Abstract
Background:
Reverse oblique trochanteric fracture of femur is a distinct fracture pattern. 95° Dynamic condylar screw (DCS) and proximal femoral nail (PFN) are currently the most commonly used implants for its fixation. This study aims to biomechanically compare the cutout resistance as well as modes of failure of DCS and PFN in reverse oblique trochanteric fractures.
Materials and Methods:
Sixteen freshly harvested cadaveric proximal femoral specimens were randomly assigned to three mean bone mineral density matched groups, eight of which were implanted with 95° DCS and the other eight with PFN. The constructs were made unstable to resemble a reverse oblique trochanteric fracture by removing a standard size posteromedial wedge. These constructs were subjected to computer controlled cyclic compressive loading with 200 kg at a frequency of 1 cycle/second (1 Hz) and end points of both the groups were analyzed.
Results:
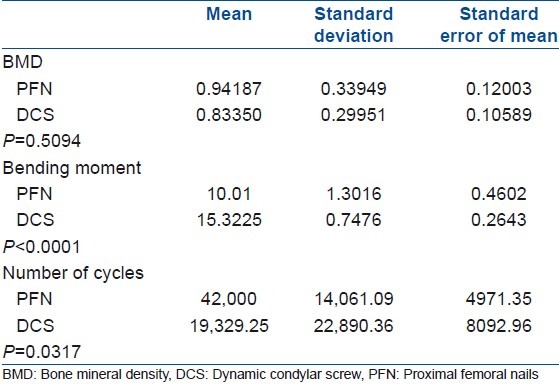
The bending moment of the PFN group was approximately 50% less than that of the DCS group (P<0.0001). The PFN group resisted more number of cycles than the DCS group (P=0.03) and showed lesser number of component failures as compared with the DCS group (P=0.003).
Conclusions:
The PFN is biomechanically superior to DCS for the fixation of reverse oblique trochanteric fractures of femur.
Keywords: Dynamic condylar screw, proximal femoral nailing, reverse oblique trochanteric fractures
INTRODUCTION
The incidence of intertrochanteric femoral fracture has been estimated to be more than 250,000 patients each year in the United States, with the reported mortality ranging from 15 to 20%.1,2 The reverse oblique trochanteric fracture of proximal part of femur is a distinct fracture pattern which is mechanically different and accounts for 2% of all the hip fractures and 5% of all the intertrochanteric and subtrochanteric fractures.3
A sliding hip screw is not indicated for stabilization of these fractures because the large diameter lag screw does not cross the primary fracture line and telescoping of implant may promote fracture separation rather than its impaction.4 This leads to an unacceptably high rate of failure when a conventional sliding hip screw is used to treat such fracture patterns. To overcome this problem, the 95° dynamic condylar screw (DCS) was introduced to stabilize this fracture pattern.3,5,6 Though its use involves a relatively simple operative procedure, various modes of failure of DCS were observed in reverse oblique trochanteric fractures like cutting out of screw, breakage of the plate, and screw or plate pull off from the bone.6,7 In an attempt to overcome some of these limitations, intramedullary devices like proximal femoral nails (PFNs) were used for these fractures.8 With the use of intramedullary devices, the shaft fixation is nearer to the center of rotation of the hip, which gives a shorter lever arm and a lower sliding moment or tensile strain on the implant. The intramedullary location provides buttress against lateral displacement and reduces bending strain on the implant.
The clinical relevance of these presumed biomechanical advantages and less complication rates of PFN are yet to be established. This study aims to biomechanically compare the cutout resistance as well as modes of failure of DCS and PFN in reverse oblique trochanteric fractures.
