Abstract
Objective:
To explore parental attitudes towards the prescription of psychotropic medication for their children.
Method:
A questionnaire built to collect socio-demographic data of parents and their attitudes was distributed among parents.
Results:
One thousand and ten questionnaires were filled by parents. Fathers who completed the questionnaire were double the number of mothers. Eight hundred and eighteen parents (84.3%) agreed to the dispensing psychotropic medication to their children if necessary. About 83.5% preferred to start with psychotherapy before trying medication. Fathers are more than twice likely than mothers to agree to the use of psychotropic drugs. Older parents more easily agreed to give their children psychotropic drugs. Parents who used psychotropic drug themselves were more likely to agree to the use of psychotropic drug by their children. Having a child with a psychiatric illness is the most significant factor in making parents accede to giving children psychotropic medication. Other factors such as pressure from schools and the side effects of drugs could also modify decision of parents.
Conclusion:
Although most parents agreed to give their children psychotropic drugs if necessary, they preferred to start with psychotherapy sessions before giving them the drugs. Fear and worries about such issues as side effects of drugs or addiction should be considered. Pressure from school should also be considered when deciding on drug therapy.
Keywords: Parents, children, attitudes, psychotropic medication
INTRODUCTION
Recent reports from the United States and other countries suggest an increase in the prescribing of psychotropic medications for children including very young children with behavior and mental health problems.1–6
The rate of utilization of psychotropic treatment for the youth in the 1990s nearly reached the rate for adults.7 Several factors have been suggested to explain the increased use of psychotropic drugs and stimulants in particular: a heightened awareness of psychiatric disorders in children resulting in more children starting therapy, an increase of girls being treated, and an increased duration of drug treatment.8–9
Children with behavioral disorders were increasingly being subjected to unnecessary pharmacologic intervention even though there is no empirical evidence to support psychotropic drug treatment in very young children.10 There is a growing concern about the increasing number of children who use psychotropic medications. Major concerns involve the lack of evidence regarding safety and efficacy of the majority of psychotropic drugs for children particularly in the long-term and the possibility of over-prescribing.11–12 In Saudi Arabian society, medications are not viewed as harmful or unsafe although as one study shows parents do feel they are overused in children.13
Despite the dramatic increase in the use of pediatric pharmacology, there is a surprising paucity of discussion about the psychological impact of medication on parents and children.14 Therefore, both parents should be contacted early in the assessment since they may object to the use of medication for their child.15 Some researchers believe that clinicians’ responsiveness to the wishes and fear of children and their families will enhance the therapeutic relationship.16
The idea behind this study is that child psychiatrists have difficulty in deciding when to commence treatment with psychotropic medications for children with psychiatric illness. The problem lies in the parents’ objection to giving their child psychotropic drugs, poor compliance with medication or even non-attendance of the child at the outpatient clinics.
The aim of this study was to explore parental attitudes toward the prescription of psychotropic medications for their children. Considering these attitudes and managing them will improve the therapeutic relationship and result in better intervention for children with psychiatric problems.
STUDY DESIGN
A questionnaire was built consisting of the demographic data of parents - and their children 12 years or younger - with psychiatric problems. In addition to items expressing the attitudes of parents towards the prescription of psychotropic medications for children, there were items which sought to find out whether those parents had children with psychiatric problem or not. The criterion for inclusion in the sample was being a parent. It did not matter if the child was healthy physically or mentally ill. The sample was randomly selected from those parents attending the outpatient child psychiatric clinic, primary care pediatric clinic, specialized pediatric outpatient clinics and those parents who attended primary care clinics at King Khalid University Hospital (KKUH), parents working at an ordinary primary school for boys and one for girls, a centre for mentally handicapped boys and another for girls, and housewives.
KKUH is the main teaching hospital for the College of Medicine, King Saud University, Riyadh. It has facilities for accident and emergency, as well as inpatient and outpatient services for most specialties including psychiatry.
