Abstract
Purpose. To examine the relationship between diet, physical activity, and obesity in Indigenous youths from northern Australia. Methods. In a cross-sectional study, physical activity and dietary intake (“short nutrition questionnaire”) were assessed among all youths during a face-to-face interview. For 92 high school youths, additional dietary information was assessed using a food-frequency questionnaire. Height and weight were measured and BMI was calculated. Multiple logistic regression was used to assess associations. Results. Of the 277 youths included, 52% had ≤2 servings of fruit and 84% had <4 servings of vegetables per day; 65% ate fish and 27%, take-away food (“fast food”) at least twice a week. One in four ate local traditional sea food including turtle and dugong (a local sea mammal) at least twice a week. Overweight/obese youths engaged in fewer days of physical activity in the previous week than normal weight youths (OR = 2.52, 95% CI 1.43–4.40), though patterns of physical activity differed by sex and age (P < 0.001). Overweight/obese youths were 1.89 times (95% CI 1.07–3.35) more likely to eat dugong regularly than nonobese youths. Analysis of food-frequency data showed no difference by weight assessment among high-school students. Conclusions. Low fruit and vegetable intake were identified in these Indigenous youths. Regular consumption of fried dugong and low frequency of physical activity were associated with overweight/obesity reinforcing the need to devise culturally appropriate health promotion strategies and interventions for Indigenous youths aimed at improving their diet and increasing their physical activity.
1. Background
Worldwide, the prevalence of obesity amongst minority groups has increased steeply over the past decades [1–3]. This is particularly so for previously traditional societies such as the American Indians [4, 5], Alaska Natives [5], Canadian Inuits [6], Papua New Guineans, Pacific Island nations [7, 8], and Aboriginal and Torres Strait Islander people (referred to as Indigenous Australians) [9]. In the remote Torres Strait region, in the far north of Australia (Figure 1), 51% of the population is classified as obese [10]. The prevalence of childhood overweight and obesity in Indigenous youths residing in this region is also very high (46%). A high proportion of children show signs of obesity-associated metabolic complications such as the metabolic syndrome (17%), acanthosis nigricans (41%), and hypertension (27%) [11].
Figure 1.
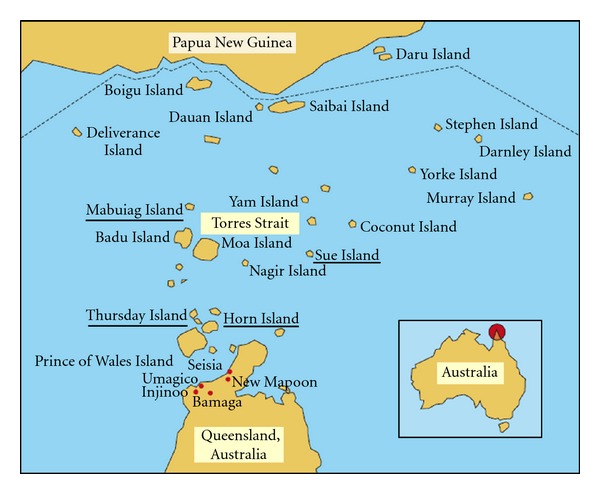
Map of the Torres Strait regions of Australia [10].
Limited data on food intake patterns and physical activity among Australian children are available. In a national survey, the food intake patterns of adolescents (mostly non-Indigenous) differed by sex with females reporting higher fruit intake and males consuming more soft drinks [12]. Reports from a school-based study [13] also showed sex and regional differences in the patterns of food intake of adolescents: those living in the nonmetropolitan areas reported higher vegetable consumption and lower consumption of fast foods than those from the metropolitan region, and females had food patterns that were more closely aligned with the Australian Guide for Healthy Eating (AGHE) [14] than males.
Sex and age differences in the patterns of physical activity have also been reported. The number of days school-aged children engage in physical activity decreased with age. Also, the number of days children engaged in physical activity was higher for boys than girls [15]. Participation in organised sports was also higher for boys aged 12–14 year (74%) than girls (55%) [16].
In national health surveys, fruit and vegetable consumption was lower for Indigenous Australians aged ≥12 years living in remote areas compared to Indigenous people in nonremote areas. Indigenous and non-Indigenous people residing in nonremote areas reported a similar vegetable intake; Indigenous people reported eating less fruit, [17] and were more likely to be sedentary [18] than other Australians in remote areas. For example, among people aged 18–34 years, 60–71% of non-Indigenous people reported low levels of exercise or were sedentary compared to 69–80% of Indigenous people [18, 19].
Torres Strait Islander residents are renowned as high consumers of seafood such as fish, marine turtles, dugong (a local sea mammal), and shellfish [20], with customary (subsistence) and commercial fishing [20] playing an important role in the region's local economy (http://www.tsra.gov.au/the-torres-strait/community-profiles.aspx). Dugong and turtle have energy content similar to baked/grilled fish. Dugong can be fried or cooked slowly (meat and fat), and when it is fried its energy content is similar to fried fish obtained from “fast-food” outlets.
Our initial report on 327 school-age Indigenous youths (5–17 years) residing in the Torres Strait region focused on the prevalence of obesity, the metabolic syndrome (as defined by the International Diabetes Federation) [21], and type 2 diabetes mellitus [11]. This paper investigates the differences in usual diet (including some traditional foods that are a large part of the local diet) and physical activity patterns between overweight or obese and normal weight Indigenous youths. This paper also examines the relationship between these factors and obesity in this group.
2. Methods
2.1. Subjects
The Torres Strait region comprises approximately 150 islands with 15 Indigenous communities. The cross-sectional study took place on 4 island communities: Thursday Island, Horn Island, Sue Island, and Mabuiag Island. Further details of the study have been previously described [22]. Briefly, the study was conducted in this region from April to September, 2003, in conjunction with a general health-screen program initiated by the local health district. Some schools also took part in the screening program at that time and were included in the study. All Indigenous and non-Indigenous youths with ages ranging between 5 and 17 years who attended one of the 5 schools on these 4 islands were eligible. Of the 1050 eligible youths enrolled across the five selected schools, 327 participated in the study (31%). Eighteen non-Indigenous youths and 32 youths with missing information on key variables were excluded (277 were included in the analysis). Participation rates varied by community: Thursday Island 29%, Horn Island 25%, Mabuiag Island 96%, and Sue Island 100%. On Thursday Island, there were 114 eligible high school adolescents attending school and of these 68 were classified as boarders. Boarders live in residential colleges near to the school on Thursday Island during the school calendar year while their families resided in one of the outer islands. The students return to their family home during the school holidays. The overall participation rate for outer island adolescents was 97%.
