Abstract
Background:
The treatment algorithm for sacral fracture associated with vertical shear pelvic fracture has not emerged. Our aim was to study a new approach of fixation for comminuted and vertically unstable fracture pattern with spinopelvic dissociation to overcome inconsistent outcome and avoid complications associated with fixations. We propose fixation with well-contoured thick reconstruction plate spreading across sacrum from one iliac bone to another with fixation points in iliac wing, sacral ala and sacral pedicle on either side. Present biomechanical study tests the four fixation pattern to compare their stiffness to vertical compressive forces.
Materials and Methods:
Dissection was performed on human cadavers through posterior midline paraspinal approach elevating erector spinae from insertion with two flaps. Feasibility of surgical exposure and placement of contoured plate for fixation was evaluated. Ten age and sex matched computed tomography scans of pelvis with both hips were obtained. Reconstructions were performed with advantage windows 4.2 (GE Light Speed QX/I, General Electric, Milwaukee, WI, USA). Using the annotation tools, direct digital CT measurement (0.6 mm increments) of three linear parameters was carried out. Readings were recorded at S2 sacral level. Pelvic CT scans were extensively studied for entry point, trajectory and estimated length for screw placement in S2 pedicle, sacral ala and iliac wing. Readings were recorded for desired angulation of screw in iliac wing ala of sacrum and sacral pedicle with respect to midline. The readings were analyzed by the values of mean and standard deviation. Biomechanical efficacy of fixation methods was studied separately on synthetic bone. Four fixation patterns given below were tested to compare their stiffness to vertical compressive forces: 1) Single S1 iliosacral screw (7.5 mm cancellous screw), 2) Two S1 and S2 iliosacral screws, 3) Isolated trans-iliosacral plate, 4) Trans-iliosacral plate + single S1 iliosacral screw.
Statistical Analysis:
Mean of desired angulation for inserting screws and percentage of displacement on biomechanical testing was evaluated.
Results:
Mean angulations for inserting sacral pedicel were 12.3° (SD 2.7°) convergent to midline and divergent of 14° (SD 2.3°) for sacral ala screw and 23° (SD 4.9°) for iliac wing screw. All screws needed to be inserted at an angle of 90° to sacral dorsum to avoid violation of root canals. Cross headed displacement across fracture site was measured and plotted against the applied vertical shear load of 300 N in five cycles each for all the four configurations. Also, the force required for cross headed displacement of 2.5 mm and 5 mm was recorded for all configurations. Transmitted load across both ischial tuberosities was measured to resolve unequal distribution of forces. Taking one screw construct (configuration 1) as standard base reference, trans-iliosacral plate construct (configuration 3) showed equal rigidity to standard reference. Two screw construct (configuration 2) was 12% stronger and trans-iliosacral plate (configuration 4) with screw was 9% stronger at 2.5 mm displacing on 300 N force, while it showed 30% and 6%, respectively, at 5 mm cross-headed displacement.
Conclusions:
Trans-iliosacral plating is feasible anatomically, biomechanically and radiologically for sacral fractures associated with vertical shear pelvic fractures. Low profile of plate reduces the risk of hardware prominence and decreases the need for implant removal. Also, the fixation pattern of plate allows to spare mobile lumbosacral junction which is an important segment for spinal mobility. Biomechanical studies revealed that rigidity offered by plate for cross headed displacement across fracture site is equal to sacroiliac screws and further rigidity of construct can be increased with addition of one more screw. There is need for precountered thicker plate in future.
Keywords: Spinopelvic dissociation, trans-iliosacral plating, unstable sacral spine fractures
INTRODUCTION
Sacral fractures occur in approximately 45% of all pelvic fractures.1 The pattern of the associated pelvic fracture has a significant impact on the location, stability, and treatment of the sacral fractures. Sacral fractures associated with vertical shear pelvic fractures are usually unstable patterns. Denis zone II and III fractures are usually associated with high degree of neurological involvement and often need decompression to offer favorable environment to aid neurological recovery.2 Vertical sacral fracture should make the surgeon more wary of fixation failure and loss of reduction.3 Trans-sacral plate, vertebro-pelvic fixator, or open reduction internal fixation are recommended by many authors for these injuries.4 Biomechanical stiffness for different types of traditional posterior fixations differs considerably according to the fracture pattern and often needs anterior ring stability, which is also a concern for surgical duration or additional surgical stabilization.