DATA ANALYSIS
Frequency count was used to determine the number and percentage of socio-demographic data and attitudes. Variables were compared using Chi square, and statistical analysis was performed using SPSS. To analyze the correlation between socio-demographic factors and opinions with parental attitudes, odds ratio, confidence limits or exact confidence limits if preferred and p-values were used.
RESULTS
One thousand two hundred questionnaires were distributed and 1010 completed questionnaires were returned. Some questions were not answered on some papers as will be noticed in the tables.
Table 1 shows the socio-demographic data. Fathers were almost double the number of mothers. About half of the sample (51.7%) were in their 4th decade. Most of them were high school graduates (27.2%) or university graduates (43.5%). Of the sample, 38.7% were working in the educational sector, 32.9% had governmental jobs other than in the health or educational sectors and 18.4% did not work (all were housewives). Most of the parents were still married and lived together (91.6%). The monthly income of two-thirds was between 5000-10000 Saudi Riyals (1350-2700 US$).
Table 1.
Socio-demographic data
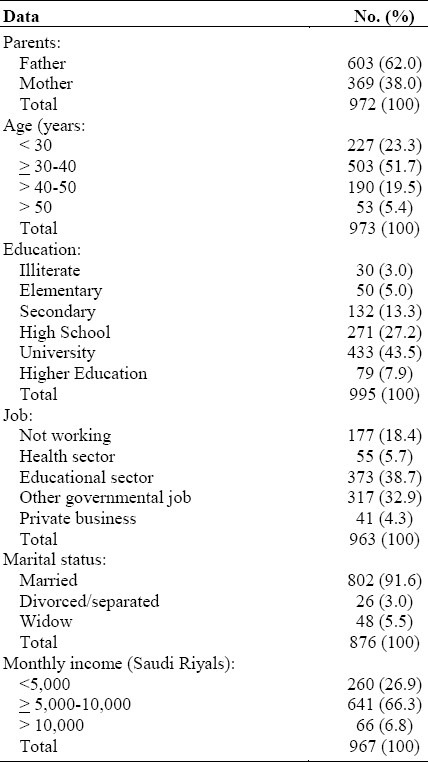
Table 2, shows parental attitudes towards the prescription of psychotropic medications for their children. Eight-hundred and eighteen parents (84.3%) agreed that their children should be given a psychotropic drug if necessary. They gave more than one explanation for their agreement. About 35.3% believed that the treating psychiatrists was more aware of the child's needs, 29.5% said that they were compelled by the pressures from the school to give the child psychotropic drug, 23.6% believed that the drug treatment produced faster results than psychotherapy, 22.7% said that the child's condition necessitated the use of psychotropic drug, 18.1% believed that they themselves had positive personal experience with psychotropic drug treatment and about 19.3% gave other reasons for their assent.
Table 2.
Parental attitudes towards prescribing psychotropic medication for children
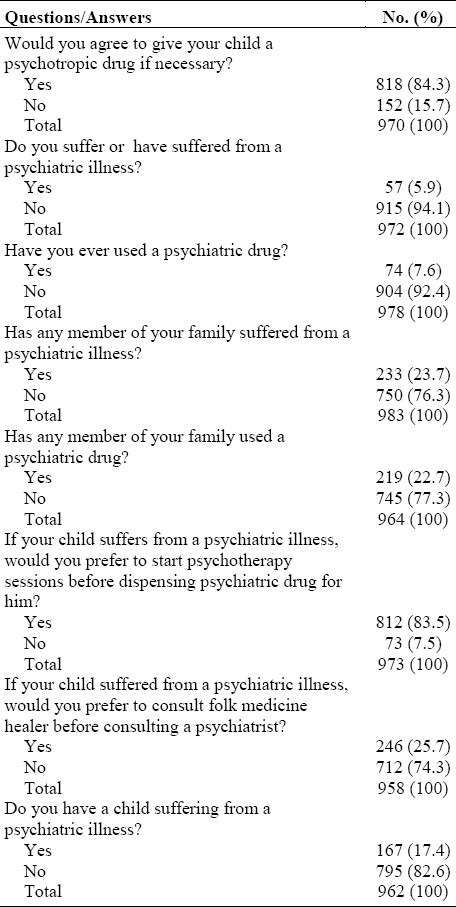
Parents who disagreed with the prescription of psychotropic drug for their children gave many reasons for their objection. About 78.3% were worried about the drug's side-effects, 71.1% thought that the child was too young to take a psychotropic drug, 52% expressed anxiety about drug addiction, 40.1% said that other alternatives, 23.7% said that there were the child's condition did not warrant the use of psychotropic drug treatment, 16.4% were anxious about drug interaction, 13.2% believed that children did not have psychiatric illness and 20.7% gave other reasons for their objection.