2.2. Study Measurements
Measurements included height, weight, and waist circumference (standardisation of these measurements have been described elsewhere) [22]. The majority of the data was collected by a nutritionist of Aboriginal descent (AM) and on the occasions by an Indigenous health worker. All youth took part in a structured face-to-face interview with AM and completed a dietary questionnaire (“short nutrition questionnaire”). Among ninety-two high school adolescents, a food frequency questionnaire (FFQ) was used to obtain additional information.
2.2.1. Short Nutrition Questionnaire
Questions were based on a validated Australian National Nutrition Survey [23, 24] with slight modification to enable data to be collected about youths on the consumption of turtle and dugong—commonly consumed marine mammals by the Indigenous population. Possible responses to the questions on fruit and vegetables were “do not eat”, “1 serving or less”, “2 to 3 servings”, “4 to 5 servings,” and “6 servings or more” (per day). Due to very small numbers in the lowest and highest group, we recategorized the responses as: “do not eat or 1 serving or less,” “2 to 3 servings,” and “4 servings or more”. Possible responses to questions on “takeaway” food (fast food), consumption of turtle, dugong and fish (“never eat”, “1 time per week”, “2 to 3 times”, “4 to 5 times,” to “6 or more times”) were also recategorised. There were also questions on types of milk, bread, bread/cracker spread, cooking oils, and breakfast cereal consumed by participants.
2.2.2. Food Frequency Questionnaire
A 108-item FFQ was completed under the supervision of a nutritionist by 92 (81%) high school adolescents to obtain additional information on frequency of consumption of food items listed on the FFQ in the past 12 months. Each food item had a response option of nine frequency categories ranging from “never” or “less than once a month” to “4+ times a day.” A slightly modified version of the 1995 Australian National Nutrition Survey (NNS) FFQ was used in this study. The modification involved excluding a list of vitamin and mineral supplements considered irrelevant to our study. The 1995 NNS FFQ was a modified version of an existing validated questionnaire developed for use in Australian populations with additional foods included [25]. The NNS FFQ was piloted and pretested before administration [26], and had been previously used to collect dietary information from respondents aged 12 years and over in Australia [27]. Participants in the 1995 NNS had provided 24-hour recall data that constituted the primary source of dietary data for that survey; however, for this study, 24-hour recall data was not collected.
We categorized food items on the FFQ into five food groups (dairy, fruit, bread and cereal, meat, vegetables) and an “energy-dense” food group according to the definitions of the Australian Guide to Healthy Eating [14]. Energy-dense foods are generally high in sugar and fats and are not meant to be consumed daily. Daily consumption of foods from each of the five food groups as defined by the AGHE was assessed using a similar method to the one reported by Savige et al. [13]. To assess the proportion of children consuming foods from the five food groups daily, the response options on the FFQ were converted to frequency per day as follows: never = 0.00 times per day; <1 per month = 0.02 times per day; 1–3 times per month = 0.07 times per day; 1 per week = 0.14 times per day; 2–4 times per week = 0.43 times per day; 5–6 times per week = 0.79 times per day; 1 per day = 1.0; 2–3 times per day = 2.5 times per day; 4+ per day = 4 times per day. To obtain a daily intake for each food group, we added up the number of times each of the items was consumed (components of each group are shown in Table 6) [13]. The summed daily frequencies were then recategorized using the following arbitrary cut-points: 0–0.14 times per day = “never/rarely consumed”, >0.14–1.0 = “consumed 1–6 times a week or most days”, and >1.0 = “consumed at least daily” to allow comparison with results of other studies on food intake pattern in Australian adolescents [13].
Table 6.
| Food groups | Items making up food groups |
|---|---|
| Dairy group | Flavoured milk, milk as a drink, milk added to cereal, milk added to hot beverage, that is, tea, yoghurt, cottage cheese, cheddar cheese |
| Fruit group—includes fresh, frozen, canned, dried fruits, and juices | Mixed fruit, apple, orange, peach, banana, mango, pineapple, berries, other fruits, that is, frozen, canned fruits, dried fruit, fruit juice |
| Bread and cereal group | White bread and wholemeal breads, muesli, porridge, cold breakfast cereals, rice, pasta, and noodles |
| Meat group and meat substitute group (excludes processed meats) | Mince, mixed beef/veal/lamb/pork dishes, liver, offal, chicken, canned fish, steamed fish, fried fish, seafood, eggs, pulses, and soybean |
| Vegetable group —includes potatoes | Green vegetables, stir-fry vegetables, potatoes, carrots, sweet potato, peas, beans, silver beet, salad greens, celery, broccoli, cauliflower, sprouts, pumpkin, zucchini, capsicum, tomatoes, tomato paste, avocado, onion, corn, mushroom |
| Energy dense foods and beverages —all foods that do not fit into the above 5 groups | cream, ice cream, muffin, biscuits, sausages, bacon, ham, luncheon, meat pie, pizza, hamburger, cakes, sweet pies, sweet puddings, plain biscuits, fancy biscuits, chocolate, other confectioneries, chips/crisps, sugar, jam, peanut butter, butter, mayonnaise, cordial, soft drinks, electrolyte, energy drinks, beer, wine, sherry, spirits, other alcohols, bread spreads |
| Water | Water including tea and coffee |
We formed four subgroups from the “energy-dense” foods, namely, high-energy drinks, sweet-snacks, savoury-snacks, and “takeaway” style food; and three “low-energy” food groups comprising all types of fruit including fruit juices, green leafy, orange, and cruciferous vegetables, and “other” vegetables (Table 4) to assess the association between daily frequency of intake of these foods and weight assessment status. These sub-groups were categorised using a similar method to the one reported by Savige et al. [13] who reported on food intake patterns of Australian adolescents.
Table 4.