MATERIALS AND METHODS
The institutional review board approval was taken before the commencement of study. The study was conducted on 16 freshly harvested cadaveric proximal femoral specimens. Dual energy X-ray absorptiometry (DEXA) was used to determine the quality of specimens and these were classified into three groups based on the bone mineral density (BMD): Group A <0.5 g/cm2; group B 0.5–1.0 g/cm2; and group C >1.0 g/cm2. Each group was further randomized into two intervention methods, i.e. PFN and DCS made up of stainless steel (Yogeshwar Pvt. Ltd, Mumbai, India). Eight specimens were implanted with DCS and the rest with PFN (with single screw in the neck) under image intensifier control. During instrumentation, the tip apex distance (TAD) was kept constant to 25 mm for each specimen.
The constructs were made unstable after putting the implant to resemble a reverse oblique trochanteric fracture by removing a standard-sized (1 cm) posteromedial wedge. Antero-posterior and lateral view radiographs of the constructs were taken. These constructs were tested with a cyclic compressive load of 200 kg to mimic the joint reaction force of an adult hip.4,5,9 The tests were conducted at a cyclic frequency of 1 Hz for 50,000 cycles or till failure (defined as more than 5 mm of vertical displacement during cyclical loading), whichever was earlier. Fatigue tests were conducted using computer controlled servohydraulic materials testing system (MTS model 810, MN, USA) of ±50 kN capacity.
The tested constructs were examined by naked eye as well as by radiographs to look for implant bending or breakage/backout/or screw fracture. The deformations in the original structure of implant which were clearly visible on clinical examination were classified as macroscopic failure and those detected only on radiographs were labeled as microscopic failures [Appendix 1].
APPENDIX 1.
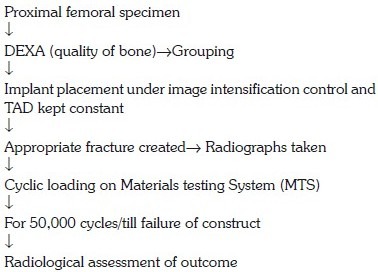
STUDY PROTOCOL
The bending moment (BM) or the moment arm of a construct is the vector of force exerted at the confluence of the axial and the angular forces which can be mathematically calculated using the formula:
F=P×L cos θ,
where F is the BM force, P is the load applied (200 kg), and L is the length of lag screw from the base of barrel of DCS or medial edge of the PFN nail.
For PFN, “θ” is the angle subtended to the normal and it is 45° (135°–90° = 45°):
cos 45° = 0.7071.
For DCS, “θ” is the angle subtended to the normal and it is 5° (95°–90° = 5°):
cos 5° = 0.9962.
Statistical analysis
All the statistical analyses were performed using InStat software for windows (GraphPad version 3.00, SanDiego, CA, USA). Student's t-test was used to analyze the difference of mean for BMD, number of cycles sustained, and BM of the constructs. Mean, standard deviation, and standard error of mean for these variables were also calculated. The test was referenced for two-tailed P value and 95% confidence interval was constructed around sensitivity proportion using normal approximation method. A value of <0.05 was considered statistically significant.
Fisher's exact test was used to comparatively evaluate the component failure in each group. It is a statistical test used to determine if there is nonrandom association (contingency) present between two kinds of interventions. The test was referenced for two-tailed P value and a value of <0.05 was considered statistically significant.
RESULTS
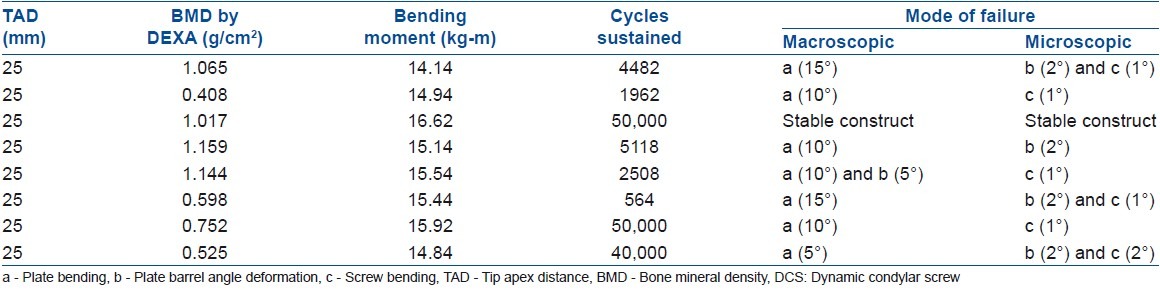
The detailed test data of both the groups were duly registered [Tables 1 and 2] and comparisons were made in construct characteristics (BMD, BM, and number of cycles sustained) and component failures.
