasts [45]. Ocn in the conditioned medium was measured using a commercially available radioimmunoassay (Biomedical Technologies, Inc., Stoughton, MA). OPG and osteopontin were measured using commercially available ELISAs, according to manufacturer's specifications (DuoSet; R&D Systems, Minneapolis, MN). In EBs, levels of secreted proteins were normalized to total DNA content (Quant-iT PicoGreen Assay; Invitrogen). EBs were then lyzed in 0.05% Triton X-100 and alkaline phosphatase specific activity was measured as the release of p-nitrophenol from p-nitrophenylphosphate at pH 10.2 and normalized to total protein content (Pierce BCA Protein Assay; Thermo Fisher, Rockford, IL) [46].
PKC assay
PKC activity was measured in response to 1α,25(OH)2D3 to determine whether PDIA3 was functional. EBs were cultured as above until day 14. Based on previous studies showing that 10 nM 1α,25(OH)2D3 causes rapid PDIA3-dependent activation of PKC in mouse osteoblasts within 9 min [39], both cell types were then treated for 9 min with either 0.01% ethanol (vehicle) or 10 nM 1α,25(OH)2D3. After incubation, EBs were spun for 3 m at 2000xg, the medium removed, and lyzed in 1 mL cold RIPA buffer (20 mM Tris-HCl, 150 mM NaCl, 5 mM disodium EDTA, 1% Nonadet P-40). PKC activity was measured using a commercially available assay kit (GE Biosciences, Piscataway, NJ) and results normalized to total protein content of the lysates as described above.
Human MSCs
We compared the expression of receptors for 1α,25(OH)2D3 in EBs to expression in human MSCs (Lonza Walkersville, Walkersville, MD) during osteoblastic differentiation. MSCs were cultured in MSC growth medium (GM, Lonza Walkersville) or hMSC Osteogenic BulletKit (OST, Lonza Walkersville) for 14 days. Western blots were performed for VDR, PDIA3, and GAPDH as described above. Effects of 1α,25(OH)2D3 on differentiation were assessed as a function of alkaline phosphatase specific activity, and osteocalcin and OPG production. MSCs were cultured for 14 days in GM or OST. 1α,25(OH)2D3 (10 nM) was added to the cultures for an additional 24 h and the conditioned medium was collected. Enzyme activity was measured in cell lysates. Secreted proteins were normalized to total cell number (Z2 Cell Counter; Beckman Coulter, Hercules, CA).
Presence of functional PDIA3 was determined by assessing 1α,25(OH)2D3-dependent PKC activity. MSCs were cultured in growth medium until confluence. Cells were treated with 1α,25(OH)2D3 for 15 min, and lyzed in RIPA immediately after treatment. PKC was assayed as described above.
Statistical analysis
Data presented are from 1 of 2 sets of experiments, with comparable results. Each data point is the mean±SEM for 6 independent cultures, with the exception of the mRNA expression experiment, where n=4. The data shown for the mRNA analyses are ratios of the mRNA for the gene of interest to Gapdh rather than treatment/control ratios to enable analysis of experimental variability. Data were analyzed by analysis of variance and significant differences between groups determined using Bonferroni's modification of the Student's t-test. P<0.05 was considered to be significant.
Results
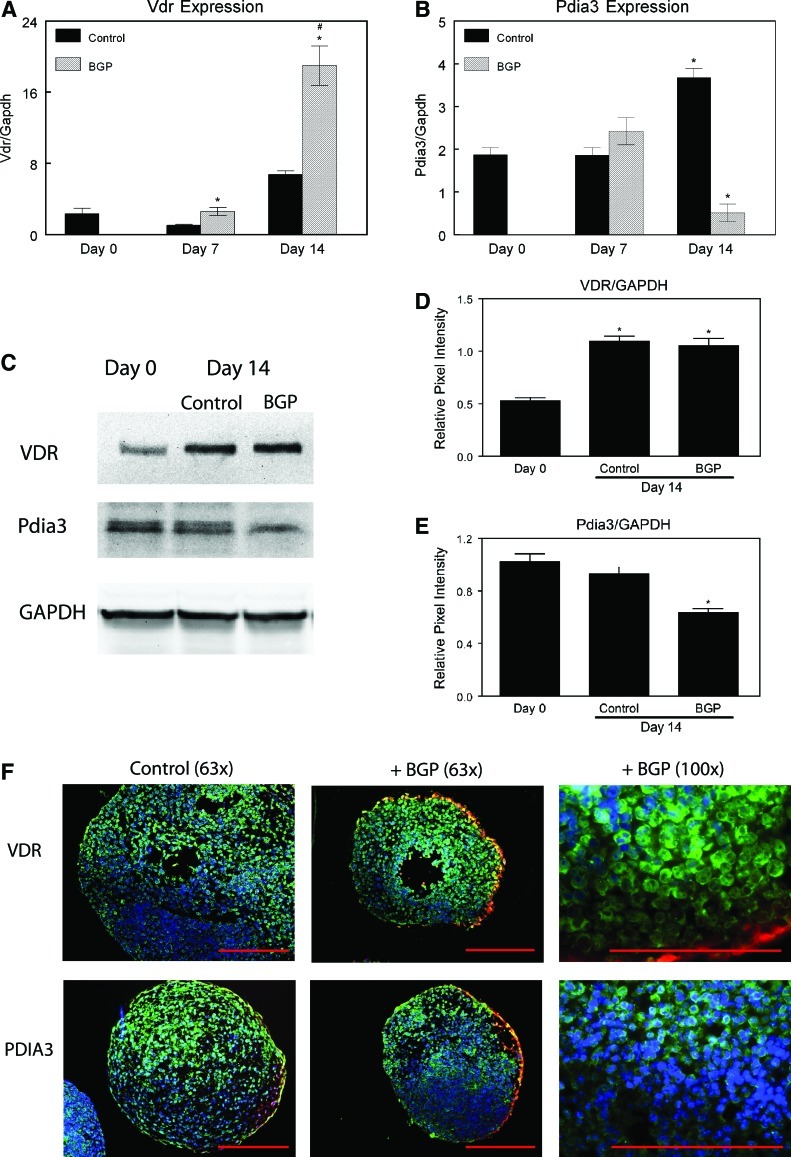
