Abstract
Objective:
To assess the pattern of follow-up and level of hypertension control according to sociodemographic, and clinical risk factors in the participants of a screening campaign.
Research Design and Methods:
In 2004, all Saudi residents in the Eastern Province, aged 30 years and above, were invited to participate in a screening campaign for the early detection of diabetes and hypertension. A structured questionnaire was completed during a face-to-face interview. The presence of hypertension and the place of follow-up were recorded. Blood pressure was measured by trained nurses using a mercury sphygmomanometer, according to the recommendations of The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII).
Results:
Thirteen point one percent of the participants had been previously diagnosed as having hypertension. In 34.3% of them, blood pressure was controlled, while 40.8% had combined uncontrolled SBP and DBP, 14.4% had isolated uncontrolled SBP, and 10.5% had isolated uncontrolled DBP. The blood pressure control was inversely associated with age. It was higher in women, singles, the educated, in those with BMI of less than 25 kg/m2, and in those with positive history of CVD (p<0.001).
Conclusion:
Co-morbidities relevant for hypertension are very prevalent, so aggressive BP control is mandatory.
Keywords: Blood pressure control, screening campaign, Saudi Arabia
INTRODUCTION
Hypertension is considered one of the commonest causes of cardiovascular morbidity and mortality1. Randomized controlled trials have convincingly shown that the control of hypertension is critical in reducing the risk of stroke, coronary heart disease, congestive heart failure, and other related adverse health outcomes.2–4
The World Health Organization reports that suboptimal blood pressure (BP) (>115 mmHg SBP) is responsible for 62% of cerebrovascular disease and 49% of ischemic heart disease (IHD). In addition, suboptimal BP is the number one risk factor for death throughout the world.4,5
In Saudi Arabia, there is a lack of current epidemiological data on the pattern of BP control and the factors associated with arterial hypertension control.
The aim of this study was to assess the status of blood pressure control and profile the risk factors of hypertensive patients in the Eastern Province.
METHODS
This study was part of large screening campaign conducted in 2004. The methodology has been previously described in detail.6 A scientific committee was set up to formulate the details of this campaign. This included the determination of standards for running the campaign, accreditations of instruments and health education materials to be used, training, finance, supervision and health education committees, data processing and entry committees. A media campaign was organized in each sector, using written materials and audiovisual media. Besides, billboards along the streets carried posters and some were displayed in various public places in the Eastern Province. The target population was 650,000 subjects, which is the estimated number of Saudi residents in the Eastern Province aged > 30 years. All Saudi residents in the Eastern Province of Saudi Arabia, aged 30 years and above were invited to participate in a screening campaign for the early detection of diabetes mellitus (DM) and hypertension. More than 300 examination posts located in all primary health care centers, governmental, and most private hospitals and dispensaries were to be used for this. In addition, there were mobile teams as well as personnel in other venues to collect data. A structured questionnaire developed through a focused group, and validated by experts in the fields of DM and hypertension, was used by pre-trained health teams who had attended a training course for the conduct of the campaign. Information on age, gender, place of residence, marital status, occupation, level of education and lifestyle patterns regarding physical activity and smoking was collected. Physical activity was grouped into four: no physical activity with complete sedentary lifestyle (reading, watching T.V), mild physical activity (ordinary housework, walking less than three hours per week, moderate (exercise for at least three hours per week engaging in sports like cycling, walking or other activities that need effort), and strenuous physical activity, as exercise for at least five hours per week in sports like jogging, swimming, etc.
Participants were also asked whether they had previously been diagnosed with hypertension and if they were being treated for it. The participants underwent measurements of weight, height, blood pressure, and capillary blood glucose. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Those with a BMI of 25.0-29.9 kg/m2 were classified as overweight, while those with a BMI ≥ 30.0 kg/m2 were classified as obese, and (18.5-24.9 kg/m2) as normal range.
Based on the recommendations of The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-VII)4 blood pressure was measured in the sitting position, with the participant at rest, twice, at an interval of 1-2 minutes. The mean of the two readings was recorded. If the difference between the two readings was greater than 5 mmHg, measurements were taken until the readings were stable. A standardized mercury sphygmo-manometer, with an appropriate-size cuff inflated to a pressure approximately 30 mmHg greater than systolic was used to take blood pressure measurements. The patient's arm was maintained at the level of the heart. The systolic pressure was taken as equal to the pressure at which the sound is first heard by auscultation (Korotkoff phase I), and the diastolic pressure as equal to phase V (the point of disappearance of the sound). The screening test was considered positive if the systolic and diastolic blood pressure were ≥ 140 and /or ≥ 90 mmHg, respectively.