Table 1.
Correlation of bone mineral density, bending moment, and number of cycles sustained with mode of failure in PFN specimens
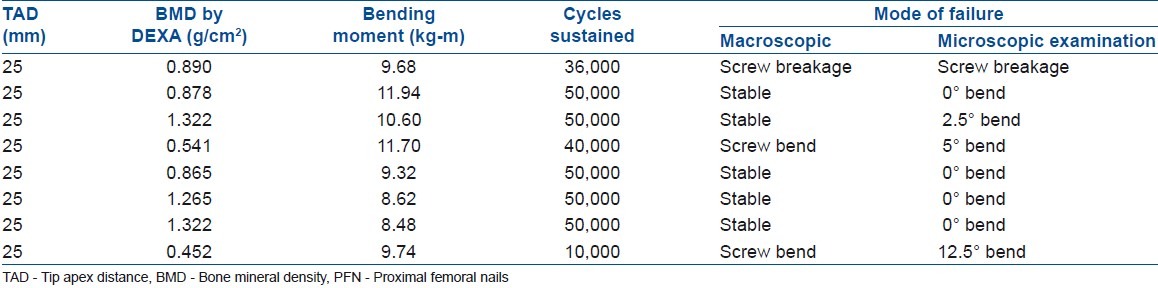
Table 2.
Correlation of bone mineral density, bending moment, and number of cycles sustained with mode of failure in DCS specimens
Comparative evaluation of construct characteristics
The difference in BMD of the specimens of both the groups was statistically not significant (P=0.51), which implies that the quality of the specimen bones was comparable in both the groups [Table 3]. Average BM of DCS group was found to be approximately 50% higher than that of PFN group. Mean BM of PFN group was 10.01, while the value was 15.32 for DCS group, and this difference was found to be statistically significant (P<0.0001). Similarly, mean numbers of cycles sustained by PFN and DCS groups were 42,000 and 19,329 respectively, and the difference was found to attain sufficient statistical significance (P=0.03) [Table 3].
Table 3.
Detailed analysis of bone mineral density of specimens, bending moment of implants, and number of cycles sustained
Comparative evaluation of component failure in each group
In the PFN group, there were four failures (three macroscopic and one microscopic). All the failures were present in screw component [Figure 1], and no failures were noticed in nail component. There was no failure in group C (BMD>1.0 g/cm2). One specimen from group A (BMD<0.5 g/cm2) failed at 10,000 cycles and this was the earliest failure seen in PFN constructs. Five out of eight constructs completed 50,000 cycles successfully without any gross failure [Figure 2]. No failure of any implant was seen in the initial 10,000 cycles. In the DCS group, we noticed plate barrel angle deformation [Figure 3] in 5 constructs, screw bending [Figures 3 and 4] in 6 constructs, and plate bending [Figures 3 and 4] in 7 constructs (18 component failures out of total 24 components). Only one specimen with BMD>1.0 g/cm2 (group C) remained stable. Five out of eight specimens failed within the initial 5000 cycles. Only two specimens completed 50,000 cycles successfully, out of which one showed microscopic deformation. Only six components actually remained stable at the end-point. Thus, there were 4 component failures (out of total 16 components) in the PFN group and 18 component failures (out of total 24 components) in the DCS group. The difference in component failures in both the groups was found to be statistically significant (P=0.003).