EBs expressed mRNAs for VDR and PDIA3 and expression of each receptor mRNA was differentially regulated (Fig 1). After 7 days of differentiation, expression of Vdr was higher in EBs cultured in medium supplemented with BGP when compared with control medium (Fig. 1A); this effect was more pronounced after 14 days. Expression of Pdia3 was similar at days 0 and 7 in both media (Fig. 1B). After 14 days, expression of Pdia3 in control cells was higher than at day 0 or day 7, but 14 days of culture in the presence of BGP decreased expression of Pdia3.
FIG. 1.
Evaluation of vitamin D receptors in mouse embryoid bodies. Embryoid bodies were cultured with control medium or medium supplemented with BGP. Real-time qPCR was performed on samples at embryoid body formation (day 0), or after 7 or 14 days in culture. mRNA expression of Vdr (A) and Pdia3 (B) were measured and are presented as normalized to GAPDH. *P<0.05, versus day 0; #P<0.05, versus control. VDR and Pdia3 proteins were analyzed by western blot using GAPDH as a reference (C). Ratios of VDR/GAPDH (D) and PDIA3/GAPDH (E) were calculated using pixel intensity of western blot bands. *P<0.05, versus Day 0. Immunofluorescent staining of embryoid bodies was performed for VDR and Pdia3 after 14 days culture in control medium or medium supplemented with BGP (F). Cells were stained for β-actin (red), DAPI nuclear staining (blue), and antibodies against either VDR or Pdia3 (green) and imaged at 63×or 100×magnification (scale bar-50 μm). BGP, β-glycerophosphate; qPCR, quantitative polymerase chain reaction; GAPDH, glyceraldehyde 3-phosphate dehydrogenase; VDR, vitamin D receptors; PDIA3, protein disulfide isomerase family A, member 3; DAPI, 4′,6-diamidino-2-phenylindole. Color images available online at www.liebertonline.com/scd
The presence of both VDR was confirmed using western blot (Fig. 1C). The ratio of VDR/GAPDH increased from day 0 to day 14 in both control and BGP culture groups (Fig. 1C, D). In contrast, PDIA3/GAPDH decreased at 14 days in cultures grown in medium containing BGP compared with day 0 (Fig. 1C, E). The presence of PDIA3 and VDR was also demonstrated by immunofluorescence staining (Fig. 1F). VDR and PDIA3 were distributed throughout the cell aggregates in control cultures after 14 days (Fig. 1F, left panels). However, EBs cultured with BGP had more VDR staining and less PDIA3 staining (Fig. 1F, middle panels), an effect more evident at higher magnification (Fig. 1F, right panels; 100×).
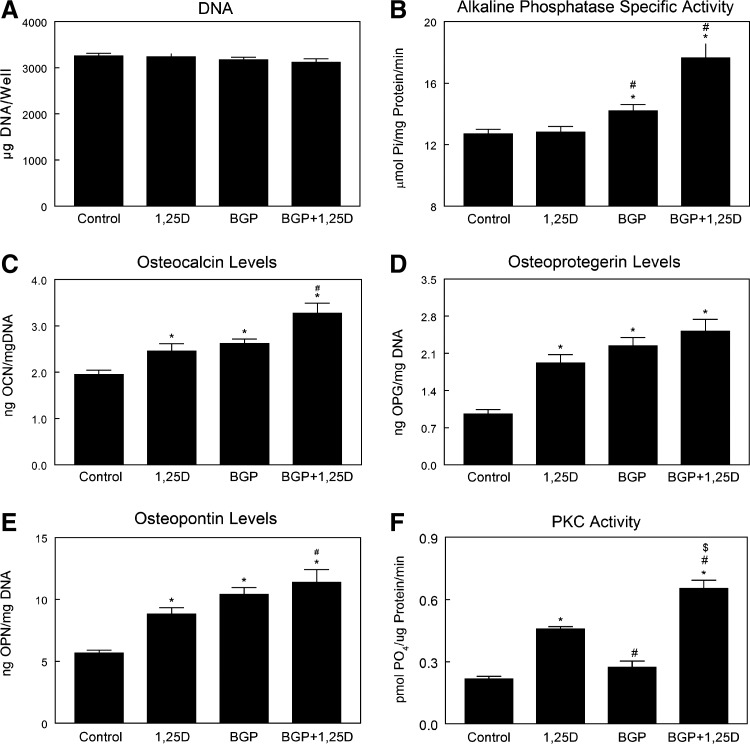
Changes in markers associated with osteogenic differentiation showed that EBs cultured in medium containing BGP exhibited an osteoblast-like phenotype and were more responsive to 1α,25(OH)2D3 than untreated cells. DNA content of EBs was similar among groups, independent of treatment (Fig. 2A). In cells cultured in control medium, alkaline phosphatase specific activity was unaffected by 1α,25(OH)2D3 treatment (Fig. 2B). However, culture with BGP stimulated alkaline phosphatase specific activity, and this effect was enhanced by 1α,25(OH)2D3 (Fig. 2B). Osteocalcin (Fig. 2C), OPG (Fig. 2D), and osteopontin (Fig. 2E) were equally stimulated by 1α,25(OH)2D3 or BGP treatment alone. Culture with BGP followed by 1α,25(OH)2D3 treatment stimulated greater osteocalcin and osteopontin secretion than 1α,25(OH)2D3 alone.