In this study, only those participants who had previously been diagnosed as hypertensive and were on a diet or blood pressure lowering agents were included in the analysis, but those who were newly diagnosed as hypertensives from the campaign were not. Participants were categorized as controlled, or not, if they had, or had not, a blood pressure of <140/90 mmHg.
Co-coordinators were assigned to each sector to supervise the examination posts, ensure the continuity of work, calibration of equipment and resolve such issues as absence of health workers, equipment breakdown, shortage of forms, to ensure that all forms had been completed, remind defaulters, pursue campaign letters and cooperate with the coordinators in other sectors and main supervisory committees.
The forms were collected from each sector, and checked again for completeness. Non-eligible people were excluded, and forms with incomplete data, or unconfirmed results were sent back to the sectors for corrections to be made.
Data analysis
Using SPSS version 16, the differences between those with and without controlled (SBP) and (DBP) were assessed using ANOVA test. Chi-squared test was used to study the relation between controlled and uncontrolled hypertension and socioeconomic and clinical risk factors. Those cardiovascular risk factors found to be associated with uncontrolled hypertension were included in multiple logistic regressions. The odds ratio and 95% confidence interval were calculated. A P value equal or less than 0.05 was considered as statistically significant.
RESULTS
The prevalence of diagnosed hypertension among adults ( > 30 years old) was 25,784 (13.1%) out of the total of 197,681 participants involved in the campaign. Data was missing on 923 (0.5%) individuals. There were more women 15,003 (15.6%) than men 10,341 (10.7%).
In subjects who were aware that they had hypertension, 97.3% were receiving treatment at different health posts; the most common place for treatment was an MOH facility (Table 1). Of all hypertensive patients, only 8851 (34.4%) were controlled, while the proportion of patients with combined uncontrolled SBP and DBP was 10502 (40.8%), the proportion with isolated uncontrolled SBP was 3713 (14.4%), and 2696(10.5%) had isolated uncontrolled DBP.
Table 1.
Hypertensive patients according to place of management
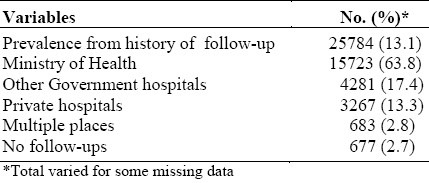
Table 2 shows the mean systolic and diastolic BP according to age and gender in previously diagnosed hypertensive subjects. In men, the mean SBP increased with age and reached its peak in the 60-69 age group, while in women the peak mean systolic BP increased with age (P<0.0001) However, the peak of DBP was in the 50-59 age group in men, and 40-49 years in women (p<0.0001). Generally, women had higher mean systolic but lower mean diastolic blood pressure than men (p<0.0001).
Table 2.
Mean systolic and diastolic BP according to age and gender in previously diagnosed hypertension
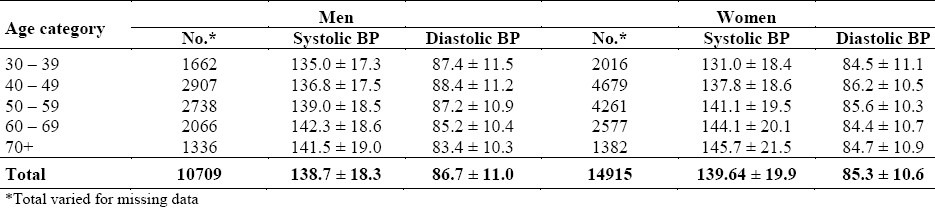
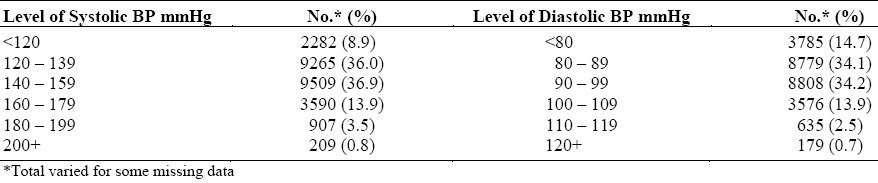
Table 3 represents the categorized level of BP in previously diagnosed hypertensive patients. The highest percentage of subjects showed a BP range 140-159 (systolic), and 90-99 mmHg (diastolic), respectively.