Proportion of high-school adolescents who consumed food from each of the selected food groups (n = 92 adolescents who answered the FFQ).
| Normal weight (n = 47) n (%) | Overweight or obese (n = 45) n (%) | Total (n = 92) n (%) | Overall P-value* | |
|---|---|---|---|---|
| Energy-dense food group | ||||
| High energy drinksa | ||||
| Never/rarely consumed | 1 (2) | 1 (2) | 2 (2) | 0.643 |
| Consumed 1 to 6 times a week | 22 (47) | 16 (36) | 38 (41) | |
| Consumed at least daily | 24 (51) | 28 (62) | 52 (57) | |
| Sweet snacksb | ||||
| Never/rarely consumed | 0 (0) | 0 (0) | 0 (0) | 0.609 |
| Consumed 1 to 6 times a week | 11 (23) | 8 (18) | 19 (21) | |
| Consumed at least daily | 36 (77) | 37 (82) | 73 (79) | |
| Savoury snacksc | ||||
| Never/rarely consumed | 3 (6) | 5 (11) | 8 (8) | 0.680 |
| Consumed 1 to 6 times a week | 31 (66) | 30 (67) | 61 (66) | |
| Consumed at least daily | 13 (28 | 10 (22) | 23 (25) | |
| Takeaway-style foodsd (e.g., pasties, meat pies, sausage rolls, pizza) | ||||
| Never/rarely consumed | 5 (11) | 9 (20) | 14 (15) | 0.162 |
| Consumed 1 to 6 times a week | 29 (62) | 30 (67) | 59 (64) | |
| Consumed at least daily | 13 (28) | 6 (13) | 19 (21) | |
| Low-energy food group | ||||
| Fruite | ||||
| Never/rarely consumed | 0 (0) | 1 (2) | 1 (1) | 0.607 |
| Consumed 1 to 6 times a week | 4 (9) | 5 (11) | 9 (10) | |
| Consumed at least daily | 43 (91) | 39 (87) | 82 (89) | |
| Green leafy, orange, and cruciferous vegetablesf | ||||
| Never/rarely consumed | 2 (4) | 2 (4) | 4 (4) | 0.900 |
| Consumed 1 to 6 times a week | 6 (13) | 4 (9) | 10 (11) | |
| Consumed at least daily | 39 (83) | 39 (87) | 78 (85) | |
| Other vegetablesg | ||||
| Never/rarely consumed | 1 (2) | 2 (4) | 3 (3) | 0.642 |
| Consumed 1 to 6 times a week | 9 (19) | 11 (24) | 20 (22) | |
| Consumed at least daily | 37 (79) | 32 (71) | 69 (75) | |
*P value from Fishers Exact test (two-tailed) as expected value in some cells are less than 5.
aEnergy drinks include cordial, soft drinks, electrolyte or sport drinks, and other high energy drinks, for example, Redbull.
bSweet snacks include cakes, sweet pies, sweet puddings, sweet plain biscuits, sweet fancy biscuits, chocolates, other confectioneries, sugar, and jam.
cSavoury snacks include nuts potato or corn chips/crisps, savoury biscuits, crisp bread, or crackers.
dTakeaway (fast food) style foods include meat pies, sausage rolls, pizza, hamburgers, other takeaway (fast food) style foods.
eFruit group include mixed fruit, apple, orange, peach, banana, mango, pineapple, berries, other fruit, dried fruit, and fruit juice.
fGreen leafy, orange, and cruciferous vegetables group include spinach, silverbeet, stir-fry vegetables, carrots, sweet potato, salad greens, broccoli, cauliflower, tomatoes, pumpkin, and green leafy vegetables.
gOther vegetables include potatoes, peas, beans, celery, sprouts, zucchini, capsicum, avocado, onion, corn, and mushroom.
2.3. Physical Activity
All youths were asked about their frequency of physical activity (“How many days did you do physical activity in the last week”) [22]. When they were not sure about the question asked, the interviewer (AM) further explained by asking the children how many days of the past seven days had they engaged in physical activity or active play that raised their heart rate or caused them to “huff and puff”.
2.4. Statistical Analysis
Overweight and obesity were defined by using body mass index (BMI = weight(kg)/height(m)2) and Cole et al.'s [28] childhood-equivalent cut-points (age and sex adjusted) to an adult BMI of 25 (overweight) and 30 (obese), respectively (BMI smaller than these cut-points was classified as “normal weight”). Age and sex-specific cut-points [29] were used to classify central obesity (waist circumference).
The Statistical Package for the Social Sciences version 17.0 (SPSS, Chicago, Ill) and SAS version 9.1 (SAS Institute, Cary, NC) were used for data analysis. Statistical significance was set at α = 0.05. Proportions and chi-squared test were used to compare categorical variables. Fisher's exact test was used when cell count was <5. Analyses of the “short nutrition questionnaire” and FFQ were conducted separately. A multiple logistic regression model (odds ratios, 95% confidence intervals) adjusting for age, sex, physical activity, and boarding status (boarder versus non-boarder) assessed the associations between being overweight/obese (dependent variable) and consumption of each of the selected food groups. A second model assessed the association between being overweight/obese and physical activity.
The study hypothesis was that frequency of physical activity and food consumption amongst normal weight youth was significantly different to that of overweight/obese youths. Estimated power for two-sample comparisons of proportions was calculated using Stata/IC 11.2 for Windows. The null hypothesis was that there is no difference in the proportion of youths reporting frequency of physical activity (or food consumption) between normal weight compared to overweight/obese youths. Assuming α = 0.05, sample sizes n1 = 150, and n2 = 127, the statistical power of the study to detect statistically significant differences was greater for the evaluation of differences in physical activity between the two groups (82% power to detect 61% versus 43%) when compared to the evaluation of food consumption (46% power to detect 55% versus 43%, and 28% power to detect 23% versus 31%).
The study, conducted in accordance with the Declaration of Helsinki, was approved by the Queensland Institute of Medical Research Human Ethics Committee, the local Health Council, Health Service District, and Regional Education Committee.
3. Results
Analysis included 277 Indigenous youths (Table 1). The mean age was 11.2 years (SD = 3.1) and 184 youths resided in the inner Torres Strait Islands (Thursday Island and nearby islands). Almost half of the youths (46%) were overweight/obese and 35% had central obesity. Compared to males, more females had central obesity (50% versus 18%, P < 0.001) or were classified as overweight/obese (51% versus 40%, P = 0.063), although the BMI comparison was not significant.
Table 1.
Characteristics of whole study population.
| Primary schools (n = 163) n (%) | High school (n = 114) n (%) | Total (n = 277) n (%) | P value | |
|---|---|---|---|---|
| Sex | ||||
| Male | 68 (42) | 60 (53) | 128 (46) | 0.073 |
| Female | 95 (58) | 54 (47) | 149 (54) | |
| BMIa | ||||
| Normal | 90 (55) | 60 (53) | 150 (54) | 0.871 |
| Overweight | 44 (27) | 34 (30) | 78 (28) | |
| Obese | 29 (18) | 20 (18) | 49 (18) | |
| Increased waist circumferenceb | 46 (28) | 51 (45) | 97 (35) | 0.004 |
aBody mass index (BMI) = weight (kg)/height (m)2; Cole et al.'s [28] childhood-equivalent cut-points to an adult BMI of 25 and 30 were used to categorise BMI;
bMissing information for 1 youth; age and sex-specific cut-points as described by Jolliffe and Janssen [29] were used to classify central obesity (large waist circumference).
