Abstract
Objective:
To determine the prevalence of psychological disorders and somatization among primary care patients from a semi-urban area of the Kingdom of Saudi Arabia.
Design:
Screening of consecutive patients with the 12-item and 28-item versions of the General Health Questionnaires and assessments of physical symptoms associated with somatization, using the HSCL-12. Eight primary care health centres in Assir, Saudi Arabia.
Results:
About half of the sample had one or more psychological disorders. The prevalence of somatization detected by the GHQ-28 was 16%. The prevalence of somatization indicated by GPs’ identification of medically unexplained symptoms was 14%. Women displayed higher levels of somatization than men.
Conclusion:
This study reported prevalence of psychological disorders that was as high as found in the more modern areas of Saudi Arabia such as Riyadh. The view that individuals in less open areas are protected from psychological disorders associated with stress and lifestyle pressure seems to be unsubstantiated. The results highlight the potential value of screening for psychological disorders using such simple instruments as the GHQ
Keywords: Psychological disorders, somatization, primary health care, Saudi Arabia
INTRODUCTION
Numerous studies of psychological morbidity among primary care patients in Western Europe and North America have indicated a prevalence ranging from 14% to 50%.1,2 Few studies have, however, been reported in Arab countries, particularly Saudi Arabia.3 Those few studies have, however, suggested a similar range of prevalence, from 18% to 47% of primary care patients.3–6
Some Arabic studies blame recent socio-cultural changes in the Arab oil producing countries for the high prevalence of psychological disorders, arguing that the speed of this development gave little time for individuals to adapt to the demands of a modern way of life.7–9 However, there are some areas of Saudi Arabia which are still considered to be closed areas, or rather, less inclined towards modern life. Based on the above reasoning, since individuals in these areas are less likely to face the pressures of lifestyle changes associated with modernisation, it is expected that a lower prevalence of psychological disorders might be reported here. Assir is a semi-urban area that is less disposed toward modern life than other parts of Saudi Arabia. The present study was, therefore, conducted in the Asir region to investigate the prevalence of psychological disorders in an area that is not greatly affected by modern influences.
In addition to establishing the prevalence of psychological disorders, we examined details of the ways in which such disorders may be presented to general practitioners. First, we described the prevalence of different types of psychological symptoms. Secondly, in the Arabic literature, there is an assumption that Arabic speaking patients may express psychological disorders in somatic terms because of cultural pressures,10,11 and that women tend to somatize their problems more than men.3,4,12,13 We, therefore, examined the possible somatic presentation of emotional distress in three ways. We investigated: the types of physical symptoms that were most likely to be reported by patients with psychological disorders; the extent to which psychological disorders were presented as medically unexplained physical symptoms (MUS); and the prevalence of somatisation identified by a screening questionnaire
METHODS
Participants and recruitment
The sample was drawn from inhabitants of Asir region, in the south of Saudi Arabia, who visited one of the participating primary health care centres during the study period. Eight geographically dispersed primary health care centres (PHCCs) were selected to represent the population of this area. The study was carried out over three months starting on September 15, 2003. The procedure followed daily was to identify randomly one GP at each clinic session every day, either male or female. Each patient was asked, upon arrival at the clinic, to participate in the study. This simple technique gave all patients an equal chance of being selected. In accordance with the culture, recruitment of female patients was carried out in the presence of their male companions.
Patients under 17 years old were excluded, as were patients attending for reasons other than health complaints, such as for vaccination, examinations and reports. Three patients refused to participate. Two were females who refused to participate because they did not want contact with the male researcher without their husbands.
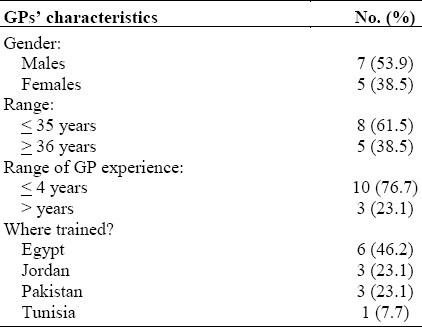
All general practitioners (GPs) who were asked to take part agreed. Their ages ranged from 29 to 41 and their experience as GPs ranged from 2 years to 9 years. Table 1 has more details of their characteristics. None of them was a Saudi citizen, none was a graduate of any Saudi college of medicine, and none had trained in a Saudi primary care centre before starting to work in this field.