Figure 1.

X-rays of cadaveric femoral specimen (a) with unstable reverse oblique trochanteric fracture with posteromedial defect implanted with proximal femoral nail and it was subjected to cyclical compression load. Screw component failed (b) to compression load after 36,000 cycles
Figure 2.
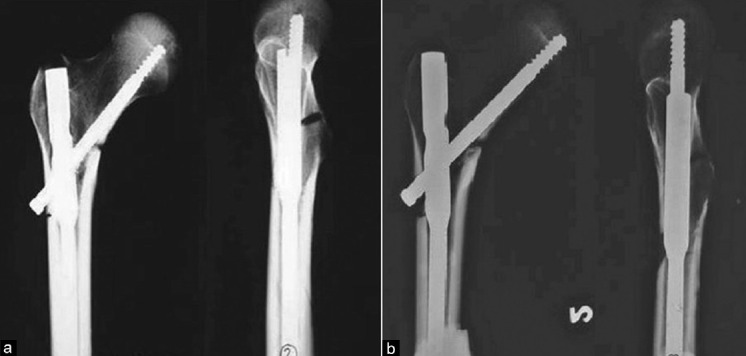
X-rays of cadaveric femoral specimen (a) with unstable reverse oblique trochanteric fracture with posteromedial defect implanted with proximal femoral nail and it was subjected to cyclical compressive load. It remained stable (b) after 50,000 cycles
Figure 3.
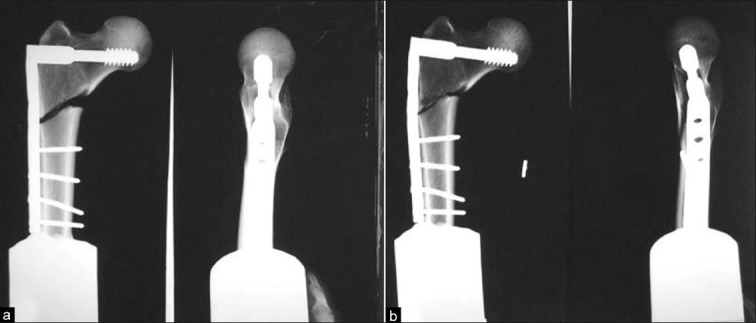
X-rays of cadaveric femoral specimen (a) with unstable reverse oblique trochanteric fracture with posteromedial defect implanted with 95° dynamic hip screw and it was subjected to cyclical compression load. (b) It failed after 4482 cycles. Plate bending of 15°, plate barrel junction deformation of 2.5°, and screw bending of 1.5° were observed at the end of cyclical loading
Figure 4.
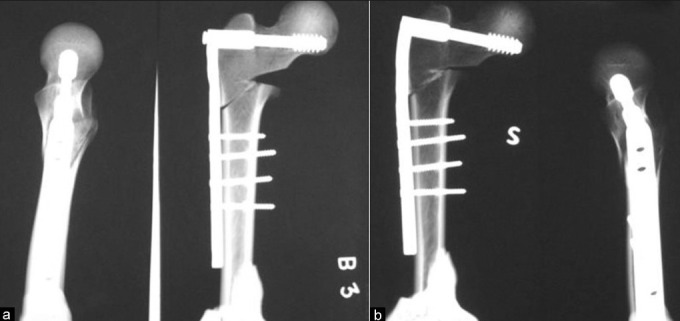
X-rays of cadaveric femoral specimen (a) with unstable reverse oblique trochanteric fracture with posteromedial defect implanted with 95° dynamic hip screw and it was subjected to cyclical compression load. (b) It failed after 1962cycles. Plate bending of 10°, and screw bending of 1° were observed at the end of cyclical loading
It was also observed that bends of 2° or less could be detected only by radiography.