Rigid segmental lumbopelvic stabilization allows for reliable fracture reduction of the lumbosacral spine and posterior pelvic ring, permitting early mobilization without external immobilization and neurological improvement in a large number of patients. However, there are complications associated with these procedures, primarily related to infection, wound healing, and asymptomatic rod breakage, and are without long term sequelae. Also, they may need removal of implants early when they are prominent.5,6
The standard treatment protocol for patients presenting with fracture dislocations of the sacrum resulting from high-energy mechanisms remains unknown. The multicenter case reviews showed satisfactory outcomes with either non-operative or a variety of surgical methods. However, over the last 20 years, no consistent treatment algorithm for these severe injuries has emerged. We propose a method of fixation with well-contoured thick reconstruction plate spreading across sacrum from one iliac bone to another with fixation points in iliac wing, sacral ala and sacral pedicle on either side.
We propose fixation with well contained thick reconstruction plate spreading across sacrum from one iliac bone to another with fixation points in iliac wing, sacral ala and sacral pedicle on either side. Present biomechanical study tests the first fixation pattern to compare their stuffness to vertical compressive forces.
MATERIALS AND METHODS
Randomly chosen and conserved single, middle aged, male human cadaver was obtained from the Department of Human anatomy. Dissection was performed through posterior midline paraspinal approach elevating erector spinae from insertion with two flaps. Posterior ligamentous structures were kept intact. Six-hole, 4.5 mm thick, LCDCP was contoured so that it could be accommodated on the dorsal surface of the sacrum. Plate was fixed on intact cadaveric pelvis with 4.5 mm cortical screw in sacral pedicle, ala of sacrum and iliac wing, respectively, on either side [Figure 1].
Figure 1.
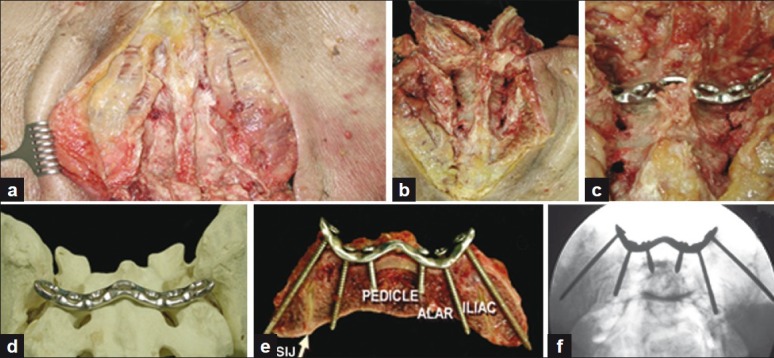
(a) Cadaveric midline exposure of sacral spine; (b) elevation of two erector spine flaps; (c) placement of contoured plate; (d) contoured plate matching dorsal surface of sacrum; (e) placement of sacral pedicle (S2) screw, ala screw and iliac wing screw; (f) inlet views of pelvis showing radiological appearance of fixation with screws
Radiological study
Ten age and sex matched computed tomography (CT) scans were obtained of pelvis with both hips. High longitudinal resolution and proper slice thickness are important for the performance of high-quality 2D and 3D reconstructions. Therefore, primary images were acquired using a standard algorithm with 1.25 mm slice thickness and 0.6 mm reconstruction interval. Reconstructions were performed with advantage windows 4.2 (GE LightSpeed QX/I, General Electric, Milwaukee, WI, USA).
Readings were recorded with multiplanar reconstructions as illustrated. Using the cursor, direct digital CT measurement (0.6 mm increments) of three linear parameters was carried out. All measurements were independently performed by both the authors [Figure 2].
Figure 2.
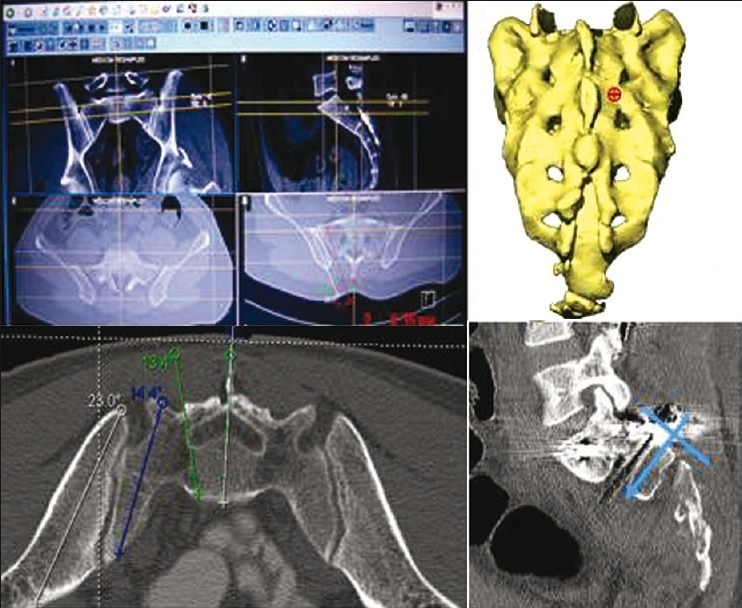
CT scan images showing use of annotation tools for trajectory of screw in axial and sagittal plane
Ideal screw placement occupies good bone stock without violation of central neural foramen and root canals. Pelvic CT scans were extensively studied for entry point, trajectory and estimated length for screw placement in S2 pedicle Sacral Ala and Iliac wing. Thirty readings were recorded at S2 sacral level. Readings were recorded for desired angulation of screw in iliac wing, ala of sacrum and sacral pedicle with respect to midline. The readings were analyzed by values of mean and standard deviation [Figure 2].