FIG. 2.
Osteogenic phenotype of mouse embryoid bodies. Embryoid bodies were cultured for 14 days in medium or medium supplemented with BGP. EBs were then treated with 0.01% ethanol or 1α,25(OH)2D3 for 24 h. DNA content (A) and alkaline phosphatase specific activity (B) were measured in cell lysates. Secreted osteocalcin (C), osteoprotegerin (D), and osteopontin (E) were measured in the conditioned medium. *P<0.05, versus control; #P<0.05, versus 1α,25(OH)2D3. To assess rapid, membrane-initiated signaling, protein kinase C activity was measured in EBs treated with 0.01% ethanol or 1α,25(OH)2D3 for 9 min (F). *P<0.05, versus control; #P<0.05, versus 1α,25(OH)2D3; $P<0.05, versus BGP. 1α,25(OH)2D3,1α,25-dihydroxyvitaminD3.
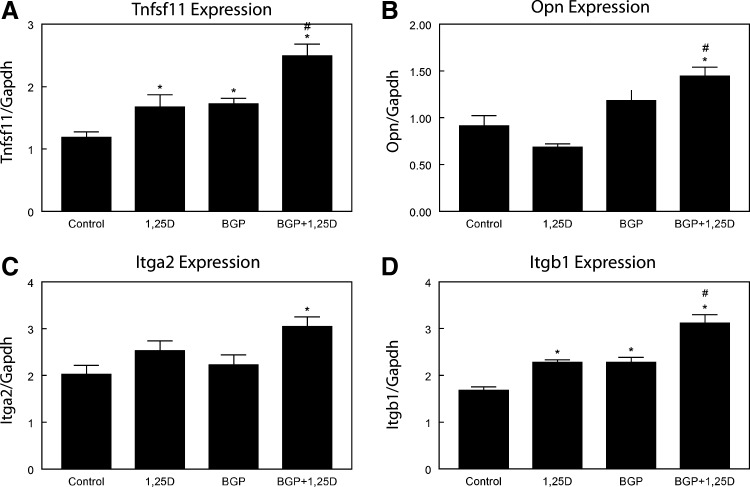
This treatment regime also affected expression of other genes. In EBs cultured in control medium, Tnfsf11 mRNA expression was upregulated after 1α,25(OH)2D3 treatment in comparison with control cultures (Fig. 3A). This effect was more robust when cells were cultured in medium containing BGP. Opn expression was not affected in cells cultured in medium with BGP or in control cultures treated with 1α,25(OH)2D3 (Fig. 3B). However, expression increased when EBs that were grown in OM were treated with 1α,25(OH)2D3. Itga2 mRNA was higher in cells cultured with BGP and treated with 1α,25(OH)2D3 than control cells (Fig. 3C). 1α,25(OH)2D3 stimulated Itgb1 expression in control medium and expression was also higher in OM compared with control medium. There was a synergistic increase in expression in cultures grown in OM and then treated with the vitamin D metabolite (Fig. 3D).
FIG. 3.
Osteogenic phenotype of mouse embryoid bodies. Embryoid bodies were cultured for 14 days in medium or medium supplemented with BGP. EBs were then treated with 0.01% ethanol or 1α,25(OH)2D3 for 12 h. Expression of Tnfsf11 (A), osteopontin (Opn, B), Itga2 (C), and Itgb1 (D) were measured by real-time qPCR. Gene expression was normalized to expression of Gapdh mRNA per 1 ug RNA. *P<0.05, versus control; #P<0.05, versus 1α,25(OH)2D3.