When parents were asked whether they preferred to start with psychotherapy or psychotropic drug treatment for their children if needed (Table 2), 83.5% preferred to start psychotherapy. About 74.3% preferred to consult a psychiatrist rather than a folk medicine healer if a child had a psychological problem.
Table 3 which deals with the socio-demographic factors affecting parental attitudes, shows that fathers were twice as likely as mothers to agree to have their children given psychotropic medication if necessary, with an odds ratio of 2.21 and p-value of 0.000. As parents advanced in age, their willingness to have psychotropic medication prescribed for their children increased.
Table 3.
Socio-demographic factors correlated to parental attitudes of dispensing psychiatric drug to their children
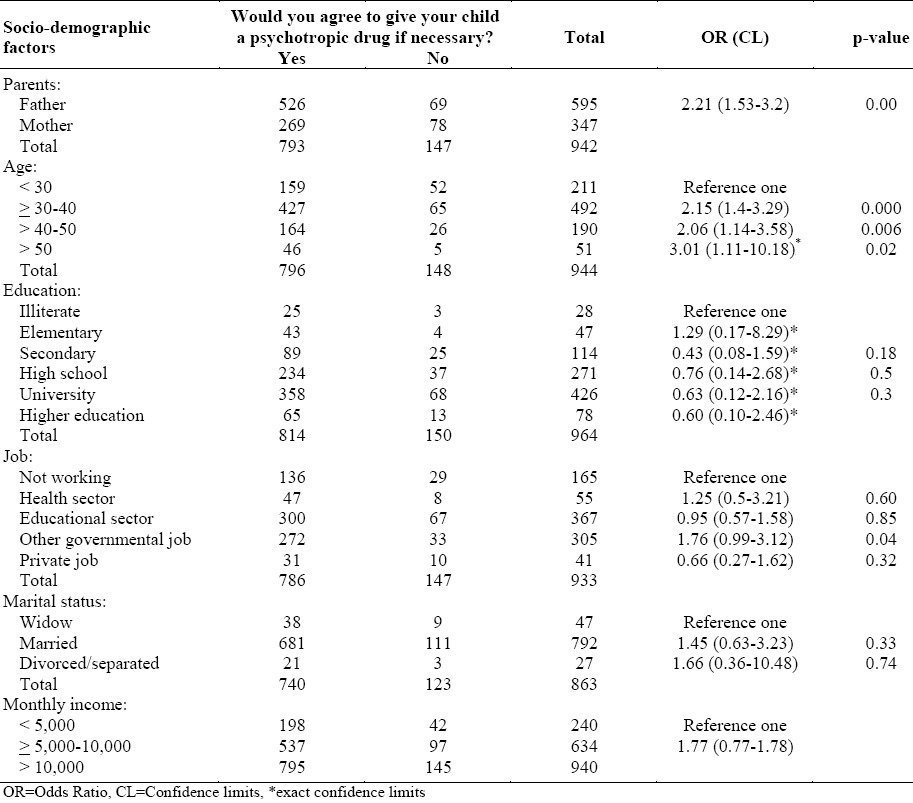
The level of education of the parents in this sample seemed not to have affected their decision to consent or object. Having a monthly income of more than 10,000 Saudi Riyals (2700US$) increased the chances for giving consent, with an odds ratio of 2.12 and p-value of 0.096.