Table 3.
Level of BP in previously diagnosed hypertensive
The distribution of hypertension control by mean BP and patient's characteristics is shown in table 4 and table 5. Generally, hypertension control was higher in the younger group. Men tended to have poorer DBP control and better SBP control than women, but overall hypertension control was better in women than men. The highest rate of BP control was found in participants screened in private health facilities, and the lowest was among participants followed up in health facilities belonging to the MOH (p<0.0001). The predominant pattern of uncontrolled hypertension was that of combined SBP and DBP. It was observed that the prevalence of isolated SBP increased and isolated DBP decreased (p<0.0001) with advancing age (Table 4).
Table 4.
Distribution of hypertension control according to age, gender and place of follow-up
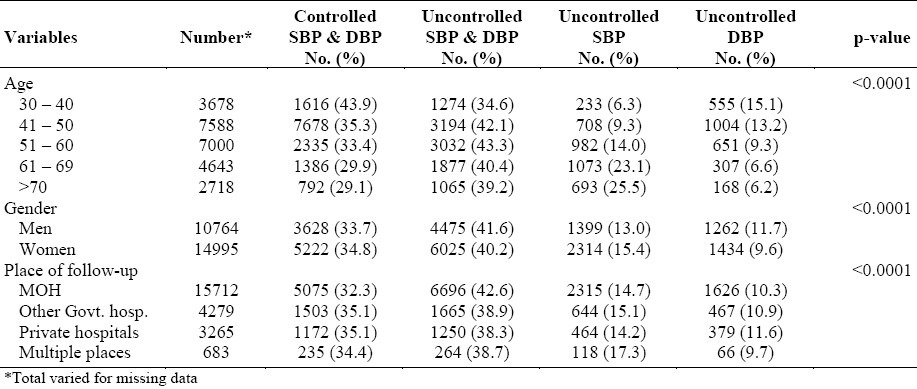
Table 5.
Distribution of hypertension control according to socioeconomic status
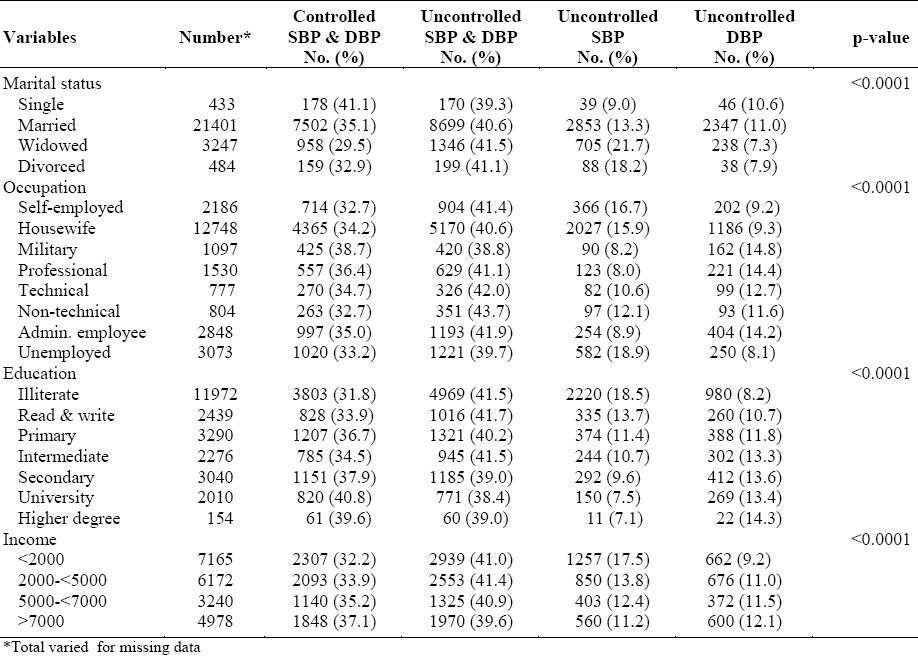
Table 5 shows the relationship of blood pressure control with socioeconomic variables. The highest rate of control was among single subjects, military personnel and professionals (p<0.0001). The highest rate of BP control was among the highly educated and those with a high income (p<0.0001).