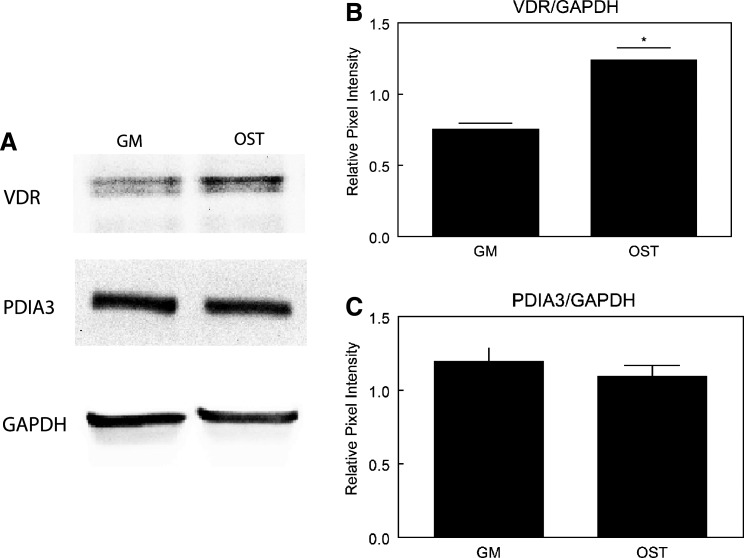
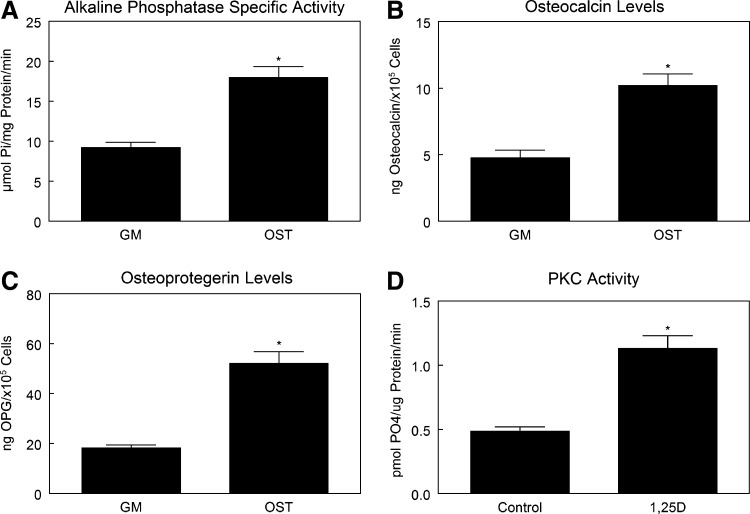
Human MSCs exhibited differential levels of VDR and PDIA3 when cultured in GM or OST in a manner comparable to EBs. VDR in cell lysates was higher in cells cultured in OST than in GM (Fig. 4A, B) and PDIA3 was similar in cells cultured in GM and OST (Fig. 4A, C). Levels of alkaline phosphatase specific activity (Fig. 5A), osteocalcin (Fig. 5B), and OPG (Fig. 5C) were higher in cells cultured in OST than in cells cultured in GM.
FIG. 4.
Western blot of vitamin D receptors in human mesenchymal stem cells. MSCs were cultured with (GM) or osteogenic medium (OST) for 14 days as described. Western blots against VDR and PDIA3 were performed. (A) Western blots of MSC lysates against VDR, PDIA3, and GAPDH. Calculated ratios of VDR/GAPDH (B) and PDIA3/GAPDH (C) using pixel intensity of western blot bands. *P<0.05, versus GM. MSC, mesenchymal stem cell.
FIG. 5.
Osteogenic phenotype of human mesenchymal stem cells. MSCs were cultured in growth medium (GM) or osteogenic medium (OST) for 14 days. MSCs were treated with fresh medium for 24 h. Alkaline phosphatase specific activity (A) was measured in the cell lysates. Levels of secreted osteocalcin (B) and osteoprotegerin (C) were measured in the conditioned medium. *P<0.05, versus control;*P<0.05, versus GM. To assess rapid, membrane-initiated signaling, protein kinase C activity was measured after 9 min treatment with 0.01% ethanol or 1α,25(OH)2D3 (D). *P<0.05, versus control; #P<0.05, versus 1α,25(OH)2D3.
PDIA3 was functional in both EBs (Fig. 2F) and in MSCs (Fig. 5D). PKC activity was comparable in control EB cultures and in EB cultures grown in medium containing BGP. 1α,25(OH)2D3 treatment caused a rapid increase in PKC activity in EBs cultured in both medium but the effect was 50% greater when EBs were grown in osteogenic medium. Similarly, 1α,25(OH)2D3 treatment caused a rapid increase in PKC activity in cultures of MSCs.
Discussion
Our results revealed that ESCs express mRNA and protein for both receptors for 1α,25(OH)2D3, VDR, and PDIA3, and they continue to be present as ESCs differentiate in the form of EBs. Interestingly, the expression of Vdr increased in EBs after 14 days of incubation, while Pdia3 expression decreased during the same period. We also examined the presence of both receptors in adult stem cells. Our results showed that osteogenic induction increased VDR whereas levels of PDIA3 remained stable after osteogenic induction. These results demonstrate that expression levels of these receptors are modulated during the course of osteogenic differentiation of stem cells. However, it is not known if changes in mRNA are required to initiate a change in osteoblast differentiation state or if they are a consequence of that state.