Table 1.
Socio-demographic characteristics of the participating GPs (n=13)
Procedure
Those who agreed to participate were given the set of questionnaires to complete in a private air-conditioned room, while waiting for their consultation. For sixteen patients (7%) who were illiterate (four male, 12 female), the questionnaires were read out by the researcher (MA) if the patient was male. If the patient was female, her male companion (usually the father or husband) read out the questionnaire.
Instruments
The GHQ12 was used to provide an index of ‘caseness’. This questionnaire has been widely used for this purpose internationally and has been translated and validated for use by Arab primary care patients.14 Using the Likert scoring method (0,1,2,3), the cut-off point chosen to best balance sensitivity and specificity was 12/13 with a previously reported sensitivity of 0.83, and specificity 0.80.14
The GHQ-28 was used to provide further information about the components of psychological disorders and to provide a further view of ‘caseness’. This questionnaire has also been translated and validated for Arab patients.4 Unlike other forms of GHQ, the GHQ-28 is a scale which provides both a total score and subscale scores. For the total score, the recommended scoring method is (0,0,1,1) while the recommended scoring method for the subscales is the Likert scoring method (0,1,2,3).15 The cut-off for ‘caseness’ using the single score is 4/5.4 The cut-off score for subscales recommended for Arab primary care patients is 9/8.16
In order to detect physical symptoms that are often associated with somatization, the Hopkins Symptom Checklist (HSCL) somatization subscale was used. This HSCL scale is a self-report inventory (12 items) of physical symptoms that are often associated with emotional distress. Reliability of HSCL somatization items range from 0.73 to 0.87.17 In the current study, internal consistency alpha was 0.79. Patients answered the question, “How have you felt during the past seven days including today?” For each symptom, respondents ticked the answer which best described how much it had bothered them during the preceding seven days. Patients rated themselves using a four-point scale of distress, with “not at all” being scored as 1 and a score of 4 representing “extreme” distress.
To identify patients presenting physical symptoms that were not explained by physical disease, a checklist18 based on that in the report of Peveler et al was used.19 It aims at identifying patients that present with physical symptoms that are physically unexplained from the viewpoint of the GPs. After each consultation, GPs completed this scale to indicate whether or not the patient: 1) had come that day with physical problems; 2) the problems could not be explained by recognisable physical disease. Patients for whom both questions were answered with a ‘yes’ were regarded as presenting unexplained symptoms. The face validity of this scale emerges from the fact that it is readily understood and applied by GPs.18 Patients who were identified in this way as presenting unexplained symptoms, and who were identified by the GHQ-12 as having psychological disorders could be regarded as somatizing.19
Statistical Analysis
Descriptive statistics were used to summarise sample characteristics, to describe frequencies of psychological cases according to the GHQ-12, and to describe GPs’ detection of unexplained symptoms. Cross-tabulations and chi-square were used to compare between GPs’ detection of unexplained symptoms and GHQ caseness. Descriptive statistics were used to summarise patients’ somatization symptoms according to the HSCL, and the Mann-Whitney test was used to make a comparison between the two diagnostic groups (i.e., cases and non-cases according to the GHQ).
RESULTS
Of the 227 patients who were approached, 224 including 104 males and 120 females agreed to participate. The age range of the patients was 17 – 68 years. The mean age was 36.7 years, reflecting the population in Saudi Arabia. The patient sample is described in detail in Table 2.
Table 2.