Table 6 shows that the most prevalent associated risk factors for hypertension were positive family history of hypertension (15.6%), positive history of cardiovascular disease (56.6%), DM (36.4%), obesity (18.5%), and little physical activity (16.5%). It shows also that frequency of smoking (8.8%) was less in hypertensive patients than in non-hypertensives (p<0.0001).
Table 6.
Co-morbidity risk factors among known hypertensive
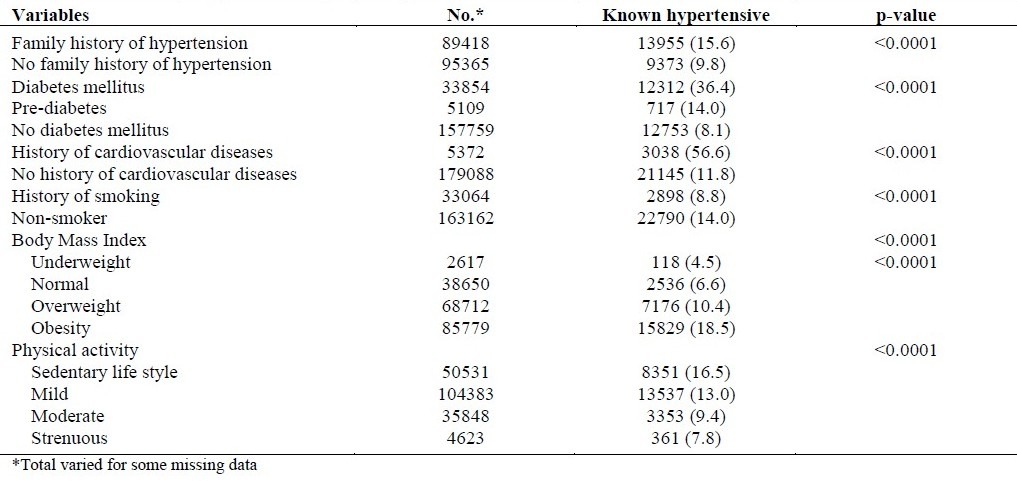
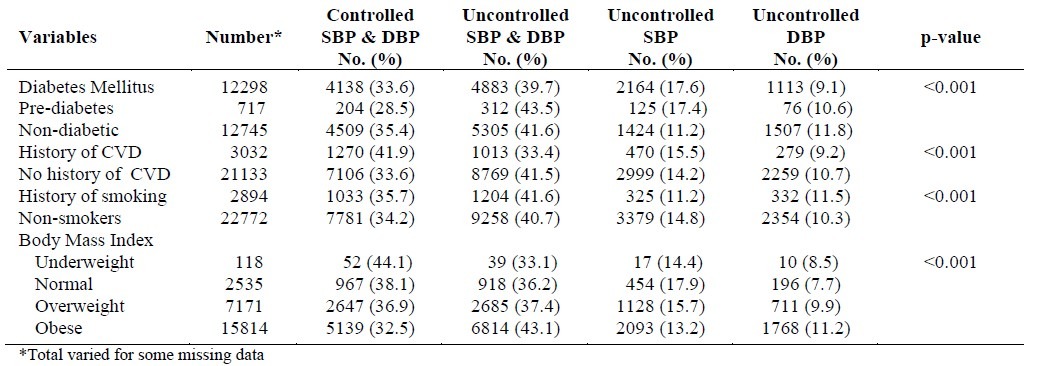
Table 7 shows the distribution of hypertension control in relation to risk factors. BP was controlled in more non-diabetic subjects than those with diabetes mellitus or pre-diabetes. Of these, there were more subjects whose SBP was uncontrolled. Also, a higher proportion of controlled BP was observed among subjects with a positive history of CVD than in those without. On the question of BMI, the highest rate of BP control was observed among subjects who were underweight, followed by those of normal weight (p<0.0001).
Table 7.
Distribution of hypertension control according to other health risk factors
To assess the variables independently associated with blood pressure control in people with diagnosed hypertension, multiple logistic regression was performed with blood pressure control as a dependent variable. Variables that were positively associated with hypertension control were advancing age (OR=1.018, p<0.0001), and positive history of CVD (OR=0.923, p<0.001). On the other hand, obesity was associated with lower control of hypertension (OR= 1.941,P<0.0001), and to a lesser but significant extent, overweight was also associated with less BP control (OR=1.483, p<0.039). A positive family history of hypertension was also associated with lower BP control (OR=1.082, p<0.0001). However, there was no significant association between BP control, smoking, physical activity, and being a diabetic. Pre-diabetes on the other hand, tended to be associated with an increased risk of uncontrolled BP (OR=1.245,p<0.011).