DISCUSSION
Historically, unstable reverse oblique trochanteric fractures have spurred the development of various implants ranging from extramedullary to intramedullary devices.4–8,10–27 The sliding hip screw is the most widely used extramedullary implant for stabilization of both stable and unstable intertrochanteric fractures. However, a number of investigators have reported unsatisfactory results with the use of a sliding hip screw for fixation of these unstable fractures.3,28–30 The overall failure rate associated with the sliding hip screw was higher when the device was used for A3 fractures as compared to that for “standard” (A1 and A2) fractures. It was recommended that a 95° fixed angle implant was a better alternative for the treatment of reverse oblique trochanteric fractures.3,5,6 On the basis of biomechanical analysis, fixed angle devices were preferred for the treatment of reverse oblique fractures against sliding hip screw.5,6 Intramedullary devices offer several theoretical advantages like more efficient loading because of their location and less tensile strain on the implant due to shorter lever arm of the intramedullary device and the consequent decrease in the risk of implant failure. It also incorporates a sliding hip screw which provides the advantage of controlled fracture impaction in addition to limited surgical exposure and leads to preservation of fracture hematoma and less periosteal stripping.7 It is postulated that this superiority of PFN may be directly attributed to its biomechanical advantage due to its less BM. We prospectively sought to determine whether there is any difference in the biomechanical performance of DCS and PFN in cadaveric proximal femoral specimens for a specific subset of unstable intertrochanteric fractures, namely, AO/OTA 31-A3 fractures.
The possible limitations of the study were its small sample size and in vitro study design. The constructs were cyclically loaded with compressive forces at a single point uniaxially in contrast to the multipoint and multiaxial nature of joint reaction forces in vivo. A single screw was used in the nail proximally in contrast to the standard PFN where two screws are used.
Detailed examination of the DCS constructs in our study revealed 18 failures of three types: Plate bending in 7, screw bending in 6, and plate barrel angle change in 5 specimens. On the other hand, there were four failures of two types seen in the PFN group, i.e. bending of screws in three and breakage of screw in one specimen. No failures were observed in the nail component of the construct. It may be pertinent to mention that shaft diameters of lag screws were identical in both the DCS and PFN groups (8 mm). Failure of the screw was the only mode of failure noted in the PFN constructs, whereas in the DCS group, additional modes of failure were also observed like proximal bending of the plate and deformation of plate-barrel junction. Obviously the BM in the DCS constructs was more than that of the PFN specimens. It may be relevant to mention that the plastic deformation would be inversely proportional to the diameter of the screw shaft, provided the properties of the material are constant. Thus, an increase in the BM explains the higher rate of failure in the DCS specimens. One could validate this hypothesis by correlating the BM, which was approximately 50% higher in the DCS group, as the diameter of the screw shaft was constant in both the groups. It may be noted that only one DCS specimen in contrast to four PFN specimens actually remained stable at the end point of cyclical loading.
Cut through of any screw from bone can be attributed to the design of screw and the quality of the bone. It is expected that osteoporotic bone would have poor purchase. However, DEXA results in the present study do not strongly correlate with the observed failure. This may be due to several factors. Loading in the MTS machine was at a single point and it was uniaxial in contrast to multipoint and multiaxial loading in vivo. The screw migration was measured radiologically in the constructs. Although no frank cut out was observed in the implants mounted in the osteoporotic bones, the radiological evidence of screw migration was observed in four PFN and four DCS specimens, all having DEXA less than 1 g/cm2. It may be suggested that on continuous cyclic loading, this radiological migration would ultimately proceed to frank cut out in vitro. Clinical extrapolation of the scenario leads to believe that continuous screw migration superolaterally in the head leads to varus collapse of the fracture, decreasing the gap present posteriomedially in the unstable reverse oblique trochanteric fractures. It would lead to union of the fracture in some cases, while in other cases, it would lead to implant cut through requiring consequent revision. Hence, loss of position i.e. varus drift of fracture, should be taken as a clear evidence of impending construct failure and early corrective steps should be taken, including conversion of surface devices to intramedullary devices.