Socio-demographic characteristics of the sample. Chi-square tests the associations between the diagnostic group (cases and non-cases) and each sample characteristic
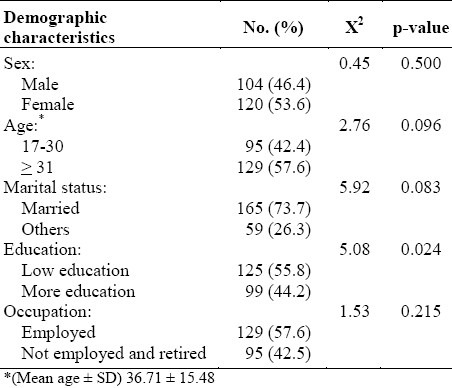
Males were slightly fewer than women in this study. Most patients were married; 6% of the female respondents and 3% of the males were in polygamous marriages. More than half of the sample had little education (i.e. had finished intermediate school or less). There was no significant difference in sex, age, marital state or occupation between cases and non-cases (for this distinction, see below). A tendency for a significant difference was found in the education level; less educated patients were more likely to have psychological disorders. However, there was no significant difference between the sixteen illiterate patients and other patients.
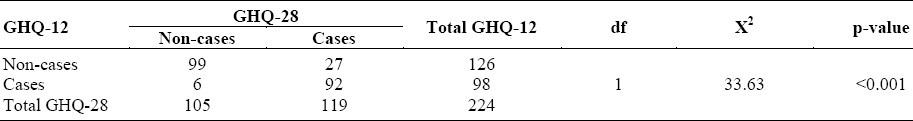
The prevalence of psychological disorders among the entire sample was 98 (43%) using the GHQ-12. The prevalence was 119 (53%) using the GHQ-28 total score. The most prevalent psychological morbidities according to the GHQ-28 subscales were depression (N=61, 27%) followed by Anxiety (N=57, 25%) and Somatic Symptoms (N=37, 16%). The prevalence of Social Dysfunction was less than the other three problems (N=21, 9%). When cross-tabulations were used to compare the GHQ-12 and GHQ-28 categorisations of ‘caseness’, the GHQ-28 detected almost the same cases as the GHQ-12. However, as can be seen in Table 3, the GHQ-28 detected additional ‘cases’.
Table 3.
Cross-tabulations of GHQ-12 and GHQ-28. Chi-square was used to compare GHQ-12 to GHQ-28 categorizations
As shown in Table 4, 14% of the patients were classified by the GP as having medically unexplained symptoms. More than half of these were also classified as ‘cases’ on the GHQ-12 and the association between ‘caseness’ and unexplained symptoms was highly significant.
Table 4.
Cross-tabulations of GP perception of medically unexplained symptoms (MUS) against the GHQ-12 and GHQ-28-somatisation subscale. Chi-square was used to compare between the two groups
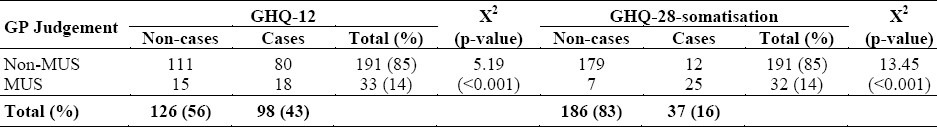
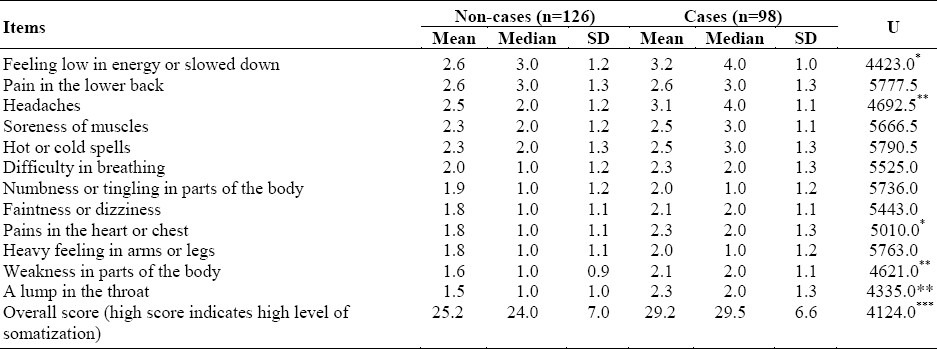
Table 5 shows that ‘cases’ and ‘non-cases’ differed in their symptom report according to the HSCL. ‘Cases’ were generally more likely to report somatization symptoms and, therefore, had a higher total score on this scale. There were some differences also in the pattern of symptoms in the two groups. ‘Cases’ were most likely to report a headache. ‘Non-cases’, on the other hand, were most likely to report being low in energy or being lethargic.