3.1. Short Nutrition Questionnaire
Overall, 52% of participants had ≤2 servings of fruit daily and 83% did not have 4 servings of vegetables daily. Fish, turtle, dugong, and takeaway foods were eaten at least twice a week by 65%, 27%, 26%, and 27% of youths, respectively (Table 2). Most youths usually consumed whole milk, white bread, soft drinks with added sugar, and breakfast cereal without added sugar. No significant differences in the pattern of food consumption by weight assessment or sex were seen.
Table 2.
Selected food frequency (“short nutrition questionnaire”) and physical activity by weight assessment for the whole study population.
| Normal weight (n = 150) n (%) | Overweight or obese (n = 127) n (%) | Total (n = 277) n (%) | P-value | |
|---|---|---|---|---|
| How many servings of…. do you usually eat each day? | ||||
| Fruita | ||||
| 1 servings/day or less | 75 (50) | 68 (54) | 143 (52) | 0.631 |
| 2-3 servings/day | 46 (31) | 39 (31) | 85 (31) | |
| 4+ servings/day | 29 (19) | 19 (15) | 48 (17) | |
| Vegetablesa | ||||
| 1 servings/day or less | 83 (55) | 54 (43) | 137 (49) | 0.070 |
| 2-3 servings/day | 43 (29) | 52 (41) | 95 (34) | |
| 4+ servings/day | 24 (16) | 20 (16) | 44 (16) | |
| Takeaway foodsa | ||||
| never eat | 11 (7) | 15 (12) | 26 (9) | 0.356 |
| 1/week or less | 99 (66) | 83 (66) | 182 (66) | |
| 2+ times/week | 40 (27) | 28 (22) | 68 (25) | |
| Turtleb | ||||
| never eat | 24 (16) | 22 (18) | 46 (17) | 0.323 |
| 1/week or less | 90 (60) | 63 (51) | 153 (56) | |
| 2+ times/week | 36 (24) | 38 (31) | 74 (27) | |
| Dugongc | ||||
| never eat | 29 (19) | 25 (20) | 54 (20) | 0.228 |
| 1/week or less | 87 (58) | 61 (49) | 148 (54) | |
| 2+ times/week | 34 (23) | 39 (31) | 73 (27) | |
| Fisha | ||||
| 1/week or less | 52 (35) | 45 (36) | 97 (35) | 0.228 |
| 2-3/week | 49 (33) | 41 (33) | 90 (33) | |
| 4+ times/week | 49 (33) | 40 (32) | 89 (32) | |
| Milkd | ||||
| Whole milk | 134 (94) | 110 (94) | 244 (94) | 0.434 |
| Low/reduced fat | 5 (4) | 6 (5) | 11 (4) | |
| Other | 4 (3) | 1 (1) | 5 (2) | |
| Bread | ||||
| White bread | 141 (94) | 113 (89) | 254 (92) | 0.163 |
| Wholemeal, grain | 9 (6) | 12 (9) | 21 (7) | |
| Do not eat bread | 0— | 2 (2) | 2 (1) | |
| Spread | ||||
| Butters | 74 (50) | 70 (55) | 144 (52) | 0.564 |
| Margarine | 71 (47) | 52 (41) | 123 (44) | |
| Do not use dairy/margarine spread | 5 (3) | 5 (4) | 10 (4) | |
| Cooking oile | ||||
| Monosaturated oils | 56 (44) | 54 (49) | 110 (47) | 0.475 |
| Polysaturated oils | 70 (56) | 56 (51) | 126 (53) | |
| Breakfast cereal | ||||
| Without added sugars | 94 (63) | 76 (60) | 170 (61) | 0.870 |
| With added sugars | 47 (31) | 42 (33) | 89 (32) | |
| Do not eat cereal | 9 (6) | 9 (7) | 18 (7) | |
| Soft Drink | ||||
| With added sugar | 132 (88) | 110 (87) | 242 (87) | 0.759 |
| Diet drinks | 17 (11) | 15 (12) | 32 (12) | |
| Do not drink soft drink | 1 (1) | 2 (2) | 3 (1) | |
| Physical activity in the last weekf | ||||
| 0–3days | 56 (39) | 72 (57) | 128 (47) | 0.003 |
| 4–7 days | 89 (61) | 55 (43) | 144 (53) | |
aMissing information for 1 youth; bmissing information for 4 youths; cmissing information for 2 youths; dmissing information for 17 youths; emissing information for 41 youths; fmissing information for 5 youths.
Sixty percent of the high school adolescents were boarders on Thursday Island (56% females, average age 13.8 years, SD = 1.4, 48% overweight/obese). We reasoned there would be little variation in the pattern of food intake among boarders compared to those who return home for their meals every day. Also, meals provided to boarders could potentially be more balanced and more likely to adhere to the Australian Guide to Healthy Eating than meals eaten at home. The analysis was, therefore, repeated comparing high school boarders with nonboarders. Consumption of most food items described in Table 2 was similar between the 2 groups (P-values ranged from 0.296 to 0.973). Exceptions included fruit consumption (75% of the boarders had at least 2 servings daily compared to 46% for nonboarders, P < 0.001), white breads (96% of the boarders had white breads versus 76% for nonboarders, P = 0.009), cereals (57% of the boarders had cereals without added sugars versus 22% for nonboarders, P = 0.003), butters instead of margarine (86% of the borders versus 59% of non-borders, P = 0.010), and oils (85% of the boarders had food cooked with monounsaturated oils versus 63% for nonboarders, P = 0.018).
3.2. Food Frequency Questionnaire
Frequency of intake data was available for 92 Indigenous high-school youths: 57% male, average age 14.3 years (SD = 1.5), 49% were overweight/obese, and 43% centrally obese. In general, except for dairy (69%), frequency of daily consumption from the five food groups was similar (90%) amongst participants. Specifically, energy dense foods and beverages' was the most commonly consumed food group on a daily basis (97%) followed by meats (94%), vegetables, and bread (91%) (Table 3). The proportion of participants who never/rarely consumed energy dense foods and beverages was 0%, dairy products 5%, vegetables 2%, with meat, fruits, and breads 1% each.
Table 3.