A complex implant, i.e. made up of an assembly of multiple components, will have higher probability of failure because failure tendency of each component will add up. In the DCS group, multiple component failure to various degrees was seen in different combinations. For example, the combination of plate bending, plate barrel angle deformation, and screw bending was seen in four specimens; plate bending and screw bending was seen in two specimens; and plate barrel angle deformation and screw bending was seen in one specimen. These complex types of failure were observed in the DCS group and not in the PFN group.
PFN appears to be biomechanically superior to DCS in reverse oblique trochanteric fractures. Future studies may be directed to comparatively evaluate these implants in vivo on a larger sample size.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States.Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop. 1990;252:163–6. [PubMed] [Google Scholar]
- 2.Cummings SR, Kelsey JL, Nevitt MC, O’Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178–208. doi: 10.1093/oxfordjournals.epirev.a036281. [DOI] [PubMed] [Google Scholar]
- 3.Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001;83:643–50. doi: 10.2106/00004623-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Koval KJ, Cantu RV. Intertrochanteric fractures. In: Bucholz RW, Heckman JD, Court-Brown CM, editors. Rockwood and Green's fractures in adults. 6th Ed. Vol. 2. Philadelphia: Lippincott Williams and Wilkins; 2006. pp. 1793–825. [Google Scholar]
- 5.Baumgaertner MR, Chrostowski JH, Levy RN. Intertrochanteric hip fracture. In: Brown BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma: Fractures, dislocations, ligamentous injuries. Philadelphia: WB Saunders; 1998. pp. 1833–81. [Google Scholar]
- 6.Sanders R, Regazzoni P. Treatment of subtrochanteric femur fractures using the dynamic condylar screw. J Orthop Trauma. 1989;3:206–13. doi: 10.1097/00005131-198909000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intratrochanteric fractures with use of an intramedullary nail or a 95° screw-plate. J Bone Joint Surg Am. 2002;84:372–81. [PubMed] [Google Scholar]
- 8.Leung KS, So WS, Shen WY, Hui PW. Gamma nails and dynamic hip screws for peritrochanteric fractures. A randomised prospective study in elderly patients. J Bone Joint Surg Br. 1992;74:345–51. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 9.Chila A. Biomechanics. In: Chila A, editor. Foundations of osteopathic medicine. 3rd edition. Philadelphia: Lippincott Williams and Wilkins; 2010. pp. 109–110. [Google Scholar]
- 10.Benum P, Grontvedt T, Braten M, Walloe A, Ekeland A, Raugstad S, et al. Gamma nail versus CHS in intertrochanteric and subtrochanteric femoral fractures- a preliminary report of a prospective randomized study. Acta Orthop Scand. 1992;63(Suppl 247):7–8. [Google Scholar]
- 11.Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur.A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73:330–4. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 12.Butt MS, Krikler SJ, Nafie S, Ali MS. Comparison of dynamic hip screw and gamma nail: A prospective, randomized, controlled trial. Injury. 1995;26:615–8. doi: 10.1016/0020-1383(95)00126-t. [DOI] [PubMed] [Google Scholar]