DISCUSSION
This study focused mainly on hypertension control. The knowledge of the actual rate of control is necessary to facilitate the assessment of societal impact and to anticipate resource requirements for the strategic planning of medical care. Considering the fact that only about 34.4% of the patients had adequate BP control. uncontrolled hypertension is a significant public health problem. This would have a significant impact on the morbidity and mortality associated with cardiovascular disease and stroke.
Our findings probably represent a “best case” scenario from the community, compared with the rate observed in USA, between 1999 and 2004, in which 29.2±2.3% in 1999-2000 and 36.8±2.3% in 2003-2004 of hypertensive patients had their BP controlled at the same cut off-point as ours.7 The lower rate of control in the USA can be explained partly by different health insurance coverage for different age groups, but even with the older subjects covered by Medicare, the control of hypertension seemed to be below expectation. The results of our study are at par with those of other settings.8 The apparent better results obtained in some studies can be explained by the fact that a higher cut-off point for control was used.9
The present study demonstrated that combined uncontrolled SBP and DBP is the most frequent form of uncontrolled hypertension, followed by isolated uncontrolled SBP, although in hypertensive patients especially in older patients the mean SBP was elevated, which was an important determinant of BP control. Control SBP was less in older patients than younger ones. In contrast, fewer younger patients had DBP control. This has been previously documented.10 Because of SBP control in older patients with normal DBP, physicians are hesitant to control their BP aggressively.11 These data support the fact that physicians are less inclined to treat hypertension in older patients aggressively to reach the required blood pressure levels12 even though these patients at the greatest risk of developing the problems of uncontrolled hypertension.
Regarding gender, there was a higher prevalence of increased hypertension in women but that rates of blood pressure control were significantly higher. This may be related to the effect of androgens, such as testosterone, and their importance in gender-associated differences in blood pressure regulation.13 Furthermore, our analysis shows that women had higher systolic blood pressure than men, in contrast to DBP. The same pattern of SBP and DBP gender difference was documented in the NHANES 1999–2004 study.14 This represents a more positive predictor of the risk of cardiovascular and renal disease than diastolic blood pressure15 in women than in men.
The present study showed significant positive influences of socioeconomic status and hypertension control. We found that the majority of subjects with uncontrolled hypertension were less educated, and belonged to the lower income group. This may be a reflection of access to different kinds of health facilities. An understanding of health issues is vital to the recognition of the risks involved in not achieving BP goal.
Our data showed a strong association of hypertension and other co-morbidities like DM, presence of CVD, overweight and obesity. Hypertension in nearly 67% of all patients with diabetes and hypertension was not controlled to the target of less than 140/90 mm Hg, although the lowering BP in patients with diabetes and hypertension is associated with a reduction in cardiovascular events and renal failure.16 The JNC4 recommend the BP goal of <130/80 mm Hg for hypertensive patients with diabetes. However, considering the BP of <140/90 in diabetic patients may overestimate the control rate. Therefore, inaccuracies in estimating BP control rates in the diabetic population could lead to an overestimation.
It was evident from the multiple regression analysis, revealed by this study, that the presence of CVD was a more significant factor in blood pressure control than other co-morbidities. Consequently, the most important concern is to bring their BP to the required level in order to reduce that risk.
It is interesting that current smoking was associated with better blood pressure control, but regression analysis could not predict it as a significant factor in BP control. There seems to be a relationship between smoking and a previous published study about our population17 in which smoking was associated with weight loss.
The limitation of this study was that a detailed history about management regimen and duration of diagnosed hypertension were not known. However, its strength lay in the large sample sizes that provided nationally representative estimates of 99.5% response rate. Besides, there was a very close correlation of the percentage of our participants with the latest census in the Eastern Province of Saudi Arabia18 on age and gender. In addition, subjects with undiagnosed hypertension were excluded from this study, since they were unaware of their hypertension for action to be taken to control blood pressure and related cardiovascular risks.
Other strengths were that in addition to the known cases of diabetes, the diagnosis of some subjects with diabetes were confirmed by means of a positive screening test.