Biomechanical study
Fracture pattern simulating comminuted transforaminal Denis type 2 fractures was created with cutting saw. Pelvis with both hips was mounted on MTS 858 Bionix Material Testing Systems (MTS Systems Corporation, Eden Prairie, MN) simulating person in sitting position with three-point loading on S1 body and both ischium. Reflective markers were used to monitor 3D motion across the fracture site and the pubic symphysis. All the movements were recorded by micro motion digital camera. Four fixation patterns given below were tested to compare their stiffness to vertical compressive forces [Figure 3]:
Figure 3.
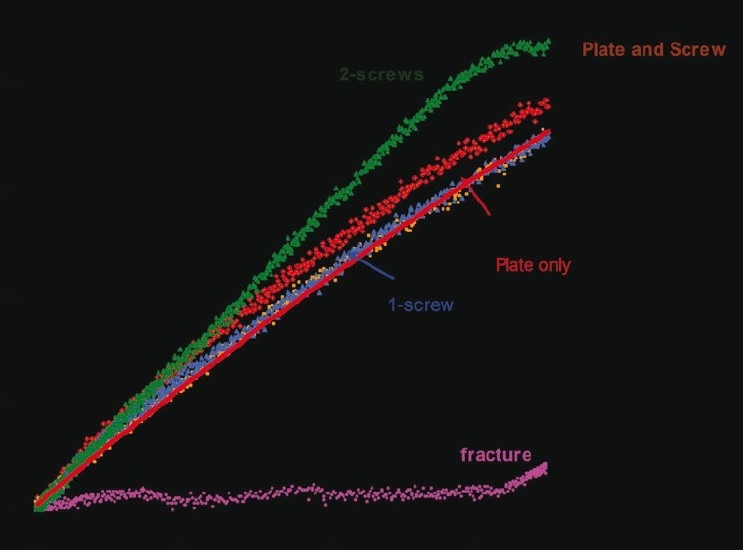
Four different fracture fixation configurations for a unilateral sacral fracture
Single S1 iliosacral screw (7.5 mm cancellous screw)
Two S1 and S2 iliosacral screws
Isolated trans-iliosacral plate
Trans-iliosacral plate + single S1 iliosacral screw
Compressive force (N) applied (Fs) on top of sacrum was measured by MTS machine [Figure 4]. Transmitted force was measured at ischial tuberosity by load cell (Ly). Cross-headed displacement (esy) of 2.5 mm and 5 mm across fracture site against the force applied was recorded using micro motion camera by displacement of radiolucent markers. Displacement of pelvis (esx) was measured with digital gauze.
Figure 4.
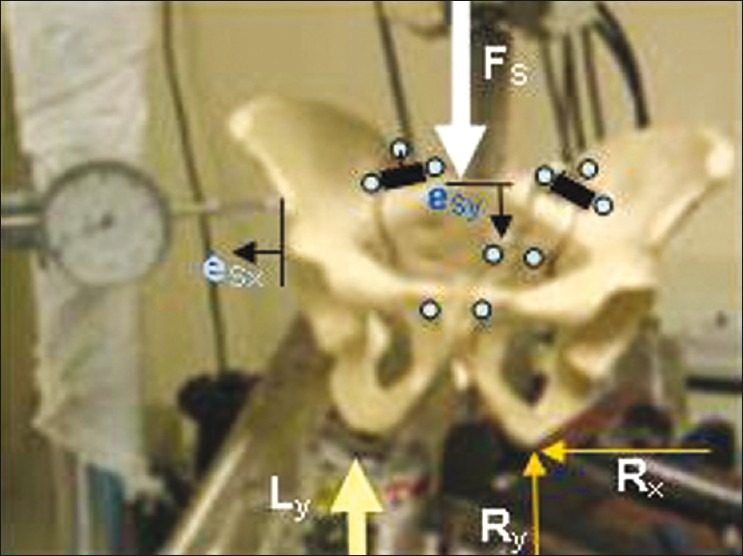
Biomechanical study to test and compare rigidity of trans-iliosacral plate
The above-mentioned four different fracture fixation configurations for a unilateral sacral fracture were evaluated with applied load (Fs) cross-head displacement (esy) curves simulating a person in a seated position. Biomechanical study done on synthetic bone not on cadaver, Mean of desired angulation for inserting screws and percentage of displacement on biomechanical testing evaluated.