Table 4, shows parental opinions that were likely to modify their attitude towards the dispensing of psychotropic medication to their children. Parents who used psychotropic drugs themselves were more likely to give their children such drugs if needed, with odds ratio of 2.11 and p-value of 0.08.
Table 4.
Parental opinions correlated to their attitude of dispensing psychiatric drug to their children
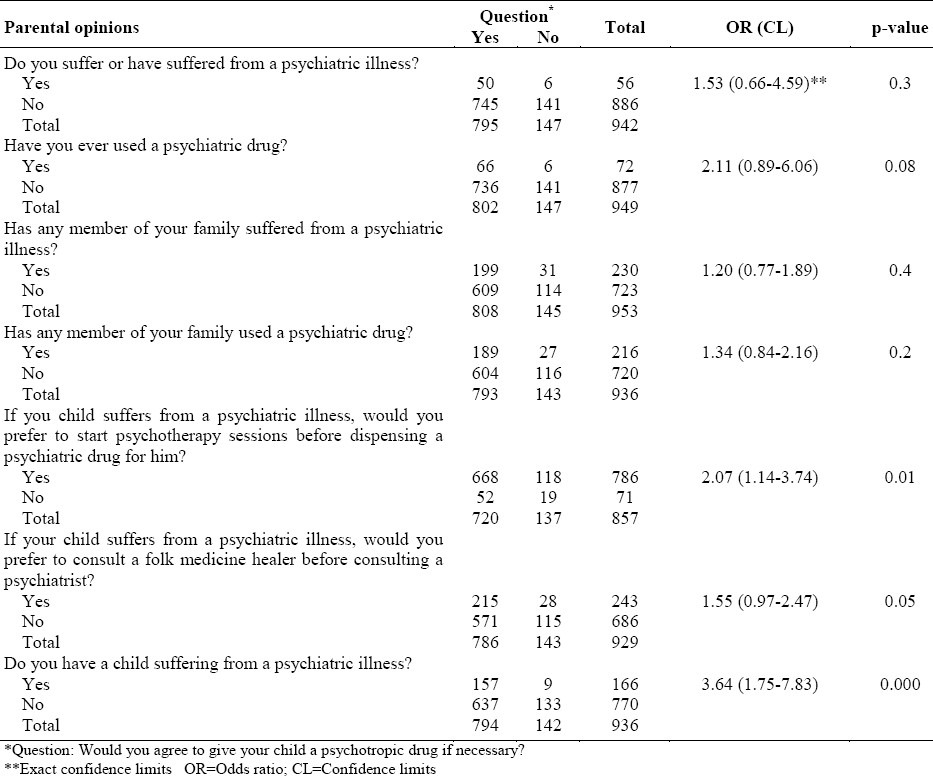
Those who preferred to start psychotherapy before trying psychotropic drug were likely to give their children psychotropic drug if necessary, with odds ratio of 2.07 and p-value of 0.01. Even those who preferred to consult a folk medicine healer first were likely to give their children psychotropic medication, if necessary, with odds ratio of 1.55 and p-value of 0.05. Having a child with a psychiatric illness was the most significant factor that made parents consent to giving him or her a psychotropic medication, with odds ratio of 3.64 and p-value of 0.00.
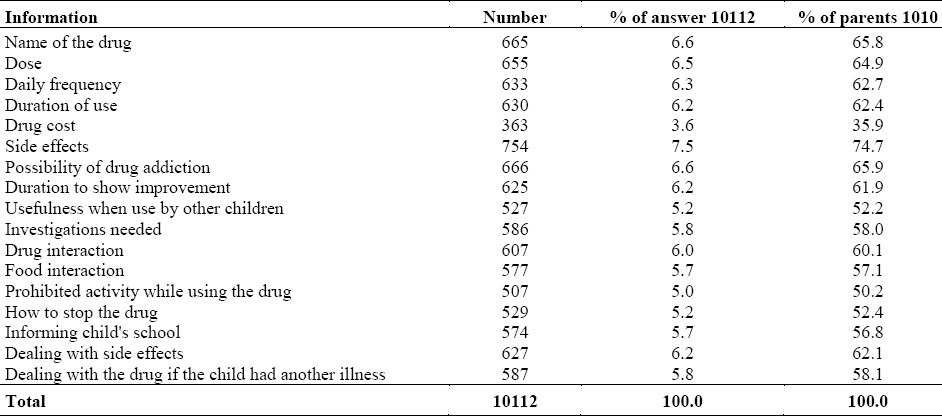
Table 5, shows the most important information requested by parents before commencing the child on a psychotropic medication. The 1010 parents gave 10,112 answers. The most frequent information requested referred to the side effects of the drug (74.7%) followed by possibility of drug addiction(65.9%) followed by its name(65.8%), then its dosage (64.9%) and then the daily frequency(62.7%).