Our results indicate that EBs are sensitive to 1α,25(OH)2D3 at all stages of embryonic development, but effects are more robust in cultures induced to differentiate along an osteoblast lineage. This is positively correlated with increased expression of VDR and, not surprisingly, there is an increase in genes and proteins that possess VDREs including Opn and Ocn. Similar results were found when ESCs were cultured in a osteogenic induction media containing ascorbic acid, BGP, and 1α,25(OH)2D3. [47] In that study, the authors found an increase in alkaline phosphatase, osteocalcin, bone sialoprotein, osteopontin, osteonectin, collagen type 1, and runx2 after treatment with 1α,25(OH)2D3 [45].
The increase in the classical VDR may be due to the cells differentiating into osteoblasts, which require a microenvironment higher in calcium to mineralize their extracellular matrix. This is supported by the observation that VDR knockout mice do not exhibit rickets until they are weaned and no longer have high serum calcium provided by their mother [48]. This suggests that at least some of the early 1α,25(OH)2D3-dependent differentiation is via PDIA3 and later osteoid production and mineralization are dependent on VDR. The differential roles of VDR and PDIA3 are not exclusive, however, as VDR is required for development of growth plate tethers, even in Ca++-replete mice [49].
1α,25(OH)2D3 caused a dose-dependent rapid increase in PKC in the EBs, indicating that PDIA3 was functional as a receptor for the vitamin D metabolite. 1α,25(OH)2D3 induces PKC activation via a membrane-associated rapid-response mechanism and downstream gene expression in a number of cell types [31,39,50]. This effect is abolished in PDIA3-knockdown cells, indicating that PDIA3 mediates the 1α,25(OH)2D3 membrane response [39]. The PDIA3 knockout mouse is embryonically lethal by day E10.5 [51], confirming the importance of this protein in stem cell differentiation and embryonic development. In addition, PDIA3 deficiency in PDIA3+/− mice results in skeletal anomalies that affect trabecular and cortical bone [51]. Interestingly, the stimulatory effect of the 1α,25(OH)2D3 on PKC activity was greater in both EBs and MSC cultures grown in osteogenic medium. These results suggest that 1α,25(OH)2D3 may have diverse effects in stem cell differentiation and embryogenesis. It is not clear if cells with a more differentiated osteoblastic phenotype have higher affinity to 1α,25(OH)2D3 or if PDIA3 and VDR form a complex that trigger the rapid membrane response.
EBs also exhibited increased expression of mRNAs for α2 and β1 integrin subunits in cultures grown in osteogenic medium. Moreover, 1α,25(OH)2D3 caused a further increase in expression and this was particularly evident in the levels of β1. Integrin receptors recognizing collagen type I have been shown to regulate early osteoblast differentiation and control the expression of key genes in osteoblastogenesis [43,44]. We have observed that maturation of osteoblasts on microtextured biomaterial surfaces are dependent on signaling by α2β1 [52] and that expression of β1 is regulated by 1α,25(OH)2D3 [53,54]. This suggests that α2β1 expression may play a similar role in EB differentiation.
Conclusion
Taken together, our results demonstrate for the first time that 1α,25(OH)2D3 causes rapid activation of PKC in ESCs and this activation increases during osteogenic differentiation. In addition, 1α,25(OH)2D3 also induced PKC activation in adult stem cells. The two receptors for this vitamin D metabolite are differentially expressed during osteoblastic differentiation, with increased Vdr expression in osteogenic medium. These results correlate with an increase in the expression of genes containing VDREs. Although there is a decrease in PDIA3 in EBs cultured in osteogenic medium, PKC activity in these cells is sensitive to 1α,25(OH)2D3 demonstrating that the receptor is still functional. These data indicate the important role of 1α,25(OH)2D3 signaling in osteogenic differentiation of embryonic and MSCs.
Acknowledgments
This research was funded by a grant from Children's Healthcare of Atlanta, Atlanta, GA. Additional support was provided by a gift from Northrup Grumman. KS also received support from the Emory Medical Scientist Training Program grant T32 GM008169.
Author Disclosure Statement
The authors have no commercial associations that may create a conflict of interest with this manuscript.