RESULTS
Radiological study
Mean angulations for inserting sacral pedicle were 12.3° (SD 2.7°) convergent to midline and divergent of 14° (SD 2.3°) for sacral ala screw and 23° (SD 4.9°) for iliac wing screw. All screws needed to be inserted at an angle of 90° to sacral dorsum to avoid violation of root canals.
Biomechanical study
Cross-headed displacement across the fracture site was measured and plotted against the applied vertical shear load of 300 N in five cycles each for all the four configurations. Also, the force required for cross headed displacement of 2.5 mm and 5 mm was recorded for all configurations. Transmitted load across both ischial tuberosities was measured to resolve unequal distribution of forces [Figure 4].
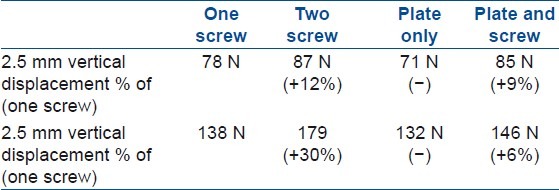
Taking one screw construct (configuration 1) as standard base reference, trans-iliosacral plate construct (configuration 3) showed equal rigidity to standard reference. Two screw construct (configuration 2) was 12% stronger and trans-iliosacral plate (configuration 4) with screw was 9% stronger at 2.5 mm displacing on 300 N force, while it showed 30% and 6%, respectively, at 5 mm cross-headed displacement [Table 1].
Table 1.
Comparison of strength (N) for a fixed displacement across the fracture site
DISCUSSION
Sacral fractures without a significant associated pelvic ring disruption, fractures not involving the lumbosacral junction, and fractures without neurological injury can be treated non operatively with restricted weight bearing. Fractures of the sacrum may result in a neurological injury in up to 25% of cases.7
While many sacral unstable fractures and fractures with associated nerve injury require surgical management, displaced or unstable sacral fractures are best treated by closed or open reduction and internal fixation. Following anatomic reduction, sacral fractures can be fixed with percutaneously placed screws, posterior sacral “tension band” plating, or posterior iliac rods. Surgical stabilization of any associated anterior pelvic ring injury is essential to improve the fixation stability.
Percutaneously placed iliosacral screws are commonly used for the fixation of sacroiliac joint disruptions and for sacral fractures. The ideal screw trajectory is more horizontal for the fixation of sacral fractures than for fixation of a sacroiliac joint disruption. Caution is exercised when fixing comminuted Denis type II fractures to avoid compression of the foramen that may result in iatrogenic neural injury. Adequate experience and intraoperative imaging are necessary to safely insert these screws as the safe corridor for placement is fairly small. In some patients, such as those with a dysmorphic sacrum, this safe corridor is even smaller and may preclude the placement of an iliosacral screw. In a review, Hasenboehler found 14.5% of trauma patients undergoing CT scan to have sacral dysmorphia.1 Inadvertent use of iliosacral screws, especially in comminuted zone II and III injuries associated with neurological injury, can be hazardous. This technique has well-recognized risks of nerve or vessel injury8,9
Transiliac posterior tension band fixation, while less commonly used than iliosacral screws, offers an alternative method for stabilization of the posterior pelvic ring.10 It is indicated in vertically unstable comminuted sacral fractures, for which iliosacral screws may be insufficient. It is also indicated in patients with a dysmorphic sacrum in whom there is no safe corridor for placement of iliosacral screws. Threaded rods or a posterior plate may be secured to the posterior ilium. Disadvantage of this fixation is the need for a larger surgical dissection, which has a greater risk of wound breakdown and infection, especially in the presence of the Morel-Lavallée lesion.11
Schildhauer et al.12 reported on the use of lumbopelvic fixation in 19 patients with Roy-Camille type 2 (n=4) sacral fractures with spinopelvic instability and cauda equina injuries. All of the sacral fractures successfully healed and none of the patients had loss of reduction. Fifteen of the 19 patients had full or partial recovery of bowel and bladder deficits. They reported that complete recovery of cauda equina function was more likely in patients with continuity of all sacral roots and in injuries where the initial deficit was incomplete.