Usual frequency of consumption from each of the five food groups, including “energy-dense” food group and water in high school adolescents who answered the FFQ (n = 92).
| Frequency of food consumption | |||
|---|---|---|---|
| Food groups consumed* | Consumed at least daily n (%) | Consumed 1–6 times a week n (%) | Never or rarely n (%) |
| Dairy | 63 (69) | 24 (26) | 5 (5) |
| Fruit | 82 (89) | 9 (10) | 1 (1) |
| Meat | 86 (94) | 5 (5) | 1 (1) |
| Vegetables | 84 (91) | 6 (7) | 2 (2) |
| Bread | 84 (91) | 7 (8) | 1 (1) |
| Energy dense foods and beverages | 89 (97) | 3 (3) | 0 (0) |
| Water (including tea and coffee) | 55 (60) | 26 (28) | 11 (12) |
*Food groups are based on the classification of the Australian Guide to Healthy Eating [14].
We found that neither frequency of daily intake of energy-dense foods including high-energy drinks, sweet snacks, savoury snacks, takeaway-style foods, nor low-energy foods including fruits, green leafy, orange, and cruciferous vegetables, and other vegetables were associated with body weight status (P > 0.05) (Table 4). Intergroup comparisons for the other food types did not reveal any significant differences. Except for daily consumption of takeaway foods (33% of boys versus 5% of girls, P = 0.001), there was no significant sex difference in usual frequency of food consumption (data not shown, P-values ranged from 0.150 to 0.834).
3.3. Physical Activity
Overweight/obese youths reported engaging in fewer days of physical activity in the previous week (mean = 3.2 days) than normal weight youths (mean = 3.9 days, P = 0.001). Fifty-seven percent of overweight/obese youths reported 0–3 days of physical activity in the previous week compared to 39% for normal weight youths (Table 2). The pattern of physical activity differed by sex and age. Overall, boys reported an average of 3.8 days of physical activity in the previous week compared to 3.3 days for girls (P = 0.021). The sex difference was most evident amongst high-school adolescents: 44% of the boys reported 4–7 days of physical activity compared to 17% of the girls (P = 0.002; mean = 3.6 days for boys, mean = 2.2 days for girls, P < 0.001). Primary school boys and girls reported similar levels of physical activity (P = 0.913). Primary school children reported an average of 4.0 days of physical activity in the previous week compared to 2.9 days for high school adolescents (P < 0.001). Amongst boarders, the pattern of physical activity also differed by sex (39% of the boys reported 5–7 days of physical activity and 19% 0-1 day compared to 8% and 29% of the girls, resp. P = 0.045).
3.4. Multivariate Analysis
Overweight/obese youths were more likely to report fewer days of physical activity (0–3 days as opposed to 4–7 days) in the preceding week than normal weight youths (OR = 2.50, 95%CI 1.44–4.34). There was also a statistically significant trend (P = 0.001) between physical activity and overweight/obesity: fewer physically active days was associated with a higher risk of being overweight/obese (OR = 1.66, 95%CI 0.98–2.89 for those reporting 2–4 days of physical activity in the last week and OR = 5.65, 95%CI 2.10–15.23 for those reporting ≤1 day, compared to 5–7 days).Youths with large waist circumference were also more likely to report fewer days (0–3 days) of physical activity in the preceding week than normal weight youths (OR = 2.9, 95%CI 1.31–6.43), and this effect was independent of weight (weight assessment was included in the model). Except for the consumption of dugong, there were very little differences in the pattern of food consumption by weight assessment (Table 5). Overweight/obese youths were 1.89 times (95%CI 1.07–3.34) more likely to eat dugong regularly than normal weight youths. No differences in food consumption by waist circumference were seen.
Table 5.
Adjusted odds ratios of selected foods and physical activity for those who were overweight or obese compared to normal weight youth*.
| Whole study population | Nonboarders | |
|---|---|---|
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Fruit (≥2 servings per day)a | 0.74 (0.43–1.26) | 0.87 (0.48–1.58) |
| Vegetables (≥4 servings per day)a | 1.03 (0.50–2.14) | 1.03 (0.50–2.14) |
| Takeaway foods (≥2 per week)a | 0.99 (0.53–1.89) | 0.99 (0.53–1.88) |
| Turtle (≥2 per week)a | 1.62 (0.85–3.09) | 1.62 (0.85–3.09) |
| Dugong (≥2 per week)a | 1.89 (1.07–3.34) | 1.80 (0.93–3.48) |
| Fish (≥2 per week)a | 0.99 (0.55–1.79) | 0.99 (0.55–1.79) |
| Physical activity in the last weeka (0–3 days) | 2.50 (1.44–4.34) | 2.33 (1.26–4.30) |
*All logistic regression models and odds ratios (unless stated) were adjusted for age, sex, physical activity, and boarder versus nonboarders.
aInformation obtained through the “short nutrition questionnaire”.
bLogistic regression model and odds ratio for physical activity were adjusted for age, sex, boarder versus nonboarders, and consumption of fruit, vegetables, turtle, and dugong.
A sensitivity analysis was conducted to assess whether findings were influenced by the boarders' distinct circumstances (potentially healthier food patterns than youths who return home for their meals every day). The multivariate analysis was repeated in the subgroup of nonboarders and odds ratios were similar to those for the total study population (Table 5).
4. Discussion
This is the first study to examine food intake and physical activity patterns of Indigenous youths residing in the Torres Strait, a group with a high prevalence of overweight/obesity and risk factors for the metabolic syndrome [10, 11]. The most significant observation was the consistent association between overweight/obesity and frequency of physical activity. In general, high school adolescents reported fewer days of physical activity in the previous week than primary school children, and high school girls reported fewer days of physical activity than boys. Adolescent Indigenous girls may, therefore, be the most likely to benefit from an intervention aimed at increasing physical activity.
A large number of Indigenous youths reported low daily frequency of fruits and vegetables consumption compared to AGHE [14]. Of particular concern is the daily consumption of sweet snacks and high-energy drinks by high school adolescents. In the past, Indigenous Australians had a very active subsistence lifestyle, their traditional diet was low in energy density, high in micronutrients, and included Indigenous fruits, vegetables, fibre, seeds, meats (i.e., kangaroo), and sea foods (e.g., fish, crustaceans, and shellfish) for those groups living near water [9, 30–32]. The diet of youths in the Torres Strait has become less “traditional” and more “Westernised”. Geographically the Torres Strait Islands are unique in that they are isolated from the Australian mainland and from the other island communities themselves by significant bodies of water (Figure 1). In general, the fresh produce from the mainland (delivered weekly to Thursday Island) travels long distances, is transferred at various points, and is exposed to high temperatures [33, 34]. Compared with stores located in major Queensland cities, the cost of fruit, vegetables, and legumes is 20.6% higher, and 9% of basic healthy food items are usually unavailable for purchase in remote areas [35]. Access and affordability of fruit and vegetables in the Torres Strait region needs to be urgently acted upon by local, State and National governments in order to improve the nutrition of local youths. There is also a need for devising public health strategies and culturally appropriate health promotion and nutrition education programs aimed at increasing the intake of vegetables and fruit and low-fat dairy products, while reducing the consumption of high energy drinks and sweet snacks. Because of the high cost of “imported food,” nutritional education programs that incorporate healthy “traditional” alternatives (more readily available and cheaper) are likely to be effective.