References
- 1.Thomson JA. Itskovitz-Eldor J. Shapiro SS. Waknitz MA. Swiergiel JJ. Marshall VS. Jones JM. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–1147. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 2.Martin GR. Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc Natl Acad Sci U S A. 1981;78:7634–7638. doi: 10.1073/pnas.78.12.7634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans MJ. Kaufman MH. Establishment in culture of pluripotential cells from mouse embryos. Nature. 1981;292:154–156. doi: 10.1038/292154a0. [DOI] [PubMed] [Google Scholar]
- 4.Nelson TJ. Martinez-Fernandez A. Terzic A. Induced pluripotent stem cells: developmental biology to regenerative medicine. Nat Rev Cardiol. 2010;7:700–710. doi: 10.1038/nrcardio.2010.159. [DOI] [PubMed] [Google Scholar]
- 5.Kitagawa M. Era T. Differentiation of mesodermal cells from pluripotent stem cells. Int J Hematol. 2010;91:373–383. doi: 10.1007/s12185-010-0518-8. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S. Leschansky L. Zussman E. Burman M. Srouji S. Abramov N. Itskovitz-Eldor J. Repair of full-thickness tendon injury using connective tissue progenitors efficiently derived from human embryonic stem cells and fetal tissues. Tissue Eng Part A. 2010;16:3119–3137. doi: 10.1089/ten.TEA.2009.0716. [DOI] [PubMed] [Google Scholar]
- 7.Kong CW. Akar FG. Li RA. Translational potential of human embryonic and induced pluripotent stem cells for myocardial repair: Insights from experimental models. Thromb Haemost. 2010;104:30–38. doi: 10.1160/TH10-03-0189. [DOI] [PubMed] [Google Scholar]
- 8.Kane NM. Meloni M. Spencer HL. Craig MA. Strehl R. Milligan G. Houslay MD. Mountford JC. Emanueli C. Baker AH. Derivation of endothelial cells from human embryonic stem cells by directed differentiation: analysis of microRNA and angiogenesis in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2010;30:1389–1397. doi: 10.1161/ATVBAHA.110.204800. [DOI] [PubMed] [Google Scholar]
- 9.Lee H. Shamy GA. Elkabetz Y. Schofield CM. Harrsion NL. Panagiotakos G. Socci ND. Tabar V. Studer L. Directed differentiation and transplantation of human embryonic stem cell-derived motoneurons. Stem Cells. 2007;25:1931–1939. doi: 10.1634/stemcells.2007-0097. [DOI] [PubMed] [Google Scholar]
- 10.Doetschman TC. Eistetter H. Katz M. Schmidt W. Kemler R. The in vitro development of blastocyst-derived embryonic stem cell lines: formation of visceral yolk sac, blood islands and myocardium. J Embryol Exp Morphol. 1985;87:27–45. [PubMed] [Google Scholar]
- 11.Doevendans PA. Kubalak SW. An RH. Becker DK. Chien KR. Kass RS. Differentiation of cardiomyocytes in floating embryoid bodies is comparable to fetal cardiomyocytes. J Mol Cell Cardiol. 2000;32:839–851. doi: 10.1006/jmcc.2000.1128. [DOI] [PubMed] [Google Scholar]
- 12.Hopfl G. Gassmann M. Desbaillets I. Differentiating embryonic stem cells into embryoid bodies. Methods Mol Biol. 2004;254:79–98. doi: 10.1385/1-59259-741-6:079. [DOI] [PubMed] [Google Scholar]
- 13.Sargent CY. Berguig GY. Kinney MA. Hiatt LA. Carpenedo RL. Berson RE. McDevitt TC. Hydrodynamic modulation of embryonic stem cell differentiation by rotary orbital suspension culture. Biotechnol Bioeng. 2010;105:611–626. doi: 10.1002/bit.22578. [DOI] [PubMed] [Google Scholar]
- 14.Coucouvanis E. Martin GR. Signals for death and survival: a two-step mechanism for cavitation in the vertebrate embryo. Cell. 1995;83:279–287. doi: 10.1016/0092-8674(95)90169-8. [DOI] [PubMed] [Google Scholar]
- 15.Keller GM. In vitro differentiation of embryonic stem cells. Curr Opin Cell Biol. 1995;7:862–869. doi: 10.1016/0955-0674(95)80071-9. [DOI] [PubMed] [Google Scholar]
- 16.Conley BJ. Young JC. Trounson AO. Mollard R. Derivation, propagation and differentiation of human embryonic stem cells. Int J Biochem Cell Biol. 2004;36:555–567. doi: 10.1016/j.biocel.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Bratt-Leal AM. Carpenedo RL. McDevitt TC. Engineering the embryoid body microenvironment to direct embryonic stem cell differentiation. Biotechnol Prog. 2009;25:43–51. doi: 10.1002/btpr.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurosawa H. Methods for inducing embryoid body formation: in vitro differentiation system of embryonic stem cells. J Biosci Bioeng. 2007;103:389–398. doi: 10.1263/jbb.103.389. [DOI] [PubMed] [Google Scholar]
- 19.Augello A. Kurth TB. De Bari C. Mesenchymal stem cells: a perspective from in vitro cultures to in vivo migration and niches. Eur Cell Mater. 2010;20:121–133. doi: 10.22203/ecm.v020a11. [DOI] [PubMed] [Google Scholar]