In a biomechanical study, triangular osteosynthesis was shown to be superior to iliosacral screws alone for fixation of unstable transforaminal sacral fractures.13 Sagi et al.14 reported on the use of triangular osteosynthesis in 58 patients with vertically unstable transforaminal sacral fractures. Patients were allowed full weight bearing at 6 weeks, with only a 5% malunion rate. The authors noted a high rate of prominent and painful hardware (95%). Additional problems included iatrogenic L5 nerve injury in 13%, delayed union in 25%, and pronounced tilting of the L5 vertebral body with distraction of the L5/S1 facet joint ipsilateral to the fixation in 15%.
We propose a new method of fixation of sacral spine by contoured trans-iliosacral plate. Our comparative biomechanical study revealed that two construct screw was 12% stronger than one screw construct, and trans-iliosacral plate with additional screw was 9% stronger at 2.5 mm displacing on 300 N force, while it showed 30% and 6% strength, respectively, at 5 mm cross headed displacement. It allows adequate decompression, screw placement in sacral pedicle, ala of sacrum and iliac wing, providing strong bone for purchase. It helps to prevent undue compression across fracture site, endangering root compressing. Relative low profile plate will help to prevent wound-related problems.
CONCLUSION
Trans-iliosacral plating is feasible anatomically, biomechanically and radiologically for sacral fractures associated with vertical shear pelvic fractures. Low profile of plate reduces the risk of hardware prominence and decreases the need for implant removal. Also, the fixation pattern of plate allows to spare mobile lumbosacral junction which is an important segment for spinal mobility. Biomechanical studies revealed that rigidity offered by plate for cross headed displacement across fracture site is equal to sacroiliac screws and further rigidity of construct can be increased with addition of one more screw. There is need for precontoured thicker plate in future.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Hasenboehler EA, Stahel PF, Williams A. Presented at: 75th Annual meeting of the American Academy of Orthopaedic Surgeons. San Francisco, CA: 2008. Mar 5-9, Prevalence of sacral dysmorphia in a prospective trauma population: Implications for a “safe” surgical corridor for SI-screw placement. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaccaro AR, Lim DH, Brodke DS, Harris M, Chapman J, Schildhauer T, et al. Diagnosis and management of sacral spine fractures. J Bone Joint Surg Am. 2004;86:166–75. [PubMed] [Google Scholar]
- 3.Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2006;20(1 Suppl):S30–6. discussion S36. [PubMed] [Google Scholar]
- 4.Pohlemann T, Angst M, Schneider E, Ganz R, Tscherne H. Fixation of transforaminal sacrum fractures: A biomechanical study. J Orthop Trauma. 1993;7:107–17. doi: 10.1097/00005131-199304000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Bellabarba C, Schildhauer TA, Vaccaro AR, Chapman JR. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino- pelvic instability. Spine (Phila Pa 1976) 2006;31(11 Suppl):S80–8. doi: 10.1097/01.brs.0000217949.31762.be. [DOI] [PubMed] [Google Scholar]
- 6.Mouhsine E, Wettstein M, Schizas C, Borens O, Blanc CH, Leyvraz PF, et al. Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J. 2006;15:857–63. doi: 10.1007/s00586-004-0858-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta S, Auerbach JD, Born CT, Chin KR. Sacral fractures. J Amer Acad Orthop Surg. 2006;14:656–65. doi: 10.5435/00124635-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Altman DT, Jones CB, Routt ML., JR Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999;13:220–7. doi: 10.1097/00005131-199903000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Routt ML, Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: Early complications of the percutaneous technique. J Orthop Trauma. 1997;11:584–9. doi: 10.1097/00005131-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki T, Hak DJ, Ziran BH, Adams SA, Stahel PF, Morgan SJ, et al. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury. 2009;40:405–9. doi: 10.1016/j.injury.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 11.Hak DJ, Baran S, Stahel P. Sacral fractures: current strategies in diagnosis and management. Orthopedics. 2009;32:752. doi: 10.3928/01477447-20090818-18. [DOI] [PubMed] [Google Scholar]
- 12.schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML, Jr, Chapman JR. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447–57. doi: 10.1097/00005131-200608000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt ML., Jr Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: A cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Sagi HC, Militano U, Caron T, Lindvall E. A Comprehensive analysis with minimum 1-year follow-up of vertically unstable transforaminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma. 2009;23:313–21. doi: 10.1097/BOT.0b013e3181a32b91. [DOI] [PubMed] [Google Scholar]