- 13.Goldhagen PR, O’Connor DR, Schwarze D, Schwartz E. A prospective comparative study of the compression hip screw and the gamma nail. J Orthop Trauma. 1994;8:367–72. doi: 10.1097/00005131-199410000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Hardy DC, Descamps PY, Krallis P, Fabeck L, Smets P, Bertens CL, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998;80:618–30. doi: 10.2106/00004623-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Hoffman CW, Lynskey TG. Intertrochanteric fractures of the femur: A randomized prospective comparison of the Gamma nail and the Ambi hip screw. Aust N Z J Surg. 1996;66:151–5. doi: 10.1111/j.1445-2197.1996.tb01144.x. [DOI] [PubMed] [Google Scholar]
- 16.O’Brien PJ, Meek RN, Blachut PA, Broekhuyse HM, Sabharwal S. Fixation of intertrochanteric hip fractures: Gamma nail versus dynamic hip screw. A randomized, prospective study. Can J Surg. 1995;38:516–20. [PubMed] [Google Scholar]
- 17.Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993;75:789–93. doi: 10.1302/0301-620X.75B5.8376441. [DOI] [PubMed] [Google Scholar]
- 18.Simmermacher RK, Bosch AM, Van der Werken C. The AO/ASIF-Proximal Femoral Nail (PFN): A new device for the treatment of unstable proximal femoral fractures. Injury. 1999;30:327–32. doi: 10.1016/s0020-1383(99)00091-1. [DOI] [PubMed] [Google Scholar]
- 19.Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop. 1998;348:87–94. [PubMed] [Google Scholar]
- 20.Bess RJ, Jolly SA. Comparison of compression hip screw and gamma nail for treatment of peritrochanteric fractures. J South Orthop Assoc. 1997;6:73–9. [PubMed] [Google Scholar]
- 21.Cole JD, Ansel LJ. Intramedullary nail and lag-screw fixation of proximal femur fractures. Operative technique and preliminary results. Orthop Rev. 1994;(Suppl):35–44. [PubMed] [Google Scholar]
- 22.Fornander P, Thorngren KG, Tornquist H, Ahrengart L, Lindgren U. Swedish experience of the first 209 randomized patients with gamma nail vs. screw-plate. Acta Orthop Scand. 1992;63(Suppl 248):90. [Google Scholar]
- 23.Guyer P, Landolt M, Eberle C, Keller H. The gamma-nail as a resilient alternative to the dynamic hip screw in unstable proximal femoral fractures in the elderly. Helv Chir Acta. 1992;58:697–703. [PubMed] [Google Scholar]
- 24.Hoffmann R, Schmidmaier G, Schulz R, Schütz M, Südkamp NP. Classic nail versus DHS. A prospective randomised study of fixation of trochanteric femur fractures. Unfallchirurg. 1999;102:182–90. doi: 10.1007/s001130050391. [DOI] [PubMed] [Google Scholar]
- 25.Høgh J, Andersen K, Duus B, Hansen D, Hellberg S, Jakobsen B, et al. Gamma nail versus DHS in the treatment of trochanteric and subtrochanteric fractures. Acta Orthop Scand. 1992;63(Suppl 248):86–7. [Google Scholar]
- 26.Parker MJ, Pryor GA. Gamma versus DHS nailing for extracapsular femoral fractures.Meta-analysis of ten randomised trials. Int Orthop. 1996;20:163–8. doi: 10.1007/s002640050055. [DOI] [PubMed] [Google Scholar]
- 27.Wagner R, Weckbach A, Sellmair U, Blattert T. Extra-articular proximal femur fracture in the elderly- dynamic hip screw or intramedullary hip screw for fracture management? Langenbecks Arch Chir Suppl Kongressbd. 1996;113:963–6. [PubMed] [Google Scholar]
- 28.Babst R, Renner N, Biedermann M, Rosso R, Heberer M, Harder F, et al. Clinical results using the trochanter stabilizing plate (TSP): The modular extension of the dynamic hip screw (DHS) for internal fixation of selected unstable intertrochanteric fractures. J Orthop Trauma. 1998;12:392–9. doi: 10.1097/00005131-199808000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Hersche O, Heim D, Bodoky A, Regazzoni P. 4 fragment fractures of the proximal femur: Is the dynamic hip screw a suitable implant? Helv Chir Acta. 1989;56:577–80. [PubMed] [Google Scholar]
- 30.Whitelaw GP, Segal D, Sanzone CF, Ober NS, Hadley N. Unstable intertrochanteric/subtrochanteric fractures of the femur. Clin Orthop. 1990;252:238–45. [PubMed] [Google Scholar]