- 20.Furedi-Milhofer H. Moradian-Oldak J. Weiner S. Veis A. Mintz KP. Addadi L. Interactions of matrix proteins from mineralized tissues with octacalcium phosphate. Connect Tissue Res. 1994;30:251–264. doi: 10.3109/03008209409015041. [DOI] [PubMed] [Google Scholar]
- 21.Golub EE. Boesze-Battaglia K. The role of alkaline phosphatase in mineralization. Curr Opin Orthop. 2007;18:444–448. [Google Scholar]
- 22.Porter RM. Huckle WR. Goldstein AS. Effect of dexamethasone withdrawal on osteoblastic differentiation of bone marrow stromal cells. J Cell Biochem. 2003;90:13–22. doi: 10.1002/jcb.10592. [DOI] [PubMed] [Google Scholar]
- 23.Castano-Izquierdo H. Alvarez-Barreto J. van den Dolder J. Jansen JA. Mikos AG. Sikavitsas VI. Pre-culture period of mesenchymal stem cells in osteogenic media influences their in vivo bone forming potential. J Biomed Mater Res A. 2007;82:129–138. doi: 10.1002/jbm.a.31082. [DOI] [PubMed] [Google Scholar]
- 24.Heng BC. Cao T. Stanton LW. Robson P. Olsen B. Strategies for directing the differentiation of stem cells into the osteogenic lineage in vitro. J Bone Miner Res. 2004;19:1379–1394. doi: 10.1359/JBMR.040714. [DOI] [PubMed] [Google Scholar]
- 25.van Leeuwen JP. van Driel M. van den Bemd GJ. Pols HA. Vitamin D control of osteoblast function and bone extracellular matrix mineralization. Crit Rev Eukaryot Gene Expr. 2001;11:199–226. [PubMed] [Google Scholar]
- 26.Kuske B. Savkovic V. zur Nieden NI. Improved media compositions for the differentiation of embryonic stem cells into osteoblasts and chondrocytes. Methods Mol Biol. 2011;690:195–215. doi: 10.1007/978-1-60761-962-8_14. [DOI] [PubMed] [Google Scholar]
- 27.St-Arnaud R. The direct role of vitamin D on bone homeostasis. Arch Biochem Biophys. 2008;473:225–230. doi: 10.1016/j.abb.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 28.Jurutka PW. Bartik L. Whitfield GK. Mathern DR. Barthel TK. Gurevich M. Hsieh JC. Kaczmarska M. Haussler CA. Haussler MR. Vitamin D receptor: key roles in bone mineral pathophysiology, molecular mechanism of action, and novel nutritional ligands. J Bone Miner Res. 2007;22(Suppl 2):V2–V10. doi: 10.1359/jbmr.07s216. [DOI] [PubMed] [Google Scholar]
- 29.Paredes R. Arriagada G. Cruzat F. Villagra A. Olate J. Zaidi K. van Wijnen A. Lian JB. Stein GS. Stein JL. Montecino M. Bone-specific transcription factor Runx2 interacts with the 1alpha,25-dihydroxyvitamin D3 receptor to up-regulate rat osteocalcin gene expression in osteoblastic cells. Mol Cell Biol. 2004;24:8847–8861. doi: 10.1128/MCB.24.20.8847-8861.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khanal RC. Nemere I. The ERp57/GRp58/1,25D3-MARRS receptor: multiple functional roles in diverse cell systems. Curr Med Chem. 2007;14:1087–1093. doi: 10.2174/092986707780362871. [DOI] [PubMed] [Google Scholar]
- 31.Boyan BD. Wang L. Wong KL. Jo H. Schwartz Z. Plasma membrane requirements for 1alpha,25(OH)2D3 dependent PKC signaling in chondrocytes and osteoblasts. Steroids. 2006;71:286–290. doi: 10.1016/j.steroids.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 32.Zanello LP. Norman A. 1alpha,25(OH)2 vitamin D3 actions on ion channels in osteoblasts. Steroids. 2006;71:291–297. doi: 10.1016/j.steroids.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 33.Breen EC. van Wijnen AJ. Lian JB. Stein GS. Stein JL. In vivo occupancy of the vitamin D responsive element in the osteocalcin gene supports vitamin D-dependent transcriptional upregulation in intact cells. Proc Natl Acad Sci U S A. 1994;91:12902–12906. doi: 10.1073/pnas.91.26.12902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kraichely DM. MacDonald PN. Transcriptional activation through the vitamin D receptor in osteoblasts. Front Biosci. 1998;3:d821–d833. doi: 10.2741/a325. [DOI] [PubMed] [Google Scholar]
- 35.Zanello LP. Norman AW. Electrical responses to 1alpha,25(OH)2-Vitamin D3 and their physiological significance in osteoblasts. Steroids. 2004;69:561–565. doi: 10.1016/j.steroids.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 36.Baran DT. Nongenomic actions of the steroid hormone 1 alpha,25-dihydroxyvitamin D3. J Cell Biochem. 1994;56:303–306. doi: 10.1002/jcb.240560305. [DOI] [PubMed] [Google Scholar]
- 37.Wali RK. Kong J. Sitrin MD. Bissonnette M. Li YC. Vitamin D receptor is not required for the rapid actions of 1,25-dihydroxyvitamin D3 to increase intracellular calcium and activate protein kinase C in mouse osteoblasts. J Cell Biochem. 2003;88:794–801. doi: 10.1002/jcb.10432. [DOI] [PubMed] [Google Scholar]
- 38.Schwartz Z. Dennis R. Bonewald L. Swain L. Gomez R. Boyan BD. Differential regulation of prostaglandin E2 synthesis and phospholipase A2 activity by 1,25-(OH)2D3 in three osteoblast-like cell lines (MC-3T3-E1, ROS 17/2.8, and MG-63) Bone. 1992;13:51–58. doi: 10.1016/8756-3282(92)90361-y. [DOI] [PubMed] [Google Scholar]