Table 5.
Information parents want to know before dispensing a psychiatric drug to their child
DISCUSSION
In this study, fathers outnumbered mothers. This could be due to over-sampling as some mothers did not fill or return questionnaires as mentioned earlier. However, it could reflect the difference in the level of awareness and knowledge between fathers and mothers about the psychotropic medications.
The conduct of the study in Riyadh, the capital city of Saudi Arabia on a sample, most of whom were young may explain why most had high school diplomas or higher, and were employed. In addition, the questionnaires were distributed outside the outpatient clinics of KKUH, in places of work such as schools. This could explain the parental level of education and the type of work they did. Two thirds of the sample had a monthly income of 5000-10000 Saudi Riyals (from different sources) which in fact reflects the situation of the average Saudi family with that level of education and work.
In this study, the cooperation of parents in answering the questionnaire was very good (84%), which may reflect their awareness of the importance of such study. The fact that some parents failed to answer some questions may reflect, in the author's opinion, inattentiveness or anxiety while filling the questionnaire. However, it may reflect subconscious unwillingness to address certain issues.
While parents are often willing to give cough medicines or antibiotics that are not efficacious for viral infections, they are much more apprehensive at the prospect of giving medications that alter their children's mood or behavior.15 So the response given by 84.3% in this study stating they would consent to their children being given psychiatric medication in a conservative community like Saudi is in the author's view high. However, most of the parents participating in this study did not have children with psychiatric problems. Possibly, it reflects the level of education and their awareness of psychiatric medications gained through the media and the Internet. However, this could be simply be an ideal theoretical answer. In practice, psychiatrists still have difficulty in convincing parents to start their children on psychiatric medication when it is needed. Psychotherapy is usually first, which is understandable since the question asked was, “Would you agree to give your child a psychiatric drug if necessary?” And for them, if necessary would mean if alternatives like psychotherapy were no longer available. In this study, most of the parents preferred to start with psychotherapy sessions rather than give psychotropic medication as a first step, and about one fourth preferred to consult a folk medicine healer before visiting a psychiatrist. Other studies confirm these findings.15,18 In fact, Dr. Steven E. Hyman, Director of the National Institute of Mental Health (NIMH) stated that, as a rule of thumb, the doctor, psychologist and the social worker should attempt to modify the behavior of a child and deal with family crises before drugs are prescribed.19
Parents in this study gave many reasons for their agreement to give their child psychiatric medication if necessary. One of the reasons given was pressure from the school. As evident from many studies, children experience behavioral problems that result in the disturbance of certain functions. This makes teachers and school personnel put pressure on parents to give their children psychiatric medications to keep them in school.15,17 One of the main concerns of parents in this study which is in accord with other studies is their objection to giving psychotropic medication to their children because of their side-effects.16 Clinicians should pay attention to the side-effects of medications and to whether parents are comfortable with the idea of giving the medications to their children.16
In the Saudi family, the father is usually the sole decision-maker for his family.13 The presence of father in the clinic during a discussion of the child's need for medication increases the chances of convincing the family of the need to prescribe a psychotropic drug. However, the presence of both parents at the discussion is likely to prevent any later parental conflict on the medication, thereby reducing the problem of non-compliance. The effect on the parents’ attitudes towards dispensing psychiatric drugs to their child was insignificant when a parent had a psychiatric illness. It is probable that the number of the parents affected was too small to determine any reason for it. Also, because of the social stigma, parents were probably reluctant to reveal any personal or family history of psychiatric problems. Their answers should therefore, be taken with caution.