We conclude that the rate of uncontrolled hypertension is very high. The socially disadvantaged population should be particularly targeted in clinical practice, and aggressive BP control undertaken.
Our study has a public health implication with regard to the evaluation of BP management within the population and the health care system, and in focusing on the target population in order to improve the cardiovascular outcome.
ACKNOWLEDGMENT
We thank all who participated in the campaign for their enthusiasm to fulfill its objectives. Our thanks are also due to the Ministry of Health, Al-Dawa Pharmacy and Algosaibi Company for funding this research, and our thanks are extended to Dr. Mohamed Anwar Alyousef, Dr. Ali Al-Atabani, and Dr. Jamal Al-Hamed, Dr. Abdullah-Alraiess for their active contribution in the campaign.
REFERENCES
- 1.Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens. 2006;24:423–30. doi: 10.1097/01.hjh.0000209973.67746.f0. [DOI] [PubMed] [Google Scholar]
- 2.Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, et al. Effects of intensive blood- pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial.HOT Study Group. Lancet. 1998;351:1755–62. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 3.Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, Weiss NS. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289:2534–44. doi: 10.1001/jama.289.19.2534. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 5.World Health Report 2002: reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organization; 2002. http://WWW.int/whr/2002/ [DOI] [PubMed] [Google Scholar]
- 6.Al-Ghamdi A, Al-Turki K, Al-Baghli N, El-Zubaier A. A community-based screening campaign for the detection of diabetes mellitus and hypertension in the eastern province, Saudi Arabia: methods and participation rate. Journal of family & Community Medicine. 2007;14(3):91–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 8.Bestehorn K, Wahle K, Kirch W. Stroke Risk Screening of Adults with Hypertension: Prospective Cross-Sectional Study in Primary Care. Clinical Drug Investigation. 2008;28(5):281–9. doi: 10.2165/00044011-200828050-00002. [DOI] [PubMed] [Google Scholar]
- 9.Van Rossum CT, van de Mheen H, Witteman JC, Hofman A, Mackenbach JP, Grobbee DE. Prevalence, Treatment, and Control of Hypertension by Sociodemographic Factors Among the Dutch Elderly. Hypertension. 2000;35:814–21. doi: 10.1161/01.hyp.35.3.814. [DOI] [PubMed] [Google Scholar]
- 10.Alexander M, Tekawa I, Hunkeler E, Fireman B, Rowell R, Selby J V, et al. Evaluating Hypertension Control in a Managed Care Setting. Arch Intern Med. 1999;159:2673–7. doi: 10.1001/archinte.159.22.2673. [DOI] [PubMed] [Google Scholar]
- 11.Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician-related Barriers to the Effective Management of Uncontrolled Hypertension. Arch Intern Med. 2002;162(4):413–20. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 12.Izzo JL, Levy D, Black HR. Clinical advisory statement: importance of systolic blood pressure in older Americans. Hypertension. 2000;35:1021–4. doi: 10.1161/01.hyp.35.5.1021. [DOI] [PubMed] [Google Scholar]
- 13.Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension. 2001;37:1199–1208. doi: 10.1161/01.hyp.37.5.1199. [DOI] [PubMed] [Google Scholar]
- 14.Ong KL, Tso AWK, Lam KSL, Cheung BMY. Gender Difference in Blood Pressure Control and Cardiovascular Risk Factors in Americans With Diagnosed Hypertension. Hypertension. 2008;51:1142. doi: 10.1161/HYPERTENSIONAHA.107.105205. [DOI] [PubMed] [Google Scholar]
- 15.He J, Whelton PK. Elevated systolic blood pressure and risk of cardiovascular and renal disease: overview of evidence from observational epidemiologic studies and randomized controlled trials. Am Heart J. 1999;138:211–9. doi: 10.1016/s0002-8703(99)70312-1. [DOI] [PubMed] [Google Scholar]
- 16.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 17.Population and housing characteristics in the Kingdom of Saudi Arabia demographic survey 1428 H. (2007) Kingdom of Saudi Arabia. Ministry of Economy and Planning. Central Department of Statistics and Information Population and Vital Statistics. 2007 [Google Scholar]
- 18.Al-Baghli AN, Al-Ghamdi A, Al-Turki K, El-Zubaier A, Al-Ameer MM, Al-Baghli AF. Overweight and obesity in the Eastern Province of Saudi Arabia. Saudi Med J. 2008;29:1319–25. [PubMed] [Google Scholar]