- 39.Chen J. Olivares-Navarrete R. Wang Y. Herman TR. Boyan BD. Schwartz Z. Protein-disulfide isomerase-associated 3 (Pdia3) mediates the membrane response to 1,25-dihydroxyvitamin D3 in osteoblasts. J Biol Chem. 2010;285:37041–37050. doi: 10.1074/jbc.M110.157115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carpenedo RL. Sargent CY. McDevitt TC. Rotary suspension culture enhances the efficiency, yield, and homogeneity of embryoid body differentiation. Stem Cells. 2007;25:2224–2234. doi: 10.1634/stemcells.2006-0523. [DOI] [PubMed] [Google Scholar]
- 41.Takahashi N. Maeda K. Ishihara A. Uehara S. Kobayashi Y. Regulatory mechanism of osteoclastogenesis by RANKL and Wnt signals. Front Biosci. 2011;16:21–30. doi: 10.2741/3673. [DOI] [PubMed] [Google Scholar]
- 42.van den Bemd GJ. Jhamai M. Staal A. van Wijnen AJ. Lian JB. Stein GS. Pols HA. van Leeuwen JP. A central dinucleotide within vitamin D response elements modulates DNA binding and transactivation by the vitamin D receptor in cellular response to natural and synthetic ligands. J Biol Chem. 2002;277:14539–14546. doi: 10.1074/jbc.M111224200. [DOI] [PubMed] [Google Scholar]
- 43.Jikko A. Harris SE. Chen D. Mendrick DL. Damsky CH. Collagen integrin receptors regulate early osteoblast differentiation induced by BMP-2. J Bone Miner Res. 1999;14:1075–1083. doi: 10.1359/jbmr.1999.14.7.1075. [DOI] [PubMed] [Google Scholar]
- 44.Xiao G. Wang D. Benson MD. Karsenty G. Franceschi RT. Role of the alpha2-integrin in osteoblast-specific gene expression and activation of the Osf2 transcription factor. J Biol Chem. 1998;273:32988–32994. doi: 10.1074/jbc.273.49.32988. [DOI] [PubMed] [Google Scholar]
- 45.zur Nieden NI. Kempka G. Ahr HJ. In vitro differentiation of embryonic stem cells into mineralized osteoblasts. Differentiation. 2003;71:18–27. doi: 10.1046/j.1432-0436.2003.700602.x. [DOI] [PubMed] [Google Scholar]
- 46.Martin JY. Dean DD. Cochran DL. Simpson J. Boyan BD. Schwartz Z. Proliferation, differentiation, and protein synthesis of human osteoblast-like cells (MG63) cultured on previously used titanium surfaces. Clin Oral Implants Res. 1996;7:27–37. doi: 10.1034/j.1600-0501.1996.070104.x. [DOI] [PubMed] [Google Scholar]
- 47.zur Nieden NI. Kempka G. Ahr HJ. In vitro differentiation of embryonic stem cells into mineralized osteoblasts. Differentiation. 2003;71:18–27. doi: 10.1046/j.1432-0436.2003.700602.x. [DOI] [PubMed] [Google Scholar]
- 48.Kato S. Takeyama K. Kitanaka S. Murayama A. Sekine K. Yoshizawa T. In vivo function of VDR in gene expression-VDR knock-out mice. J Steroid Biochem Mol Biol. 1999;69:247–251. doi: 10.1016/s0960-0760(99)00042-4. [DOI] [PubMed] [Google Scholar]
- 49.Lee CS. Chen J. Wang Y. Williams JK. Ranly DM. Schwartz Z. Boyan BD. Coordinated tether formation in anatomically distinct mice growth centers is dependent on a functional vitamin D receptor and is tightly linked to three-dimensional tissue morphology. Bone. 2011;49:419–427. doi: 10.1016/j.bone.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 50.Tunsophon S. Nemere I. Protein kinase C isotypes in signal transduction for the 1,25D3-MARRS receptor (ERp57/PDIA3) in steroid hormone-stimulated phosphate uptake. Steroids. 2010;75:307–313. doi: 10.1016/j.steroids.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 51.Wang Y. Chen J. Lee CS. Nizkorodov A. Riemenschneider K. Martin D. Hyzy S. Schwartz Z. Boyan BD. Disruption of Pdia3 gene results in bone abnormality and affects 1alpha,25-dihydroxy-vitamin D3-induced rapid activation of PKC. J Steroid Biochem Mol Biol. 2010;121:257–260. doi: 10.1016/j.jsbmb.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 52.Olivares-Navarrete R. Raz P. Zhao G. Chen J. Wieland M. Cochran DL. Chaudhri RA. Ornoy A. Boyan BD. Schwartz Z. Integrin alpha2beta1 plays a critical role in osteoblast response to micron-scale surface structure and surface energy of titanium substrates. Proc Natl Acad Sci U S A. 2008;105:15767–15772. doi: 10.1073/pnas.0805420105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schwartz Z. Bell BF. Wang L. Zhao G. Olivares-Navarrete R. Boyan BD. Beta-1 integrins mediate substrate dependent effects of 1alpha,25(OH)2D3 on osteoblasts. J Steroid Biochem Mol Biol. 2007;103:606–609. doi: 10.1016/j.jsbmb.2006.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang L. Zhao G. Olivares-Navarrete R. Bell BF. Wieland M. Cochran DL. Schwartz Z. Boyan BD. Integrin beta1 silencing in osteoblasts alters substrate-dependent responses to 1,25-dihydroxy vitamin D3. Biomaterials. 2006;27:3716–3725. doi: 10.1016/j.biomaterials.2006.02.022. [DOI] [PubMed] [Google Scholar]