In this study, it was revealed that previous positive experience of parents with psychotropic drugs facilitated the family's assent to the dispensing psychotropic medication for their children if necessary. Other studies confirm the finding.15,18 Parents who have responded well to their own medication are usually more receptive to giving a medication to their child as a trial.15 It has been found that parents whose children had used either medication or counseling in the past had more favorable feelings towards the two types of therapy.18 One of the significant findings in this study was that the presence of a child with a psychiatric illness would make parents significantly more agreeable to his being given a psychotropic drug. This could be due to the severity of the child's very disruptive behavior for which medication is indicated or the result of previous positive experience with the psychiatrist or with the drug.
The information requested by parents in this study before psychiatric drug is dispensed to their child was similar to that requested in other studies.18 The second most important piece of information requested by most parents was the possibility of drug addiction. Some people wrongly believe that some, if not all psychotropic medications are addictive. In fact, apart from stimulants, none of these drugs cause tolerance or addiction. In practice, it has been proved that using stimulants like methylphenidate to treat Attention Deficit Hyperactivity Disorder did not increase the possibility of substance abuse. The lack of recognition of the disorder, the absence of treatment, or incomplete treatment might, however, increase the possibility of substance abuse during adolescence.20
Although most psychiatric drugs are considered expensive, parents in this study ranked cost the least important information they want to have. One explanation is that very few of them had any previous experience with psychiatric drugs so they had no idea of their cost. The other explanation is that most people receive their medications free through governmental agencies.
LIMITATION
It was difficult to find similar studies for comparison. This is probably due to the paucity of discussion about the psychological impact of psychotropic medication on children and their parents.
Because of social stigma, some responses given by parents particularly in relation to personal or family history with regard to psychiatric problems might be unreliable and should be taken with caution.
Although the author tried to cover most of community sectors, conducting the study in a city like Riyadh was difficult, so some social strata particularly people living on outskirts or those with a Bedouin background might have been excluded.
CONCLUSION AND CLINICAL IMPLICATIONS
Although most parents in this study said they would agree to give their children psychiatric medication when necessary, they would prefer to start with psychotherapy sessions before drugs are prescribed for them. Both parents should be present when discussing the use of psychotropic medication for a child. Their fears and worries about such issues as side effects and addiction should be raised and discussed. Finally, pressure from school should be considered.
ACKNOWLEDGMENT
The author would like to express her thanks and appreciation to Dr. Abdulaziz Bin Saeed for his statistical advice and to Mr. Jose Wendell Cuyos for his secretarial work.