Overweight/obese youths were almost twice as likely to eat dugong regularly and to a lesser extent turtle than normal weight youths. In this region, dugong and turtle are prepared in a variety of ways, some of which involves cooking in significant quantities of fat (oral communication and R Edwards, 1988) [36]. Dugong (3.1 grams/100 g, 526 kJ/100 g) has higher amount of fats than turtle (0.7 grams/100 g, 453 kJ/100 g), but compared to other foods both are reasonably lower in fat (i.e., 2% low fat milk has 4.7 grams/100 g) and have an energy content similar to baked/grilled fish (520 kJ/100 g) [37, 38]. The method of cooking dugong, especially if fried or cooked slowly (meat and fat) may contribute to the observed association with obesity as the energy content of fried dugong is about 900 kJ/100 g, which is similar in energy content to fried fish obtained from “fast-food” outlets.
Our findings about usual frequency of fruit and vegetable consumption differ slightly from studies of mostly non-Indigenous children conducted in the states of Victoria [39] and Queensland (both used Food Frequency Questionnaire for data collection) [15]. In these studies, 50–66% of the children met the AGHE for fruit and about 15% for vegetable consumption. In our study, 48% of the youths reported eating 2+ servings of fruit daily and 16% reported eating 4+ servings of vegetables daily. The consumption of fast foods amongst the Torres Strait youths was higher than that of children from mainland Queensland (up to 27% of Torres Strait youths had it 2+ times/week compared to 8.7% for mainland Queensland children). In Victoria [39], females had food patterns that were more closely aligned with the Guidelines than males. Except for takeaway foods for which consumption was higher for males than females, we found no gender differences in food consumption.
Data are scant on food intake patterns among Indigenous Australian youths. Our findings about usual fruit and vegetable intake were similar to those of a national survey which included a small number of 12–14-year-old Indigenous children; 53% met the Guidelines for fruit and 12% for vegetable consumption [17] compared to 48% and 16%, respectively, for the Torres Strait youths. Our findings about usual fruit and vegetable intake differ from results of a study of 72 Indigenous children residing in mainland Queensland; 65% met the Guidelines for fruit and 33% for vegetable consumption [40]. The differences between the Queensland mainland study and the Torres Strait data probably relate to the reduced availability of fresh produce on the islands.
Our findings about physical activity by sex are similar to previous reports on physical activity in Australian children [15, 16]. A Queensland-wide study of 3691 mostly non-Indigenous children reported that the number of days children engaged in physical activity or active play in the previous week decreased with age and was higher in boys than girls [15]. Many factors may influence a child's frequency and level of physical activity (i.e., physical environment, socioeconomic issues). The factors influencing physical activity amongst Indigenous children in the Torres Strait are currently unknown. Given the high prevalence of overweight/obesity in this population, [10, 11] the limitations to physical activity need to be identified.
There are a number of limitations inherent in the current study. Firstly, because of the cross-sectional design of our study, it is not possible to draw causal inferences only probable associations. Other studies have shown that a “healthy volunteer effect” among participants in epidemiologic studies can occur [41, 42]. Selection bias in our study may have resulted in a healthier and more active group of participants compared to the general population. Therefore, our findings may have potentially overestimated behaviours perceived as “healthy” (i.e., fruits) and underestimated the food intake patterns of “unhealthy foods” (i.e., sweet snacks). The FFQ did not include portion sizes, which may be important for foods that do not come in natural or typical units. Although the FFQ is comprehensive, it might not include all foods eaten by the Indigenous population. Furthermore, our study FFQ, though not validated, was based on the NNS questionnaire with slight modification. The NNS FFQ was, however, a modified version of a validated questionnaire developed for use in Australian populations (Ireland et al.) and has been used in a national nutrition survey [12] as well as studies involving adolescents [27, 43]. The measure of physical activity used was general and did not capture the other dimensions of physical activity (type, intensity, and duration) [44]. Although not all youths might have interpreted “physical activity” in the same way, they all had the opportunity to ask for clarification. Nevertheless, simple, self-reported questions on children's physical activity appear to have acceptable reliability, and validity, [45–47] and have practical value in indicating situations where an increase in physical activity would be beneficial. Lastly, our study was small and consequently had limited power to detect small differences between the groups with certainty; consequently, there may have been differences that the study did not detect.
Our findings illustrate how a “Westernised” life-style (high calorie diet and little exercise) is associated with weight status (overweight/obesity) in this population. This experience is similar to that of Aboriginal groups in other parts of Australia (e.g., Western Australia) [48] and to other previously traditional societies now in transition to an urbanized, Western existence (e.g., Pima Indians in North America, [49] Inuit in Canada, [50] Papua New Guineans, and other Pacific Island nations) [7, 8]. For example, nearly half of the Inuit population in Nunavut are overweight or obese, and 60% of adults are physically inactive [6]. As in the Torres Strait, Inuit communities are isolated with foods coming from a limited number of grocery stores or through traditional hunting and fishing. Recent reports of the usual diet of this group highlighted that non-nutrient-dense store-bought foods (high in fat and sugar) were consumed much more frequently than the nutrient-dense traditional foods [50].
Torres Strait residents are faced with many challenges in relation to their ability to access certain other food groups because of their geographic isolation [33, 34]. Locally, our findings contribute to the limited knowledge available on frequency of food consumption and physical activity of Indigenous Australian youths and provide useful information that is particularly relevant to the Torres Strait region. A number of diet inadequacies were identified but the most striking observation emerging here is the consistent association between overweight/obesity and physical activity. Our data reinforce the importance of physical activity in Indigenous populations with high prevalence of obesity. Interventions aimed at raising levels of physical activity in youths are likely to play an important role in the primary and secondary prevention of obesity [51]. There is an urgent need for research (relevant to the local setting) to identify the factors that may influence a child's frequency and level of physical activity, and the cultural and social barriers to behaviour change so that effective interventions can be developed.
Conflict of Interests
The authors declare no conflict of interests.
Funding
The study was supported by Queensland Institute of Medical Research. P. C. Valery was supported by an Australian Research Council Future Fellowship (no. FT100100511). A. Moloney was supported by a scholarship from Merck Sharpe & Dohme.