Table 5.
Means, median and SD for items and total score of the HSCL somatization scale. Values shown are for the two diagnostic groups: Non-cases and cases according to the GHQ. Results were ranked according to numbers of non-cases identifying each. Mann-Whitney U compares the two groups
In order to assess whether women displayed higher levels of somatization than men, sociodemographic characteristics were tested against the total score of the HSCL somatization scale. Women reported more somatic symptoms than men (χ2= 118.44; p= <0.001). When the sociodemographic characteristics were tested against GHQ-28 somatisation ‘caseness’, prevalence was higher in women (N=39, 32%) than men (N= 11, 11%) (χ2= 13.43; p= <0.001). For the other sociodemographic characteristic no significant difference was found. When the prevalence of MUS was compared between genders, no significant difference was found. For the other sociodemographic characteristics, no significant difference was found.
Finally, we tested the agreement between the GHQ-28 somatization subscale and the GPs’ detection of unexplained symptoms. About one fifth of the sample (N= 43; 19.19%) were detected as ‘cases’ by one or more of these criteria. As shown in Figure 1, the agreement between the GP and the GHQ-28-somataization was highly significant (p < .001).
Figure 1.
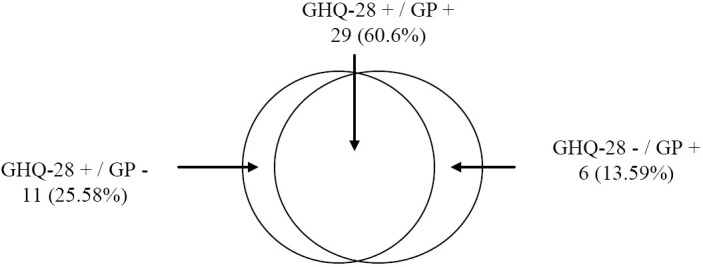
Cases identified by GPs’ ratings of MUS and the GHQ-28-somatization scale
DISCUSSION
The current study is the first to explore psychological disorders and somatisation among consecutive Saudi patients attending primary care in an area of Saudi Arabia relatively closed to western influence and modernisation. The very high level of participation means that this sample is representative of day-to-day activity in the primary health care centres in the area.
The characteristics of the sample were consistent with expected societal characteristics of the region at the time of this research. The slight preponderance of women is consistent with previous studies of primary care patients in Saudi Arabia.3–6 More than one third of the sample was not employed, but 93% of the unemployed patients were women, reflecting the tendency, particularly in the study area, for women not to work outside the home.
The overall prevalence of psychological disorders according to the GHQ was high, and similar to the prevalence of 47% reported in primary care patients in Riyadh by Al-Fares et al.4 Our finding contrasts, however, with two other studies of primary care patients in Riyadh. Al-Khathami and Ogbeide3 reported psychological disorders in only 18% of their sample, and Becker et al5 reported psychological disorders in only 33% of their sample. These differences may be due to methodology used. Al-Khathami and Ogbeide3 used a questionnaire developed in Arab countries: Rahmim Anxiety-Depression (RAD), which they suggested was less sensitive and specific than the General Health Questionnaire. Becker et al5 used the Patient Health Questionnaire (PHQ) which had modest or poor performance in Saudi primary care centers, judged by agreement with psychiatric assessment.