REFERENCES
- 1.Efron D, Hiscock H, Sewell J, et al. Prescribing of psychotropic medications for children by Australian pediatricians and child psychiatrists. 2003;111(2):372-5. Pediatrics. 2003;111(2):372–5. doi: 10.1542/peds.111.2.372. [DOI] [PubMed] [Google Scholar]
- 2.Hewson PH, Anderson PK, Dinning AH, et al. A12-months profiles of community paediatric consultation in Barown region. J Paeditr Child Health. 1999;35:16–22. doi: 10.1046/j.1440-1754.1999.00340.x. [DOI] [PubMed] [Google Scholar]
- 3.Safer DJ. Changing patterns of psychotropic medications prescribed by child psychiatrists in the 1990s. J Child Adolesc Psychopharmacol. 1997;7:267–74. doi: 10.1089/cap.1997.7.267. [DOI] [PubMed] [Google Scholar]
- 4.Rappley MD, Mullan PB, Alverz FJ, Enli IU, Wang J. Diagnosis of attention defficit/hyperactivity disorder and use of psychotropic medication in very young children.1999;153:1039-45. Arch Pediatr Adolesc Med. 1999;153:1039–45. doi: 10.1001/archpedi.153.10.1039. [DOI] [PubMed] [Google Scholar]
- 5.Zito JM, Safer DJ, dosReir S, Gardner JF, Boles M, Lynch F. Trends in prescribing of psychotropic medications to preschoolers. JAMA. 2000;283:1025–30. doi: 10.1001/jama.283.8.1025. [DOI] [PubMed] [Google Scholar]
- 6.Rushton JL, Whitmire T. Pediatric stimulant and selective serotonin reuptake inhibitor prescriptions trends1992-1998. 2001; 155:560-5. Arch Pediatr Adolesc Med. 2001;155:560–5. doi: 10.1001/archpedi.155.5.560. [DOI] [PubMed] [Google Scholar]
- 7.Zito JM, Safer DJ, Ros Reis S, Gardner JF, Magder L, Soeken K, Bales M, Lynch F, Riddle MA. Psychotropic practice patterns for youth: a 10 year perspective. Arch Pediatr Adolesc Med. 2003;157(1):6–14. doi: 10.1001/archpedi.157.1.17. [DOI] [PubMed] [Google Scholar]
- 8.Safer DJ, Zito JM, Fine EM. Increased methylphenidate usage for attention deficit disorder in the1990s. Pediatrics. 1996;98:1084–8. [PubMed] [Google Scholar]
- 9.Swanson JM, Lerner M. Williams L.More frequent diagnosis of attention deficit/hyperactivity disorder. N Engl J Med. 1995;3:933–44. doi: 10.1056/NEJM199510053331419. [DOI] [PubMed] [Google Scholar]
- 10.Coyle JT. Psychotropic drug use in very young children. JAMA. 2000;283:1059–60. doi: 10.1001/jama.283.8.1059. [DOI] [PubMed] [Google Scholar]
- 11.Angold A, Erkanli A, Egger HL, Costello EJ. Stimulant treatment for children: a community perspective. J Am Acad Child Adolesc Psychiatry. 2000;39:975–84. doi: 10.1097/00004583-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Jensen PS, Bahatra VS, Vitiello B, Hoagwood K, Feil M, Burke LB. Psychoactive medication prescribing practice for U.S. children: gaps between research and clinical practice. J Am Acad Child Adolesc Psychiatry. 1999;38:557–65. doi: 10.1097/00004583-199905000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Al-Omran O, MacAdam A, Gard P. Factors affecting medication adherence in Saudi children. The Pharmaceutical Journal. 2000;265(7114):10–3. [Google Scholar]
- 14.Bastiens L. Compliance with pharmacotherapy in adolescents: effects of patients’ and parents’ knowledge and attitudes towards treatment. J Child Adolesc Psychopharmacol. 1995;5:39–48. [Google Scholar]
- 15.Pappaport N, Chubinsky P. The meaning of psychotropic medications for children, adolescents and their parents. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1198–200. doi: 10.1097/00004583-200009000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Jesen PS, Bhatara VS, Vitiello B, Hoagwood K, Feil M, Burke L. Psychoactive medication practice for US children; gaps between research and clinical practice. J Am Acad Child Adolesc Psychiatry. 1999;38:557–65. doi: 10.1097/00004583-199905000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Babares WJ. Use of psychotropic medications in young, preschool children: Arch Pediatr Adolesc Med. 2003;157(2):121–3. doi: 10.1001/archpedi.157.2.121. [DOI] [PubMed] [Google Scholar]
- 18.The facts for families. AACAP. Washington, DC. USA: 2003. AACAP. Psychiatric medications for children and adolescents. Part III: Questions to ask. [Google Scholar]
- 19.Pear R. Young children and psychiatric medications. The New York Times, as quoted in the Palm Beach Post 3.2. 2000, USA [Google Scholar]
- 20.Silver L. Psychopharmachology. In: Silver Larry., editor. Attention Deficit/Hyperactivity Disorder. Third edition. Washington, DC: American psychiatric publication; 2004. pp. 159–81. [Google Scholar]