Acknowledgments
The author's contributions were as follows: P. C. Valery, A. Moloney, A. C. Green, A. Cotterill, and A. K. Sinha contributed to the design; P. C. Valery conducted the statistical analysis together with TI; PCV was the primary writer of the paper; and all authors (including G. Garvey) have contributed to the writing of this paper, seen and approved the final version. The sponsors of the study had no role in the study design, collection, analysis, or interpretation of the data, writing of the report or in the decision to submit the paper for publication. The authors wish to thank Mrs Valerie Logan, Professor Peter O'Rourke, Dr Terry Coyne and Mrs Raima Toolis (study cultural advisor). The authors are particularly grateful to the children and their families who participated in the study, without whom this work would not have been possible. The study was supported by Queensland Institute of Medical Research. They are also grateful for the invaluable support of the participating Torres Strait Island communities as well as the District Health Council of the Torres Strait Health and Northern Peninsula Area, who amongst other things, helped with data collection, Queensland Health, and the Commonwealth Government.
Appendix
Food groups classified according to Australian Guide to Healthy Eating [13]. See Table 6.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Zaninotto P, Wardle H, Stamatakis E, Mindell J, Head J. Forecasting Obesity to 2010. London, UK: Department of Health; 2006. [Google Scholar]
- 3.Jotangia D, Moody A, Stamatakis E, Wardle H. Obesity Among Children under 11. London, UK: National Centre for Social Research; 2005. [Google Scholar]
- 4.Styne DM. Childhood obesity in American Indians. Journal of Public Health Management and Practice. 2010;16(5):381–387. doi: 10.1097/PHH.0b013e3181e887ae. [DOI] [PubMed] [Google Scholar]
- 5.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Archives of Pediatrics and Adolescent Medicine. 2009;163(4):344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 6.Nunavut report on comparable health indicators. Department of Health and Social Services GoN, 2007.
- 7.Zimmet P, Dowse G, Finch C, Serjeantson S, King H. The epidemiology and natural history of NIDDM—lessons from the south pacific. Diabetes/Metabolism Reviews. 1990;6(2):91–124. doi: 10.1002/dmr.5610060203. [DOI] [PubMed] [Google Scholar]
- 8.Dowse GK. Incidence of NIDDM and the natural history of IGT in Pacific and Indian Ocean populations. Diabetes Research and Clinical Practice. 1996;34:S45–S50. doi: 10.1016/s0168-8227(96)90007-8. [DOI] [PubMed] [Google Scholar]
- 9.Gracey M. Historical, cultural, political, and social influences on dietary patterns and nutrition in Australian aboriginal children. American Journal of Clinical Nutrition. 2000;72(5):1361S–1367S. doi: 10.1093/ajcn/72.5.1361s. [DOI] [PubMed] [Google Scholar]
- 10.Leonard D, McDermott R, O’Dea K, et al. Obesity, diabetes and associated cardiovascular risk factors among Torres Strait Islander people. Australian and New Zealand Journal of Public Health. 2002;26(2):144–149. doi: 10.1111/j.1467-842x.2002.tb00907.x. [DOI] [PubMed] [Google Scholar]
- 11.Valery PC, Moloney A, Cotterill A, Harris M, Sinha AK, Green AC. Prevalence of obesity and metabolic syndrome in Indigenous Australian youths. Obesity Reviews. 2009;10(3):255–261. doi: 10.1111/j.1467-789X.2008.00545.x. [DOI] [PubMed] [Google Scholar]
- 12.Australian Bureau of Statistics. ABS Catalogue. 4805.0. Canberra, Australia: Australian Bureau of Statistics; 1998. National nutrition survey—nutrient intakes and physical measurements, Australia 1995. [Google Scholar]
- 13.Savige GS, Ball K, Worsley A, Crawford D. Food intake patterns among Australian adolescents. Asia Pacific Journal of Clinical Nutrition. 2007;16(4):738–747. [PubMed] [Google Scholar]
- 14.Smith A, Kellet E, Schmerlaib Y. The Australian Guide to Healthy Eating. Canberra, Australia: Commonwealth Department of Health and Ageing; 1998. [Google Scholar]
- 15.Abbott R, Macdonald D, Mackinnon L, et al. Healthy Kids Queensland Survey, 2006—Summary Report. Brisbane, Australia: Queensland Health; 2007. [Google Scholar]
- 16.Australian Bureau of Statistics. Children’s Participation in Cultural and Leisure Activities. Canberra, Australia : Australian Bureau of Statistics; 2009. [Google Scholar]
- 17.Australian Bureau of Statistics. ABS Catalogue. 4715.0. Canberra, Australia: Australia Bureau of Statistics; 2006. National aboriginal and torres strait Islander Health Survey, 2004-05 (Catalogue No. 4715.0) [Google Scholar]
- 18.Australian Bureau of Statistics. Tech. Rep. 4704.0. Canberra, Australia: Australia Bureau of Statistics; 2008. The health and welfare of Aboriginal and Torres Strait Islander peoples. [Google Scholar]
- 19.Australian Bureau of Statistics. Tech. Rep. 4364.0. Canberra, Australia: Australian Bureau of Statistics; 2009. National Health Survey: Summary of Results, 2007-8 (catalogue No.4364.0) [Google Scholar]
- 20.Kwan D, Marsh H, Delean S. Factors influencing the sustainability of customary dugong hunting by a remote indigenous community. Environmental Conservation. 2006;33(2):164–171. [Google Scholar]
- 21.Zimmet P, Alberti GKMM, Kaufman F, et al. The metabolic syndrome in children and adolescents—an IDF consensus report. Pediatric Diabetes. 2007;8(5):299–306. doi: 10.1111/j.1399-5448.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 22.Valery PC, Chang AB, Masters IB, Stirling J, Laifoo Y, Twist A. Stable prevalence of asthma symptoms in school-aged children in the Torres Strait region. Respirology. 2008;13(3):447–451. doi: 10.1111/j.1440-1843.2008.01239.x. [DOI] [PubMed] [Google Scholar]
- 23.Riley M, Rutishauser I, Webb K. Comparison of Short Questions with 3-Day Food Records. Food and Nutrition Monitoring Unit, Commonwealth Department of Health and Aged Care; 2001. [Google Scholar]
- 24.Rutishauser I, Webb K, Abraham B, Allsopp R. Evaluation of Short Dietary Questions from the 1995 National Nutrition Survey. Food and Nutrition Monitoring Unit, Commonwealth Department of Health and Aged Care; 2001. [Google Scholar]