Using the single score of the GHQ-28 the prevalence was 53%, which is slightly higher than that calculated from the GHQ-12 (43 %). This might be because the GHQ-28 includes a subscale of somatic symptoms, which are not measured by the GHQ-12. Some somatizing patients might, therefore, be identified by the GHQ-28 and missed by the GHQ-12. In the matter of further information provided by the GHQ-28, depression was the most prevalent psychological morbidity, followed by anxiety and somatic symptoms. This result is consistent with Becker et al,5 who reported depression as the most common of psychological morbidities in Saudi primary care.
The current study had two indicators of physical symptoms that might be indications of somatization of emotional distress. The prevalence of somatization detected by the somatization subscale of the GHQ-28 was 16%. The prevalence of somatization indicated by the GPs’ rating of unexplained symptoms was 14%. A similar prevalence has been reported in Western studies. For example, unexplained symptoms indicated by the opinion of GPs were 19% in a study by Peveler et al19 and 16% in a study by Ring et al.18
As expected, ‘cases’ detected by the GHQ-12 were generally more likely to report somatization symptoms (indicated by the HSCL) than ‘non-cases’. The most common symptom presented by ‘cases’ was headache, which was reported also by El-Rufaie et al.10 For Arab primary care patients, headache, backache, abdominal pain, pain in the upper and lower limbs, fatigue and chest pain were the most frequent somatic presentation.20,10 Al-Faris21 reported that headache, tiredness and back pain in patients were frequently reported by GPs. As well as being more likely to report physical symptoms characteristic of somatisation, ‘cases’ were more likely to be regarded by their GP as presenting MUS.
It is frequently reported that Arabic women in general and Saudi women in particular are more vulnerable to psychological disorders than men.3,4,12,13 The present study did not confirm this. Nevertheless, there was some evidence that women reported more somatization symptoms than men. Our finding, therefore, contrasts with previous Saudi studies conducted in the Riyadh capital area and among the primary care patients.3,4,12
CONCLUSION
About half of primary care patients in Asir region have psychological disorders. That means that the reported prevalence of psychological disorders by patients attending primary care in a semi-urban area, relatively closed to western influences and modernisation was as high as in the more modern areas of Saudi Arabia such as Riyadh. The view that individuals in less ‘open’ areas of the society are protected from psychological disorders associated with stress and lifestyle pressures seems to be unsustainable. For future studies, it is important to find out what proportion of this high prevalence of psychological disorders is detected by GPs. The results highlight the potential value of screening for psychological disorders using a simple instrument such as the GHQ.
Although psychological disorders were associated with increased reporting of physical symptoms, only a minority of patients with psychological disorders presented medically unexplained symptoms. Therefore, contrary to expectation, somatic symptoms do not seem to be a major way in which psychological cases present. Nevertheless, a headache is the most common symptom presented by ‘cases’, and this could be used initially by GPs as a signal to consider the diagnosis of a psychological disorder.
REFERENCES
- 1.Richards J, Ryan P, McCabe M, Groom G, Hickie I. Barriers to the effective management of depression in general practice. Australian and New Zealand Journal of Psychiatry. 2004;38:795–803. doi: 10.1080/j.1440-1614.2004.01464.x. [DOI] [PubMed] [Google Scholar]
- 2.Pini S, Perkonnig A, Tansella M, Wittchen H, Psich D. Prevalence and 12-month outcome of threshold and subthreshold mental disorders in primary care. Journal of Affective Disorders. 1999;56:37–8. doi: 10.1016/s0165-0327(99)00141-x. [DOI] [PubMed] [Google Scholar]
- 3.Al-Khathami A, Ogbeide D. Prevalence of mental illness among Saudi adult primary-care patients in Central Saudi Arabia. Saudi Medical Journal. 2002;23:721–4. [PubMed] [Google Scholar]
- 4.Al-Fares E, Al-Shammari S, Al-Ahmad A. Prevalence of Psychiatric Disorders in an academic primary care department in Riyadh. Saudi Medical Journal. 1992;13:49–53. [Google Scholar]
- 5.Becker S, Al Zaid K, Al Faris E. Screening for somatization and depression in Saudi Arabia: A validation study of the PHQ in primary care. International Journal of Psychiatry in Medicine. 2002;32:271–83. doi: 10.2190/XTDD-8L18-P9E0-JYRV. [DOI] [PubMed] [Google Scholar]
- 6.Becker S. Detection of somatization and depression in primary care in Saudi Arabia. Social Psychiatry and Psychiatric Epidemiology. 2004;36:962–6. doi: 10.1007/s00127-004-0835-4. [DOI] [PubMed] [Google Scholar]
- 7.Al-Shammari S, Jarallah J, Felimban F. Long-Term care experience in Saudi Arabia. Social Science and Medicine. 1997;44:693–7. doi: 10.1016/s0277-9536(96)00196-7. [DOI] [PubMed] [Google Scholar]
- 8.Dwairy M. Mental health in the Arab world. In: Bellack H, editor. Comprehensive clinical psychology: Sociocultural and individual differences. Vol. 10. New York: Pergamon Press; 1998. [Google Scholar]
- 9.Ghubash R, Daradkeh T, Al-Muzafari S, Al-Manssori M, Abou-Saleh M. Al-Ain community psychiatric survey IV: socio-cultural changes (traditionality-liberalism) and prevalence of psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology. 2001;36:565–70. doi: 10.1007/s001270170008. [DOI] [PubMed] [Google Scholar]
- 10.El-Rufaie O, Al-Sabosy M, Bener A, Abuzeid M. Somatized mental disorder among primary care Arab patients. Journal of Psychosomatic Research. 1999;46:549–55. doi: 10.1016/s0022-3999(98)00101-9. [DOI] [PubMed] [Google Scholar]
- 11.Dwairy M. A biopsychosocial model of metaphor therapy with holistic cultures. Clinical Psychology Review. 1997;17:719–32. doi: 10.1016/s0272-7358(97)00027-5. [DOI] [PubMed] [Google Scholar]
- 12.Racy J. Somatization in Saudi women: a therapeutic challenge. British Journal of Psychiatry. 1980;137:212–6. doi: 10.1192/bjp.137.3.212. [DOI] [PubMed] [Google Scholar]
- 13.El-Rufaie O. A Psychiatric clinic in a primary care setting: Evaluating the experience. Saudi Medical Journal. 1988;9:20–4. [Google Scholar]
- 14.El-Rufaie O, Daradkeh T. Validation of the Arabic versions of the thirty- and twelve-item General Health Questionnaires in primary care patients. The British Journal of Psychiatry. 1996;169:662–4. doi: 10.1192/bjp.169.5.662. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg D. Manual of the General Health Questionnaire: NFER-Nelson. 1978 [Google Scholar]
- 16.Al-Haddad M, Al-Garf A, Al-Jowder S, Al-Zurba F. Psychiatric morbidity in primary care. East Mediterranean Health Journal. 1999;5:21–6. [PubMed] [Google Scholar]
- 17.Derogatis L, Lipman R, Rickels K, Uhlenhuth E, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 18.Ring A, Dowrick C, Humphris G, Davies J, Salmon P. The somatising effect of clinical consultation: what patients and doctors say and do not say when patients present medically unexplained physical symptoms. Social Science and Medicine. 2005;61:1505–15. doi: 10.1016/j.socscimed.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 19.Peveler R, Kilkenny L, Kinmonth A. Medically unexplained physical symptoms in primary care: a comparison of selfreport screening questionnaires and clinical opinion. Journal of Psychosomatic Research. 1997;42:245–52. doi: 10.1016/s0022-3999(96)00292-9. [DOI] [PubMed] [Google Scholar]
- 20.Al-Arfaj A, Al-Saleh S, Alballa S, Al-Dalaan A, Bahabri S, Al-Sekeit M, et al. How common is back pain in Al-Qasem region. Saudi Medical Journal. 2003;24:170–3. [PubMed] [Google Scholar]
- 21.Al-Faris E, AI-Hamad A, AI-Shammari S. Hidden and conspicuous psychiatric morbidity in Saudi primary care health care. The Arab Journal of Psychiatry. 1995;6:162–75. [Google Scholar]