- 25.Ireland P, Jolley D, Giles G, et al. Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pacific Journal of Clinical Nutrition. 1994;3:19–31. [PubMed] [Google Scholar]
- 26.McLennan W, Podger A. National Nutrition Survey Users’ Guide (catalogue no. 4801.0. ) Canberra, Australia: Australian Bureau of Statistics; 1998 . [Google Scholar]
- 27.McNaughton SA, Ball K, Mishra GD, Crawford DA. Dietary patterns of adolescents and risk of obesity and hypertension. Journal of Nutrition. 2008;138(2):364–370. doi: 10.1093/jn/138.2.364. [DOI] [PubMed] [Google Scholar]
- 28.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. British Medical Journal. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jolliffe CJ, Janssen I. Development of age-specific adolescent metabolic syndrome criteria that are linked to the adult treatment panel III and international diabetes federation criteria. Journal of the American College of Cardiology. 2007;49(8):891–898. doi: 10.1016/j.jacc.2006.08.065. [DOI] [PubMed] [Google Scholar]
- 30.Lee A. The transition of Australian aboriginal diet and nutritional health. World Review of Nutrition and Dietetics. 1996;79:1–52. [PubMed] [Google Scholar]
- 31.O’Dea K. Diabetes in Australian Aborigines: impact of the western diet and life style. Journal of Internal Medicine. 1992;232(2):103–117. doi: 10.1111/j.1365-2796.1992.tb00559.x. [DOI] [PubMed] [Google Scholar]
- 32.Gracey M. Child health in an urbanizing world. Acta Paediatrica. 2002;91(1):1–8. doi: 10.1080/080352502753457842. [DOI] [PubMed] [Google Scholar]
- 33.Leonard D, Beilin R, Moran M. Which way kaikai blo umi? Food and nutrition in the Torres Strait. Australian Journal of Public Health. 1995;19(6):589–595. doi: 10.1111/j.1753-6405.1995.tb00463.x. [DOI] [PubMed] [Google Scholar]
- 34.NATSINSAP Working Party. National Aboriginal and Torres Strait Islander Nutrition Strategy and Action Plan and first phase activities 2000-2001. 2001.
- 35.Harrison M, Lee A, Findlay M, Nicholls R, Leonard D, Martin C. The increasing cost of healthy food. Australian and New Zealand Journal of Public Health. 2010;34(2):179–186. doi: 10.1111/j.1753-6405.2010.00504.x. [DOI] [PubMed] [Google Scholar]
- 36.Edwards R. Traditional Torres Strait Island cooking Kuranda. Queensland, Australia: The Rams Skull Press; 1988. [Google Scholar]
- 37.Food Standards Australia New Zealand. NUTTAB 2006. Online Database of the Nutritional Composition of Australian Foods. Canberra, Australia: FSANZ; 2006. [Google Scholar]
- 38.Food Standards Australia New Zealand. AUSNUT 2007. Brisbane, Queensland, Australia: Xyris Software; 2007. (Professional edition). [Google Scholar]
- 39.Salmon J, Campbell KJ, Crawford DA. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Medical Journal of Australia. 2006;184(2):64–67. doi: 10.5694/j.1326-5377.2006.tb00117.x. [DOI] [PubMed] [Google Scholar]
- 40.Heath DL, Panaretto KS. Nutrition status of primary school children in Townsville. Australian Journal of Rural Health. 2005;13(5):282–289. doi: 10.1111/j.1440-1584.2005.00718.x. [DOI] [PubMed] [Google Scholar]
- 41.Froom P, Melamed S, Kristal-Boneh E, Benbassat J, Ribak J. Healthy volunteer effect in industrial workers. Journal of Clinical Epidemiology. 1999;52(8):731–735. doi: 10.1016/s0895-4356(99)00070-0. [DOI] [PubMed] [Google Scholar]
- 42.Thomson CA, Harris RB, Craft NE, Hakim IA. A cross-sectional analysis demonstrated the healthy volunteer effect in smokers. Journal of Clinical Epidemiology. 2005;58(4):378–382. doi: 10.1016/j.jclinepi.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 43.Baghurst K. Red meat consumption in Australia: intakes, contributions to nutrient intake and associated dietary patterns. European Journal of Cancer Prevention. 1999;8(3):185–191. doi: 10.1097/00008469-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Ness AR, Leary SD, Mattocks C, et al. Objectively measured physical activity and fat mass in a large cohort of children. PLoS Medicine. 2007;4(3):476–484. doi: 10.1371/journal.pmed.0040097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Booth ML, Okely AD, Chey T, Bauman A. The reliability and validity of the physical activity questions in the WHO health behaviour in schoolchildren (HBSC) survey: a population study. British Journal of Sports Medicine. 2001;35(4):263–267. doi: 10.1136/bjsm.35.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Booth ML, Okely AD, Chey T, Bauman A. The reliability and validity of the adolescent physical activity recall questionnaire. Medicine and Science in Sports and Exercise. 2002;34(12):1986–1995. doi: 10.1097/00005768-200212000-00019. [DOI] [PubMed] [Google Scholar]
- 47.Sallis JF, Strikmiller PK, Harsha DW, et al. Validation of interviewer- and self-administered physical activity checklists for fifth grade students. Medicine and Science in Sports and Exercise. 1996;28(7):840–851. doi: 10.1097/00005768-199607000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Gracey M. New world syndrome in Western Australian Aborigines. Clinical and Experimental Pharmacology and Physiology. 1995;22(3):220–225. doi: 10.1111/j.1440-1681.1995.tb01985.x. [DOI] [PubMed] [Google Scholar]
- 49.Knowler WC, Pettit DJ, Saad MF, Bennett PH. Diabetes mellitus in the pima indians: incidence, risk factors and pathogenesis. Diabetes/Metabolism Reviews. 1990;6(1):1–27. doi: 10.1002/dmr.5610060101. [DOI] [PubMed] [Google Scholar]
- 50.Sharma S, Cao X, Roache C, Buchan A, Reid R, Gittelsohn J. Assessing dietary intake in a population undergoing a rapid transition in diet and lifestyle: the Arctic Inuit in Nunavut, Canada. British Journal of Nutrition. 2010;103(5):749–759. doi: 10.1017/S0007114509992224. [DOI] [PubMed] [Google Scholar]
- 51.Riddoch CJ, Leary SD, Ness AR, et al. Prospective associations between objective measures of physical activity and fat mass in 12-14 year old children: the Avon Longitudinal Study of Parents and Children (ALSPAC) British Medical Journal. 2009;339:p. b4544. doi: 10.1136/bmj.b4544. [DOI] [PMC free article] [PubMed] [Google Scholar]


